Investigating the Role of Second Chance Schools and COVID-19 Pandemic on the Mental Health and Self-Image of Greek Adult Students
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics
- The Ethics Committee of the Democritus University of Thrace (relevant document with protocol number 18,658/89 issued on 14 November 2019);
- The competent administrative body of the SCS in Greece, which is the Department of Adult Education Program and Organization Studies, which is under the Ministry of Education and Religious Affairs of the Hellenic Republic (relevant document with protocol number K1/20,484 issued on 12 February 2020).
2.2. Sample
2.3. Instruments
2.3.1. Demographics
2.3.2. Anxiety
2.3.3. Depression
2.3.4. Well-Being
2.3.5. Self-Esteem
2.3.6. Self-Efficacy
2.4. Data Collection
2.5. Statistical Analysis
3. Results
3.1. Descriptive Analysis of the Sample
3.2. Measuring the Reliability of Research Tools
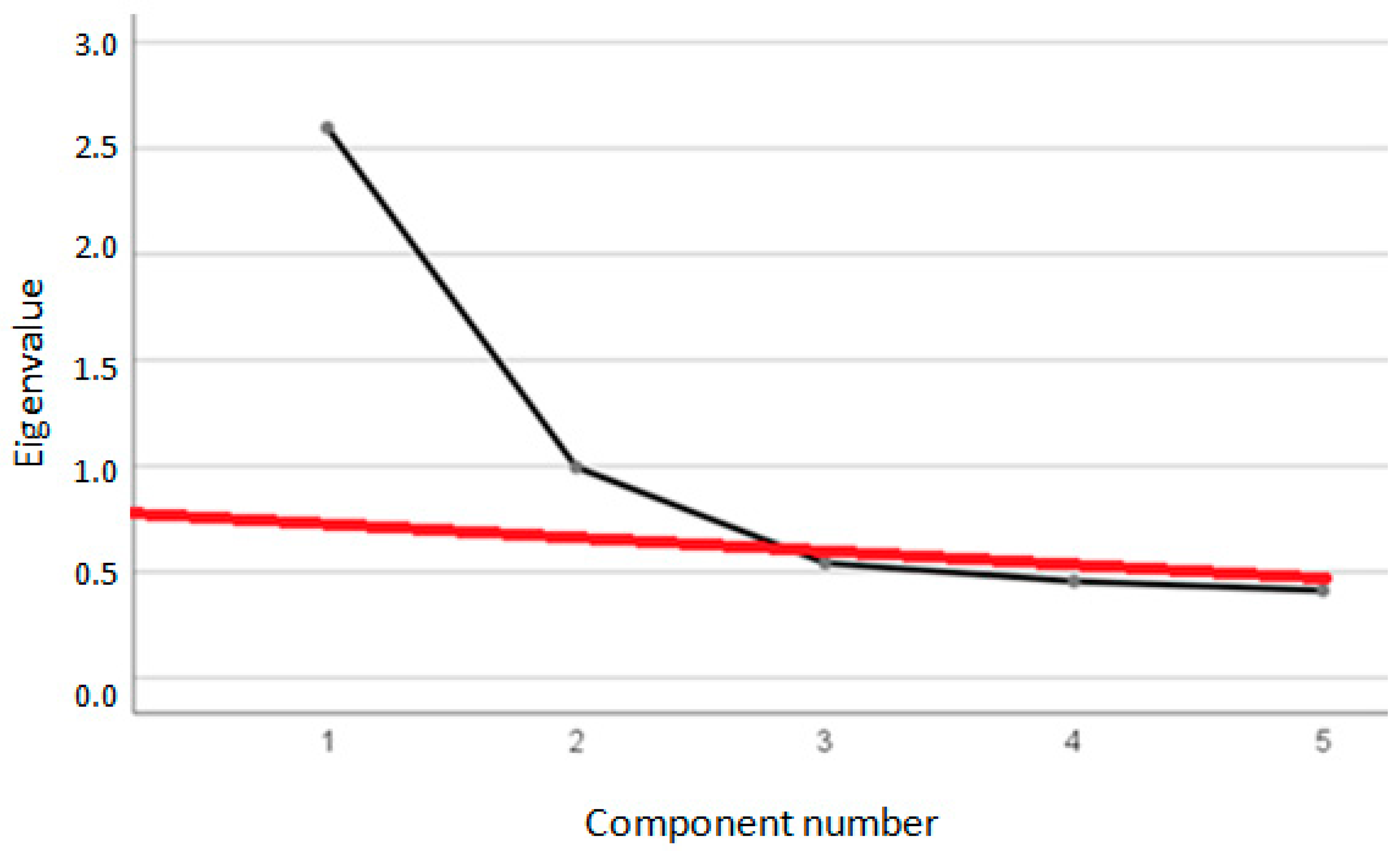
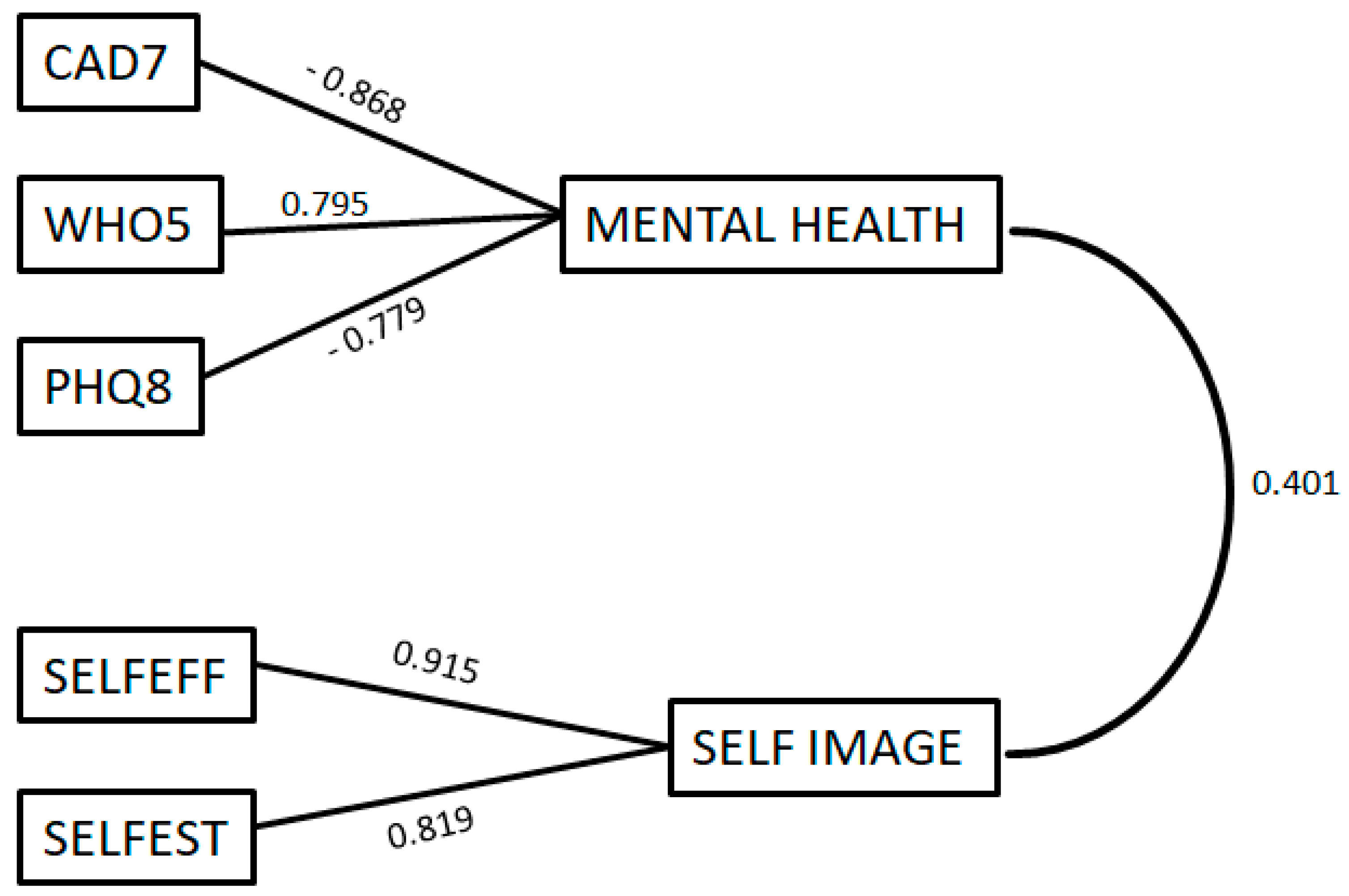
3.3. PCA Factor Analysis
3.4. Simple Linear Regression Analyses
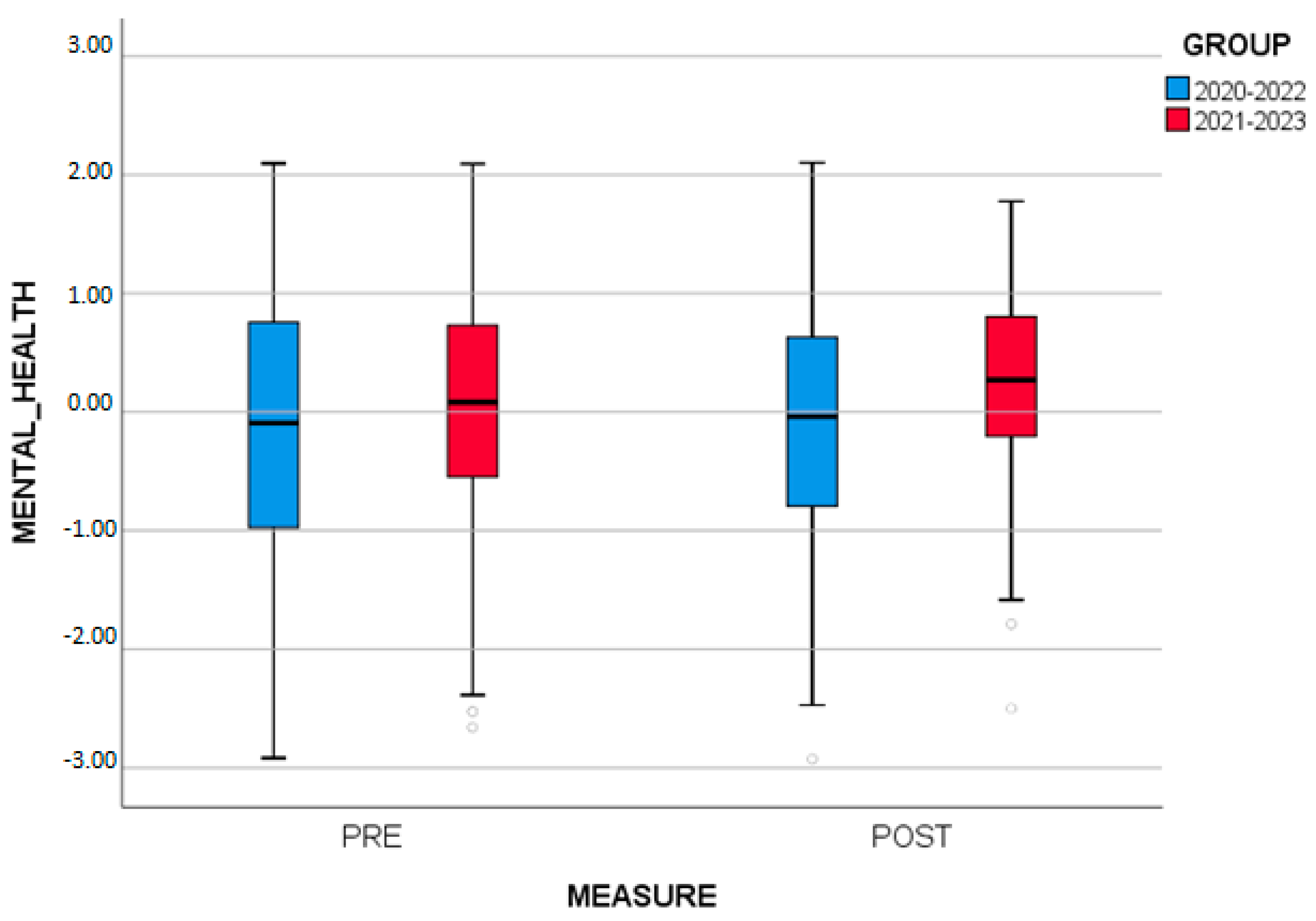
3.5. Two-Way Repeated Measures ANOVA
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| Abbreviation | Definition of the abbreviations |
| SCS | Second Chance School |
| GAD7 | The value extracted from the questionnaire GAD-7 (the variable includes observations, regardless of whether they are before or after the studies) |
| PHQ8 | The value extracted from the questionnaire PHQ-8 (the variable includes observations, regardless of whether they are before or after the studies) |
| WHO5 | The value extracted from the questionnaire WHO-5 (the variable includes observations, regardless of whether they are before or after the studies) |
| SELFEFF | The value extracted from the questionnaire Generalized Self-Efficacy Scale (the variable includes observations, regardless of whether they are before or after the studies) |
| SELFEST | The value extracted from the questionnaire Rosenberg Self-Esteem Scale (RSES) (the variable includes observations, regardless of whether they are before or after the studies) |
| MENTAL_HEALTH_POST | The value (factor scores) of mental health after the completion of the studies |
