The Mediating Role of Social Camouflaging on the Relationship Between Autistic Traits and Orthorexic Symptoms
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sample and Procedures
2.2. Measures
2.2.1. The AdAS Spectrum
2.2.2. The CAT-Q
2.2.3. The ORTO-R
2.3. Statistical Analysis
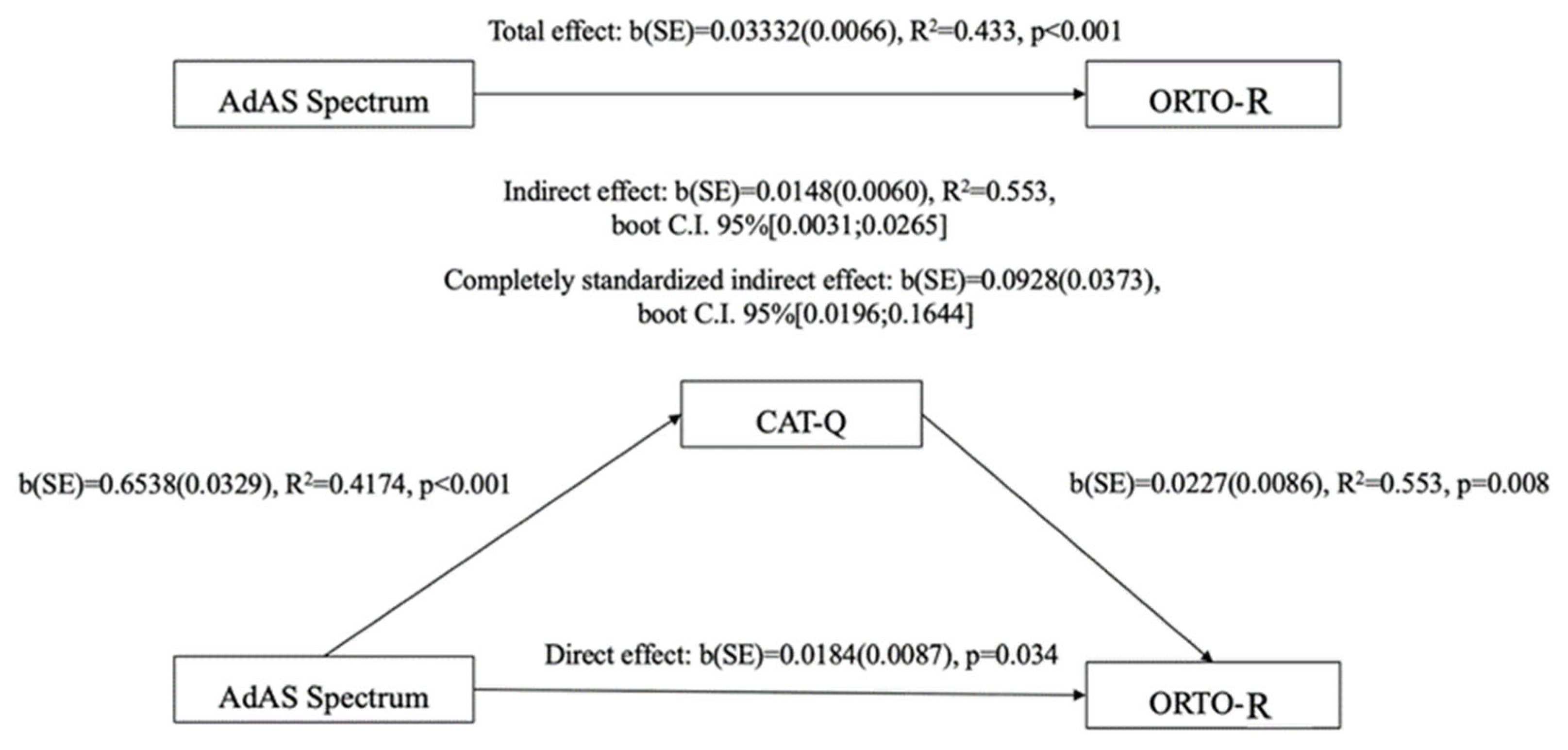
3. Results
4. Discussion
Limits
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Clemente-Suárez, V.J.; Beltrán-Velasco, A.I.; Redondo-Flórez, L.; Martín-Rodríguez, A.; Tornero-Aguilera, J.F. Global Impacts of Western Diet and Its Effects on Metabolism and Health: A Narrative Review. Nutrients 2023, 15, 2749. [Google Scholar] [CrossRef] [PubMed]
- Herrero, M.; Hugas, M.; Lele, U.; Wirakartakusumah, A.; Torero, M. A Shift to Healthy and Sustainable Consumption Patterns. In Science and Innovations for Food Systems Transformation; von Braun, J., Ed.; Springer: Cham, Switzerland, 2023; pp. 59–85. [Google Scholar]
- Chung, A.; Vieira, D.; Donley, T.; Tan, N.; Jean-Louis, G.; Kiely Gouley, K.; Seixas, A. Adolescent Peer Influence on Eating Behaviors via Social Media: Scoping Review. J. Med. Internet Res. 2021, 23, e19697. [Google Scholar] [CrossRef] [PubMed]
- Pilař, L.; Stanislavská, L.K.; Kvasnička, R.; Hartman, R.; Tichá, I. Healthy Food on Instagram Social Network: Vegan, Homemade and Clean Eating. Nutrients 2021, 13, 1991. [Google Scholar] [CrossRef] [PubMed]
- Springmann, M.; Wiebe, K.; Mason-D’Croz, D.; Sulser, T.B.; Rayner, M.; Scarborough, P. Health and nutritional aspects of sustainable diet strategies and their association with environmental impacts: A global modelling analysis with country-level detail. Lancet Planet. Health 2018, 2, e451–e461. [Google Scholar] [CrossRef]
- Barrett, B. Health and sustainability co-benefits of eating behaviors: Towards a science of dietary eco-wellness. Prev. Med. Rep. 2022, 28, 101878. [Google Scholar] [CrossRef]
- Rizzo, G.; Storz, M.A. Editorial: Ethical and sustainable food choice: Drivers and health effects. Front. Nutr. 2024, 11, 1455664. [Google Scholar] [CrossRef]
- Hargreaves, S.M.; Raposo, A.; Saraiva, A.; Zandonadi, R.P. Vegetarian Diet: An Overview through the Perspective of Quality of Life Domains. Int. J. Environ. Res. Public Health 2021, 18, 4067. [Google Scholar] [CrossRef]
- Mathieu, S.; Hanras, E.; Dorard, G. Associations between vegetarianism, body mass index, and eating disorders/disordered eating behaviours: A systematic review of literature. Int. J. Food Sci. Nutr. 2023, 74, 424–462. [Google Scholar] [CrossRef]
- Oussalah, A.; Levy, J.; Berthezène, C.; Alpers, D.H.; Guéant, J.L. Health outcomes associated with vegetarian diets: An umbrella review of systematic reviews and meta-analyses. Clin. Nutr. 2020, 39, 3283–3307. [Google Scholar] [CrossRef]
- Selinger, E.; Neuenschwander, M.; Koller, A.; Gojda, J.; Kühn, T.; Schwingshackl, L.; Arbaresko, J.; Schlesinger, S. Evidence of a vegan diet for health benefits and risks—An umbrella review of meta-analyses of observational and clinical studies. Crit. Rev. Food Sci. Nutr. 2023, 63, 9926–9936. [Google Scholar] [CrossRef]
- Godos, J.; Guglielmetti, M.; Ferraris, C.; Frias-Toral, E.; Domínguez Azpíroz, I.; Lipari, V.; Di Mauro, A.; Furnari, F.; Castellano, S.; Galvano, F.; et al. Mediterranean Diet and Quality of Life in Adults: A Systematic Review. Nutrients 2025, 17, 577. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Available online: https://www.who.int/news-room/fact-sheets/detail/healthy-diet (accessed on 14 February 2025).
- Bratman, S. Orthorexia vs. theories of healthy eating. Eat. Weight Disord. 2017, 22, 381–385. [Google Scholar] [CrossRef]
