Value of Glycemic Indices for Delayed Cerebral Ischemia after Aneurysmal Subarachnoid Hemorrhage: A Retrospective Single-Center Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patient Selection
2.2. Data Collection
2.3. Standard Treatment Algorithm
2.4. Determination of the Times for aSAH Event and DCI Onset
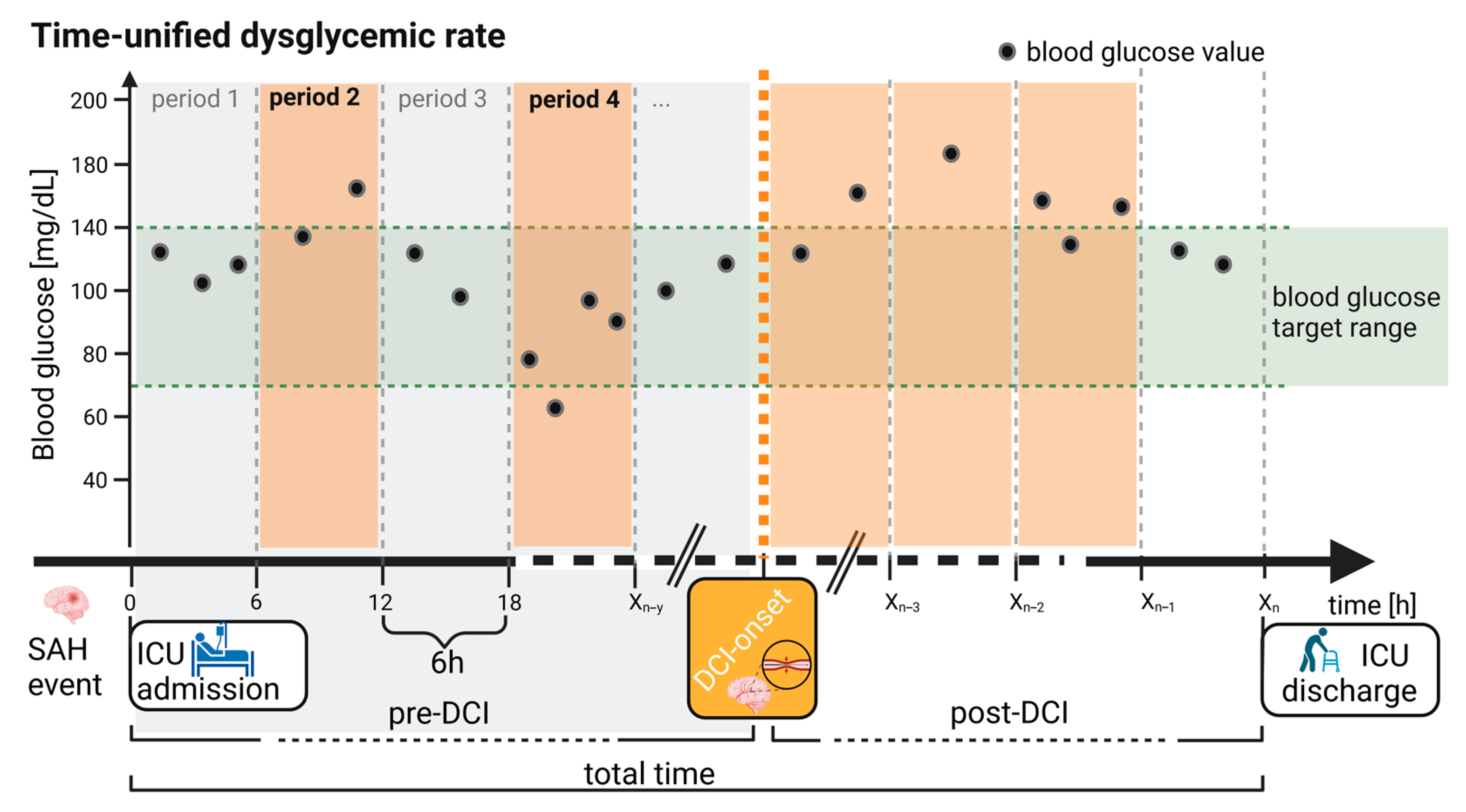
2.5. Analysis of Blood Glucose Values
2.6. Statistics
3. Results
3.1. Study Population
3.2. Increased Blood Glucose Values before DCI Onset
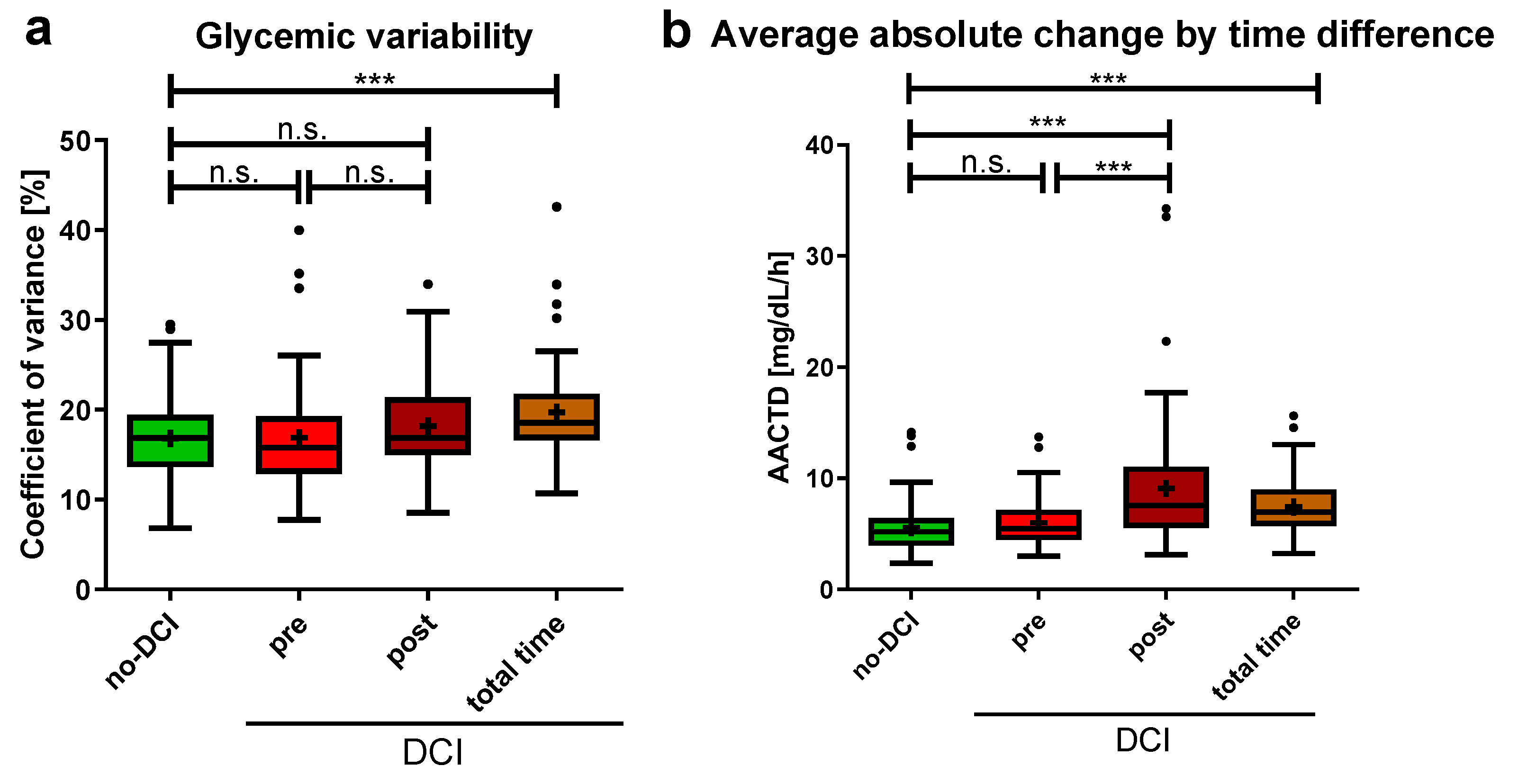
3.3. No Difference in Blood Glucose Fluctuation before DCI Onset
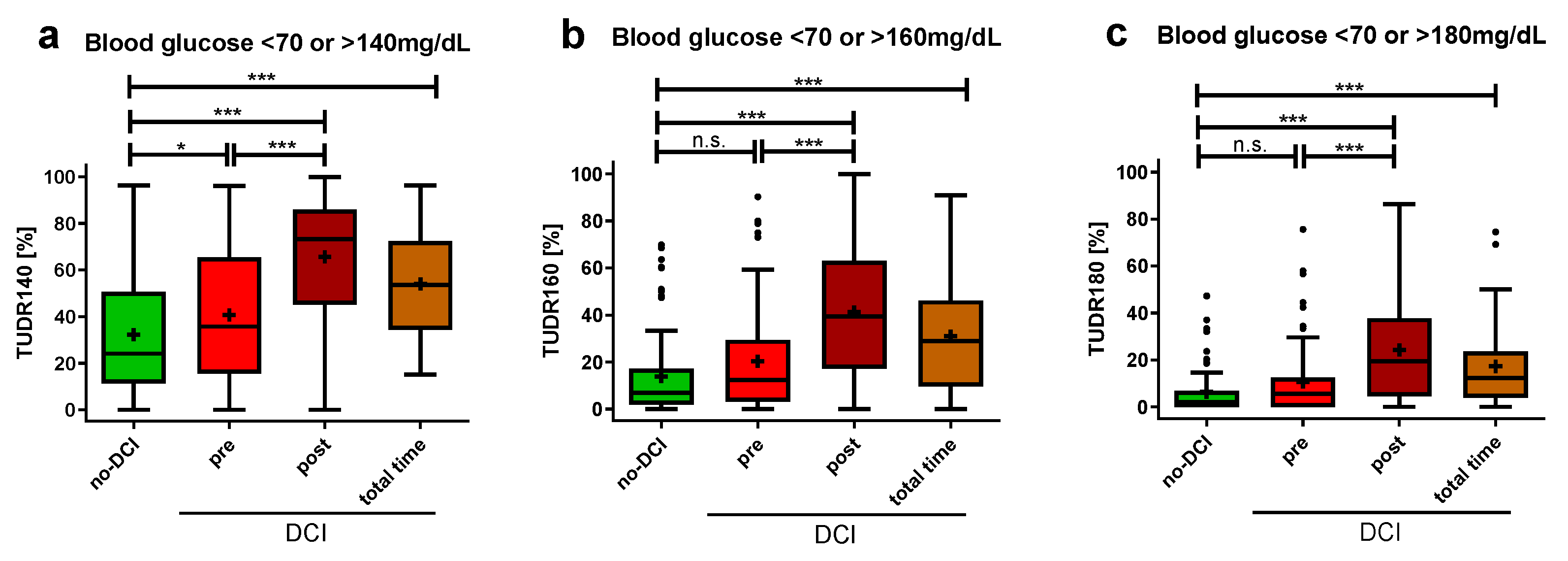
3.4. Higher Time-Unified Dysglycemic Rate before DCI Onset
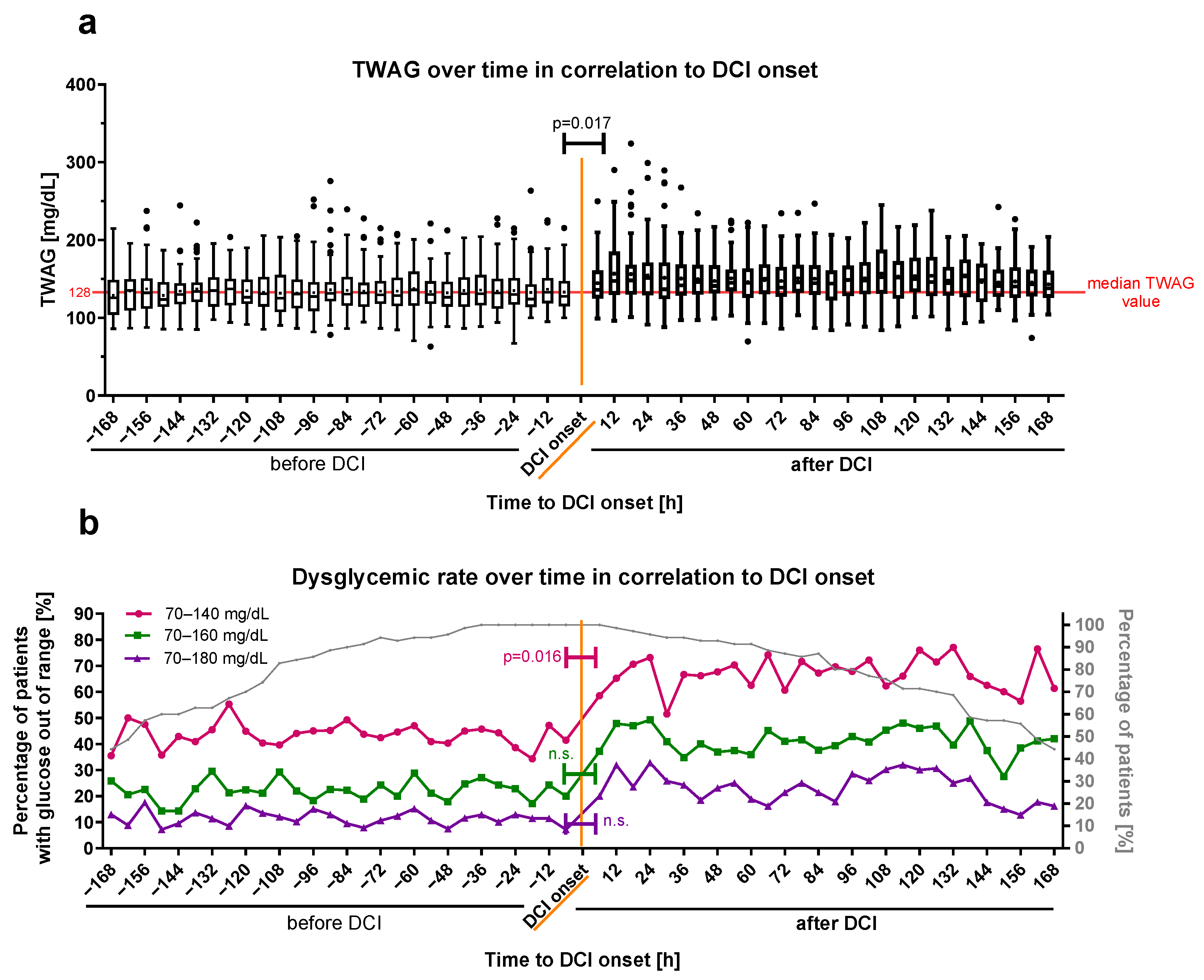
3.5. Time-Weighted Average Glucose Associated Positively with DCI
3.6. Time-Weighted Average Glucose and Time-Unified Dysglycemic Rate as Marker for DCI Onset
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AACTD | Average absolute change by time difference |
| aSAH | Aneurysmal subarachnoid hemorrhage |
| CV | Coefficient of glycemic variation |
| CT | Computed tomography scan |
| DCI | Delayed cerebral ischemia |
| ICD | International Classification of Diseases |
| ICH | Intracranial hemorrhage |
| ICU | Intensive care unit |
| MBG | Mean blood glucose |
| mFisher score | Modified Fisher score |
| SAH | Subarachnoid hemorrhage |
| SDH | Subdural hematoma |
| SAPS II | Simplified acute physiology score |
| TUDR | Time-unified dysglycemic rate |
| TUDR140 | Time-unified dysglycemic rate with target blood glucose range: 70–140 mg/dL |
| TUDR160 | Time-unified dysglycemic rate with target blood glucose range: 70–160 mg/dL |
| TUDR180 | Time-unified dysglycemic rate with target blood glucose range: 70–180 mg/dL |
| TWAG | Time-weighted average glucose |
References
- Lawton, M.T.; Vates, G.E. Subarachnoid Hemorrhage. N. Engl. J. Med. 2017, 377, 257–266. [Google Scholar] [CrossRef] [PubMed]
- Oka, F.; Chung, D.Y.; Suzuki, M.; Ayata, C. Delayed Cerebral Ischemia after Subarachnoid Hemorrhage: Experimental-Clinical Disconnect and the Unmet Need. Neurocrit. Care 2020, 32, 238–251. [Google Scholar] [CrossRef]
- Rigante, L.; van Lieshout, J.H.; Vergouwen, M.D.I.; van Griensven, C.H.S.; Vart, P.; van der Loo, L.; de Vries, J.; Vinke, R.S.; Etminan, N.; Aquarius, R.; et al. Time trends in the risk of delayed cerebral ischemia after subarachnoid hemorrhage: A meta-analysis of randomized controlled trials. Neurosurg. Focus 2022, 52, E2. [Google Scholar] [CrossRef]