| MENTAL_HEALTH_PRE | The value (factor scores) of mental health at the beginning of the studies |
| SELF_IMAGE_POST | The value (factor scores) of self-image after the completion of the studies |
| SELF_IMAGE_PRE | The value (factor scores) of self-image at the beginning of the studies |
| GAD7AFTERNUMBER | The value extracted from the questionnaire GAD-7 after the completion of the studies |
| GAD7BEFORENUMBER | The value extracted from the questionnaire GAD-7 at the beginning of the studies |
| PHQ8AFTERNUMBER | The value extracted from the questionnaire PHQ-8 after the completion of the studies |
| PHQ8BEFORENUMBER | The value extracted from the questionnaire PHQ-8 at the beginning of the studies |
| WHO5AFTERNUMBER | The value extracted from the questionnaire WHO-5 after the completion of the studies |
| WHO5BEFORENUMBER | The value extracted from the questionnaire WHO-5 at the beginning of the studies |
| SELFESTEEMAFTERNUMBER | The value extracted from the questionnaire Rosenberg Self-Esteem Scale (RSES) after the completion of the studies |
| SELFESTEEMBEFORENUMBER | The value extracted from the questionnaire Rosenberg Self-Esteem Scale (RSES) at the beginning of the studies |
| SELFEFFICACYAFTERNUMBER | The value extracted from the questionnaire Generalized Self-Efficacy Scale after the completion of the studies |
| SELFEFFICACYBEFORENUMBER | The value extracted from the questionnaire Generalized Self-Efficacy Scale at the beginning of the studies |
References
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Ou, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. Clinical Characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Güner, H.R.; Hasanoğlu, İ.; Aktaş, F. COVID-19: Prevention and control measures in community. Turk. J. Med. Sci. 2020, 50, 571–577. [Google Scholar] [PubMed]
- Wei, W.E.; Li, Z.; Chiew, C.J.; Yong, S.E.; Toh, M.P.; Lee, V.J. Presymptomatic Transmission of SARS-CoV-2—Singapore, January 23–March 16, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 411–415. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Responding to Community Spread of COVID-19. 2020. Available online: https://www.who.int/publications-detail/responding-to-community-spread-of-covid-19 (accessed on 28 February 2023).