- López-Gil, J.F.; Tárraga-López, P.J.; Soledad Hershey, M.; López-Bueno, R.; Gutiérrez-Espinoza, H.; Soler-Marín, A.; Fernández-Montero, A.; Victoria-Montesinos, D. Overall proportion of orthorexia nervosa symptoms: A systematic review and meta-analysis including 30 476 individuals from 18 countries. J. Glob. Health 2023, 13, 04087. [Google Scholar] [CrossRef] [PubMed]
- Carpita, B.; Nardi, B.; Bonelli, C.; Pronestì, C.; Tognini, V.; Cremone, I.M.; Dell’Osso, L. Prevalence of orthorexia nervosa in clinical and non-clinical populations: A systematic review. CNS Spectr. 2024, 29, 549–569. [Google Scholar] [CrossRef]
- Ng, Q.X.; Lee, D.Y.X.; Yau, C.E.; Han, M.X.; Liew, J.J.L.; Teoh, S.E.; Ong, C.; Yaow, C.Y.L.; Chee, K.T. On Orthorexia Nervosa: A Systematic Review of Reviews. Psychopathology 2024, 57, 345–358. [Google Scholar] [CrossRef]
- Hanras, E.; Boujut, E.; Barrada, J.R.; Dorard, G. Differentiating healthy orthorexia from orthorexia nervosa: Sociodemographic, psychological and dietary characteristics in a French sample. Public Health Nutr. 2024, 27, e255. [Google Scholar] [CrossRef]
- Brodock, J.L.; Hopfer, H.; Masterson, T.D.; Hayes, J.E. Orthorexia Nervosa and Healthy Orthorexia in a Physically Active North American Population. Nutrients 2024, 16, 1107. [Google Scholar] [CrossRef] [PubMed]
- Dunn, T.M.; Bratman, S. On orthorexia nervosa: A review of the literature and proposed diagnostic criteria. Eat. Behav. 2016, 21, 11–17. [Google Scholar] [CrossRef]
- Dell’Osso, L.; Abelli, M.; Carpita, B.; Pini, S.; Castellini, G.; Carmassi, C.; Ricca, V. Historical evolution of the concept of anorexia nervosa and relationships with orthorexia nervosa, autism, and obsessive-compulsive spectrum. Neuropsychiatr. Dis. Treat. 2016, 12, 1651–1660. [Google Scholar]
- Dell’Osso, L.; Cremone, I.M.; Chiarantini, I.; Arone, A.; Casagrande, D.; Massimetti, G.; Carmassi, C.; Carpita, B. Investigating Orthorexia Nervosa With the ORTO-R in a Sample of University Students With or Without Subthreshold Autism Spectrum: Focus on Dietary Habits and Gender Differences. Front. Psychiatry 2022, 13, 900880. [Google Scholar] [CrossRef]
- Vaccari, G.; Cutino, A.; Luisi, F.; Giambalvo, N.; Navab Daneshmand, S.; Pinelli, M.; Maina, G.; Galeazzi, G.M.; Kaleci, S.; Albert, U.; et al. Is orthorexia nervosa a feature of obsessive-compulsive disorder? A multicentric, controlled study. Eat. Weight Disord. 2021, 26, 2531–2544. [Google Scholar] [CrossRef] [PubMed]
- Zagaria, A.; Vacca, M.; Cerolini, S.; Ballesio, A.; Lombardo, C. Associations between orthorexia, disordered eating, and obsessive compulsive symptoms: A systematic review and meta-analysis. Int. J. Eat. Disord. 2022, 55, 295–312. [Google Scholar] [CrossRef] [PubMed]
- Pontillo, M.; Zanna, V.; Demaria, F.; Averna, R.; Di Vincenzo, C.; De Biase, M.; Di Luzio, M.; Foti, B.; Tata, M.C.; Vicari, S. Orthorexia Nervosa, Eating Disorders, and Obsessive-Compulsive Disorder: A Selective Review of the Last Seven Years. J. Clin. Med. 2022, 11, 6134. [Google Scholar] [CrossRef] [PubMed]
- Cosh, S.M.; Olson, J.; Tully, P.J. Exploration of orthorexia nervosa and diagnostic overlap with eating disorders, anorexia nervosa and obsessive-compulsive disorder. Int. J. Eat. Disord. 2023, 56, 2155–2161. [Google Scholar] [CrossRef]
- Skella, P.; Chelmi, M.E.; Panagouli, E.; Garoufi, A.; Psaltopoulou, T.; Mastorakos, G.; Sergentanis, T.N.; Tsitsika, A. Orthorexia and Eating Disorders in Adolescents and Young Adults: A Systematic Review. Children 2022, 9, 514. [Google Scholar] [CrossRef]
- Atchison, A.E.; Zickgraf, H.F. Orthorexia nervosa and eating disorder behaviors: A systematic review of the literature. Appetite 2022, 177, 106134. [Google Scholar] [CrossRef]
