Mortality Prediction of Patients with Subarachnoid Hemorrhage Using a Deep Learning Model Based on an Initial Brain CT Scan
Abstract
:1. Introduction
2. Materials and Methods
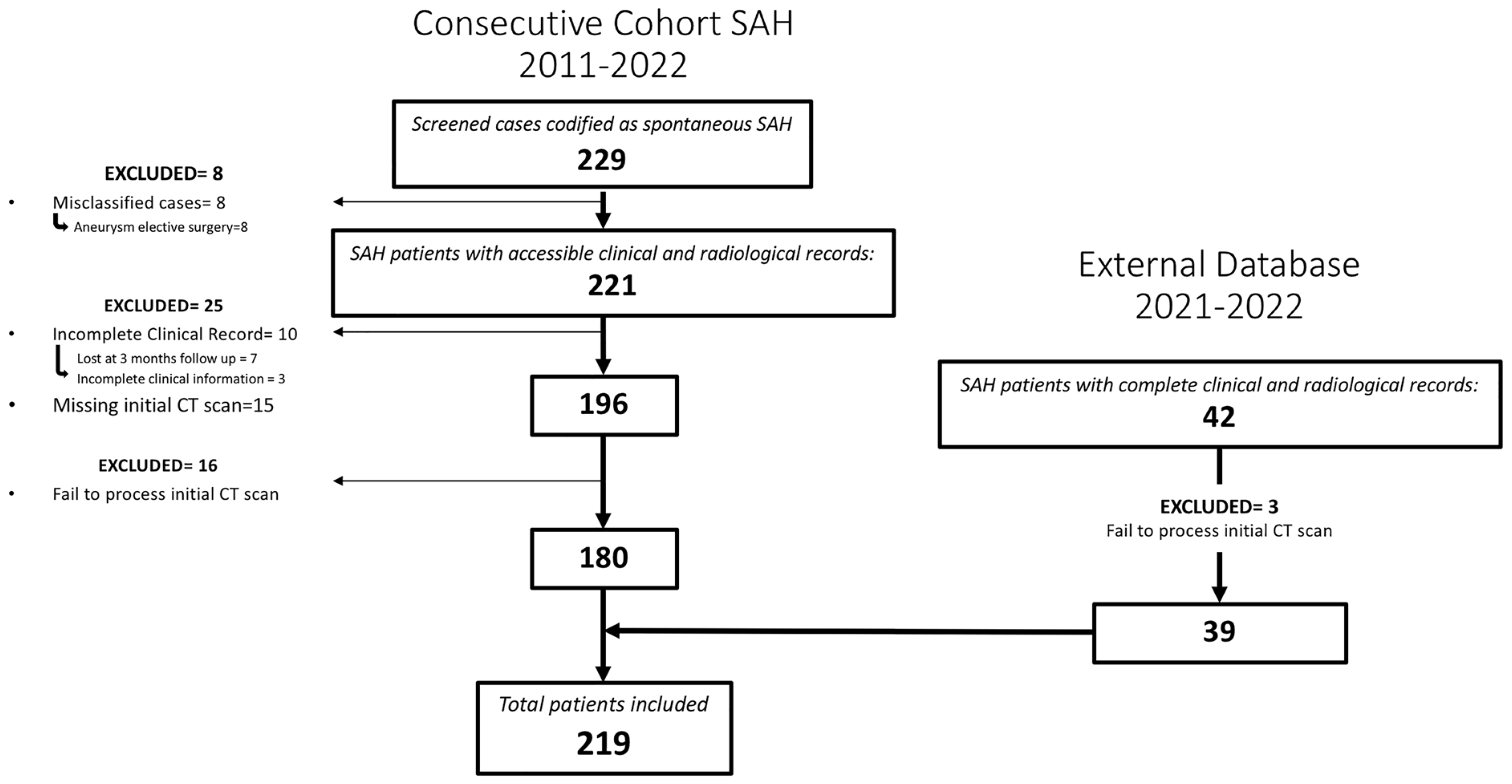
2.1. Study Population
2.2. Variables
2.3. Image Acquisition
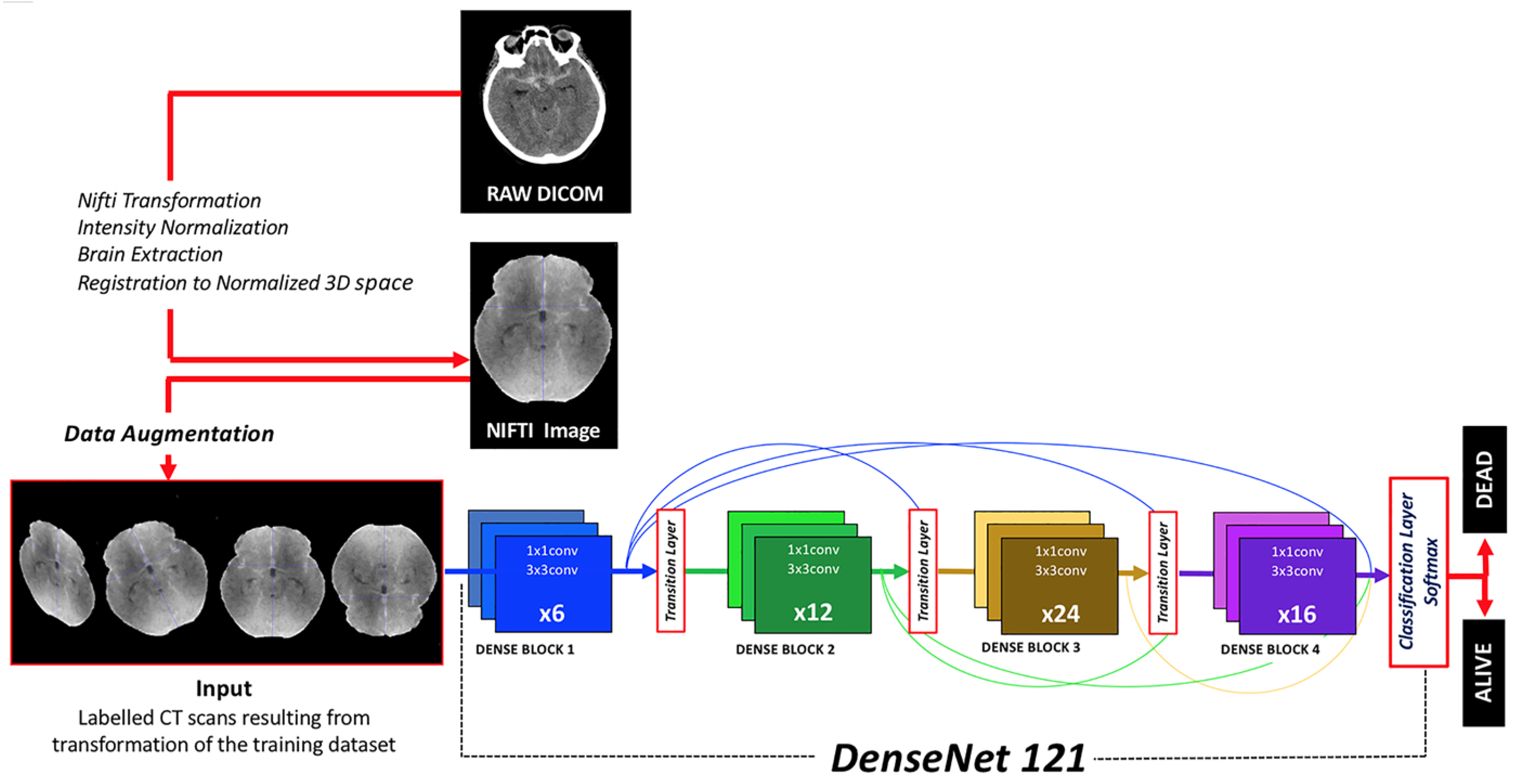
2.4. Image Preprocessing
2.5. Neural Network
2.6. Architecture
2.7. Activation Output
2.8. Class Imbalance and Loss Function
2.9. Data Augmentation
2.10. Callbacks
2.11. Transfer Learning
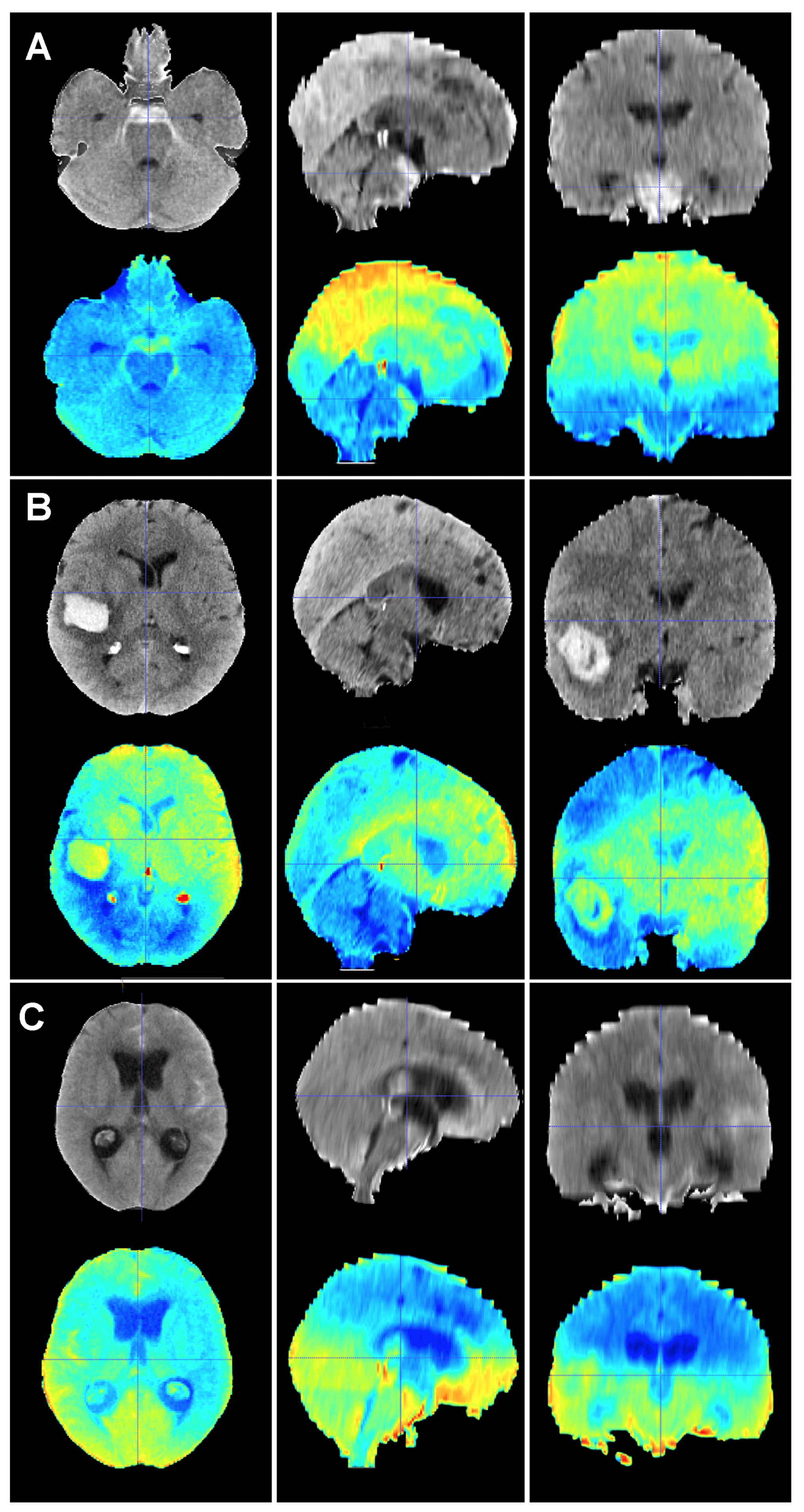
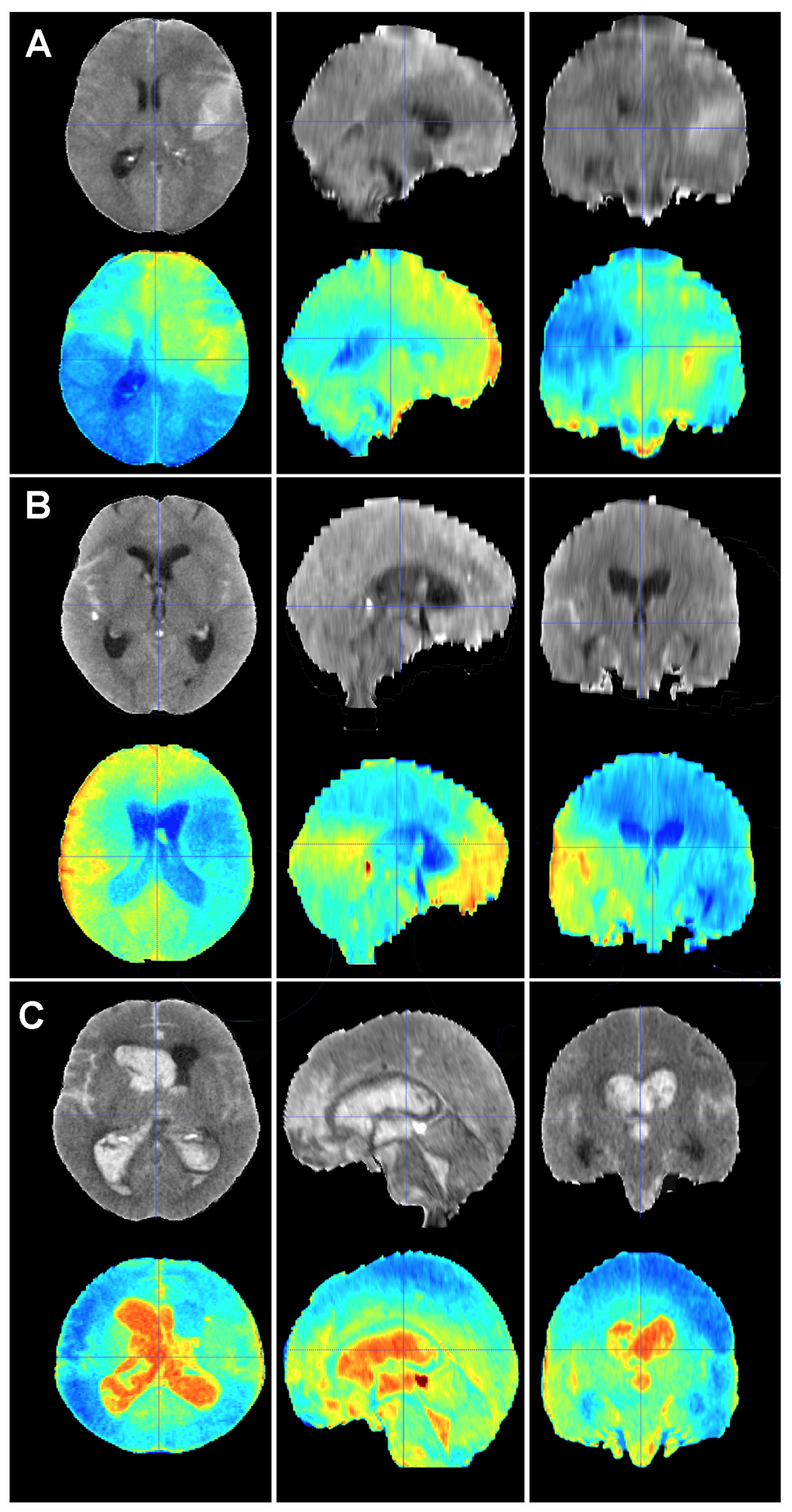
2.12. Explainable Artificial Intelligence
2.13. Metadata
2.14. Statistics
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Linn, F.H.; Rinkel, G.J.; Algra, A.; van Gijn, J. Incidence of subarachnoid hemorrhage: Role of region, year, and rate of computed tomography: A meta-analysis. Stroke 1996, 27, 625–629. [Google Scholar] [CrossRef] [PubMed]
- Mensing, L.A.; Vergouwen, M.D.I.; Laban, K.G.; Ruigrok, Y.M.; Velthuis, B.K.; Algra, A.; Rinkel, G.J.E. Perimesencephalic Hemorrhage: A Review of Epidemiology, Risk Factors, Presumed Cause, Clinical Course, and Outcome. Stroke 2018, 49, 1363–1370. [Google Scholar] [CrossRef] [PubMed]
- GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021, 20, 795–820. [Google Scholar] [CrossRef] [PubMed]
- Stienen, M.N.; Germans, M.; Burkhardt, J.K.; Neidert, M.C.; Fung, C.; Bervini, D.; Zumofen, D.; Rothlisberger, M.; Marbacher, S.; Maduri, R.; et al. Predictors of In-Hospital Death After Aneurysmal Subarachnoid Hemorrhage: Analysis of a Nationwide Database (Swiss SOS [Swiss Study on Aneurysmal Subarachnoid Hemorrhage]). Stroke 2018, 49, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Nieuwkamp, D.J.; Setz, L.E.; Algra, A.; Linn, F.H.; de Rooij, N.K.; Rinkel, G.J. Changes in case fatality of aneurysmal subarachnoid haemorrhage over time, according to age, sex, and region: A meta-analysis. Lancet Neurol. 2009, 8, 635–642. [Google Scholar] [CrossRef] [PubMed]