- Official Gazette 42/A/25-2-2020; Urgent Measures to Avoid and Limit the Spread of Coronavirus. Available online: https://www.e-nomothesia.gr/kat-ygeia/astheneies/praxe-nomothetikou-periekhomenou-tes-25-2-2020.html (accessed on 10 March 2023).
- Official Gazette 64/A/14-3-2020; Urgent Measures to Avoid and Limit the Spread of Coronavirus. Available online: https://www.kodiko.gr/nomothesia/document/609933/p.n.p.-14-3-2020-2020 (accessed on 10 March 2023).
- Joint Ministerial Decision (KYA) 2867/Y1. Imposing the Measure of the Temporary Ban on the Performance of All Kinds of Functions and Services in Religious Places of Worship for the Period from 16.3.2020 to 30.3.2020; Official Gazette 872/B/16-3-2020. Available online: https://www.e-nomothesia.gr/kat-ygeia/astheneies/koine-upourgike-apophase-2867u1.html (accessed on 10 March 2023).
- Joint Ministerial Decision (KYA) D1 20036/2020. Imposition of the Measure of Temporary Restriction of the Movement of Citizens to Deal with the Risk of the Spread of the COVID-19 Coronavirus; Official Gazette 986/B/22-3-2020. Available online: https://www.elinyae.gr/ethniki-nomothesia/ya-d1agp-oik-200362020-fek-986b-2232020 (accessed on 10 March 2023).
- Joint Ministerial Decision KYA 29114/2020. Distance Rules in Private Businesses, Public Services and Other Public Gathering Places throughout the Territory, to Limit the Spread of the COVID-19 Coronavirus; Official Gazette 1780/B/10-5-2020. Available online: https://www.e-nomothesia.gr/kat-ygeia/astheneies/koine-upourgike-apophase-dia-gp-oik-29114-2020.html (accessed on 10 March 2023).
- World Health Organization. Coronavirus Disease (COVID-19) Disease. Available online: https://www.who.int/europe/emergencies/situations/covid-19 (accessed on 29 July 2023).
- Rubin, J.G. The psychological effects of quarantining a city. BMJ 2020, 368, 313. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Taylor, S. The Psychology of Pandemics: Preparing for the Next Global Outbreak of Infectious Disease; Cambridge Scholars Publishing: Newcastle upon Tyne, UK, 2019. [Google Scholar]
- Duan, L.; Zhu, G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet 2020, 7, 300–302. [Google Scholar] [CrossRef]
- Magson, N.R.; Freeman, J.Y.; Rapee, R.M.; Richardson, C.E.; Oar, E.L.; Fardouly, J. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J. Youth Adolesc. 2021, 50, 44–57. [Google Scholar] [CrossRef]
- Rauschenberg, C.; Schick, A.; Hirjak, D.; Seidler, A.; Paetzold, I.; Apfelbacher, C.; Reininghaus, U. Evidence synthesis of digital interventions to mitigate the negative impact of the COVID-19 pandemic on public mental health: Rapid meta-review. J. Med. Internet Res. 2021, 23, 23365. [Google Scholar] [CrossRef]
- Bruine de Bruin, W. Age differences in COVID-19 risk perceptions and mental health: Evidence from a national US survey conducted in March 2020. J. Gerontol. Ser. B 2021, 76, 24–29. [Google Scholar] [CrossRef]
- Kumar, A.; Nayar, K.R. COVID 19 and its mental health consequences. J. Ment. Health 2021, 30, 1–2. [Google Scholar] [CrossRef]
- World Health Organization. COVID-19 and Violence Against Women: What the Health Sector/System Can Do; WHO: Geneva, Switzerland, 2020; Available online: https://www.who.int/reproductivehealth/publications/emergencies/COVID-19-VAW-full-text.pdf (accessed on 10 March 2023).