- Łucka, I.; Mazur, A.; Łucka, A.; Sarzyńska, I.; Trojniak, J.; Kopańska, M. Orthorexia as an Eating Disorder Spectrum-A Review of the Literature. Nutrients 2024, 16, 3304. [Google Scholar] [CrossRef]
- Brytek-Matera, A.; Donini, L.M.; Krupa, M.; Poggiogalle, E.; Hay, P. Orthorexia nervosa and self-attitudinal aspects of body image in female and male university students. J. Eat. Disord. 2016, 4, 16. [Google Scholar] [CrossRef]
- Barnes, M.A.; Caltabiano, M.L. The interrelationship between orthorexia nervosa, perfectionism, body image and attachment style. Eat. Weight Disord. 2017, 22, 177–184. [Google Scholar] [CrossRef]
- Zickgraf, H.F.; Ellis, J.M.; Essayli, J.H. Disentangling orthorexia nervosa from healthy eating and other eating disorder symptoms: Relationships with clinical impairment, comorbidity, and self-reported food choices. Appetite 2019, 134, 40–49. [Google Scholar] [CrossRef]
- Oberle, C.D.; De Nadai, A.S.; Madrid, A.L. Orthorexia Nervosa Inventory (ONI): Development and validation of a new measure of orthorexic symptomatology. Eat. Weight Disord. 2021, 26, 609–622. [Google Scholar] [CrossRef] [PubMed]
- Cassone, S.; Rieger, E.; Crisp, D.A. Reducing anorexia nervosa stigma: An exploration of a social consensus intervention and the moderating effect of blameworthy attributions. J. Ment. Health 2020, 29, 506–512. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, C.; McNamara, N.; O’Hara, L.; McNicholas, M.; McNicholas, F. How do people with eating disorders experience the stigma associated with their condition? A mixed-methods systematic review. J. Ment. Health 2021, 30, 454–469. [Google Scholar] [CrossRef]
- Westwood, H.; Eisler, I.; Mandy, W.; Leppanen, J.; Treasure, J.; Tchanturia, K. Using the Autism-Spectrum Quotient to Measure Autistic Traits in Anorexia Nervosa: A Systematic Review and Meta-Analysis. J. Autism Dev. Disord. 2016, 46, 964–977. [Google Scholar] [CrossRef] [PubMed]
- Boltri, M.; Sapuppo, W. Anorexia Nervosa and Autism Spectrum Disorder: A Systematic Review. Psychiatry Res. 2021, 306, 114271. [Google Scholar] [CrossRef]
- Carpita, B.; Cremone, I.M.; Amatori, G.; Cappelli, A.; Salerni, A.; Massimetti, G.; Borgioli, D.; Carmassi, C.; Massai, R.; Dell’Osso, L. Investigating the relationship between orthorexia nervosa and autistic traits in a university population. CNS Spectr. 2022, 27, 613–620. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2022. [Google Scholar]
- Abu-Akel, A.; Allison, C.; Baron-Cohen, S.; Heinke, D. The distribution of autistic traits across the autism spectrum: Evidence for discontinuous dimensional subpopulations underlying the autism continuum. Mol. Autism 2019, 10, 24. [Google Scholar] [CrossRef]
- Talantseva, O.I.; Romanova, R.S.; Shurdova, E.M.; Dolgorukova, T.A.; Sologub, P.S.; Titova, O.S.; Kleeva, D.F.; Grigorenko, E.L. The global prevalence of autism spectrum disorder: A three-level meta-analysis. Front. Psychiatry 2023, 14, 1071181. [Google Scholar] [CrossRef]
- Demartini, B.; Ingrosso, G.; Serio, F.; Nisticò, V.; Broglia, G.; Bertani, A.; Faggioli, R.; Gambini, O.; Massimetti, G.; Dell’Osso, L.; et al. Prevalence of autistic traits and their relationships with other psychopathological domains in young adults seeking psychiatric attention: A cluster analysis. Eur. Psychiatry 2024, 67, e71. [Google Scholar] [CrossRef]
- Dell’Osso, L.; Cremone, I.M.; Chiarantini, I.; Nardi, B.; Pronestì, C.; Amatori, G.; Massimetti, E.; Signorelli, M.S.; Rocchetti, M.; Castellini, G.; et al. Autistic traits are associated with the presence of post-traumatic stress symptoms and suicidality among subjects with autism spectrum conditions and Anorexia nervosa. J. Psychiatr. Res. 2025, 181, 492–502. [Google Scholar] [CrossRef]
