Improving Outcomes in People with Spinal Cord Injury: Encouraging Results from a Multidisciplinary Advanced Rehabilitation Pathway
Abstract
1. Introduction
- -
- Evaluate the feasibility of an integrated intervention path for SCI.
- -
- Investigate how the intervention path influences the overall quality of life for individuals with SCI.
- -
- Observe and measure the impact of the intervention path on cognitive, motor, and behavioral outcomes.
2. Materials and Methods
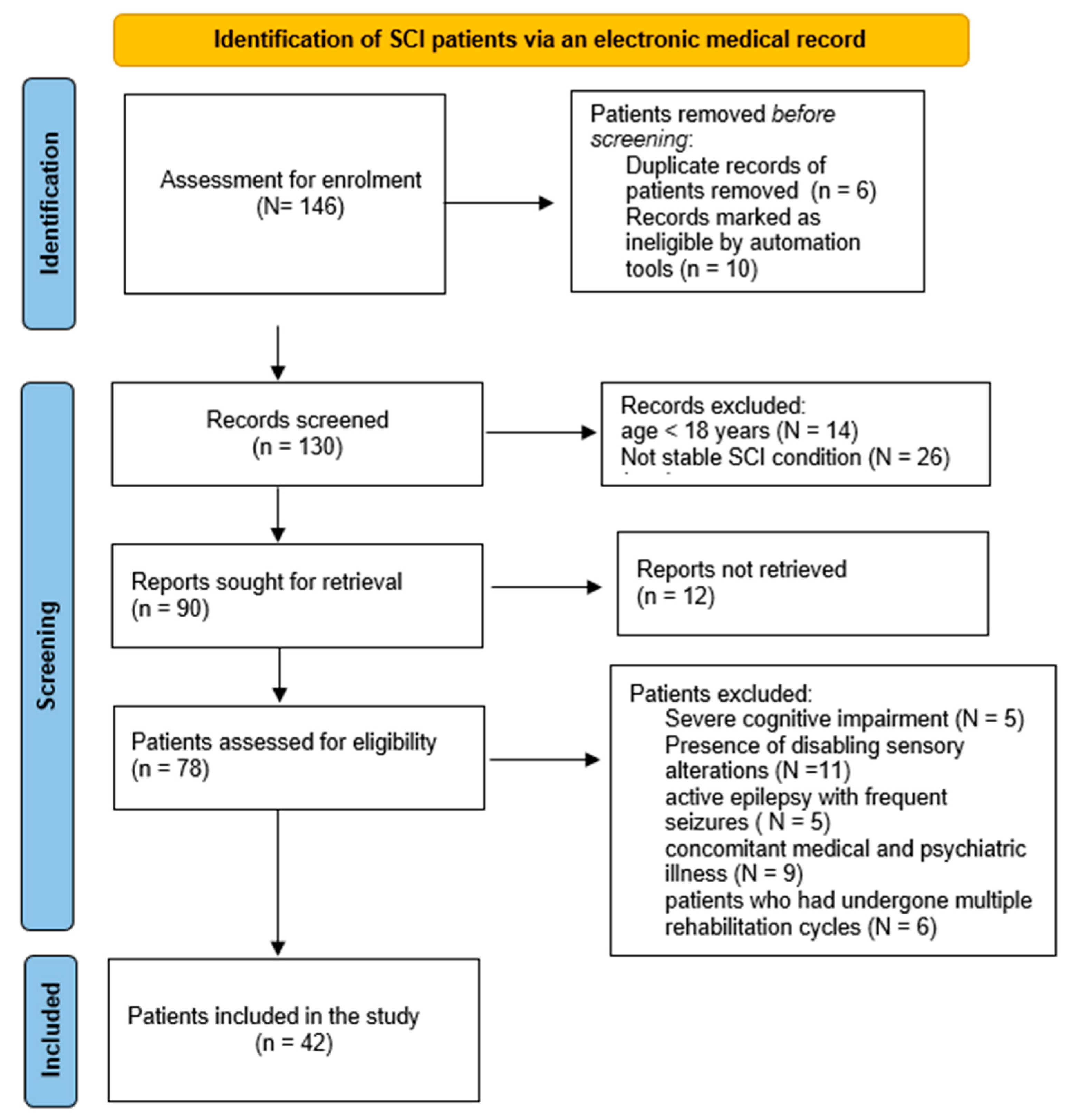
2.1. Study Design and Population
2.2. Procedures
2.3. Description of the Innovative Pathway
- (A)
- Evaluation at the admission
- (B)
- Rehabilitation Plan
- (C)
- Rehabilitation protocol
- -
- A total of 5 to 7 physiotherapy sessions tailored to individual needs.
- -
- A total of 6 to 10 robotic treatments per week, meticulously customized according to the patient’s specific physical requirements.
- -
- A total of 3 psychological sessions weekly, comprising a supportive interview and two cognitive treatments employing VR or other innovative tools, targeting specific areas for improvement.
- -
- A total of 2 to 5 speech therapy sessions every week.
- -
- A total of 3 to 5 occupational therapy sessions per week.
- -
- A total of 1 neuro-sexual consultation per week, readily available upon request.