- Li, W.; Yang, Y.; Liu, Z.H.; Zhao, Y.J.; Zhang, Q.; Zhang, L.; Cheung, T.; Xiang, Y.T. Progression of Mental Health Services during the COVID-19 Outbreak in China. Int. J. Biol. Sci. 2020, 16, 1732–1738. [Google Scholar] [CrossRef] [PubMed]
- Moukaddam, N.; Shah, A. Psychiatrists beware! The impact of COVID-19 and pandemics on mental health. Psychiatr. Times 2020, 37, 11–12. [Google Scholar]
- Yao, H.; Chen, J.; Xu, Y. Patients with mental health disorders in the COVID-19 epidemic. Lancet 2020, 7, 21. [Google Scholar] [CrossRef]
- Golberstein, E.; Wen, H.; Miller, B.F. Coronavirus Disease 2019 (COVID-19) and Mental Health for Children and Adolescents. JAMA Pediatr. 2020, 174, 819–820. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, R.; Dubey, M.J.; Chatterjee, S.; Dubey, S. Impact of COVID-19 on children: Special focus on the psychosocial aspect. Minerva Pediatr. 2020, 72, 226–235. [Google Scholar] [CrossRef] [PubMed]
- Saddik, B.; Hussein, A.; Albanna, A.; Elbarazi, I.; Al-Shujairi, A.; Temsah, M.-H.; Sharif-Askari, F.S.; Stip, E.; Hamid, Q.; Halwani, R. The psychological impact of the COVID-19 pandemic on adults and children in the United Arab Emirates: A nationwide cross-sectional study. BMC Psychiatry 2021, 21, 224. [Google Scholar] [CrossRef] [PubMed]
- Lopez, A.; Caffò, A.O.; Tinella, L.; Di Masi, M.N.; Bosco, A. Variations in mindfulness associated with the COVID-19 outbreak: Differential effects on cognitive failures, intrusive thoughts and rumination. Appl. Psychol. Health 2021, 13, 761–780. [Google Scholar]
- Kaparounaki, C.K.; Patsali, M.E.; Mousa, D.P.V.; Papadopoulou, E.V.; Papadopoulou, K.K.; Fountoulakis, K.N. University students’ mental health amidst the COVID-19 quarantine in Greece. Psychiatry Res. 2020, 290, 113111. [Google Scholar] [CrossRef]
- Pokhrel, S.; Chhetri, R. A literature review on impact of COVID-19 pandemic on teaching and learning. High. Educ. Future 2021, 8, 133–141. [Google Scholar] [CrossRef]
- Daniel, S.J. Education and the COVID-19 pandemic. Prospects 2020, 49, 91–96. [Google Scholar] [CrossRef]
- Patrinos, H.A.; Shmis, T. Can Technology Help Mitigate the Impact of COVID-19 on Education Systems in Europe and Central Asia? The World Bank Group: Washington, DC, USA, 2020. Available online: https://blogs.worldbank.org/europeandcentralasia/can-technology-help-mitigate-impact-covid-19-education-systems-europe-and (accessed on 15 March 2023).
- Beaunoyer, E.; Dupere, S.; Guitton, M.J. COVID-19 and digital inequalities: Reciprocal impacts and mitigation strategies. Comput. Hum. Behav. 2020, 111, 106424. [Google Scholar]
- James, N.; Virginie, T. Adult education in times of the COVID-19 pandemic: Inequalities, changes, and resilience. Stud. Educ. Adults 2020, 52, 129–133. [Google Scholar]
- Jæger, M.M.; Blaabæk, E.H. Inequality in learning opportunities during COVID-19: Evidence from library takeout. Res. Soc. Stratif. Mobil. 2020, 68, 100524. [Google Scholar] [PubMed]
- Tinella, L.; Tinterri, A.; Dipace, A.; Ladogana, M.; Loiodice, I.; Bosco, A. Sociodemographic and digital education factors are associated to general health, coping strategies, and academic outcomes of undergraduate students during the post-pandemic period. Eur. J. Investig. Health Psychol. Educ. 2022, 12, 1334–1348. [Google Scholar]
- Cuerdo-Vilches, T.; Navas-Martín, M.Á. Confined students: A visual-emotional analysis of study and rest spaces in the homes. Int. J. Environ. Res. Public Health 2021, 18, 5506. [Google Scholar] [PubMed]
- Stoilescu, D.; Carapanait, C. Renegotiating relations among teacher, community and students. Eur. Educ. 2011, 43, 54–73. [Google Scholar] [CrossRef]
- Ross, S.; Gray, J. Transition and re-engagement through Second Chance Education. Aust. Educ. Res. 2005, 32, 103–140. [Google Scholar] [CrossRef]
- Arico, F.; Lasselle, L. Enhancing Interns’ Aspirations towards the Labour Market through Skill Acquisition: The Second Chance Schools Experience. Sire Discussion Paper (56). Scottish Institute for Research in Economics. 2010. Available online: https://www.researchgate.net/publication/46467689_Enhancing_Internsa_Aspirations_towards_the_Labour_Market_through_Skill-Acquisition_The_Second_Chance_Schools_Experience (accessed on 14 April 2023).
- European Commission. White Paper on Education and Training, Teaching and Learning. Towards the Knowledge Society. Office for Official Publications of the European Communities: Luxembourg, 1996. Available online: https://europa.eu/documents/comm/white_papers/pdf/com95_590_en.pdf (accessed on 16 April 2023).
- FEK 188/1997. Available online: https://www.kodiko.gr/nomothesia/document/205665/nomos-2525-1997 (accessed on 22 March 2023).
- FEK 1861/2014. Available online: https://edu.klimaka.gr/nomothesia/fek/2434-fek-1861-2014-kanonismos-leitourgias-sde (accessed on 28 March 2023).
- Inedivim. Second Chance Schools. 2018. Available online: https://www.inedivim.gr/%CF%80%CF%81%CE%BF%CE%B3%CF%81%CE%AC%CE%BC%CE%BC%CE%B1%CF%84%CE%B1-%CE%B4%CF%81%CE%AC%CF%83%CE%B5%CE%B9%CF%82/%CF%83%CF%87%CE%BF%CE%BB%CE%B5%CE%AF%CE%B1-%CE%B4%CE%B5%CF%8D%CF%84%CE%B5%CF%81%CE%B7%CF%82-%CE%B5%CF%85%CE%BA%CE%B1%CE%B9%CF%81%CE%AF%CE%B1%CF%82 (accessed on 28 March 2023).
- Vergidis, D. External evaluation of second chance schools. In Study Specifications for Second Chance Schools; Vekris, L., Hontolidou, E., Eds.; GSEE-IDEKE: Athens, Greece, 2003; pp. 65–74. [Google Scholar]
- Doukas, X. Lifelong Learning. In Identities, States and Politics; GSEE: Athens, Greece, 2003. [Google Scholar]
- Vergidis, D.; Prokou, E. Planning, management, evaluation of adult education programs. In Elements of Socio-Economic Functioning and Institutional Framework; EAP: Patras, Greece, 2005; Volume A. [Google Scholar]
- Vergidis, D.; Efstratoglou, A.; Nikolopoulou, B. Second Chance Schools: Innovative elements, problems and perspectives. Adult Educ. 2007, 12, 25–26. [Google Scholar]
- McGregor, G.; Mills, M. Alternative education sites and marginalized young people: ‘I wish there were more schools like this one’. Int. J. Incl. Educ. 2012, 16, 843–862. [Google Scholar]
- Hammarstrom, A.; Janlert, U. Early unemployment can contribute to adult health problems: Results from a longitudinal study of school leavers. J. Epidemiol. Community Health 2002, 56, 624–630. [Google Scholar]
- Collett, K.; Shoesmith, K.; Jones, P.; Miller, C.; Pickernell, D.; Packham, G. The role of education, training and skills development in social inclusion: The university of the heads of the valley case study. Educ. Train. 2011, 53, 638–651. [Google Scholar]
- McGregor, G.; Mills, M.; Te Riele, K.; Hayes, D. Excluded from school: Getting a second chance at a ‘meaningful’ education. Int. J. Incl. Educ. 2014, 19, 608–625. [Google Scholar] [CrossRef]
- Francis, B.; Mills, M. Schools as Damaging Organisations: Instigating a Dialogue Concerning Alternative Models of Schooling. Pedagog. Cult. Soc. 2012, 20, 251–271. [Google Scholar] [CrossRef]
- Hayes, D. Re-engaging Marginalised Young People in Learning: The Contribution of Informal Learning and Community-Based Collaborations. J. Educ. Policy 2012, 27, 641–653. [Google Scholar]
- Michail, D.; Anastasiou, D. Gender discrimination and learning disabilities as the main reasons of dropping-out of basic education: A retrospective study in the context of Second-Chance School in Greece. In Lifelong Learning and Active Citizenship; Cunningham, P., Fretwell, N., Eds.; CiCe: London, UK, 2010. [Google Scholar]
- Landritsi, I. The learners of the Second Chance Schools: Research on Their Characteristics and Cultural Capital in the SDE of Patras, Pyrgos and Agrinio. Bachelor’s Thesis, University of Patras, Patras, Greece, 2010. [Google Scholar]
- Kritikos, A. I grow old and learn. The social profile of the students of a second chance school. Pedagog. Rev. 2013, 56, 65–81. [Google Scholar]
- Papanis, E.; Roumeliotou, M. Basic Principles of Adult Education: Pedagogical Theories and Enhancing self-Esteem. Greek Social Survey. 2007. Available online: http://epapanis.blogspot.com/2007/09/blog-post_5311.html (accessed on 28 March 2023).