- Macdonald, R.L.; Schweizer, T.A. Spontaneous subarachnoid haemorrhage. Lancet 2017, 389, 655–666. [Google Scholar] [CrossRef]
- Vergouwen, M.D.; Vermeulen, M.; van Gijn, J.; Rinkel, G.J.; Wijdicks, E.F.; Muizelaar, J.P.; Mendelow, A.D.; Juvela, S.; Yonas, H.; Terbrugge, K.G.; et al. Definition of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage as an outcome event in clinical trials and observational studies: Proposal of a multidisciplinary research group. Stroke 2010, 41, 2391–2395. [Google Scholar] [CrossRef] [PubMed]
- Geraghty, J.R.; Testai, F.D. Delayed Cerebral Ischemia after Subarachnoid Hemorrhage: Beyond Vasospasm and towards a Multifactorial Pathophysiology. Curr. Atheroscler. Rep. 2017, 19, 50. [Google Scholar] [CrossRef] [PubMed]
- Horst, V.; Kola, V.; Lemale, C.L.; Major, S.; Winkler, M.K.L.; Hecht, N.; Santos, E.; Platz, J.; Sakowitz, O.W.; Vatter, H.; et al. Spreading depolarization and angiographic spasm are separate mediators of delayed infarcts. Brain Commun. 2023, 5, fcad080. [Google Scholar] [CrossRef]
- Labak, C.M.; Shammassian, B.H.; Zhou, X.; Alkhachroum, A. Multimodality Monitoring for Delayed Cerebral Ischemia in Subarachnoid Hemorrhage: A Mini Review. Front. Neurol. 2022, 13, 869107. [Google Scholar] [CrossRef]
- Snider, S.B.; Migdady, I.; LaRose, S.L.; McKeown, M.E.; Regenhardt, R.W.; Lai, P.M.R.; Vaitkevicius, H.; Du, R. Transcranial-Doppler-Measured Vasospasm Severity is Associated with Delayed Cerebral Infarction after Subarachnoid Hemorrhage. Neurocrit. Care 2022, 36, 815–821. [Google Scholar] [CrossRef]
- Scherschinski, L.; Catapano, J.S.; Karahalios, K.; Koester, S.W.; Benner, D.; Winkler, E.A.; Graffeo, C.S.; Srinivasan, V.M.; Jha, R.M.; Jadhav, A.P.; et al. Electroencephalography for detection of vasospasm and delayed cerebral ischemia in aneurysmal subarachnoid hemorrhage: A retrospective analysis and systematic review. Neurosurg. Focus 2022, 52, E3. [Google Scholar] [CrossRef]
- Veldeman, M.; Albanna, W.; Weiss, M.; Conzen, C.; Schmidt, T.P.; Schulze-Steinen, H.; Wiesmann, M.; Clusmann, H.; Schubert, G.A. Invasive neuromonitoring with an extended definition of delayed cerebral ischemia is associated with improved outcome after poor-grade subarachnoid hemorrhage. J. Neurosurg. 2021, 134, 1527–1534. [Google Scholar] [CrossRef] [PubMed]
- Han, H.; Chen, Y.; Li, R.; Lin, F.; Lu, J.; Chen, X.; Wang, S. The value of early CT perfusion parameters for predicting delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage: A systematic review and meta-analysis. Neurosurg. Rev. 2022, 45, 2517–2531. [Google Scholar] [CrossRef] [PubMed]
