Supratentorial Lymphocytic Inflammation with Parenchymal Perivascular Enhancement Responsive to Steroids (SLIPPERS)—Does it Really Exist?
Abstract
1. Introduction
2. Methods
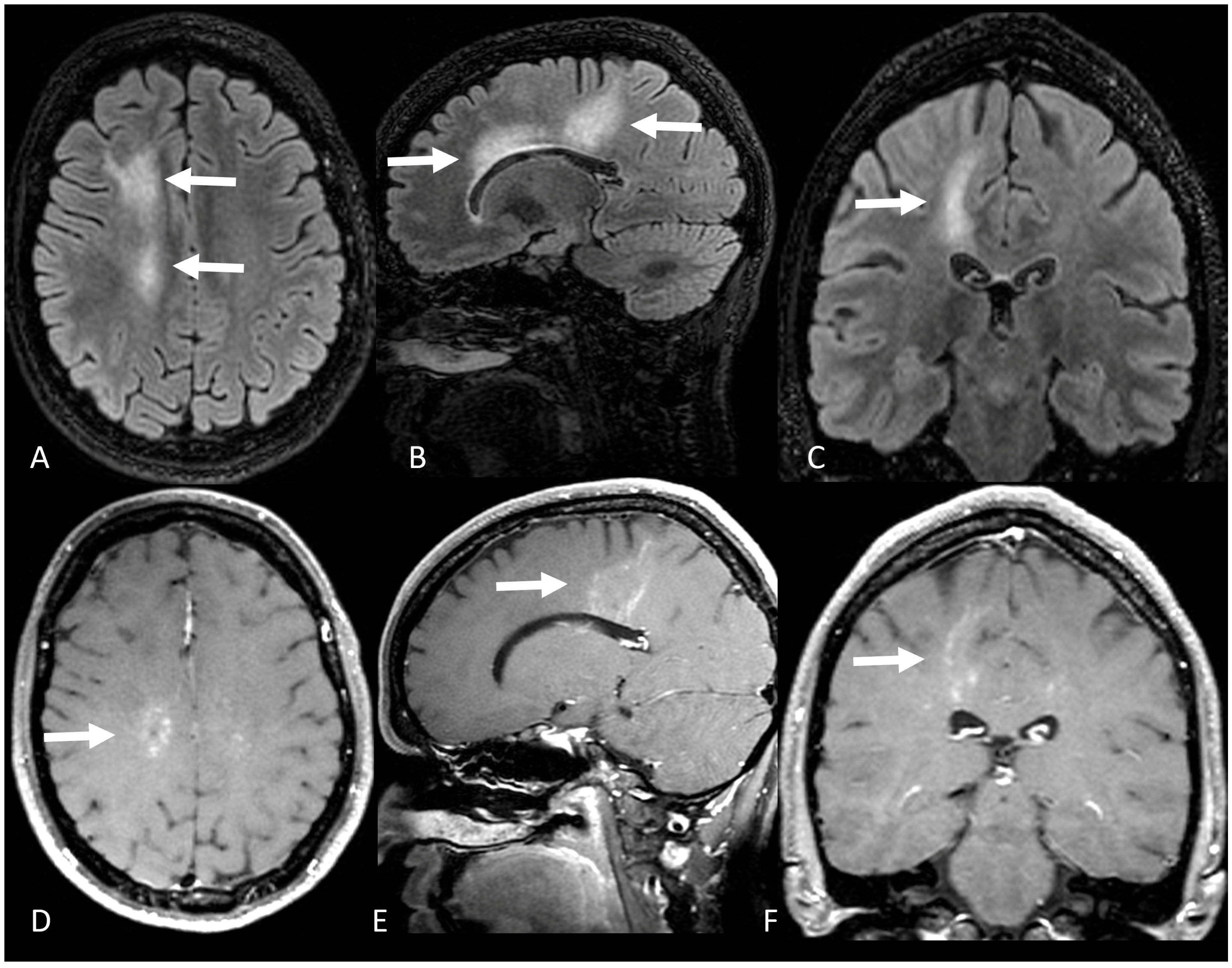
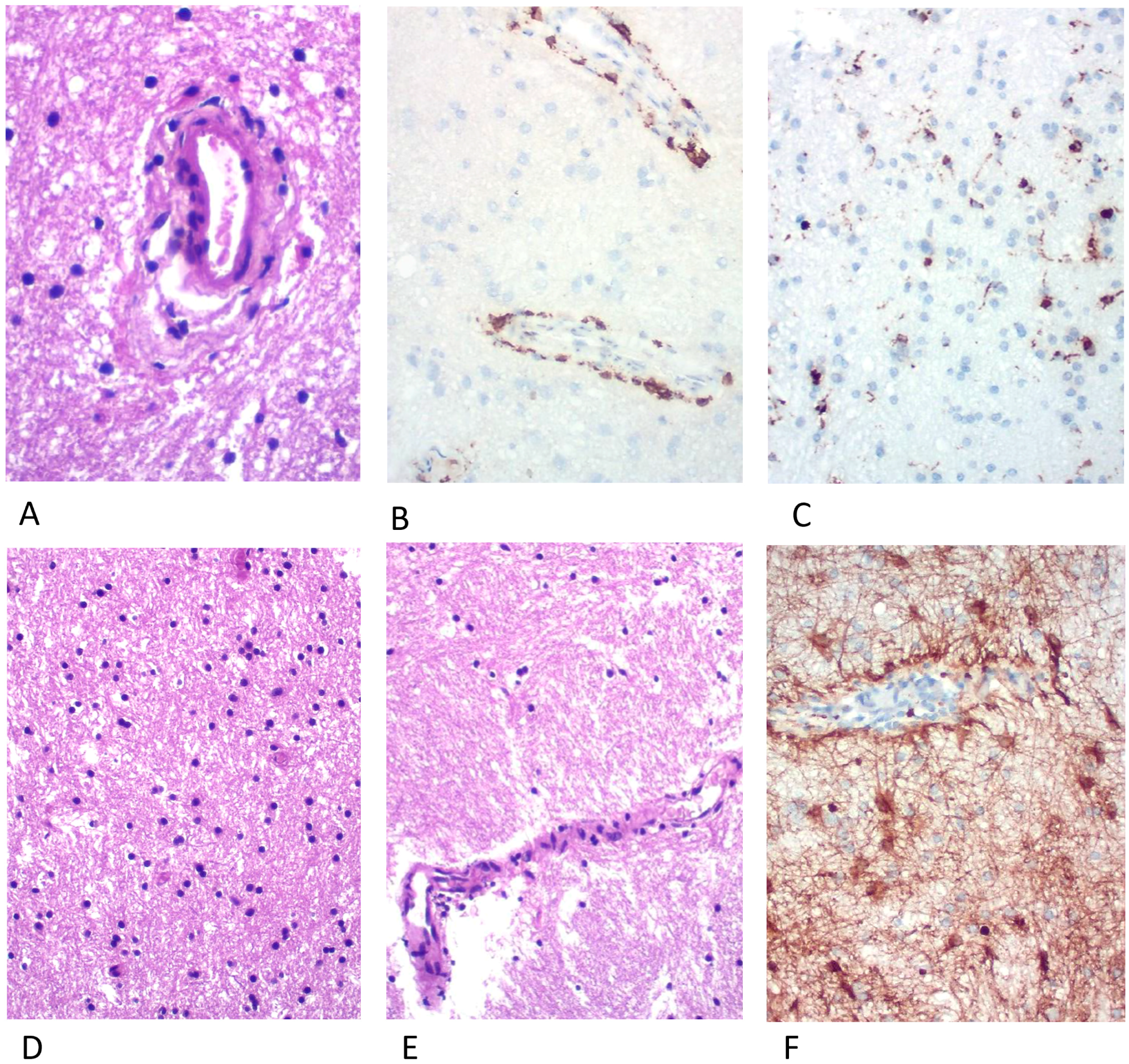
3. Case Report
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pittock, S.J.; Debruyne, J.; Krecke, K.N.; Giannini, C.; Van Den Ameele, J.; De Herdt, V.; McKeon, A.; Fealey, R.D.; Weinshenker, B.G.; Aksamit, A.J.; et al. Chronic Lymphocytic Inflammation with Pontine Perivascular Enhancement Responsive to Steroids (CLIPPERS). Brain 2010, 133, 2626–2634. [Google Scholar] [CrossRef] [PubMed]
- Taieb, G.; Allou, T.; Labauge, P. Therapeutic Approaches in CLIPPERS. Curr. Treat. Options Neurol. 2017, 19, 17. [Google Scholar] [CrossRef]
- Armand, C.; Graber, J.; Lado, F.; LaSala, P.; Weidenheim, K. SLIPPERS: Supratentorial Lymphocytic Inflammation with Parenchymal Perivascular Enhancement Responsive to Steroids: A Case Report (P5.118). Neurology 2015, 84, P5.118. [Google Scholar]
- Aglave, V.; Ojha, P.; Ansari, R.; Barvalia, P. A Case of Clippers with Spinal Cord Presentation. J. Neurol. Sci. 2019, 405, 159. [Google Scholar] [CrossRef]