- Lovelock, C.E.; Rinkel, G.J.; Rothwell, P.M. Time trends in outcome of subarachnoid hemorrhage: Population-based study and systematic review. Neurology 2010, 74, 1494–1501. [Google Scholar] [CrossRef] [PubMed]
- Mayfrank, L.; Hutter, B.O.; Kohorst, Y.; Kreitschmann-Andermahr, I.; Rohde, V.; Thron, A.; Gilsbach, J.M. Influence of intraventricular hemorrhage on outcome after rupture of intracranial aneurysm. Neurosurg. Rev. 2001, 24, 185–191. [Google Scholar] [CrossRef]
- Catapano, J.S.; Labib, M.A.; Srinivasan, V.M.; Nguyen, C.L.; Rumalla, K.; Rahmani, R.; Cole, T.S.; Baranoski, J.F.; Rutledge, C.; Chapple, K.M.; et al. Saccular aneurysms in the post-Barrow Ruptured Aneurysm Trial era. J. Neurosurg. 2021, 137, 148–155. [Google Scholar] [CrossRef]
- Spetzler, R.F.; McDougall, C.G.; Zabramski, J.M.; Albuquerque, F.C.; Hills, N.K.; Russin, J.J.; Partovi, S.; Nakaji, P.; Wallace, R.C. The Barrow Ruptured Aneurysm Trial: 6-year results. J. Neurosurg. 2015, 123, 609–617. [Google Scholar] [CrossRef]
- Molyneux, A.; Kerr, R.; Stratton, I.; Sandercock, P.; Clarke, M.; Shrimpton, J.; Holman, R.; International Subarachnoid Aneurysm Trial Collaborative Group. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: A randomised trial. Lancet 2002, 360, 1267–1274. [Google Scholar] [CrossRef]
- Ngiam, K.Y.; Khor, I.W. Big data and machine learning algorithms for health-care delivery. Lancet Oncol. 2019, 20, e262–e273. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Garcia, S.; Garcia-Galindo, M.; Arrese, I.; Sarabia, R.; Cepeda, S. Current Evidence, Limitations and Future Challenges of Survival Prediction for Glioblastoma Based on Advanced Noninvasive Methods: A Narrative Review. Medicina 2022, 58, 1746. [Google Scholar] [CrossRef] [PubMed]
- Helbok, R.; Kurtz, P.; Vibbert, M.; Schmidt, M.J.; Fernandez, L.; Lantigua, H.; Ostapkovich, N.D.; Connolly, S.E.; Lee, K.; Claassen, J.; et al. Early neurological deterioration after subarachnoid haemorrhage: Risk factors and impact on outcome. J. Neurol. Neurosurg. Psychiatry 2013, 84, 266–270. [Google Scholar] [CrossRef] [PubMed]