- Lai, M.C.; Lombardo, M.V.; Ruigrok, A.N.; Chakrabarti, B.; Auyeung, B.; Szatmari, P.; Happé, F.; Baron-Cohen, S. MRC AIMS Consortium Quantifying and exploring camouflaging in men and women with autism. Autism 2017, 21, 690–702. [Google Scholar] [CrossRef]
- Cook, J.; Hull, L.; Crane, L.; Mandy, W. Camouflaging in autism: A systematic review. Clin. Psychol. Rev. 2021, 89, 102080. [Google Scholar] [CrossRef]
- McQuaid, G.A.; Lee, N.R.; Wallace, G.L. Camouflaging in autism spectrum disorder: Examining the roles of sex, gender identity, and diagnostic timing. Autism 2022, 26, 552–559. [Google Scholar] [CrossRef]
- Loomes, R.; Hull, L.; Mandy, W.P.L. What Is the Male-to-Female Ratio in Autism Spectrum Disorder? A Systematic Review and Meta-Analysis. J. Am. Acad. Child Adolesc. Psychiatry 2017, 56, 466–474. [Google Scholar] [CrossRef] [PubMed]
- Huke, V.; Turk, J.; Saeidi, S.; Kent, A.; Morgan, J.F. Autism spectrum disorders in eating disorder populations: A systematic review. Eur. Eat. Disord. Rev. 2013, 21, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Adams, K.L.; Mandy, W.; Catmur, C.; Bird, G. Potential mechanisms underlying the association between feeding and eating disorders and autism. Neurosci. Biobehav. Rev. 2024, 162, 105717. [Google Scholar] [CrossRef]
- Schröder, S.S.; Danner, U.N.; Spek, A.A.; van Elburg, A.A. Exploring the intersection of autism spectrum disorder and eating disorders: Understanding the unique challenges and treatment considerations for autistic women with eating disorders. Curr. Opin. Psychiatry 2023, 36, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Dell’Osso, L.; Carpita, B.; Nardi, B.; Benedetti, F.; Dell’Oste, V.; Massimetti, G.; Cremone, I.M.; Barlati, S.; Castellini, G.; Luciano, M.; et al. Autistic traits distribution in different psychiatric conditions: A cluster analysis on the basis of the Adult Autism Subthreshold Spectrum (AdAS Spectrum) questionnaire. Psychiatry Res. 2023, 326, 115270. [Google Scholar] [CrossRef]
- Inal-Kaleli, I.; Dogan, N.; Kose, S.; Bora, E. Investigating the Presence of Autistic Traits and Prevalence of Autism Spectrum Disorder Symptoms in Anorexia Nervosa: A Systematic Review and Meta-Analysis. Int. J. Eat. Disord. 2025, 58, 66–90. [Google Scholar] [CrossRef]
- Giles, S.; Toohey, M.; Hughes, E.K.; Fuller-Tyszkiewicz, M.; Krug, I. Do orthorexia and intolerance of uncertainty mediate the relationship between autism spectrum traits and disordered eating symptoms? Eat. Weight Disord. 2021, 26, 2309–2316. [Google Scholar] [CrossRef]
- Dell’Osso, L.; Nardi, B.; Benedetti, F.; Cremone, I.M.; Casagrande, D.; Massimetti, G.; Carmassi, C.; Carpita, B. Orthorexia and autism spectrum in University workers: Relationship with gender, body mass index and dietary habits. Eat. Weight Disord. 2022, 27, 3713–3723. [Google Scholar] [CrossRef] [PubMed]
- Dell’Osso, L.; Gesi, C.; Massimetti, E.; Cremone, I.M.; Barbuti, M.; Maccariello, G.; Moroni, I.; Barlati, S.; Castellini, G.; Luciano, M.; et al. Adult Autism Subthreshold Spectrum (AdAS Spectrum): Validation of a questionnaire investigating subthreshold autism spectrum. Compr. Psychiatry 2017, 73, 61–83. [Google Scholar] [CrossRef] [PubMed]
- Hull, L.; Mandy, W.; Lai, M.C.; Baron-Cohen, S.; Allison, C.; Smith, P.; Petrides, K.V. Development and Validation of the Camouflaging Autistic Traits Questionnaire (CAT-Q). J. Autism Dev. Disord. 2019, 49, 819–833. [Google Scholar] [CrossRef]
- Dell’Osso, L.; Cremone, I.M.; Muti, D.; Massimetti, G.; Lorenzi, P.; Carmassi, C.; Carpita, B. Validation of the Italian version of the Camouflaging Autistic Traits Questionnaire (CAT-Q) in a University population. Compr. Psychiatry 2022, 114, 152295. [Google Scholar] [CrossRef] [PubMed]