- (D)
- End of hospitalization
2.4. Outcome Measures
2.5. Statistical Analysis
3. Results
4. Discussion
4.1. Motor Outcome
4.2. Cognitive Domains
4.3. Mood and Depression
4.4. Motivation, Patient Satisfaction, Quality of Life
4.5. Limits to the Use of Innovative Devices
4.6. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dumont, R.J.; Okonkwo, D.O.; Verma, S.; Hurlbert, R.J.; Boulos, P.T.; Ellegala, D.B.; Dumont, A.S. Acute spinal cord injury, part I: Pathophysiologic mechanisms. Clin. Neuropharmacol. 2001, 24, 254–264. [Google Scholar] [CrossRef]
- Zhou, H.; Lou, Y.; Chen, L.; Kang, Y.; Liu, L.; Cai, Z.; Anderson, D.B.; Wang, W.; Zhang, C.; Wang, J.; et al. Epidemiological and clinical features, treatment status, and economic burden of traumatic spinal cord injury in China: A hospital-based retrospective study. Neural Regen. Res. 2024, 19, 1126–1133. [Google Scholar] [CrossRef] [PubMed]
- Han, J.M.; Choi, W.S.; Choi, H.; Jang, B.-H.; Kim, H.-J.; Son, C.H.; Park, J.Y.; Kim, Y.S.; Jang, H.J.; Kim, J.H. Treatment of major depressive disorder (MDD) or dysthymic disorder (DD) in spinal cord injury (SCI) patients: A protocol for a systematic review and network meta-analysis. BMJ Open 2022, 12, e055800. [Google Scholar] [CrossRef] [PubMed]
- Maroufi, S.F.; Mohammadi, E.; Ohadi, M.A.D.; Hagen, E.-M.; Chalangari, M.; Jazayeri, S.B.; Safdarian, M.; Zadegan, S.A.; Ghodsi, Z.; Rahimi-Movaghar, V. Incidence of traumatic spinal cord injury worldwide: A systematic review, data integration, and update. World Neurosurg X 2023, 18, 100171. [Google Scholar] [CrossRef]
- Hachem, L.D.; Ahuja, C.S.; Fehlings, M.G. Assessment and management of acute spinal cord injury: From point of injury to rehabilitation. J. Spinal Cord Med. 2017, 40, 665–675. [Google Scholar] [CrossRef] [PubMed]
- Bennett, J.M.; Das, J.; Emmady, P.D. Spinal Cord Injuries. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Maggio, M.G.; Naro, A.; De Luca, R.; Latella, D.; Balletta, T.; Caccamo, L.; Pioggia, G.; Bruschetta, D.; Calabrò, R.S. Body Representation in Patients with Severe Spinal Cord Injury: A Pilot Study on the Promising Role of Powered Exoskeleton for Gait Training. J. Pers. Med. 2022, 12, 619. [Google Scholar] [CrossRef] [PubMed]
- Torregrossa, F.; Sallì, M.; Grasso, G. Emerging Therapeutic Strategies for Traumatic Spinal Cord Injury. World Neurosurg. 2020, 140, 591–601. [Google Scholar] [CrossRef] [PubMed]
- Miguel-Rubio, A.; Rubio, M.D.; Salazar, A.; Moral-Munoz, J.A.; Requena, F.; Camacho, R.; Lucena-Anton, D. Is Virtual Reality Effective for Balance Recovery in Patients with Spinal Cord Injury? A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 2861. [Google Scholar] [CrossRef] [PubMed]
- Riva, G.; Baños, R.M.; Botella, C.; Mantovani, F.; Gaggioli, A. Transforming Experience: The Potential of Augmented Reality and Virtual Reality for Enhancing Personal and Clinical Change. Front. Psychiatry 2016, 7, 164. [Google Scholar] [CrossRef]
- Sheridan, T.B. Musing on telepresence and virtual presence. Presence Teleoperators Virtual Environ. 1992, 1, 120–125. [Google Scholar] [CrossRef]
- Formica, C.; Bonanno, L.; Latella, D.; Ferrera, M.C.; Maresca, G.; Logiudice, A.L.; Sorbera, C.; Brigandì, A.; Di Lorenzo, G.; Marino, S. The effect of Computer Assisted Rehabilitation Environment (CAREN) in cognitive impairment and coping strategies in Parkinson’s disease: A preliminary study. Sci. Rep. 2023, 13, 2214. [Google Scholar] [CrossRef]
- Settimo, C.; De Cola, M.C.; Pironti, E.; Muratore, R.; Giambò, F.M.; Alito, A.; Tresoldi, M.; La Fauci, M.; De Domenico, C.; Tripodi, E.; et al. Virtual Reality Technology to Enhance Conventional Rehabilitation Program: Results of a Single-Blind, Randomized, Controlled Pilot Study in Patients with Global Developmental Delay. J. Clin. Med. 2023, 12, 4962. [Google Scholar] [CrossRef]
- De Miguel-Rubio, A.; Muñoz-Pérez, L.; Alba-Rueda, A.; Arias-Avila, M.; Rodrigues-de-Souza, D.P. A Therapeutic Approach Using the Combined Application of Virtual Reality with Robotics for the Treatment of Patients with Spinal Cord Injury: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 8772. [Google Scholar] [CrossRef]