- Lagares, A.; Jimenez-Roldan, L.; Gomez, P.A.; Munarriz, P.M.; Castano-Leon, A.M.; Cepeda, S.; Alen, J.F. Prognostic Value of the Amount of Bleeding After Aneurysmal Subarachnoid Hemorrhage: A Quantitative Volumetric Study. Neurosurgery 2015, 77, 898–907; discussion 907. [Google Scholar] [CrossRef] [PubMed]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gotzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M.; Initiative, S. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Epidemiology 2007, 18, 805–835. [Google Scholar] [CrossRef] [PubMed]
- Mongan, J.; Moy, L.; Kahn, C.E., Jr. Checklist for Artificial Intelligence in Medical Imaging (CLAIM): A Guide for Authors and Reviewers. Radiol. Artif. Intell. 2020, 2, e200029. [Google Scholar] [CrossRef]
- Frontera, J.A.; Claassen, J.; Schmidt, J.M.; Wartenberg, K.E.; Temes, R.; Connolly, E.S., Jr.; MacDonald, R.L.; Mayer, S.A. Prediction of symptomatic vasospasm after subarachnoid hemorrhage: The modified fisher scale. Neurosurgery 2006, 59, 21–27; discussion 21–27. [Google Scholar] [CrossRef]
- Teasdale, G.M.; Drake, C.G.; Hunt, W.; Kassell, N.; Sano, K.; Pertuiset, B.; De Villiers, J.C. A universal subarachnoid hemorrhage scale: Report of a committee of the World Federation of Neurosurgical Societies. J. Neurol. Neurosurg. Psychiatry 1988, 51, 1457. [Google Scholar] [CrossRef]
- Hunt, W.E.; Hess, R.M. Surgical risk as related to time of intervention in the repair of intracranial aneurysms. J. Neurosurg. 1968, 28, 14–20. [Google Scholar] [CrossRef]
- Müller, D.; Hartmann, D.; Soto-Rey, I.; Kramer, F. (Eds.) Abstract: AUCMEDI2023; Springer Fachmedien Wiesbaden: Wiesbaden, Germany, 2023. [Google Scholar]
- Huang, G.; Liu, Z.; Pleiss, G.; Maaten, L.V.; Weinberger, K.Q. Convolutional Networks with Dense Connectivity. IEEE Trans. Pattern Anal. Mach. Intell. 2022, 44, 8704–8716. [Google Scholar] [CrossRef]
- King, G.; Zeng, L. Logistic Regression in Rare Events Data. Political Anal. 2001, 9, 137–163. [Google Scholar] [CrossRef]