- Weiss, B.D.; Francis, K.; Senf, J.H.; Heist, K.; Hargarves, R. Literacy education as treatment for depression in patients with limited literacy and depression: A randomized controlled trial. J. Gen. Intern. Med. 2006, 21, 823–828. [Google Scholar]
- Andreadakis, N.; Maggopoulos, G. Evaluation of counseling services in Second Chance Schools: A multi-methodological empirical investigation. Educ. Sci. 2017, 3, 125–144. [Google Scholar]
- Katsarou, E.; Tsafos, V. Collaborative school innovation project as a pivot for teachers’ professional development: The case of Acharnes’ Second Chance School in Greece. Teach. Dev. 2008, 12, 125–138. [Google Scholar]
- Cullen, W.; Gulati, G.; Kelly, B.D. Mental health in the COVID-19 pandemic. QJM An. Int. J. Med. 2020, 113, 311–312. [Google Scholar] [CrossRef]
- Papageorgiou, G. Quantitative Research. 2014. Available online: http://sociology.soc.uoc.gr/pegasoc/wp-content/uploads/2014/10/Microsoft-Word-Papageorgiou_DEIGMATOLHPTIKH1.pdf (accessed on 28 March 2023).
- Galanis, P. Sampling methods in epidemiological studies. Arch. Hell. Med. 2012, 29, 57–60. [Google Scholar]
- Spitzer, R.L.; Kroenke, K.W.; Janet, B.W.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed]
- Swinon, R.P. The GAD-7 scale was accurate for diagnosing generalized anxiety disorder. Evid. Based Med. 2006, 11, 184. [Google Scholar] [CrossRef] [PubMed]
- Lowe, Β.; Decker, O.; Muller, S.; Brahler, E.; Schellberg, D.; Herzog, W.; Herzberg, P.Y. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med. Care 2008, 46, 266–274. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Monahan, P.O.; Löwe, B. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Ann. Intern. Med. 2007, 146, 317–325. [Google Scholar] [CrossRef]
- Wu, Y.; Levis, B.; Riehm, K.; Saadat, N.; Levis, A.; Azar, M.; Thombs, B. Equivalency of the diagnostic accuracy of the PHQ-8 and PHQ-9: A systematic review and individual participant data meta-analysis. Psychol. Med. 2020, 50, 1368–1380. [Google Scholar]
- Cameron, I.M.; Crawford, J.R.; Lawton, K.; Reid, I.C. Psychometric Comparison of PHQ-9 and HADS for Measuring Depression Severity in Primary Care. Br. J. Gen. Pract. 2008, 58, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Carey, M.; Boyes, A.; Noble, N.; Waller, A.; Inder, K. Validation of the PHQ-2 against the PHQ-9 for Detecting Depression in a Large Sample of Australian General Practice Patients. Aust. J. Prim. Health 2016, 22, 262–266. [Google Scholar]
- Pfizer Inc. Screener Overview. 2020. Available online: https://www.phqscreeners.com/select-screener (accessed on 10 August 2020).
- The WHO-5 Website. About the WHO-5. 2019. Available online: https://www.psykiatri-regionh.dk/who-5/about-the-who-5/Pages/default.aspx (accessed on 8 July 2019).
- Papanas, N.; Tsapas, A.; Papatheodorou, K.; Papazoglou, D.; Bekiari, E.; Sarigianni, M.; Paletas, K.; Maltezos, E. Glycaemic control is correlated with Well Being Index (WHO-5) in subjects with type 2 diabetes. Exp. Clin. Endocrinol. 2010, 118, 364–367. [Google Scholar] [CrossRef]
- Shea, S.; Skovlund, S.; Bech, P.; Kalo, I.; Home, P.D. Routine assessment of psychological wellbeing in people with diabetes in primary care—Validation of the WHO-5-Well-being-Index in six countries. Diabetologia 2003, 46, A88. [Google Scholar]
- Topp, C.W.; Ostergaard, S.D.; Sondergaard, S.; Bech, P. The WHO-5 Well-Being Index: A systematic review of the literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar]
- The World Health Organization. Five Well Being Index (WHO-5). Available online: https://www.corc.uk.net/outcome-experience-measures/the-world-health-organisation-five-well-being-index-who-5/#:~:text=Terms%20of%20use,not%20require%20permission%20to%20use (accessed on 20 May 2023).
- Galanou, C.; Galanakis, M.; Alexopoulos, E.; Darviri, C. Rosenberg self-esteem scale Greek validation on student sample. Psychology 2014, 5, 819–827. [Google Scholar] [CrossRef]
- Robins, R.W.; Hendin, H.M.; Trzesniewski, K.H. Measuring Global Self-Esteem: Construct Validation of a Single-Item Measure and the Rosenberg Self-Esteem Scale. Pers. Soc. Psychol. Bull. 2001, 27, 151–161. [Google Scholar] [CrossRef]
- Rosenberg Self-Esteem Scale (RES). Available online: https://www.psytoolkit.org/survey-library/self-esteem-rosenberg.html#:~:text=%22%22%20May%20I%20have%20permission%20to,scale%20in%20your%20professional%20research (accessed on 20 May 2023).
- Schwarzer, R.; Jerusalem, M. Generalized Self-Efficacy scale. In Measures in Health Psychology: A User’s Portfolio; Weinman, J., Wright, S., Johnston, M., Eds.; Causal and control beliefs (35–37); NFER-NELSON: Windsor, UK, 1995. [Google Scholar]
- Glynou, E.; Jerusalem, M.; Schwarzer, R. Greek Version of the General Self-Efficacy Scale. 1992. Available online: http://www.ralfschwarzer.de (accessed on 5 March 2023).