- Daunoraviciene, K.; Adomaviciene, A.; Svirskis, D.; Griškevičius, J.; Juocevicius, A. Necessity ofearly stage verticalization in patients with brain and spinal cord injuries: Preliminary study. Technol. Health Care 2018, 26, 613–623. [Google Scholar] [CrossRef]
- Stampacchia, G.; Gazzotti, V.; Olivieri, M.; Andrenelli, E.; Bonaiuti, D.; Calabrò, R.S.; Carmignano, S.M.; Cassio, A.; Fundaro, C.; Companini, I.; et al. Gait robot-assisted rehabilitation in persons with spinal cord injury: A scoping review. NeuroRehabilitation 2022, 51, 609–647. [Google Scholar] [CrossRef]
- Herrera-Valenzuela, D.; Díaz-Peña, L.; Redondo-Galán, C.; Arroyo, M.J.; Cascante-Gutiérrez, L.; Gil-Agudo, Á.; Moreno, J.C.; Del-Ama, A.J. A qualitative study to elicit user requirements for lower limb wearable exoskeletons for gait rehabilitation in spinal cord injury. J. Neuroeng. Rehabil. 2023, 20, 138. [Google Scholar] [CrossRef]
- Maggioni, S.; Lünenburger, L.; Riener, R.; Curt, A.; Bolliger, M.; Melendez-Calderon, A. Assessing walking ability using a robotic gait trainer: Opportunities and limitations of assist-as-needed control in spinal cord injury. J. Neuroeng. Rehabil. 2023, 20, 121. [Google Scholar] [CrossRef]
- Shin, J.C.; Jeon, H.R.; Kim, D.; Min, W.K.; Lee, J.S.; Cho, S.I.; Oh, D.S.; Yoo, J. Effects of end-effector robot-assisted gait training on gait ability, muscle strength, and balance in patients with spinal cord injury. NeuroRehabilitation 2023, 53, 335–346. [Google Scholar] [CrossRef]
- den Brave, M.; Beaudart, C.; de Noordhout, B.M.; Gillot, V.; Kaux, J.F. Effect of robot-assisted gait training on quality of life and depression in neurological impairment: A systematic review and meta-analysis. Clin. Rehabil. 2023, 37, 876–890. [Google Scholar] [CrossRef]
- Sachdeva, R.; Gao, F.; Chan, C.C.H.; Krassioukov, A.V. Cognitive function after spinal cord injury: A systematic review. Neurology 2018, 91, 611–621. [Google Scholar] [CrossRef]
- Maggio, M.G.; Bonanno, M.; Manuli, A.; Calabrò, R.S. Do Individuals with Spinal Cord Injury Benefit from Semi-Immersive Virtual Reality Cognitive Training? Preliminary Results from an Exploratory Study on an Underestimated Problem. Brain Sci. 2023, 13, 945. [Google Scholar] [CrossRef]
- Calabrò, R.S.; Naro, A.; Leo, A.; Bramanti, P. Usefulness of robotic gait training plus neuromodulation in chronic spinal cord injury: A case report. J. Spinal Cord Med. 2017, 40, 118–121. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Kirshblum, S.; Waring, W., 3rd. Updates for the International Standards for Neurological Classification of Spinal Cord Injury. Phys. Med. Rehabil. Clin. N. Am. 2014, 25, 505–517. [Google Scholar] [CrossRef]
- Fugl-Meyer, A.R.; Jääskö, L.; Leyman, I.; Olsson, S.; Steglind, S. The post-stroke hemiplegic patient. 1. a method for evaluation of physical performance. Scand. J. Rehabil. Med. 1975, 7, 13–31. [Google Scholar] [CrossRef]
- Wei, W.; Ke, L.; Na, W.; Cuiping, Y.; Shouwei, Y. Evaluation of postural instability in stroke patient during quiet standing. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2017, 2017, 2522–2525. [Google Scholar]
- Di Rauso, G.; Castellucci, A.; Cavallieri, F.; Tozzi, A.; Fioravanti, V.; Monfrini, E.; Gessani, A.; Rossi, J.; Campanini, I.; Merlo, A.; et al. Speech, Gait, and Vestibular Function in Cerebellar Ataxia with Neuropathy and Vestibular Areflexia Syndrome. Brain Sci. 2023, 13, 1467. [Google Scholar] [CrossRef]
- World Health Organization. Towards a Common Language for Functioning, Disability and Health ICF; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Manuli, A.; Maggio, M.G.; Tripoli, D.; Gullì, M.; Cannavò, A.; La Rosa, G.; Sciarrone, F.; Avena, G.; Calabrò, R.S. Patients’ perspective and usability of innovation technology in a new rehabilitation pathway: An exploratory study in patients with multiple sclerosis. Mult. Scler. Relat. Disord. 2020, 44, 102312. [Google Scholar] [CrossRef]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.; Erbauch, J. Beck Depression Inventory (BDI) [Database Record]; APA PsycTests; American Psychological Association: Washington, DC, USA, 1961. [Google Scholar] [CrossRef]
- An, J.; Cao, Q.; Lin, W.; An, J.; Wang, Y.; Yang, L.; Yang, C.; Wang, D.; Sun, S. Cognition in patients with traumatic brain injury measured by the Montreal Cognitive Assessment-Basic. Appl. Neuropsychol. Adult 2021, 28, 124–131. [Google Scholar] [CrossRef]