- Rogoza, R.; Donini, L.M. Introducing ORTO-R: A revision of ORTO-15: Based on the re-assessment of original data. Eat. Weight Disord. 2021, 26, 887–895. [Google Scholar] [CrossRef]
- Donini, L.M.; Marsili, D.; Graziani, M.P.; Imbriale, M.; Cannella, C. Orthorexia nervosa: Validation of a diagnosis questionnaire. Eat. Weight Disord. 2005, 10, e28–e32. [Google Scholar] [CrossRef]
- Özdengül, F.; Yargic, M.P.; Solak, R.; Yaylali, O.; Kurklu, G.B. Assessment of orthorexia nervosa via ORTO-R scores of Turkish recreational and competitive athletes and sedentary individuals: A cross-sectional questionnaire study. Eat. Weight Disord. 2021, 26, 1111–1118. [Google Scholar] [CrossRef]
- McComb, S.E.; Mills, J.S. Orthorexia nervosa: A review of psychosocial risk factors. Appetite 2019, 140, 50–75. [Google Scholar] [CrossRef]
- Novara, C.; Pardini, S.; Visioli, F.; Meda, N. Orthorexia nervosa and dieting in a non-clinical sample: A prospective study. Eat. Weight Disord. 2022, 27, 2081–2093. [Google Scholar] [CrossRef]
- Brytek-Matera, A. Vegetarian diet and orthorexia nervosa: A review of the literature. Eat. Weight Disord. 2021, 26, 1–11. [Google Scholar] [CrossRef]
- McLean, C.P.; Kulkarni, J.; Sharp, G. Disordered eating and the meat-avoidance spectrum: A systematic review and clinical implications. Eat. Weight Disord. 2022, 27, 2347–2375. [Google Scholar] [CrossRef] [PubMed]
- Białek-Dratwa, A.; Stoń, W.; Staśkiewicz-Bartecka, W.; Grajek, M.; Krupa-Kotara, K.; Kowalski, O. The Psychosocial Aspects of Vegetarian Diets: A Cross-Sectional Study of the Motivations, Risks, and Limitations in Daily Life. Nutrients 2024, 16, 2504. [Google Scholar] [CrossRef] [PubMed]
- Heiss, S.; Hormes, J.M.; Timko, C.A. Vegetarianism and eating disorders. In Vegetarian and Plant-Based Diets in Health and Disease Prevention; Academic Press: Cambridge, MA, USA, 2017; pp. 51–69. [Google Scholar]
- Timko, C.A.; Hormes, J.M.; Chubski, J. Will the real vegetarian please stand up? An investigation of dietary restraint and eating disorder symptoms in vegetarians versus non-vegetarians. Appetite 2012, 58, 982–990. [Google Scholar] [CrossRef]
- Trautmann, J.; Rau, S.I.; Wilson, M.A.; Walters, C. Vegetarian students in their first year of college: Are they at risk for restrictive or disordered eating behaviors? Coll. Stud. J. 2008, 42, 340–347. [Google Scholar]
- Çiçekoğlu, P.; Tunçay, G.Y. A comparison of eating attitudes between vegans/vegetarians and nonvegans/nonvegetarians in terms of orthorexia nervosa. Arch. Psychiatr. Nurs. 2018, 32, 200–205. [Google Scholar] [CrossRef]
- Heiss, S.; Coffino, J.A.; Hormes, J.M. Eating and health behaviors in vegans compared to omnivores: Dispelling common myths. Appetite 2017, 118, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Fox, N.; Ward, K. Health, ethics and environment: A qualitative study of vegetarian motivations. Appetite 2008, 50, 422–429. [Google Scholar] [CrossRef]
- Donini, L.M.; Marsili, D.; Graziani, M.P.; Imbriale, M.; Cannella, C. Orthorexia nervosa: A preliminary study with a proposal for diagnosis and an attempt to measure the dimension of the phenomenon. Eat. Weight Disord. 2004, 9, 151–157. [Google Scholar] [CrossRef]
- Barthels, F.; Meyer, F.; Pietrowsky, R. Orthorexic and restrained eating behaviour in vegans, vegetarians, and individuals on a diet. Eat. Weight Disord. 2018, 23, 159–166. [Google Scholar] [CrossRef]
- Brzęk, A.; Ziora, K. A study on the relationship between orthorexia and vegetarianism using the BOT (Bratman Test for Orthorexia). Psychiatr. Pol. 2017, 51, 1133–1144. [Google Scholar]