- Melinosky, C.; Kincaid, H.; Claassen, J.; Parikh, G.; Badjatia, N.; Morris, N.A. The Modified Fisher Scale Lacks Interrater Reliability. Neurocrit. Care 2021, 35, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Megjhani, M.; Terilli, K.; Weiss, M.; Savarraj, J.; Chen, L.H.; Alkhachroum, A.; Roh, D.J.; Agarwal, S.; Connolly, E.S., Jr.; Velazquez, A.; et al. Dynamic Detection of Delayed Cerebral Ischemia: A Study in 3 Centers. Stroke 2021, 52, 1370–1379. [Google Scholar] [CrossRef]
- López-Gambero, A.J.; Martínez, F.; Salazar, K.; Cifuentes, M.; Nualart, F. Brain Glucose-Sensing Mechanism and Energy Homeostasis. Mol. Neurobiol. 2019, 56, 769–796. [Google Scholar] [CrossRef]
- Stoudt, K.; Chawla, S. Don’t Sugar Coat It: Glycemic Control in the Intensive Care Unit. J. Intensive Care Med. 2019, 34, 889–896. [Google Scholar] [CrossRef] [PubMed]
- Schmutzhard, E.; Rabinstein, A.A.; Participants in the International Multi-Disciplinary Consensus Conference on the Critical care Management of Subarachnoid Hemorrhage. Spontaneous subarachnoid hemorrhage and glucose management. Neurocrit. Care 2011, 15, 281–286. [Google Scholar] [CrossRef]
- Charpentier, C.; Audibert, G.; Guillemin, F.; Civit, T.; Ducrocq, X.; Bracard, S.; Hepner, H.; Picard, L.; Laxenaire, M.C. Multivariate analysis of predictors of cerebral vasospasm occurrence after aneurysmal subarachnoid hemorrhage. Stroke 1999, 30, 1402–1408. [Google Scholar] [CrossRef]
- Inagawa, T.; Yahara, K.; Ohbayashi, N. Risk factors associated with cerebral vasospasm following aneurysmal subarachnoid hemorrhage. Neurol. Med. Chir. 2014, 54, 465–473. [Google Scholar] [CrossRef]
- Kruyt, N.D.; Roos, Y.W.; Dorhout Mees, S.M.; van den Bergh, W.M.; Algra, A.; Rinkel, G.J.; Biessels, G.J. High mean fasting glucose levels independently predict poor outcome and delayed cerebral ischaemia after aneurysmal subarachnoid haemorrhage. J. Neurol. Neurosurg. Psychiatry 2008, 79, 1382–1385. [Google Scholar] [CrossRef]
- Badjatia, N.; Topcuoglu, M.A.; Buonanno, F.S.; Smith, E.E.; Nogueira, R.G.; Rordorf, G.A.; Carter, B.S.; Ogilvy, C.S.; Singhal, A.B. Relationship between hyperglycemia and symptomatic vasospasm after subarachnoid hemorrhage. Crit. Care Med. 2005, 33, 1603–1609, quiz 1623. [Google Scholar] [CrossRef]