- Thayaparan, A.J.; Mahdi, E. The Patient Satisfaction Questionnaire Short Form (PSQ-18) as an adaptable, reliable, and validated tool for use in various settings. Med. Educ. Online 2013, 18, 21747. [Google Scholar] [CrossRef]
- Ware, J., Jr.; Kosinski, M.; Keller, S.D. A 12-Item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef]
- Calabrò, R.S.; Cacciola, A.; Bertè, F.; Manuli, A.; Leo, A.; Bramanti, A.; Naro, A.; Milardi, D.; Bramanti, P. Robotic gait rehabilitation and substitution devices in neurological disorders: Where are we now? Neurol. Sci. 2016, 37, 503–514. [Google Scholar] [CrossRef]
- Calabrò, R.S.; Russo, M.; Naro, A.; De Luca, R.; Leo, A.; Tomasello, P.; Molonia, F.; Dattola, V.; Bramanti, A.; Bramanti, P. Robotic gait training in multiple sclerosis rehabilitation: Can virtual reality make the difference? Findings from a randomized controlled trial. J. Neurol. Sci. 2017, 377, 25–30. [Google Scholar] [CrossRef]
- Langhorne, P.; Coupar, F.; Pollock, A. Motor recovery after stroke: A systematic review. Lancet Neurol. 2009, 8, 741–754. [Google Scholar] [CrossRef]
- Kwakkel, G.; Kollen, B.J.; Krebs, H.I. Effects of robot-assisted therapy on upper limb recovery after stroke: A systematic review. Neurorehabil. Neural Repair 2008, 22, 111–121. [Google Scholar] [CrossRef]
- Oña, E.D.; Garcia-Haro, J.M.; Jardón, A.; Balaguer, C. Robotics in Health Care: Perspectives of Robot-Aided Interventions in Clinical Practice for Rehabilitation of Upper Limbs. Appl. Sci. 2019, 9, 2586. [Google Scholar] [CrossRef]
- Aderinto, N.; Olatunji, G.; Abdulbasit, M.O.; Edun, M.; Aboderin, G.; Egbunu, E. Exploring the efficacy of virtual reality-based rehabilitation in stroke: A narrative review of current evidence. Ann Med. 2023, 55, 2285907. [Google Scholar] [CrossRef]
- Nam, K.Y.; Kim, H.J.; Kwon, B.S.; Park, J.W.; Lee, H.J.; Yoo, A. Robot-assisted gait training (Lokomat) improves walking function and activity in people with spinal cord injury: A systematic review. J. Neuroeng. Rehabil. 2017, 14, 24. [Google Scholar] [CrossRef]
- Zhao, H.; Yang, J.; Yang, J.; Jiang, H.; Qin, Y.; Lei, Q. Evaluation of the improvement of walking ability in patients with spinal cord injury using lower limb rehabilitation robots based on data science. Transl. Neurosci. 2023, 14, 20220320. [Google Scholar] [CrossRef]
- Maggio, M.G.; Latella, D.; Maresca, G.; Sciarrone, F.; Manuli, A.; Naro, A.; De Luca, R.; Calabrò, R.S. Virtual Reality and Cognitive Rehabilitation in People with Stroke: An Overview. J. Neurosci. Nurs. 2019, 51, 101–105. [Google Scholar] [CrossRef]
- Calabrò, R.S.; Naro, A.; Russo, M.; Leo, A.; De Luca, R.; Balletta, T.; Buda, A.; La Rosa, G.; Bramanti, A.; Bramanti, P. The role of virtual reality in improving motor performance as revealed by EEG: A randomized clinical trial. J. Neuroeng. Rehabil. 2017, 14, 53. [Google Scholar] [CrossRef]
- Scandola, M.; Aglioti, S.M.; Lazzeri, G.; Avesani, R.; Ionta, R.; Moro, V. Visuo-motor and interoceptive influences on peripersonal space representation following spinal cord injury. Sci. Rep. 2020, 10, 5162. [Google Scholar] [CrossRef]
- Craig, A.; Guest, R.; Tran, Y.; Middleton, J. Cognitive Impairment and Mood States after Spinal Cord Injury. J. Neurotrauma 2017, 34, 1156–1163. [Google Scholar] [CrossRef]
- Epstein, N.E. Multidisciplinary in-hospital teams improve patient outcomes: A review. Surg. Neurol. Int. 2014, 5, S295–S303. [Google Scholar] [CrossRef] [PubMed]
- Pasipanodya, E.C.; Dirlikov, B.; Castillo, K.; Shem, K.L. Cognitive Profiles among Individuals with Spinal Cord Injuries: Predictors and Relations with Psychological Well-being. Arch. Phys. Med. Rehabil. 2021, 102, 431–439. [Google Scholar] [CrossRef]
- Alcántar-Garibay, O.V.; Incontri-Abraham, D.; Ibarra, A. Spinal cord injury-induced cognitive impairment: A narrative review. Neural Regen. Res. 2022, 17, 2649–2654. [Google Scholar] [CrossRef]
- Huang, X.; Naghdy, F.; Naghdy, G.; Du, H.; Todd, C. Robot-assisted post-stroke motion rehabilitation in upper extremities: A survey. Int. J. Dis. Hum. Develop. 2017, 16, 233–247. [Google Scholar] [CrossRef]