- Schwarzer, R.; Hallum, S. Perceived Self-Efficacy as a Predictor of Job Stress and Burnout: Mediation Analyses. Appl. Psychol: Int. Rev. 2008, 57, 152–171. [Google Scholar] [CrossRef]
- Documentation of the Self-Efficacy Scale. Available online: https://userpage.fu-berlin.de/~health/faq_gse.pdf (accessed on 20 May 2023).
- FEK 3780/2020. Available online: https://www.esos.gr/sites/default/files/articles-legacy/leitoyrgia_ton_ekpaideytikon_monadon.pdf (accessed on 3 March 2023).
- FEK 4187/2021. Available online: https://www.especial.gr/wp-content/uploads/2021/09/leitourgia-domwn-ekpaidefsis-metra-covid-2021-22.pdf (accessed on 3 March 2023).
- FEK 2676/2022. Available online: https://www.alfavita.gr/sites/default/files/2022-06/metra-sxoleia-koronoios.pdf (accessed on 3 March 2023).
- Mooi, E.; Sarstedt, M.; Mooi-Reci, I. Principal component and factor analysis. In Market Research: The Process, Data, and Methods Using Stata; Springer: Singapore, 2018; pp. 265–311. [Google Scholar]
- Plakias, S.; Kokkotis, C.; Moustakidis, S.; Tsatalas, T.; Papalexi, M.; Kasioura, C.; Giakas, G.; Tsaopoulos, D. Identifying playing styles of european soccer teams during the key moments of the game. J. Phys. Educ. Sport. 2023, 23, 878–890. [Google Scholar]
- Tarhan, N.; Demirsoy, Ç.; Tutgun-Ünal, A. Measuring the Awareness Levels of Individuals with Alcohol and Substance Use Disorders: Tertiary Prevention Standards and Development of Uskudar Result Awareness and Harm Perception Scales. Brain Sci. 2023, 13, 901. [Google Scholar] [PubMed]
- Taherdoost, H.; Sahibuddin, S.; Jalaliyoon, N. Exploratory factor analysis; concepts and theory. Adv. Pure Appl. Math. 2022, 27, 375–382. [Google Scholar]
- Shrestha, N. Factor analysis as a tool for survey analysis. Am. J. Appl. Math. Stat. 2021, 9, 4–11. [Google Scholar] [CrossRef]
- Rojas-Valverde, D.; Pino-Ortega, J.; Gómez-Carmona, C.D.; Rico-González, M. A systematic review of methods and criteria standard proposal for the use of principal component analysis in team’s sports science. Int. J. Environ. Res. Public Health 2020, 17, 8712. [Google Scholar] [CrossRef]
- Cattell, R.B. The scree test for the number of factors. Multivar. Behav. Res. 1966, 1, 245–276. [Google Scholar] [CrossRef]
- Ledesma, R.D.; Valero-Mora, P.; Macbeth, G. The scree test and the number of factors: A dynamic graphics approach. Span. J. Psychol. 2015, 18, E11. [Google Scholar] [CrossRef]
- Ruscio, J.; Roche, B. Determining the number of factors to retain in an exploratory factor analysis using comparison data of known factorial structure. Psychol. Assess. 2012, 24, 282. [Google Scholar] [CrossRef] [PubMed]
- Ndayishimiye, J.B.; Schneider, B.H.; Simbananiye, L.; Baubet, T. The Relationship between Trauma and Attachment in Burundi’s School-Aged Children. Brain Sci. 2023, 13, 666. [Google Scholar] [CrossRef] [PubMed]
- Zou, K.H.; Tuncali, K.; Silverman, S.G. Correlation and simple linear regression. Radiology 2003, 227, 617–628. [Google Scholar] [CrossRef] [PubMed]
- Mishra, P.; Singh, U.; Pandey, C.M.; Mishra, P.; Pandey, G. Application of student’s t-test, analysis of variance, and covariance. Ann. Card. Anaesth. 2019, 22, 407. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Xu, Y.; Deshpande, G.; Li, K.; Sun, P.; Liang, P. The effect of light sedation with midazolam on functional connectivity of the dorsal attention network. Brain Sci. 2021, 11, 1107. [Google Scholar] [CrossRef]
- Li, S.; Li, Y.; Liu, S.; He, W.; Luo, W. Emotional Valence in the Eye Region Modulates the Attentional Blink in a Task-Dependent Manner: Evidence from Event-Related Potentials. Brain Sci. 2022, 12, 1665. [Google Scholar]
- Turner, N.E. The effect of common variance and structure pattern on random data eigenvalues: Implications for the accuracy of parallel analysis. Educ. Psychol. Meas. 1998, 58, 541–568. [Google Scholar]
- Bergersen, H.; Froslie, K.F.; Sunnerhagen, K.S.; Schanke, A.K. Anxiety, Depression and Psychological Well-Being 2 to 5 years Poststroke. J. Stroke Cerevobrasc. Dis. 2010, 19, 364–369. [Google Scholar] [CrossRef]
- Jorm, A.F.; Korten, A.E.; Christensen, H.; Jacomb, P.A.; Rodgers, B.; Parslow, R.A. Association of obesity with anxiety, depression and emotional well-being: A community survey. Aust. N. Z. J. Public Health 2022, 27, 434–440. [Google Scholar]
- Lattie, E.G.; Adkins, E.C.; Winquist, N.; Stiles- Shields, C.; Wafford, Q.E.; Graham, A.K. Digital mental health interventions for depression, anxiety and enhancement of psychological well-being among college students: A systematic review. J. Med. Internet Res. 2019, 21, e12869. [Google Scholar]
- McMahon, E.M.; Corcoran, P.; O’Regan, G.; Keeley, H.; Cannon, M.; Carli, V.; Wasserman, C.; Hadlaczky, G.; Sarchiapone, M.; Apter, A.; et al. Physical activity in European adolescents and association with anxiety, depression and well-being. Eur. Child Adoles. Psychiatry 2017, 26, 111–122. [Google Scholar] [CrossRef]
- Headey, B.; Kelley, J.; Wearing, A. Dimensions of mental health: Life satisfaction, positive affect, anxiety and depression. Soc. Indic. Res. 1993, 29, 63–82. [Google Scholar] [CrossRef]
- Garaika, G.; Margahana, H.M.; Negara, S.T. Self efficacy, self personality and self confidence on entrepreneurial intention: Study on young enterprises. J. Entrep. Educ. 2019, 22, 1–12. [Google Scholar]
- Brookes, J. The effect of overt and covert narcissism on self-esteem and self-efficacy beyond self-esteem. Pers. Individ. Differ. 2015, 85, 172–175. [Google Scholar] [CrossRef]
- Wong, M.C.S.; Lau, T.C.M.; Lee, A. The impact of leadership programme on self-esteem and self-efficacy in school: A randomized control trial. PLoS ONE 2012, 7, e52023. [Google Scholar] [CrossRef]