- Yeung, M.; Sala, E.; Schonlieb, C.B.; Rundo, L. Unified Focal loss: Generalising Dice and cross entropy-based losses to handle class imbalanced medical image segmentation. Comput. Med. Imaging Graph. 2022, 95, 102026. [Google Scholar] [CrossRef] [PubMed]
- Isensee, F.; Jaeger, P.F.; Kohl, S.A.A.; Petersen, J.; Maier-Hein, K.H. nnU-Net: A self-configuring method for deep learning-based biomedical image segmentation. Nat. Methods 2021, 18, 203–211. [Google Scholar] [CrossRef]
- Selvaraju, R.R.; Cogswell, M.; Das, A.; Vedantam, R.; Parikh, D.; Batra, D. Grad-CAM: Visual Explanations from Deep Networks via Gradient-Based Localization. Int. J. Comput. Vis. 2020, 128, 23. [Google Scholar] [CrossRef]
- Muller, D.; Soto-Rey, I.; Kramer, F. Towards a guideline for evaluation metrics in medical image segmentation. BMC Res. Notes 2022, 15, 210. [Google Scholar] [CrossRef] [PubMed]
- Chilamkurthy, S.; Ghosh, R.; Tanamala, S.; Biviji, M.; Campeau, N.G.; Venugopal, V.K.; Mahajan, V.; Rao, P.; Warier, P. Deep learning algorithms for detection of critical findings in head CT scans: A retrospective study. Lancet 2018, 392, 2388–2396. [Google Scholar] [CrossRef] [PubMed]
- Heit, J.J.; Coelho, H.; Lima, F.O.; Granja, M.; Aghaebrahim, A.; Hanel, R.; Kwok, K.; Haerian, H.; Cereda, C.W.; Venkatasubramanian, C.; et al. Automated Cerebral Hemorrhage Detection Using RAPID. AJNR Am. J. Neuroradiol. 2021, 42, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Mansour, R.F.; Aljehane, N.O. An optimal segmentation with deep learning based inception network model for intracranial hemorrhage diagnosis. Neural Comput. Appl. 2021, 33, 12. [Google Scholar] [CrossRef]
- Thanellas, A.; Peura, H.; Lavinto, M.; Ruokola, T.; Vieli, M.; Staartjes, V.E.; Winklhofer, S.; Serra, C.; Regli, L.; Korja, M. Development and External Validation of a Deep Learning Algorithm to Identify and Localize Subarachnoid Hemorrhage on CT Scans. Neurology 2023, 100, e1257–e1266. [Google Scholar] [CrossRef]
- Rajagopal, M.; Buradagunta, S.; Almeshari, M.; Alzamil, Y.; Ramalingam, R.; Ravi, V. An Efficient Framework to Detect Intracranial Hemorrhage Using Hybrid Deep Neural Networks. Brain Sci. 2023, 13, 400. [Google Scholar] [CrossRef]