- Noh, D.; Shim, M.-S. Effectiveness of Robot Interventions for Cognitive and Psychological Outcomes among Older Adults with Cognitive Impairment: A Meta-Analysis. Healthcare 2023, 11, 2341. [Google Scholar] [CrossRef]
- Murray, R.F.; Asghari, A.; Egorov, D.D.; Rutkowski, S.B.; Siddall, P.J.; Soden, R.J.; Ruff, R. Impact of spinal cord injury on self-perceived pre- and postmorbid cognitive, emotional and physical functioning. Spinal Cord 2007, 45, 429–436. [Google Scholar] [CrossRef]
- Molina, B.; Segura, A.; Serrano, J.P.; Alonso, F.J.; Molina, L.; Pérez-Borrego, Y.A.; Ugarte, M.I.; Oliviero, A. Cognitive performance of people with traumatic spinal cord injury:a cross-sectional study comparing people with subacute and chronic injuries. Spinal Cord 2018, 56, 796–805. [Google Scholar] [CrossRef]
- Chiaravalloti, N.D.; Weber, E.; Wylie, G.; Dyson-Hudson, T.; Wecht, J.M. Patterns of cognitive deficits in persons with spinal cord injury as compared with both age-matched and older individuals without spinal cord injury. J. Spinal Cord Med. 2020, 43, 88–97. [Google Scholar] [CrossRef]
- Chiaravalloti, N.D.; Weber, E.; Wylie, G.; Dyson-Hudson, T.; Wecht, J.M. The impact of level of injury on patterns of cognitive dysfunction in individuals with spinal cord injury. J. Spinal Cord Med. 2020, 43, 633–641. [Google Scholar] [CrossRef]
- Kennedy, P.; Hasson, L. The relationship between pain and mood following spinal cord injury. J. Spinal Cord Med. 2017, 40, 275–279. [Google Scholar] [CrossRef]
- Pollard, C.; Kennedy, P. A longitudinal analysis of emotional impact, coping strategies and post-traumatic psychological growth following spinal cord injury: A 10-year review. Br. J. Health Psychol. 2007, 12, 347–362. [Google Scholar] [CrossRef]
- Hoffman, J.M.; Bombardier, C.H.; Graves, D.E.; Kalpakjian, C.Z.; Krause, J.S. A longitudinal study of depression from 1 to 5 years after spinal cord injury. Arch. Phys. Med. Rehabil. 2011, 92, 411–418. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Massaro, J.F.; Krause, J.S.; Chen, Y.; Devivo, M.J. Suicide mortality after spinal cord injury in the United States: Injury cohorts analysis. Arch. Phys. Med. Rehabil. 2014, 95, 230–235. [Google Scholar] [CrossRef] [PubMed]
- Zanatta, F.; Farhane-Medina, N.Z.; Adorni, R.; Steca, P.; Giardini, A.; D’addario, M.; Pierobon, A. Combining robot-assisted therapy with virtual reality or using it alone? A systematic review on health-related quality of life in neurological patients. Health Qual. Life Outcomes 2023, 21, 18. [Google Scholar] [CrossRef]
- Šumec, R.; Filip, P.; Sheardová, K.; Bareš, M. Psychological Benefits of Nonpharmacological Methods Aimed for Improving Balance in Parkinson’s Disease: A Systematic Review. Behav. Neurol. 2015, 2015, 620674. [Google Scholar] [CrossRef]
- Verrienti, G.; Raccagni, C.; Lombardozzi, G.; De Bartolo, D.; Iosa, M. Motivation as a Measurable Outcome in Stroke Rehabilitation: A Systematic Review of the Literature. Int. J. Environ. Res. Public Health 2023, 20, 4187. [Google Scholar] [CrossRef] [PubMed]
- Castelli, L.; Iacovelli, C.; Fusco, A.; Amoruso, V.; Cuccagna, C.; Loreti, C.; Giovannini, S.; Padua, L. The Role of Technological Rehabilitation in Patients with Intensive Care Unit Weakness: A Randomized Controlled Pilot Study. J. Clin. Med. 2023, 12, 2612. [Google Scholar] [CrossRef]
- Semprini, M.; Laffranchi, M.; Sanguineti, V.; Avanzino, L.; De Icco, R.; De Michieli, L.; Chiappalone, M. Technological Approaches for Neurorehabilitation: From Robotic Devices to Brain Stimulation and Beyond. Front. Neurol. 2018, 9, 212. [Google Scholar] [CrossRef] [PubMed]
- Engle, R.L.; Mohr, D.C.; Holmes, S.K.; Seibert, M.N.; Afable, M.; Leyson, J.; Meterko, M. Evidence-based practice and patient-centered care: Doing both well. Health Care Manag. Rev. 2021, 46, 174–184. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, J. Neuroplasticity and Clinical Practice: Building Brain Power for Health. Front. Psychol. 2016, 7, 1118. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, A.M. Reward, motivation and brain imaging in human healthy participants- A narrative review. Front. Behav. Neurosci. 2023, 17, 1123733. [Google Scholar] [CrossRef]
