The Impact of Revascularization Surgery on Headaches in Association with Cerebrovascular Reactivity in Patients with Moyamoya Angiopathy
Abstract
1. Introduction
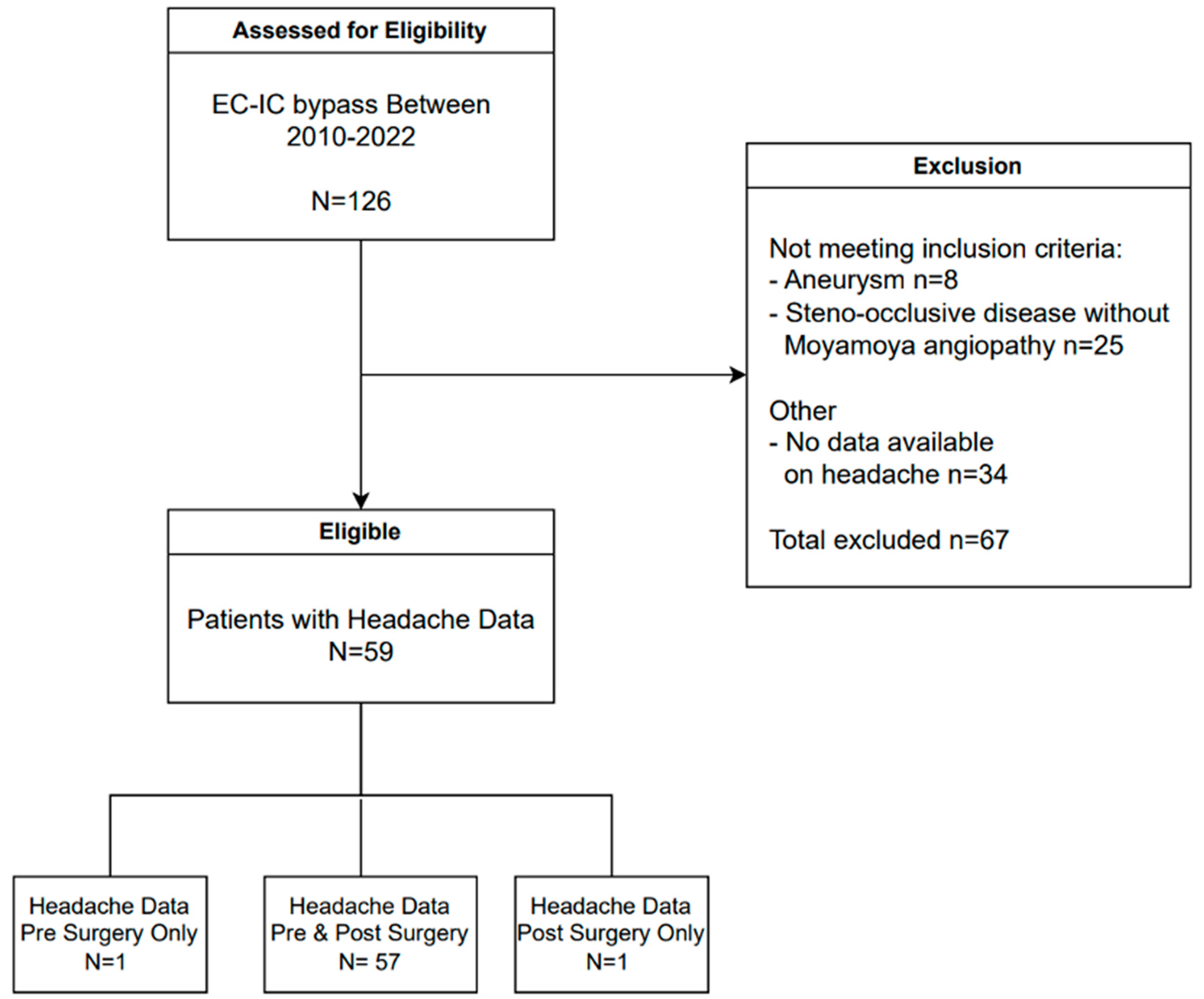
2. Materials and Methods
Statistical Analysis
3. Results
3.1. Headaches before and after Flow Augmentation Surgery
3.2. Cerebrovascular Reserve before and after Flow Augmentation Surgery
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shang, S.; Zhou, D.; Ya, J.; Li, S.; Yang, Q.; Ding, Y.; Ji, X.; Meng, R. Progress in Moyamoya disease. Neurosurg. Rev. 2020, 43, 371–382. [Google Scholar] [CrossRef] [PubMed]
- Scott, R.M.; Smith, E.R. Moyamoya disease and Moyamoya syndrome. N. Engl. J. Med. 2009, 360, 1226–1237. [Google Scholar] [CrossRef] [PubMed]
- Guzman, R.; Lee, M.; Achrol, A.; Bell-Stephens, T.; Kelly, M.; Do, H.M.; Marks, M.P.; Steinberg, G.K. Clinical outcome after 450 revascularization procedures for Moyamoya disease. J. Neurosurg. 2009, 111, 927–935. [Google Scholar] [CrossRef] [PubMed]
- Bersano, A.; Khan, N.; Fuentes, B.; Acerbi, F.; Canavero, I.; Tournier-Lasserve, E.; Vajcoczy, P.; Zedde, M.L.; Hussain, S.; Lémeret, S.; et al. European Stroke Organisation (ESO) Guidelines on Moyamoya angiopathy endorsed by Vascular European Reference Network (VASCERN). Eur. Stroke J. 2023, 8, 55–84. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, N.R.; Amin-Hanjani, S.; Bang, O.Y.; Coffey, C.; Du, R.; Fierstra, J.; Fraser, J.F.; Kuroda, S.; Tietjen, G.E.; Yaghi, S.; et al. Adult Moyamoya disease and Syndrome: Current Perspectives and Future Directions: A Scientific Statement from the American Heart Association/American Stroke Association. Stroke 2023, 54, e465–e479. [Google Scholar] [CrossRef] [PubMed]
- Van Niftrik, C.H.B.; Sebok, M.; Germans, M.R.; Halter, M.; Pokorny, T.; Stumpo, V.; Bellomo, J.; Piccirelli, M.; Pangalu, A.; Katan, M.; et al. Increased risk of recurrent stroke in symptomatic large vessel disease with impaired BOLD cerebrovascular reactivity. Stroke 2024, 55, 613–621. [Google Scholar] [CrossRef] [PubMed]
- Raghavan, V.; Sobczyk, O.; Sayin, E.S.; Poublanc, J.; Skanda, A.; Duffin, J.; Venkatraghavan, L.; Fisher, J.A.; Mikulis, D.J. Assessment of cerebrovascular reactivity using CO2-BOLD MRI: A 15-year, single center experience. J. Magn. Reson. Imaging 2024, 60, 954–961. [Google Scholar] [CrossRef] [PubMed]