- Mijiti, M.; Mijiti, P.; Axier, A.; Amuti, M.; Guohua, Z.; Xiaojiang, C.; Kadeer, K.; Xixian, W.; Geng, D.; Maimaitili, A. Incidence and Predictors of Angiographic Vasospasm, Symptomatic Vasospasm and Cerebral Infarction in Chinese Patients with Aneurysmal Subarachnoid Hemorrhage. PLoS ONE 2016, 11, e0168657. [Google Scholar] [CrossRef] [PubMed]
- Naidech, A.M.; Levasseur, K.; Liebling, S.; Garg, R.K.; Shapiro, M.; Ault, M.L.; Afifi, S.; Batjer, H.H. Moderate Hypoglycemia is associated with vasospasm, cerebral infarction, and 3-month disability after subarachnoid hemorrhage. Neurocrit. Care 2010, 12, 181–187. [Google Scholar] [CrossRef]
- Dumont, T.; Rughani, A.; Silver, J.; Tranmer, B.I. Diabetes mellitus increases risk of vasospasm following aneurysmal subarachnoid hemorrhage independent of glycemic control. Neurocrit. Care 2009, 11, 183–189. [Google Scholar] [CrossRef]
- van Donkelaar, C.E.; Dijkland, S.A.; van den Bergh, W.M.; Bakker, J.; Dippel, D.W.; Nijsten, M.W.; van der Jagt, M. Early Circulating Lactate and Glucose Levels After Aneurysmal Subarachnoid Hemorrhage Correlate with Poor Outcome and Delayed Cerebral Ischemia: A Two-Center Cohort Study. Crit. Care Med. 2016, 44, 966–972. [Google Scholar] [CrossRef]
- Matano, F.; Fujiki, Y.; Mizunari, T.; Koketsu, K.; Tamaki, T.; Murai, Y.; Yokota, H.; Morita, A. Serum Glucose and Potassium Ratio as Risk Factors for Cerebral Vasospasm after Aneurysmal Subarachnoid Hemorrhage. J. Stroke Cerebrovasc. Dis. 2019, 28, 1951–1957. [Google Scholar] [CrossRef] [PubMed]
- McIntyre, M.K.; Halabi, M.; Li, B.; Long, A.; Van Hoof, A.; Afridi, A.; Gandhi, C.; Schmidt, M.; Cole, C.; Santarelli, J.; et al. Glycemic indices predict outcomes after aneurysmal subarachnoid hemorrhage: A retrospective single center comparative analysis. Sci. Rep. 2021, 11, 158. [Google Scholar] [CrossRef]
- Okazaki, T.; Hifumi, T.; Kawakita, K.; Shishido, H.; Ogawa, D.; Okauchi, M.; Shindo, A.; Kawanishi, M.; Tamiya, T.; Kuroda, Y. Blood Glucose Variability: A Strong Independent Predictor of Neurological Outcomes in Aneurysmal Subarachnoid Hemorrhage. J. Intensive Care Med. 2018, 33, 189–195. [Google Scholar] [CrossRef]
- Sadan, O.; Feng, C.; Vidakovic, B.; Mei, Y.; Martin, K.; Samuels, O.; Hall, C.L. Glucose Variability as Measured by Inter-measurement Percentage Change is Predictive of In-patient Mortality in Aneurysmal Subarachnoid Hemorrhage. Neurocrit. Care 2020, 33, 458–467. [Google Scholar] [CrossRef]