- Kvarnström, K.; Westerholm, A.; Airaksinen, M.; Liira, H. Factors Contributing to Medication Adherence in Patients with a Chronic Condition: A Scoping Review of Qualitative Research. Pharmaceutics 2021, 13, 1100. [Google Scholar] [CrossRef] [PubMed]
- Resquín, F.; Cuesta Gómez, A.; Gonzalez-Vargas, J.; Brunetti, F.; Torricelli, D.; Molina Rueda, F.; Cano de la Cuerda, R.; Miangolarra, J.C.; Pons, J.L. Hybrid robotic systems for upper limb rehabilitation after stroke: A review. Med. Eng. Phys. 2016, 38, 1279–1288. [Google Scholar] [CrossRef]
- Pei, Y.C.; Chen, J.L.; Wong, A.M.K.; Tseng, K.C. An Evaluation of the Design and Usability of a Novel Robotic Bilateral Arm Rehabilitation Device for Patients with Stroke. Front. Neurorobot. 2017, 11, 36. [Google Scholar] [CrossRef]
- De Luca, R.; Maggio, M.G.; Maresca, G.; Latella, D.; Cannavò, A.; Sciarrone, F.; Voi, E.L.; Accorinti, M.; Bramanti, P.; Calabrò, R.S. Improving cognitive function after traumatic brain injury: A clinical trial on the potential use of the semi-immersive virtual reality. Behav. Neurol. 2019, 2019, 9268179. [Google Scholar] [CrossRef]
- Maggio, M.G.; Maresca, G.; Russo, M.; Stagnitti, M.C.; Anchesi, S.; Casella, C.; Zichitella, C.; Manuli, A.; De Cola, M.C.; De Luca, R.; et al. Effects of domotics on cognitive, social and personal functioning in patients with chronic stroke: A pilot study. Dis. Health J. 2020, 13, 100838. [Google Scholar] [CrossRef]
- Payedimarri, A.B.; Ratti, M.; Rescinito, R.; Vanhaecht, K.; Panella, M. Effectiveness of Platform-Based Robot-Assisted Rehabilitation for Musculoskeletal or Neurologic Injuries: A Systematic Review. Bioengineering 2022, 9, 129. [Google Scholar] [CrossRef]
- Tarnacka, B.; Korczyński, B.; Frasuńska, J. Impact of Robotic-Assisted Gait Training in Subacute Spinal Cord Injury Patients on Outcome Measure. Diagnostics 2023, 13, 1966. [Google Scholar] [CrossRef] [PubMed]
- Marchal-Crespo, L.; Reinkensmeyer, D.J. Review of control strategies for robotic movement training after neurologic injury. J. NeuroEng. Rehabil. 2009, 6, 20. [Google Scholar] [CrossRef] [PubMed]
- Lapitskaya, N.; Nielsen, J.F.; Fuglsang-Frederiksen, A. Robotic gait training in patients with impaired consciousness due to severe traumatic brain injury. Brain Inj. 2011, 25, 1070–1079. [Google Scholar] [CrossRef] [PubMed]
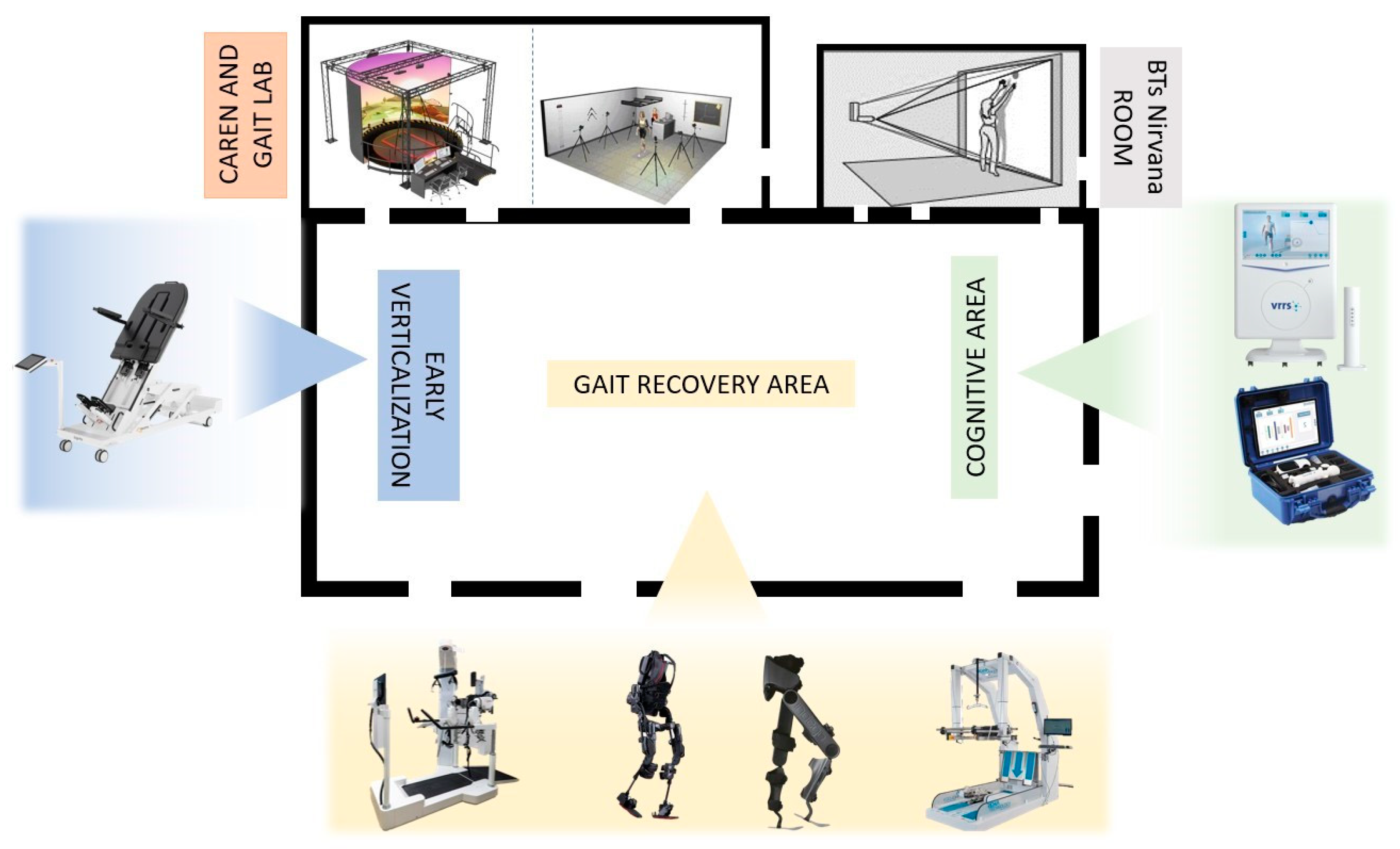
| Type of Intervention | Device/Tool | Outcome | Description |
|---|---|---|---|
| Robotic | Erigo (Hocoma, Volketswil, Switzerland) | Verticalization | Erigo consists of a robotic oscillating table that allows early and progressive robotic verticalization in the acute post-SCI phases and is combined with allowing cyclical leg movement. The tilting table, from 45° to 90°, can be adapted by therapists according to the patient’s needs, and it is also possible to customize the step speed. In addition to verticalization, the device helps to improve the cardiovascular system by activating the muscles and promoting venous return. |
| Lokomat (Hocoma, Volketswil, Switzerland) | Gait training | The Lokomat is a robotic exoskeleton equipped with a treadmill and a weight relief system. It is a tethered exoskeleton with powered orthoses at the hip and knee, passive ankle control during the swing phase, and variable levels of assistance. It can be fitted with a VR screen (Lokomat Pro) to enhance patients’ motivation during training. Additionally, the Free D model allows pelvic movement, simulating physiological human gait. | |
| Ekso-GT/-NR (Ekso Bionics, San Rafael, CA, USA) | Gait training | The Ekso, in contrast, is an untethered exoskeleton designed as a wearable powered orthosis at the hip and knee joints. Patient-initiated walking is facilitated through lateral weight-shifting movements. This untethered design allows flexibility in mobility. The Ekso provides adaptable assistance based on individual patient needs, accommodating unilateral or bilateral support. It is specifically intended for individuals with functional upper extremity strength and spinal cord injury levels T4-L5, as well as C7-T3 (AIS D), making it a versatile solution for diverse rehabilitation scenarios. | |