- Kraemer, M.; Lee, S.I.; Ayzenberg, I.; Schwitalla, J.C.; Diehl, R.R.; Berlit, P.; Bosche, B.; Katsarava, Z.; Obermann, M. Headache in Caucasian patients with Moyamoya angiopathy—A systematic cohort study. Cephalalgia 2017, 37, 496–500. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.K.; Cho, B.K.; Phi, J.H.; Lee, J.Y.; Chae, J.H.; Kim, K.J.; Hwang, Y.S.; Kim, I.O.; Lee, D.S.; Lee, J.; et al. Pediatric Moyamoya disease: An analysis of 410 consecutive cases. Ann. Neurol. 2010, 68, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Zach, V.; Bezov, D.; Lipton, R.B.; Ashina, S. Headache associated with Moyamoya disease: A case story and literature review. J. Headache Pain. 2010, 11, 79–82. [Google Scholar] [CrossRef] [PubMed]
- Fujimura, M.; Tominaga, T. Diagnosis of Moyamoya disease: International standard and regional differences. Neurol. Med. Chir. 2015, 55, 189–193. [Google Scholar] [CrossRef] [PubMed]
- Amin, F.M.; Ashgar, M.S.; Hougaard, A.; Hansen, A.E.; Larsen, V.A.; de Koning, P.J.; Larsson, H.B.; Olesen, J.; Ashina, M. Magnetic resonance angiography of intracranial and extracranial arteries in patients with spontaneous migraine without aura: A cross-sectional study. Lancet Neurol. 2013, 12, 454–461. [Google Scholar] [CrossRef] [PubMed]
- Gao, B.; Kang, K.; Zhang, J.; Zhang, D.; Zhao, X. Clinical Characteristics and long-term outcome of headaches associated with Moyamoya disease in the Chinese population—A cohort study. Front. Neurol. 2020, 11, 605636. [Google Scholar] [CrossRef] [PubMed]
- Chiang, C.C.; Shahid, A.H.; Harriott, A.M.; Tietjen, G.E.; Savastano, L.E.; Klaas, J.P.; Lanzino, G. Evaluation and treatment of headache associated with Moyamoya disease—A narrative review. Cephalalgia 2022, 42, 542–552. [Google Scholar] [CrossRef] [PubMed]
- Haas, P.; Kittelberger, B.B.; Hurth, H.; Wang, S.; Tellermann, J.; Tatagiba, M.; Khan, N.; Roder, C. Health-related quality of life and neuropsychological outcome after EC-IC bypass revascularization in adult patients with Moyamoya disease. Neurosurgery 2024, 94, 1107–1115. [Google Scholar] [CrossRef] [PubMed]