- Din, M.; Agarwal, S.; Grzeda, M.; Wood, D.A.; Modat, M.; Booth, T.C. Detection of cerebral aneurysms using artificial intelligence: A systematic review and meta-analysis. J. Neurointerv. Surg. 2023, 15, 262–271. [Google Scholar] [CrossRef] [PubMed]
- Bo, Z.H.; Qiao, H.; Tian, C.; Guo, Y.; Li, W.; Liang, T.; Li, D.; Liao, D.; Zeng, X.; Mei, L.; et al. Toward human intervention-free clinical diagnosis of intracranial aneurysm via deep neural network. Patterns 2021, 2, 100197. [Google Scholar] [CrossRef] [PubMed]
- de Winkel, J.; Cras, T.Y.; Dammers, R.; van Doormaal, P.J.; van der Jagt, M.; Dippel, D.W.J.; Lingsma, H.F.; Roozenbeek, B. Early predictors of functional outcome in poor-grade aneurysmal subarachnoid hemorrhage: A systematic review and meta-analysis. BMC Neurol. 2022, 22, 239. [Google Scholar] [CrossRef] [PubMed]
- Dengler, N.F.; Madai, V.I.; Unteroberdorster, M.; Zihni, E.; Brune, S.C.; Hilbert, A.; Livne, M.; Wolf, S.; Vajkoczy, P.; Frey, D. Outcome prediction in aneurysmal subarachnoid hemorrhage: A comparison of machine learning methods and established clinico-radiological scores. Neurosurg. Rev. 2021, 44, 2837–2846. [Google Scholar] [CrossRef] [PubMed]
- De Toledo, P.; Rios, P.M.; Ledezma, A.; Sanchis, A.; Alen, J.F.; Lagares, A. Predicting the outcome of patients with subarachnoid hemorrhage using machine learning techniques. IEEE Trans. Inf. Technol. Biomed. 2009, 13, 794–801. [Google Scholar] [CrossRef] [PubMed]
- Lo, B.W.; Macdonald, R.L.; Baker, A.; Levine, M.A. Clinical outcome prediction in aneurysmal subarachnoid hemorrhage using Bayesian neural networks with fuzzy logic inferences. Comput. Math. Methods Med. 2013, 2013, 904860. [Google Scholar] [CrossRef] [PubMed]
- Lissak, I.A.; Edlow, B.L.; Rosenthal, E.; Young, M.J. Ethical Considerations in Neuroprognostication Following Acute Brain Injury. Semin. Neurol. 2023, 43, 758–767. [Google Scholar] [CrossRef] [PubMed]
- Pinto, A.; McKinley, R.; Alves, V.; Wiest, R.; Silva, C.A.; Reyes, M. Stroke Lesion Outcome Prediction Based on MRI Imaging Combined with Clinical Information. Front. Neurol. 2018, 9, 1060. [Google Scholar] [CrossRef]