- Kurtz, P.; Claassen, J.; Helbok, R.; Schmidt, J.; Fernandez, L.; Presciutti, M.; Stuart, R.M.; Connolly, E.S.; Lee, K.; Badjatia, N.; et al. Systemic glucose variability predicts cerebral metabolic distress and mortality after subarachnoid hemorrhage: A retrospective observational study. Crit. Care 2014, 18, R89. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. PLoS Med. 2007, 4, e296. [Google Scholar] [CrossRef] [PubMed]
- Weiss, M.; Albanna, W.; Conzen-Dilger, C.; Kastenholz, N.; Seyfried, K.; Ridwan, H.; Wiesmann, M.; Veldeman, M.; Schmidt, T.P.; Megjhani, M.; et al. Intraarterial Nimodipine versus Induced Hypertension for Delayed Cerebral Ischemia: A Modified Treatment Protocol. Stroke 2022, 53, 2607–2616. [Google Scholar] [CrossRef] [PubMed]
- Weiss, M.; Albanna, W.; Conzen, C.; Megjhani, M.; Tas, J.; Seyfried, K.; Kastenholz, N.; Veldeman, M.; Schmidt, T.P.; Schulze-Steinen, H.; et al. Optimal Cerebral Perfusion Pressure during Delayed Cerebral Ischemia after Aneurysmal Subarachnoid Hemorrhage. Crit. Care Med. 2022, 50, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Badawi, O.; Yeung, S.Y.; Rosenfeld, B.A. Evaluation of glycemic control metrics for intensive care unit populations. Am. J. Med. Qual. 2009, 24, 310–320. [Google Scholar] [CrossRef]
- Song, J.W.; Shim, J.K.; Yoo, K.J.; Oh, S.Y.; Kwak, Y.L. Impact of intraoperative hyperglycaemia on renal dysfunction after off-pump coronary artery bypass. Interact. Cardiovasc. Thorac. Surg. 2013, 17, 473–478. [Google Scholar] [CrossRef]
- Yoo, S.; Lee, H.J.; Lee, H.; Ryu, H.G. Association Between Perioperative Hyperglycemia or Glucose Variability and Postoperative Acute Kidney Injury after Liver Transplantation: A Retrospective Observational Study. Anesth. Analg. 2017, 124, 35–41. [Google Scholar] [CrossRef]
- Hryciw, B.N.; Ghossein, J.; Rochwerg, B.; Meggison, H.; Fernando, S.M.; Kyeremanteng, K.; Tran, A.; Seely, A.J.E. Glycemic Variability as a Prognostic Factor for Mortality in Patients with Critical Illness: A Systematic Review and Meta-Analysis. Crit. Care Explor. 2024, 6, e1025. [Google Scholar] [CrossRef]
- Shi, M.; Zhang, T.B.; Li, X.F.; Zhang, Z.Y.; Li, Z.J.; Wang, X.L.; Zhao, W.Y. The prognostic value of hyperglycemia in aneurysmal subarachnoid hemorrhage: A systematic review and meta-analysis. Neurosurg. Rev. 2022, 45, 3717–3728. [Google Scholar] [CrossRef]
- Joya, A.; Plaza-García, S.; Padro, D.; Aguado, L.; Iglesias, L.; Garbizu, M.; Gómez-Vallejo, V.; Laredo, C.; Cossío, U.; Torné, R.; et al. Multimodal imaging of the role of hyperglycemia following experimental subarachnoid hemorrhage. J. Cereb. Blood Flow. Metab. 2024, 44, 726–741. [Google Scholar] [CrossRef]