- Kawabori, M.; Kuroda, S.; Nakayama, N.; Hirata, K.; Shiga, T.; Houkin, K.; Tamaki, N. Effective surgical revascularization improves cerebral hemodynamics and resolves headache in pediatric Moyamoya disease. World Neurosurg. 2013, 80, 612–619. [Google Scholar] [CrossRef] [PubMed]
- Bohara, M.; Sugata, S.; Nishimuta, Y.; Karki, P.; Nagayama, T.; Sakamoto, S.; Tokimura, H.; Arita, K. Effect of revascularization on headache associated with Moyamoya disease in pediatric patients. Hiroshima J. Med. Sci. 2015, 64, 39–44. [Google Scholar] [PubMed]
| n = 59 | |
|---|---|
| Age (yr) | 47 ± 14 |
| Female sex | 43/59 (73%) |
| Moyamoya disease | 41/59 (70%) |
| Unilateral | 11/41 (27%) |
| Bilateral | 30/41 (73%) |
| Moyamoya syndrome | 18/59 (31%) |
| Unilateral | 10/18 (56%) |
| Bilateral | 8/18 (44%) |
| History of stroke | |
| Only ischemic | 35/59 (59%) |
| Only hemorrhagic | 6/59 (10%) |
| Ischemic and hemorrhagic | 9/59 (15%) |
| No history of stroke | 9/59 (15%) |
| Bypass surgery n (%) | |
| EC–IC bypass left | 22/59 (37%) |
| EC–IC bypass right | 18/59 (31%) |
| EC–IC bypass bilateral | 19/59 (32%) |
| EC–IC bypass + EDAS | 4/59 (7%) |
| Interval CVR-MRI & bypass surgery (median (IQR), months) | 5 (3–8) |
| Interval bypass surgery & CVR-MRI (median (IQR), months) | 6 (3–12) |
| n (%) | |
|---|---|
| Headaches before surgery | 41/57 (72%) |
| Headaches improved after surgery | 28/41 (68%) |
| Headaches were unchanged after surgery | 11/41 (27%) |
| Headaches worsened after surgery | 2/41 (5%) |
| New onset headaches after surgery | 2/57 (4%) |
| Before Surgery n (%) | After Surgery n (%) | |
|---|---|---|
| Completed questionnaires | 31/59 (53%) | 31/59 (53%) |
| Presence of headaches | 25/31 (81%) | 19/31 (61%) |
| Types of Headaches | ||
| Throbbing headache | 9/25 (36%) | 6/19 (32%) |
| Pressure-type headache | 7/25 (28%) | 6/19 (32%) |
| Dull headache | 6/25 (24%) | 6/19 (32%) |
| Sharp headache | 4/25 (16%) | 2/19 (11%) |
| Localization of Headaches | ||
| Bilateral | 19/25 (76%) | 14/19 (74%) |
| Unilateral | 6/25 (24%) | 5/19 (26%) |
| Headache Triggers | ||
| Lack of sleep | 6/25 (24%) | 5/19 (26%) |
| Menses | 4/25 (16%) | 4/19 (21%) |
| Exercise | 3/25 (12%) | 1/19 (5%) |
| Mental stress | 3/25 (12%) | 2/19 (11%) |
| Weather changes | 1/25 (4%) | 1/19 (5%) |
| Accompanying Symptoms | ||
| Preceding aura | 6/25 (24%) | 6/19 (32%) |