- Ningrum, D.N.A.; Yuan, S.P.; Kung, W.M.; Wu, C.C.; Tzeng, I.S.; Huang, C.Y.; Li, J.Y.; Wang, Y.C. Deep Learning Classifier with Patient’s Metadata of Dermoscopic Images in Malignant Melanoma Detection. J. Multidiscip. Healthc. 2021, 14, 877–885. [Google Scholar] [CrossRef]
- Mitani, A.; Huang, A.; Venugopalan, S.; Corrado, G.S.; Peng, L.; Webster, D.R.; Hammel, N.; Liu, Y.; Varadarajan, A.V. Detection of anaemia from retinal fundus images via deep learning. Nat. Biomed. Eng. 2020, 4, 18–27. [Google Scholar] [CrossRef]
- Van der Velden, B.H.M.; Kuijf, H.J.; Gilhuijs, K.G.A.; Viergever, M.A. Explainable artificial intelligence (XAI) in deep learning-based medical image analysis. Med. Image Anal. 2022, 79, 102470. [Google Scholar] [CrossRef] [PubMed]
- Windisch, P.; Weber, P.; Furweger, C.; Ehret, F.; Kufeld, M.; Zwahlen, D.; Muacevic, A. Implementation of model explainability for a basic brain tumor detection using convolutional neural networks on MRI slices. Neuroradiology 2020, 62, 1515–1518. [Google Scholar] [CrossRef] [PubMed]


| Variable | Mean/Mode | Number | Percentage |
|---|---|---|---|
| Female | 115 | 52.5% | |
| Age | 57.9 (SD = 13.06) years | ||
| RISK FACTORS | |||
| HT | 96 | 43.8% | |
| Tobacco | 90 | 41% | |
| Smoker, Female | 40 | 34.8% of females | |
| HT + Tobacco | 36 | 16.5% of total | |
| Diabetes | 20 | 9% | |
| Dyslipidemia | 81 | 37% | |
| Familial History | 3 | 1.5% | |
| Idiopathic SAH | 39 | 18% | |
| Aneurysmal SAH | 180 | 82% | |
| Multiple | 36 | 20% | |
| Anterior Circulation | 174 | 97% | |
| Aneurysm Diameter | 7.9 mm (SD = 5.6) | ||
| TREATMENT | |||
| Surgical | 91 | 50.5% | |
| Endovascular | 72 | 40% | |
| No Treatment | 17 | 9% | |
| Timing of Treatment | |||
| Ultra Early (<24 h) | 114 | 70% | |
| Early (24–72 h) | 33 | 20% | |
| Delayed (>72 h) | 16 | 10% | |
| ADMISSION | |||
| Hunt and Hess | 2.2/2 | ||
| I | 103 | 47% | |
| II | 45 | 20.5% | |
| III | 10 | 4.5% | |
| IV | 17 | 8% | |