| Indego (Ekso Bionics, San Rafael, CA, USA) | Gait training | The Indego, a hip–knee exoskeleton, is a dynamic and powered wearable device designed specifically for gait training. Engineered for individuals with spinal cord injuries at C7 and lower levels within rehabilitation facilities, and T3 and lower levels for home and community use, the Indego provides a versatile solution for diverse settings. Activation of walking is initiated by the individual’s intentional center of pressure (COP) movement, either in the anterior direction to commence walking, sit–stand maneuvers, or in the posterior direction to initiate stopping or stand–sit transitions. This sophisticated exoskeleton thus responds to the user’s intentional cues, promoting an intuitive and personalized gait-training experience. | |
| G-EO System (Reha Technology, Olten, Switzerland) | Gait training | Gait training with the G-EO System involves a robotic end effector system that replicates the movements of walking, as well as ascending and descending stairs. The patient’s feet are securely fastened to platforms capable of multidirectional movements, facilitated by six engines aiding in various directions—upwards, downwards, forwards, and backwards. This innovative system offers a comprehensive approach to gait simulation, promoting a dynamic and effective training experience for patients. | |
| Virtual reality | BTs Nirvana (BTS Bioengineering, Milano, Italy) | Motor and cognitive functions | BTS-Nirvana is a semi-immersive virtual reality (VR) system composed of computer software, two markerless optoelectronic infrared sensors, a video camera, and a projector connected to a large screen. Users interact fully with the virtual environment through their movements, effortlessly captured by the infrared sensors. The proposed activities include exercises that require patients to perform specific actions, such as reaching, touching, or grabbing projected objects, as well as interacting with projected images on the floor, such as balls, providing dual-task activities that involve both motor and cognitive aspects. |
| VRRS (Khymeia, Padua, Italy) | Balance, language, and cognitive functions | The Virtual Reality Rehabilitation System (VRRS) is designed around a central hub, connectable via USB, accompanied by a set of specialized peripherals meticulously synchronized and seamlessly integrated with the system. VRRS is outfitted with exercise modules catering to cognitive, language, postural, and motor rehabilitation. Therapists have the capability to select and incorporate virtual exercises into the rehabilitation program, shaping the difficulty level in correlation to the timing of execution and the nature of the activity. This adaptable and comprehensive system allows for tailored rehabilitation programs to meet individual patient needs. | |
| CAREN (Motek, Amsterdam, The Netherlands) | Gait training, balance, and cognitive functions | The Computer Assisted Rehabilitation Environment (CAREN) is comprised of an electro-hydraulic 2 m diameter motion platform, offering manipulation across 6 degrees of freedom. During each session, the patient stands on this dynamic platform, featuring force plates beneath a double-banded treadmill capable of reaching speeds of up to 5 m/s. The platform’s movement is either user-driven or preprogrammed, synchronized with function curves defining specific pathways within the virtual environment. Additionally, the device incorporates a 180° screen, providing varying levels of virtual reality immersion, ranging from flat video and dual-channel audio to a fully enveloping 360-surround sound dome enclosure. | |
| Telerehabilitation | VRRS-HomeKit (Khymeia, Padua, Italy) | Motor functions (lower and upper limbs, balance) and cognitive functions | The Virtual Reality Rehabilitation System (VRRS) HomeKit is a portable device featuring a tablet that facilitates virtual exercises for patients. Interaction occurs with 2D scenarios and objects using the touchscreen or various sensors. For instance, the K-wand is employed for movement tracking and orientation, manipulated by the patient during catching and reaching exercises for upper limbs. Additionally, a pair of K-sensors, comprising sensors on wearable strips of varying sizes, is utilized for conducting full-body motor tele-training activities. |
| Strengths of the Rehabilitation Pathway |
|---|
| 1. Initial Objective Assessment |