| Nausea/vomiting | 9/25 (36%) | 9/19 (47%) |
| Photo-/phonophobia | 4/25 (16%) | 3/19 (16%) |
| Dizziness | 4/25 (16%) | 2/19 (11%) |
| Transient focal weakness/sensory symptoms | 2/25 (8%) | 0/19 (0%) |
| Analgesic Use | 21/25 (84%) | 10/25 (40%) * |
| Acetaminophen | 16/25 (64%) | 5/25 (20%) |
| Non-steroidal anti-inflammatory drugs | 5/25 (20%) | 2/25 (8%) |
| Triptans | 3/25 (12%) | 1/25 (4%) |
| Anticonvulsants | 5/25 (20%) | 2/25 (8%) |
| Opioids (codeine, caffeine, morphine) | 3/25 (12%) | 3/25 (12%) |
| Multiple drug classes | 7/25 (28%) | 3/25 (12%) |
| Headache impact | ||
| Pain severity: VAS-score (median (IQR)) | 5 (0–9) | 2.5 (0–5) * |
| Feelings of depression | 11/25 (44%) | 8/25 (32%) |
| Sick leave/quit job | 15/25 (60%) | 4/25 (16%) * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gallego Moyano, F.D.; Janssen, H.C.; Venkatraghavan, L.; Mikulis, D.J.; Andrade Barazarte, H.; Radovanovic, I.; Hendriks, E.J.; Schaafsma, J.D. The Impact of Revascularization Surgery on Headaches in Association with Cerebrovascular Reactivity in Patients with Moyamoya Angiopathy. Brain Sci. 2024, 14, 967. https://doi.org/10.3390/brainsci14100967
Gallego Moyano FD, Janssen HC, Venkatraghavan L, Mikulis DJ, Andrade Barazarte H, Radovanovic I, Hendriks EJ, Schaafsma JD. The Impact of Revascularization Surgery on Headaches in Association with Cerebrovascular Reactivity in Patients with Moyamoya Angiopathy. Brain Sciences. 2024; 14(10):967. https://doi.org/10.3390/brainsci14100967
Chicago/Turabian StyleGallego Moyano, Francy D., Helena C. Janssen, Lashmi Venkatraghavan, David J. Mikulis, Hugo Andrade Barazarte, Ivan Radovanovic, Eef J. Hendriks, and Joanna D. Schaafsma. 2024. "The Impact of Revascularization Surgery on Headaches in Association with Cerebrovascular Reactivity in Patients with Moyamoya Angiopathy" Brain Sciences 14, no. 10: 967. https://doi.org/10.3390/brainsci14100967
APA StyleGallego Moyano, F. D., Janssen, H. C., Venkatraghavan, L., Mikulis, D. J., Andrade Barazarte, H., Radovanovic, I., Hendriks, E. J., & Schaafsma, J. D. (2024). The Impact of Revascularization Surgery on Headaches in Association with Cerebrovascular Reactivity in Patients with Moyamoya Angiopathy. Brain Sciences, 14(10), 967. https://doi.org/10.3390/brainsci14100967