| V | 44 | 20% | |
| WFNS | 2.5/2 | ||
| I | 93 | 42.5% | |
| II | 46 | 21% | |
| III | 8 | 3.5% | |
| IV | 26 | 12% | |
| V | 46 | 21% | |
| Modified Fisher | 3.2/4 | ||
| I | 15 | 7% | |
| II | 25 | 11.5% | |
| III | 35 | 16% | |
| IV | 144 | 65.5% | |
| Intraparenchymal Hematoma | 63 | 35% | |
| Subdural Hematoma | 9 | 5% | |
| COMPLICATIONS | |||
| Acute Hydrocephalus | 96 | 44% | |
| Shunt-Dependent Hydrocephalus | 38 | 17.5% | |
| Seizure | 37 | 17% | |
| Epilepsy | 12 | 6.5% | |
| Symptomatic Vasospasm | 38 | 17.5% | |
| Delayed Cerebral Ischemia | 52 | 23.5% | |
| Length of Stay | 24 days | ||
| OUTCOME | |||
| mRS at 3 Months | 3/6 | ||
| 0 | 46 | 21% | |
| 1 | 37 | 17% | |
| 2 | 16 | 7.5% | |
| 3 | 19 | 8.5% | |
| 4 | 15 | 7% | |
| 5 | 23 | 10.5% | |
| 6 | 63 | 28.5% | |
| Mortality | 63 | 28.5% | |
| Variable | Reference | Degrees of Freedom | p-Value | OR | 95% CI |
|---|---|---|---|---|---|
| Sex (Male) | Male | 1 | 0.042 | 0.54 | 0.30–0.98 |
| Age | 1 | 0.014 | 1.03 | 1.01–1.05 | |
| Hypertension | Yes | 1 | 0.002 | 2.55 | 1.41–4.63 |
| Intraparenchimatous Hematoma | Yes | 1 | <0.001 | 3.34 | 1.79–6.22 |
| Acute Hydrocephalus | Yes | 1 | <0.001 | 3.01 | 1.64–5.55 |
| WFNS | 1 | 4 | <0.001 | ||
| WFNS 2 | 0.007 | 3.67 | 1.44–9.42 | ||
| WFNS 3 | 0.033 | 5.60 | 1.14–27.40 | ||
| WFNS 4 | 0.001 | 5.83 | 2.05–16.62 | ||
| WFNS 5 | <0.001 | 17.50 | 6.99–43.77 | ||
| Hunt and Hess | 1 | 4 | <0.001 | ||
| HH 2 | 0.002 | 4.51 | 1.72–11.86 | ||
| HH 3 | 0.047 | 5.00 | 1.02–24.51 | ||
| HH 4 | 0.02 | 4.63 | 1.27–16.87 | ||
| HH 5 | <0.001 | 25.00 | 8.99–69.56 | ||
| Modified Fisher, Dichotomized | <2 | 1 | <0.001 | ||
| mF > 2 | 0.003 | 21.70 | 2.91–161.72 |
| Model | Image-Based Neural Network Performance | IMAGE- and Metadata-Based Neural Network Performance | ||||||
|---|---|---|---|---|---|---|---|---|
| Epoch | Best AUC | Best F1 | Best Loss | Last | Best AUC | Best F1 | Best Loss | Last |
| Metric | ||||||||
| TP | 14.5 | 15 | 15 | 16 | 16 | 16.5 | 15.5 | 15 |
| TN | 14.5 | 15 | 15 | 16 | 16 | 16.5 | 15.5 | 15 |