- Luck-Sikorski, C.; Jung, F.; Schlosser, K.; Riedel-Heller, S.G. Is orthorexic behavior common in the general public? A large representative study in Germany. Eat. Weight Disord. 2019, 24, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Herranz Valera, J.; Acuña Ruiz, P.; Romero Valdespino, B.; Visioli, F. Prevalence of orthorexia nervosa among ashtanga yoga practitioners: A pilot study. Eat. Weight Disord. 2014, 19, 469–472. [Google Scholar] [CrossRef] [PubMed]
- Heiss, S.; Coffino, J.A.; Hormes, J.M. What does the ORTO-15 measure? Assessing the construct validity of a common orthorexia nervosa questionnaire in a meat avoiding sample. Appetite 2019, 135, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Brytek-Matera, A. Restrained Eating and Vegan, Vegetarian and Omnivore Dietary Intakes. Nutrients 2020, 12, 2133. [Google Scholar] [CrossRef]
- Şentürk, E.; Güler Şentürk, B.; Erus, S.; Geniş, B.; Coşar, B. Dietary patterns and eating behaviors on the border between healthy and pathological orthorexia. Eat. Weight Disord. 2022, 27, 3279–3288. [Google Scholar] [CrossRef]
- Koven, N.S.; Abry, A.W. The clinical basis of orthorexia nervosa: Emerging perspectives. Neuropsychiatr. Dis. Treat. 2015, 11, 385–394. [Google Scholar] [CrossRef]
- Mayes, S.D.; Zickgraf, H. Atypical eating behaviors in children and adolescents with autism, ADHD, other disorders, and typical development. Res. Autism Spectr. Disord. 2019, 64, 76–83. [Google Scholar] [CrossRef]
- Oldershaw, A.; Treasure, J.; Hambrook, D.; Tchanturia, K.; Schmidt, U. Is anorexia nervosa a version of autism spectrum disorders? Eur. Eat. Disord. Rev. 2011, 19, 462–474. [Google Scholar] [CrossRef]
- Dell’Osso, L.; Carpita, B.; Gesi, C.; Cremone, I.M.; Corsi, M.; Massimetti, E.; Muti, D.; Calderani, E.; Castellini, G.; Luciano, M.; et al. Subthreshold autism spectrum disorder in patients with eating disorders. Compr. Psychiatry 2018, 81, 66–72. [Google Scholar] [CrossRef]
- Carpita, B.; Muti, D.; Cremone, I.M.; Fagiolini, A.; Dell’Osso, L. Eating disorders and autism spectrum: Links and risks. CNS Spectr. 2022, 27, 272–280. [Google Scholar] [CrossRef]
- Dell’Osso, L.; Lorenzi, P.; Carpita, B. Autistic Traits and Illness Trajectories. Clin. Pract. Epidemiol. Ment. Health 2019, 15, 94–98. [Google Scholar] [CrossRef] [PubMed]
- Ratto, A.B.; Kenworthy, L.; Yerys, B.E.; Bascom, J.; Wieckowski, A.T.; White, S.W.; Wallace, G.L.; Pugliese, C.; Schultz, R.T.; Ollendick, T.H.; et al. What About the Girls? Sex-Based Differences in Autistic Traits and Adaptive Skills. J. Autism Dev. Disord. 2018, 48, 1698–1711. [Google Scholar] [CrossRef]
- Adamson, J.; Brede, J.; Babb, C.; Serpell, L.; Jones, C.R.G.; Fox, J.; Mandy, W. Towards identifying a method of screening for autism amongst women with restrictive eating disorders. Eur. Eat. Disord. Rev. 2022, 30, 592–603. [Google Scholar] [CrossRef]
- Brede, J.; Babb, C.; Jones, C.R.G.; Serpell, L.; Hull, L.; Adamson, J.; Baker, H.; Fox, J.R.E.; Mandy, W. The clinical characteristics of autistic women with restrictive eating disorders. BJPsych Open 2024, 10, e131. [Google Scholar] [CrossRef] [PubMed]
- Bradley, S.; Moore, F.; Duffy, F.; Clark, L.; Suratwala, T.; Knightsmith, P.; Gillespie-Smith, K. Camouflaging, not sensory processing or autistic identity, predicts eating disorder symptoms in autistic adults. Autism 2024, 28, 2858–2868. [Google Scholar] [CrossRef] [PubMed]
- Freeman, H. Green is the new black: The unstoppable rise of the healthy-eating guru. The Guardian: Health & Wellbeing, 27 June 2015. [Google Scholar]
- Marsh, S.; Campbell, D. Clean eating trend can be dangerous for young people, experts warn. The Guardian, 31 October 2016. [Google Scholar]