- Huang, Y.H.; Chung, C.L.; Tsai, H.P.; Wu, S.C.; Chang, C.Z.; Chai, C.Y.; Lee, T.C.; Kwan, A.L. Hyperglycemia Aggravates Cerebral Vasospasm after Subarachnoid Hemorrhage in a Rat Model. Neurosurgery 2017, 80, 809–815. [Google Scholar] [CrossRef]
- Vergouwen, M.D.; van Geloven, N.; de Haan, R.J.; Kruyt, N.D.; Vermeulen, M.; Roos, Y.B. Increased cortisol levels are associated with delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Neurocrit. Care 2010, 12, 342–345. [Google Scholar] [CrossRef]
- Chen, H.Y.; Elmer, J.; Zafar, S.F.; Ghanta, M.; Moura Junior, V.; Rosenthal, E.S.; Gilmore, E.J.; Hirsch, L.J.; Zaveri, H.P.; Sheth, K.N.; et al. Combining Transcranial Doppler and EEG Data to Predict Delayed Cerebral Ischemia after Subarachnoid Hemorrhage. Neurology 2022, 98, e459–e469. [Google Scholar] [CrossRef] [PubMed]
- Csók, I.; Grauvogel, J.; Scheiwe, C.; Bardutzky, J.; Wehrum, T.; Beck, J.; Reinacher, P.C.; Roelz, R. Basic Surveillance Parameters Improve the Prediction of Delayed Cerebral Infarction after Aneurysmal Subarachnoid Hemorrhage. Front. Neurol. 2022, 13, 774720. [Google Scholar] [CrossRef] [PubMed]
- Whittle, C.; Hollingworth, M.A.; Dulhanty, L.; Patel, H.C. What are the predictors of delayed cerebral ischaemia (DCI) after aneurysmal subarachnoid haemorrhage? An up-to-date systematic review. Acta Neurochir. 2023, 165, 3643–3650. [Google Scholar] [CrossRef]
- Hu, P.; Li, Y.; Liu, Y.; Guo, G.; Gao, X.; Su, Z.; Wang, L.; Deng, G.; Yang, S.; Qi, Y.; et al. Comparison of Conventional Logistic Regression and Machine Learning Methods for Predicting Delayed Cerebral Ischemia after Aneurysmal Subarachnoid Hemorrhage: A Multicentric Observational Cohort Study. Front. Aging Neurosci. 2022, 14, 857521. [Google Scholar] [CrossRef] [PubMed]
- Ge, S.; Chen, J.; Wang, W.; Zhang, L.-b.; Teng, Y.; Yang, C.; Wang, H.; Tao, Y.; Chen, Z.; Li, R.; et al. Predicting who has delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage using machine learning approach: A multicenter, retrospective cohort study. BMC Neurol. 2024, 24, 177. [Google Scholar] [CrossRef] [PubMed]
- Steiner, T.; Juvela, S.; Unterberg, A.; Jung, C.; Forsting, M.; Rinkel, G.; European Stroke, O. European Stroke Organization guidelines for the management of intracranial aneurysms and subarachnoid haemorrhage. Cerebrovasc. Dis. 2013, 35, 93–112. [Google Scholar] [CrossRef]
- Liu, D.; Tang, Y.; Zhang, Q. Admission Hyperglycemia Predicts Long-Term Mortality in Critically Ill Patients with Subarachnoid Hemorrhage: A Retrospective Analysis of the MIMIC-III Database. Front. Neurol. 2021, 12, 678998. [Google Scholar] [CrossRef]