| FP | 7 | 6.5 | 6.5 | 5.5 | 5.5 | 5 | 6 | 6.5 |
| FN | 7 | 6.5 | 6.5 | 5.5 | 5.5 | 5 | 6 | 6.5 |
| Sensitivity | 0.53 | 0.61 | 0.74 | 0.75 | 0.60 | 0.75 | 0.69 | 0.50 |
| Specificity | 0.53 | 0.61 | 0.74 | 0.75 | 0.60 | 0.75 | 0.69 | 0.50 |
| Precision | 0.56 | 0.63 | 0.70 | 0.72 | 0.75 | 0.73 | 0.68 | 0.35 |
| FP Rate | 0.47 | 0.39 | 0.26 | 0.25 | 0.40 | 0.25 | 0.31 | 0.50 |
| FN Rate | 0.47 | 0.39 | 0.26 | 0.25 | 0.40 | 0.25 | 0.31 | 0.50 |
| FDR | 0.44 | 0.37 | 0.30 | 0.28 | 0.25 | 0.27 | 0.32 | 0.15 |
| Accuracy | 0.67 | 0.70 | 0.70 | 0.74 | 0.74 | 0.77 | 0.72 | 0.70 |
| F1 | 0.51 | 0.61 | 0.69 | 0.72 | 0.60 | 0.74 | 0.68 | 0.41 |
| AUC | 0.72 | 0.74 | 0.73 | 0.82 | 0.78 | 0.80 | 0.78 | 0.35 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-García, S.; Cepeda, S.; Müller, D.; Mosteiro, A.; Torné, R.; Agudo, S.; de la Torre, N.; Arrese, I.; Sarabia, R. Mortality Prediction of Patients with Subarachnoid Hemorrhage Using a Deep Learning Model Based on an Initial Brain CT Scan. Brain Sci. 2024, 14, 10. https://doi.org/10.3390/brainsci14010010
García-García S, Cepeda S, Müller D, Mosteiro A, Torné R, Agudo S, de la Torre N, Arrese I, Sarabia R. Mortality Prediction of Patients with Subarachnoid Hemorrhage Using a Deep Learning Model Based on an Initial Brain CT Scan. Brain Sciences. 2024; 14(1):10. https://doi.org/10.3390/brainsci14010010
Chicago/Turabian StyleGarcía-García, Sergio, Santiago Cepeda, Dominik Müller, Alejandra Mosteiro, Ramón Torné, Silvia Agudo, Natalia de la Torre, Ignacio Arrese, and Rosario Sarabia. 2024. "Mortality Prediction of Patients with Subarachnoid Hemorrhage Using a Deep Learning Model Based on an Initial Brain CT Scan" Brain Sciences 14, no. 1: 10. https://doi.org/10.3390/brainsci14010010
APA StyleGarcía-García, S., Cepeda, S., Müller, D., Mosteiro, A., Torné, R., Agudo, S., de la Torre, N., Arrese, I., & Sarabia, R. (2024). Mortality Prediction of Patients with Subarachnoid Hemorrhage Using a Deep Learning Model Based on an Initial Brain CT Scan. Brain Sciences, 14(1), 10. https://doi.org/10.3390/brainsci14010010