- Steese, S.; Dollette, M.; Phillips, W.; Hossfeld, E.; Matthews, G.; Taormina, G. Understanding girls’ circle as an intervention on perceived social support, body image, self-efficacy, locus of control and self-esteem. Adolescence 2006, 41, 55–74. [Google Scholar]
- Bacchini, D.; Magliulo, F. Self-Image and Perceived Self-Efficacy During Adolescence. J. Youth Adolesc. 2003, 32, 337–349. [Google Scholar] [CrossRef]
- Doswell, W.M.; Millor, G.K.; Thompson, H. Self-image and self-esteem in African-American preteen girls: Implications for mental health. Issues Ment. Health Nurs. 1998, 19, 71–94. [Google Scholar] [CrossRef]
- Mejstad, L.; Heiling, K.; Svedin, C.G. Mental health and self-image among deaf and hard of hearing children. Am. Ann. Deaf. 2008, 153, 504–516. [Google Scholar] [CrossRef]
- Heinrich, L.M.; Gullone, E. The clinical significance of loneliness: A literature review. Clin. Psychol. Rev. 2006, 26, 695–718. [Google Scholar] [CrossRef]
- Ozer, S. Social Support, Self-Efficacy, Self-Esteem, and Well-Being during COVID-19 Lockdown: A Two-Wave Study of Danish Students; Wiley: Hoboken, NJ, USA, 2022. [Google Scholar]
- Rossi, A.; Panzeri, A.; Pietrabissa, G.; Manzoni, G.M.; Castelnuovo, G.; Mannarini, S. The anxiety-buffer hypothesis in the time of COVID-19: When self-esteem protects from the impact of loneliness and fear on anxiety and depression. Front. Psychol. 2020, 11, 2177. [Google Scholar] [CrossRef] [PubMed]
- Karakitsiou, G.; Tsiakiri, A.; Kedraka, K. Investigating the Effects of Sociodemographic Characteristics on Psychological Factors That Impact on Educational Process of Adult Learners in Second Chance Schools in Greece. Rev. Eur. Stud. 2021, 13, 122. [Google Scholar] [CrossRef]
- Dimitriou-Christidi, E. “The Self-Perception and Self-Esteem of Second Chance School Graduates”. Available online: http://www.eur-alpha.eu/IMG/pdf/the_self-perception_and_self-esteem_of_second_chance_school_graduates.pdf (accessed on 7 July 2023).
- Papaioannou, E.; Gravani, M.N. Empowering vulnerable adults through second-change education: A case study from Cyprus. Int. J. Lifelong Educ. 2018, 37, 435–450. [Google Scholar] [CrossRef]
- Panayiotou, G.; Kokkinos, C.M. Self-consciousness and psychological distress: A study using the Greek SCS. Pers. Individ. Differ. 2006, 41, 83–93. [Google Scholar] [CrossRef]
- Giménez-Llort, L.; Martín-González, J.J.; Maurel, S. Secondary Impacts of COVID-19 Pandemic in Fatigue, Self-Compassion, Physical and Mental Health of People with Multiple Sclerosis and Caregivers: The Teruel Study. Brain Sci. 2021, 11, 1233. [Google Scholar]
- Tsamakis, K.; Tsiptsios, D.; Ouranidis, A.; Mueller, C.; Schizas, D.; Terniotis, C.; Nikolakakis, N.; Tyros, G.; Kympouropoulos, S.; Lazaris, A. COVID-19 and its consequences on mental health. Exp. Ther. Med. 2021, 21, 1. [Google Scholar] [CrossRef]
- Aknin, L.; De Neve, J.E.; Dunn, E.; Fancourt, D.; Goldberg, E.; Helliwell, J.F.; Jones, S.P.; Karam, E.; Layard, R.; Lyubomirsky, S. Mental health during the first year of the COVID-19 pandemic: A review and recommendations for moving forward. Perspect. Psychol. Sci. 2021, 17, 915–936. [Google Scholar]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health Sci. 2020, 16, 1–11. [Google Scholar]
- Varga, T.V.; Bu, F.; Dissing, A.S.; Elsenburg, L.K.; Bustamante, J.J.H.; Matta, J.; van Zon, S.K.R.; Brouwer, S.; Bültmann, U.; Fancourt, D. Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID-19 pandemic: A longitudinal analysis of 200,000 Western and Northern Europeans. Lancet Reg. Health 2021, 2, 100020. [Google Scholar]
- Zhou, S.-J.; Zhang, L.-G.; Wang, L.-L.; Guo, Z.-C.; Wang, J.-Q.; Chen, J.-C.; Liu, M.; Chen, X.; Chen, J.-X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry 2020, 29, 749–758. [Google Scholar] [CrossRef]
- Duan, L.; Shao, X.; Wang, Y.; Huang, Y.; Miao, J.; Yang, X.; Zhu, G. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. J. Affect. Disord. 2020, 275, 112–118. [Google Scholar] [CrossRef]
- Gazmararian, J.; Weingart, R.; Campbell, K.; Cronin, T.; Ashta, J. Impact of COVID-19 pandemic on the mental health of students from 2 semi-rural high schools in Georgia. J. Sch. Health 2021, 91, 356–369. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zhang, D.; Fang, J.; Wan, Y.; Tao, F.; Sun, Y. Assessment of mental health of Chinese primary school students before and after school closing and opening during the COVID-19 pandemic. JAMA Netw. Open. 2020, 3, 2021482. [Google Scholar] [CrossRef] [PubMed]
- Hou, T.Y.; Mao, X.F.; Dong, W.; Cai, W.P.; Deng, G.H. Prevalence of and factors associated with mental health problems and suicidality among senior high school students in rural China during the COVID-19 outbreak. Asian J. Psychiatr. 2020, 54, 102305. [Google Scholar] [CrossRef]
- Drelich-Zbroja, A.; Jamroz-Wiśniewska, A.; Kuczyńska, M.; Zbroja, M.; Cyranka, W.; Drelich, K.; Pustelniak, O.; Dąbrowska, I.; Markiewicz, K. The Impact of Study Mode (Online vs. Hybrid) on Early Symptoms of Depression and Coping Strategies among University Students in Poland in Time of COVID-19 Pandemic—Preliminary Study. Brain Sci. 2021, 11, 1578. [Google Scholar] [CrossRef] [PubMed]
- Boeren, E.; Roumell, E.A.; Roessger, K.M. COVID-19 and the future of adult education: An editorial. Adult Educ. Q. 2020, 70, 201–204. [Google Scholar] [CrossRef]
- Waller, R.; Hodge, S.; Holford, J.; Milana, M.; Webb, S. Lifelong education, social inequality and the COVID-19 health pandemic. Int. J. Lifelong Educ. 2020, 39, 243–246. [Google Scholar] [CrossRef]
- Watts, J. COVID-19 and the digital divide in the UK. Lancet 2020, 2, 395–396. [Google Scholar] [CrossRef]
- Lasby, D. Imagine Canada’s Sector Monitor: Charities & the COVID-19 Pandemic. Imagine Canada. 2020. Available online: https://imaginecanada.ca/sites/default/files/COVID-19%20Sector%20Monitor%20Report%20ENGLISH_0.pdf (accessed on 10 April 2023).