- Frontera, J.A.; Fernandez, A.; Claassen, J.; Schmidt, M.; Schumacher, H.C.; Wartenberg, K.; Temes, R.; Parra, A.; Ostapkovich, N.D.; Mayer, S.A. Hyperglycemia after SAH: Predictors, associated complications, and impact on outcome. Stroke 2006, 37, 199–203. [Google Scholar] [CrossRef]
- Bilotta, F.; Spinelli, A.; Giovannini, F.; Doronzio, A.; Delfini, R.; Rosa, G. The effect of intensive insulin therapy on infection rate, vasospasm, neurologic outcome, and mortality in neurointensive care unit after intracranial aneurysm clipping in patients with acute subarachnoid hemorrhage: A randomized prospective pilot trial. J. Neurosurg. Anesthesiol. 2007, 19, 156–160. [Google Scholar] [CrossRef]
- DeJournett, J.; Nekludov, M.; DeJournett, L.; Wallin, M. Performance of a closed-loop glucose control system, comprising a continuous glucose monitoring system and an AI-based controller in swine during severe hypo- and hyperglycemic provocations. J. Clin. Monit. Comput. 2021, 35, 317–325. [Google Scholar] [CrossRef] [PubMed]


| Study Population | Delayed Cerebral Ischemia | |||
|---|---|---|---|---|
| Variable | Total (n = 151) | No (n = 81) | Yes (n = 70) | p-Value |
| Demography | ||||
| Age [years] | 55.2 ± 12.4 | 57.2 ± 12.6 | 52.9 ± 11.8 | 0.035 |
| Sex (female) | 101 (66.9%) | 53 (65.4%) | 48 (68.6%) | 0.731 |
| Body mass index [kg/m2] a | 26.3 ± 5.5 | 26.0 ± 4.9 | 26.5 ± 6.1 | 0.691 |
| Medical history | ||||
| Diabetes mellitus type 2 | 7 (4.6%) | 6 (7.4%) | 1 (1.4%) | 0.123 |
| Hypertension | 66 (43.7%) | 39 (48.1%) | 27 (38.6%) | 0.254 |
| Stroke history | 7 (4.6%) | 3 (3.7%) | 4 (5.7%) | 0.705 |
| History of SAH | 6 (4.0%) | 3 (3.7%) | 3 (4.3%) | 1.000 |
| Chronic kidney failure | 1 (0.7%) | 1 (1.2%) | 0 (0.0%) | 1.000 |
| Chronic liver disease | 3 (2.0%) | 2 (2.5%) | 1 (1.4%) | 1.000 |
| Psychiatric disorder | 14 (9.3%) | 9 (11.1%) | 5 (7.1%) | 0.575 |
| Alcohol addiction | 13 (8.6%) | 6 (7.4%) | 7 (10.0%) | 0.578 |
| Smoking history | 51 (33.8%) | 26 (32.1%) | 25 (35.7%) | 0.731 |
| Sah scores | ||||
| Hunt and Hess score | ||||
| 1–3 | 105 (69.5%) | 60 (74.1%) | 45 (64.3%) | 0.293 |
| 4–5 | 46 (30.4%) | 21 (25.9%) | 25 (35.7%) | 0.217 |
| mFisher score | ||||
| 1–2 | 72 (47.7%) | 51 (63.0%) | 21 (30.0%) | <0.001 |
| 3–4 | 79 (52.3%) | 30 (37.0%) | 49 (70.0%) | <0.001 |
| Sah treatment | ||||
| Endovascular treatment b | 90 (59.6%) | 49 (60.4%) | 41 (58.6%) | 1.000 |