| The rehabilitation process begins with an initial objective evaluation, using specific scales to define the patient’s global profile and define a personalized rehabilitation project. |
| 2. In-Depth Gait Analysis |
| After the initial assessment, an in-depth gait analysis is conducted by using the BTS Gaitlab (e.g., optoelectronic system with markers and electromyographic probes) to objectively analyze the patient’s locomotor capabilities (kinetic, kinematic, and electromyographic parameters). |
| 3. Individualized Rehabilitation Plan |
| Based on the assessments, an individualized rehabilitation plan is formulated, aligning with the International Classification of Functioning, Disability, and Health (ICF) model. |
| 4. Multidisciplinary Rehabilitation |
| Rehabilitation integrates conventional treatments with innovative ones aimed at improving motor, emotional, cognitive, speech therapy, occupational, and social outcomes. |
| 5. Integration of Robotics |
| Throughout the hospitalization, the integration of robotics is a pivotal strength, providing innovative interventions tailored to enhance neurorehabilitation and providing repetitive, intensive, and task-oriented training. |
| 6. Virtual Reality Rehabilitation |
| Virtual reality is seamlessly incorporated into the rehabilitation program, offering advanced cognitive rehabilitation and immersive experiences for patients. |
| 7. Pre-Domiciliation Trials with Home Automation |
| Starting a month before discharge, weekly pre-domiciliation trials, including home automation, are introduced to familiarize patients with daily activities. |
| 8. Continuation through Day Hospital and Outpatient Programs |
| The holistic approach extends beyond hospital admission, maintaining rehabilitation through day hospital services and outpatient programs, ensuring continuous and sustained progression toward the patient’s functional recovery. |
| 9. Telerehabilitation |
| Telerehabilitation is implemented as a vital component, facilitating remote interventions to support patients residing far from main hospitals and ensuring continuity of care based on their needs. |
| Patients | |
|---|---|
| Number of patients | 42 |
| Age (years) | 52.21 ± 15.26 |
| Gender | |
| Female | 25 (59.5%) |
| Male | 17 (40.5%) |
| Education | - |
| Elementary school | 1 (2.4%) |
| Middle school | 12 (28.6%) |
| High school | 23 (54.8%) |
| University | 6 (14.2%) |
| Spinal Injury Disability (AIS) | |
| AIS-A patients | 20 (47.6%) |
| AIS-B patients | 22 (52.3%) |
| Time post-injury in months | |
| AIS-A patients | 7 ± 2 |
| AIS-B patients | 7 ± 2 |
| T0 Mean ± SD | T1 Mean ± SD | p-Value | Mean Change (95% Confidence Interval) | |
|---|---|---|---|---|
| MoCA | 22.1 ± 3.3 | 24.6 ± 2.8 | <0.0001 * | 2.5 (1.66, 3.34) |
| BDI | 13.7 ± 7.0 | 9.9 ± 7.1 | <0.0001 * | −3.8 (−5.54, −2.06) |
| SF-12 TOT | 26.1 ± 6.1 | 31.7 ± 8.1 | <0.0001 * | 5.6 (4.15, 7.05) |
| SF-12 MENT | 17.0 ± 5.5 | 20.6 ± 5.8 | <0.0001 * | 3.6 (2.54, 4.66) |
| SF-12 PHY | 12.8 ± 3.7 | 16.9 ± 3.6 | <0.0001 * | 4.1 (1.08, 7.12) |
| FMA | 13.5 ± 3.8 | 19.7 ± 6.0 | <0.0001 * | 6.2 (1.79, 10.61) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maggio, M.G.; Bonanno, M.; Manuli, A.; Calabrò, R.S. Improving Outcomes in People with Spinal Cord Injury: Encouraging Results from a Multidisciplinary Advanced Rehabilitation Pathway. Brain Sci. 2024, 14, 140. https://doi.org/10.3390/brainsci14020140
Maggio MG, Bonanno M, Manuli A, Calabrò RS. Improving Outcomes in People with Spinal Cord Injury: Encouraging Results from a Multidisciplinary Advanced Rehabilitation Pathway. Brain Sciences. 2024; 14(2):140. https://doi.org/10.3390/brainsci14020140
Chicago/Turabian StyleMaggio, Maria Grazia, Mirjam Bonanno, Alfredo Manuli, and Rocco Salvatore Calabrò. 2024. "Improving Outcomes in People with Spinal Cord Injury: Encouraging Results from a Multidisciplinary Advanced Rehabilitation Pathway" Brain Sciences 14, no. 2: 140. https://doi.org/10.3390/brainsci14020140
APA StyleMaggio, M. G., Bonanno, M., Manuli, A., & Calabrò, R. S. (2024). Improving Outcomes in People with Spinal Cord Injury: Encouraging Results from a Multidisciplinary Advanced Rehabilitation Pathway. Brain Sciences, 14(2), 140. https://doi.org/10.3390/brainsci14020140