- Seal, E.; Vu, J.; Winfield, A.; Fenesi, B. Impact of COVID-19 on Physical Activity in Families Managing ADHD and the Cyclical Effect on Worsening Mental Health. Brain Sci. 2023, 13, 887. [Google Scholar] [CrossRef]
- Lagravinese, G.; Castellana, G.; Castellana, F.; Genco, M.; Petrelli, R.; Ruccia, M.; Aliani, M.; Carone, M.; Sardone, R.; Battista, P. Cognitive Deficits among Individuals Admitted to a Post-Acute Pneumological Rehabilitation Unit in Southern Italy after COVID-19 Infection. Brain Sci. 2023, 13, 84. [Google Scholar] [CrossRef]

| Academic Year of Distribution of Questionnaires | No. of Participants | Cycle | Conditions in Regard to COVID-19 |
|---|---|---|---|
| September 2020–June 2021 | 132 | A1 | Universal lockdown |
| September 2021–June 2022 | 132 | B1 | Lessons with special |
| 119 | A2 | measures | |
| September 2022–June 2023 | 119 | B2 | Non-COVID-19 year |
| Demographics | Frequency | Percentage |
|---|---|---|
| Sex | ||
| Male | 105 | 41.8 |
| Female | 146 | 58.2 |
| Total | 251 | 100.00 |
| Age group | ||
| 18–25 | 15 | 6 |
| 26–35 | 41 | 16.3 |
| 36–45 | 78 | 31.1 |
| 46–55 | 78 | 31.1 |
| 55+ | 39 | 15.5 |
| Total | 251 | 100.00 |
| Marital status | ||
| Married | 131 | 52.2 |
| Unmarried | 56 | 22.3 |
| Divorced | 36 | 14.3 |
| Widowed | 11 | 4.4 |
| In symbiosis | 17 | 6.8 |
| Total | 251 | 100.00 |
| Number of children | ||
| 0 | 74 | 29.5 |
| 1 | 37 | 14.7 |
| 2 | 85 | 33.9 |
| 3 | 37 | 14.7 |
| 4+ | 18 | 7.2 |
| Total | 251 | 100.00 |
| Occupation | ||
| Unemployed | 111 | 44.2 |
| Public employee | 32 | 12.7 |
| Working in the private sector | 92 | 36.7 |
| Retired | 14 | 5.6 |
| Other | 2 | 0.8 |
| Total | 251 | 100.00 |
| Component | Initial Eigenvalues | Extraction Sums of Squared Loadings | Rotation Sums of Squared Loadings | ||||
|---|---|---|---|---|---|---|---|
| Total | % of Variance | Cumulative % | Total | % of Variance | Cumulative % | Total | |
| 1 | 2.596 | 51.924 | 51.924 | 2.596 | 51.924 | 51.924 | 2.302 |
| 2 | 0.994 | 19.889 | 71.813 | 0.994 | 19.889 | 71.813 | 1.907 |
| 3 | 0.542 | 10.834 | 82.647 | ||||
| 4 | 0.455 | 9.108 | 91.755 | ||||
| 5 | 0.412 | 8.245 | 100 | ||||
| Number of Regression Analysis | Dependent Variable | Independent Variable | Unstandardized Coefficients B | |
|---|---|---|---|---|
| Constant | Independent Variable | |||
| 1 | MENTAL_HEALTH_POST | MENTAL_HEALTH_PRE | 0.091 | 0.622 |
| 2 | SELF_IMAGE_POST | SELF_IMAGE_PRE | 0.131 | 0.821 |
| 3 | GAD7AFTERNUMBER | GAD7BEFORENUMBER | 2.498 | 0.654 |
| 4 | PHQ8AFTERNUMBER | PHQ8BEFORENUMBER | 4.229 | 0.493 |
| 5 | WHO5AFTERNUMBER | WHO5BEFORENUMBER | 32.875 | 0.505 |
| 6 | SELFESTEEMAFTERNUMBER | SELFESTEEMBEFORENUMBER | 3.625 | 0.834 |
| 7 | SELFEFFICACYAFTERNUMBER | SELFEFFICACYBEFORENUMBER | 7.612 | 0.765 |
| Number of Regression Analysis | R | R Square | Adjusted R-Squared | F Change | df1 | df2 | Sig. F Change |
|---|---|---|---|---|---|---|---|
| 1 | 0.721 | 0.52 | 0.514 | 269.899 | 1 | 249 | <0.001 |
| 2 | 0.9 | 0.81 | 0.804 | 1059.223 | 1 | 249 | <0.001 |
| 3 | 0.679 | 0.462 | 0.459 | 213.453 | 1 | 249 | <0.001 |
| 4 | 0.549 | 0.301 | 0.299 | 107.434 | 1 | 249 | <0.001 |
| 5 | 0.591 | 0.349 | 0.347 | 133.759 | 1 | 249 | <0.001 |
| 6 | 0.867 | 0.752 | 0.751 | 756.901 | 1 | 249 | <0.001 |
| 7 | 0.833 | 0.694 | 0.693 | 564.797 | 1 | 249 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karakitsiou, G.; Plakias, S.; Kedraka, K.; Arvaniti, A.; Kokkotis, C.; Tsiakiri, A.; Samakouri, M. Investigating the Role of Second Chance Schools and COVID-19 Pandemic on the Mental Health and Self-Image of Greek Adult Students. Brain Sci. 2023, 13, 1203. https://doi.org/10.3390/brainsci13081203
Karakitsiou G, Plakias S, Kedraka K, Arvaniti A, Kokkotis C, Tsiakiri A, Samakouri M. Investigating the Role of Second Chance Schools and COVID-19 Pandemic on the Mental Health and Self-Image of Greek Adult Students. Brain Sciences. 2023; 13(8):1203. https://doi.org/10.3390/brainsci13081203
Chicago/Turabian StyleKarakitsiou, Georgia, Spyridon Plakias, Katerina Kedraka, Aikaterini Arvaniti, Christos Kokkotis, Anna Tsiakiri, and Maria Samakouri. 2023. "Investigating the Role of Second Chance Schools and COVID-19 Pandemic on the Mental Health and Self-Image of Greek Adult Students" Brain Sciences 13, no. 8: 1203. https://doi.org/10.3390/brainsci13081203
APA StyleKarakitsiou, G., Plakias, S., Kedraka, K., Arvaniti, A., Kokkotis, C., Tsiakiri, A., & Samakouri, M. (2023). Investigating the Role of Second Chance Schools and COVID-19 Pandemic on the Mental Health and Self-Image of Greek Adult Students. Brain Sciences, 13(8), 1203. https://doi.org/10.3390/brainsci13081203