| Surgical clipping b | 57 (37.7%) | 29 (35.8%) | 28 (40.0%) | 0.617 |
| Time from onset to ICU admission [h] | 10.1 ± 12.7 | 10.2 ± 13.9 | 9.9 ± 11.2 | 0.902 |
| Ruptured aneurysm location | ||||
| Internal carotid | 18 (11.9%) | 7 (8.6%) | 11 (15.7%) | 0.213 |
| Anterior cerebral | 15 (9.9%) | 8 (9.9%) | 7 (10.0%) | 1.000 |
| Anterior communicating | 52 (34.4%) | 26 (32.1%) | 26 (37.1%) | 0.607 |
| Middle cerebral | 34 (22.5%) | 19 (23.5%) | 15 (21.4%) | 0.846 |
| Posterior communicating | 15 (9.9%) | 9 (11.1%) | 6 (8.6%) | 0.786 |
| Vertebral | 6 (4.0%) | 4 (4.9%) | 2 (2.9%) | 0.686 |
| Basilar | 10 (6.6%) | 7 (8.6%) | 3 (4.3%) | 0.341 |
| Other | 1 (0.7%) | 1 (1.2%) | 0 (0.0%) | 1.000 |
| ICU key facts | ||||
| SAPS II Score a | 37.4 ± 9.1 | 36.0 ± 9.0 | 39.1 ± 9.2 | 0.039 |
| ICU length of stay [d] | 25.2 ± 15.0 | 19.6 ± 10.8 | 31.7 ± 16.5 | <0.001 |
| ICU mortality | 28 (18.5%) | 9 (11.1%) | 19 (27.1%) | 0.020 |
| Hospital length of stay [d] | 30.2 ± 16.2 | 25.2 ± 12.1 | 36.1 ± 18.3 | <0.001 |
| Mechanical ventilation [h] | 366.4 ± 417.5 | 235.8 ± 328.0 | 517.6 ± 459.3 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Deininger, M.M.; Weiss, M.; Wied, S.; Schlycht, A.; Haehn, N.; Marx, G.; Hoellig, A.; Schubert, G.A.; Breuer, T. Value of Glycemic Indices for Delayed Cerebral Ischemia after Aneurysmal Subarachnoid Hemorrhage: A Retrospective Single-Center Study. Brain Sci. 2024, 14, 849. https://doi.org/10.3390/brainsci14090849
Deininger MM, Weiss M, Wied S, Schlycht A, Haehn N, Marx G, Hoellig A, Schubert GA, Breuer T. Value of Glycemic Indices for Delayed Cerebral Ischemia after Aneurysmal Subarachnoid Hemorrhage: A Retrospective Single-Center Study. Brain Sciences. 2024; 14(9):849. https://doi.org/10.3390/brainsci14090849
Chicago/Turabian StyleDeininger, Matthias Manfred, Miriam Weiss, Stephanie Wied, Alexandra Schlycht, Nico Haehn, Gernot Marx, Anke Hoellig, Gerrit Alexander Schubert, and Thomas Breuer. 2024. "Value of Glycemic Indices for Delayed Cerebral Ischemia after Aneurysmal Subarachnoid Hemorrhage: A Retrospective Single-Center Study" Brain Sciences 14, no. 9: 849. https://doi.org/10.3390/brainsci14090849
APA StyleDeininger, M. M., Weiss, M., Wied, S., Schlycht, A., Haehn, N., Marx, G., Hoellig, A., Schubert, G. A., & Breuer, T. (2024). Value of Glycemic Indices for Delayed Cerebral Ischemia after Aneurysmal Subarachnoid Hemorrhage: A Retrospective Single-Center Study. Brain Sciences, 14(9), 849. https://doi.org/10.3390/brainsci14090849