- Carrotte, E.R.; Vella, A.M.; Lim, M.S. Predictors of “Liking” Three Types of Health and Fitness-Related Content on Social Media: A Cross-Sectional Study. J. Med. Internet Res. 2015, 17, e205. [Google Scholar] [CrossRef]
- Turner, P.G.; Lefevre, C.E. Instagram use is linked to increased symptoms of orthorexia nervosa. Eat. Weight Disord. 2017, 22, 277–284. [Google Scholar] [CrossRef]
- Zemlyanskaya, Y.; Valente, M.; Syurina, E.V. Orthorexia nervosa and Instagram: Exploring the Russian-speaking conversation around #opтopeкcия. Eat. Weight Disord. 2022, 27, 1011–1020. [Google Scholar]
- Valente, M.; Renckens, S.; Bunders-Aelen, J.; Syurina, E.V. The #orthorexia community on Instagram. Eat. Weight Disord. 2022, 27, 473–482. [Google Scholar]
- Bhattacharya, A.; Cooper, M.; McAdams, C.; Peebles, R.; Timko, C.A. Cultural shifts in the symptoms of Anorexia Nervosa: The case of Orthorexia Nervosa. Appetite 2022, 170, 105869. [Google Scholar] [CrossRef]
- Lai, M.C.; Lombardo, M.V.; Auyeung, B.; Chakrabarti, B.; Baron-Cohen, S. Sex/gender differences and autism: Setting the scene for future research. J. Am. Acad. Child Adolesc. Psychiatry 2015, 54, 11–24. [Google Scholar] [CrossRef] [PubMed]
- Attwood, T.; Grandin, T.; Faherty, C. Asperger’s and Girls; Future Horizons: Arlington, TX, USA, 2006. [Google Scholar]
- Hiller, R.M.; Young, R.L.; Weber, N. Sex Differences in Autism Spectrum Disorder based on DSM-5 Criteria: Evidence from Clinician and Teacher Reporting. J. Abnorm. Child Psychol. 2014, 42, 1381–1393. [Google Scholar] [CrossRef]
- Carpita, B.; Nardi, B.; Pronestì, C.; Parri, F.; Giovannoni, F.; Cremone, I.M.; Pini, S.; Dell’Osso, L. May Female Autism Spectrum Be Masked by Eating Disorders, Borderline Personality Disorder, or Complex PTSD Symptoms? A Case Series. Brain Sci. 2023, 14, 37. [Google Scholar] [CrossRef]
- Nakazato, M. Do autism spectrum traits run in severe anorexia nervosa? Psychiatry Clin. Neurosci. 2022, 76, 415. [Google Scholar] [CrossRef] [PubMed]
- Brown, C.M.; Stokes, M.A. Intersection of Eating Disorders and the Female Profile of Autism. Psychiatr. Clin. N. Am. 2020, 43, 735–743. [Google Scholar] [CrossRef] [PubMed]
- Odent, M. Autism and anorexia nervosa: Two facets of the same disease? Med. Hypotheses 2010, 75, 79–81. [Google Scholar] [CrossRef]
- Dell’Osso, L.; Lorenzi, P.; Carpita, B. Camouflaging: Psychopathological meanings and clinical relevance in autism spectrum conditions. CNS Spectr. 2020, 26, 437–439. [Google Scholar] [CrossRef]
| Omnivorous | Vegetarian/Vegan | t | p | Cohen’s d | |
|---|---|---|---|---|---|
| AdAS Spectrum | |||||
| Childhood adolescence | 7.22 ± 3.92 | 7.79 ± 4.10 | −1.143 | 0.254 | −0.192 |
| Verbal Communication | 5.51 ± 3.13 | 6.21 ± 3.12 | −1.131 | 0.184 | −0.224 |
| Nonverbal Communication | 10.31 ± 4.95 | 11.63 ± 5.96 | −1.562 | 0.119 | −0.263 |
| Empathy | 2.94 ±2.08 | 2.66 ± 2.35 | 0.802 | 0.423 | −0.135 |
| Inflexibility and adherence to routine | 13.24 ± 6.91 | 15.08 ± 8.00 | −1.564 | 00.118 | −0.263 |
| Restricted interests and rumination | 8.13 ± 4.27 | 10.18 ± 4.63 | −2.838 | 0.005 * | −0.478 |
| Hyper/Hypo-reactivity to sensory input | 4.33 ± 3.28 | 5.24 ± 3.41 | −1.627 | 0.104 | −0.274 |
| AdAS Spectrum total score | 51.69 ± 23.08 | 58.97 ± 25.25 | −1.863 | 0.063 | −0.314 |
| CAT-Q | |||||
| Compensation | 24.75 ± 9.52 | 23.79 ± 9.85 | 0.601 | 0.548 | 0.101 |
| Masking | 31.26 ± 7.86 | 31.63 ± 8.67 | −0.280 | 0.780 | −0.047 |
| Assimilation | 26.84 ± 10.46 | 27.68 ± 10.15 | −0.482 | 0.630 | 0.081 |
| CAT-Q total score | 82.85 ± 23.65 | 83.10 ± 25.43 | 0.063 | 0.949 | −0.011 |
| ORTO-R | |||||
| ORTO-R total score | 13.57 ± 3.78 | 14.63 ± 3.31 | −1.680 | 0.001 * | −0.283 |
| AdAS High Scorers (N = 132) | AdAS Low Scorers (N = 422) | t | p | Cohen’s d | |
| ORTO-R | 14.73 ± 3.89 | 13.28 ± 3.64 | −3.93 | <0.001 * | −0.392 |
| CAT-Q High Scorers (N = 135) | CAT-Q Low Scorers (N = 419) | t | p | Cohen’s d | |
| ORTO-R | 14.70 ± 3.64 | 13.28 ± 3.72 | −3.88 | <0.001 * | −0.384 |
| Source | Type III Sum of Squares | df | Mean Square | F | p |
|---|---|---|---|---|---|
| Corrected Model | 308.426 | 3 | 102.809 | 7.594 | <0.001 * |
| Intercept | 61,119.312 | 1 | 61,119.312 | 4514.753 | <0.001 * |
| AdAS Spectrum 3 quartile | 60.201 | 1 | 60.201 | 4.447 | 0.035 * |
| CAT-Q 3 quartile | 51.184 | 1 | 51.184 | 3.781 | 0.052 |
| AdAS Spectrum 3 quartile * CAT-Q 3 quartile | 26.930 | 1 | 26.930 | 1.989 | 0.159 |
| Error | 7445.728 | 550 | 13.538 | ||
| Total | 110,565.000 | 554 | |||
| Corrected total | 7754.153 | 553 |
| b (SE) | BETA | t | p | C.I. 95% | ||
|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||
| constant | 10.777 (0.563) | 19.126 | <0.001 * | 9.670 | 11.883 | |
| AdAS Spectrum total score | 0.018 (0.009) | 0.115 | 2.127 | 0.034 * | 0.001 | 0.035 |
| CAT-Q total score | 0.023 (0.009) | 0.144 | 2.647 | 0.008 * | 0.006 | 0.039 |
| b (SE) | BETA | t | p | C.I. 95% | ||
|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||
| constant | 10.335 (0.636) | 16.253 | <0.001 * | 9.086 | 11.585 | |
| Compensation | 0.050 (0.023) | 0.127 | 2.213 | 0.027 * | 0.006 | 0.094 |
| Masking | 0.071 (0.026) | 0.150 | 2.771 | 0.006 * | 0.021 | 0.121 |
| Assimilation | −0.006 (0.019) | −0.017 | −0.313 | 0.755 | −0.044 | 0.032 |
| b (SE) | BETA | t | p | C.I. 95% | ||
|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||
| constant | 11.786 (0.389) | 30.280 | <0.001 * | 11.021 | 12.551 | |
| Childhood adolescence | −0.002 (0.051) | −0.002 | −0.037 | 0.971 | −0.103 | 0.099 |
| Verbal Communication | −0.209 (0.071) | −0.176 | −2.929 | 0.004 * | −0.349 | −0.069 |
| Nonverbal Communication | 0.163 (0.050) | 0.219 | 3.267 | 0.001 * | 0.065 | 0.262 |
| Empathy | −0.131 (0.087) | −0.074 | −1.510 | 0.132 | −0.301 | 0.039 |
| Inflexibility and adherence to routine | 0.069 (0.036) | 0.131 | 1.934 | 0.054 | −0.001 | 0.140 |
| Restricted interests and rumination | 0.106 (0.060) | 0.123 | 1.768 | 0.078 | −0.012 | 0.224 |
| Hyper/Hypo-reactivity to sensory input | −0.026 (0.066) | −0.023 | −0.399 | 0.690 | −0.155 | 0.103 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carpita, B.; Nardi, B.; Pronestì, C.; Cerofolini, G.; Filidei, M.; Bonelli, C.; Massimetti, G.; Cremone, I.M.; Pini, S.; Dell’Osso, L. The Mediating Role of Social Camouflaging on the Relationship Between Autistic Traits and Orthorexic Symptoms. Brain Sci. 2025, 15, 503. https://doi.org/10.3390/brainsci15050503
Carpita B, Nardi B, Pronestì C, Cerofolini G, Filidei M, Bonelli C, Massimetti G, Cremone IM, Pini S, Dell’Osso L. The Mediating Role of Social Camouflaging on the Relationship Between Autistic Traits and Orthorexic Symptoms. Brain Sciences. 2025; 15(5):503. https://doi.org/10.3390/brainsci15050503
Chicago/Turabian StyleCarpita, Barbara, Benedetta Nardi, Cristiana Pronestì, Gianluca Cerofolini, Matilde Filidei, Chiara Bonelli, Gabriele Massimetti, Ivan Mirko Cremone, Stefano Pini, and Liliana Dell’Osso. 2025. "The Mediating Role of Social Camouflaging on the Relationship Between Autistic Traits and Orthorexic Symptoms" Brain Sciences 15, no. 5: 503. https://doi.org/10.3390/brainsci15050503
APA StyleCarpita, B., Nardi, B., Pronestì, C., Cerofolini, G., Filidei, M., Bonelli, C., Massimetti, G., Cremone, I. M., Pini, S., & Dell’Osso, L. (2025). The Mediating Role of Social Camouflaging on the Relationship Between Autistic Traits and Orthorexic Symptoms. Brain Sciences, 15(5), 503. https://doi.org/10.3390/brainsci15050503