- Nguyen, P.B.; Prentice, D.; Brazel, R.; Leong, W.K. Case Report: Hemidysgeusia, Phantosmia and Respiratory Arrest: A Case of CLIPPERS. BMJ Case Rep. 2019, 12, 230094. [Google Scholar] [CrossRef] [PubMed]
- Vola, E.; Russo, C.; Macera, A.; Del Vecchio, W.; Puoti, G.; Caranci, F.; Elefante, A. Unusual CLIPPERS Presentation and Role of MRI Examination in the Proper Diagnostic Assessment: A Case Report. Eur. J. Radiol. Open 2019, 6, 212–214. [Google Scholar] [CrossRef] [PubMed]
- Blaabjerg, M.; Ruprecht, K.; Sinnecker, T.; Kondziella, D.; Niendorf, T.; Kerrn-Jespersen, B.M.; Lindelof, M.; Lassmann, H.; Kristensen, B.W.; Paul, F.; et al. Widespread Inflammation in CLIPPERS Syndrome Indicated by Autopsy and Ultra-High-Field 7T MRI. Neurol. Neuroimmunol. Neuroinflamm. 2016, 3, 226. [Google Scholar] [CrossRef] [PubMed]
- Taieb, G.; Mulero, P.; Psimaras, D.; Van Oosten, B.W.; Seebach, J.D.; Marignier, R.; Pico, F.; Rigau, V.; Ueno, Y.; Duflos, C.; et al. CLIPPERS and Its Mimics: Evaluation of New Criteria for the Diagnosis of CLIPPERS. J. Neurol. Neurosurg. Psychiatry 2019, 90, 1027–1038. [Google Scholar] [CrossRef] [PubMed]
- Horng, S.; Crary, J.; Fabian, M. A Case of SLIPPERS (Supratentorial Lymphocytic Inflammation with Parenchymal Perivascular Enhancement Responsive to Steroids) Presenting with Isolated Cognitive Dysfunction. (P1.336). Neurology 2017, 88, P1.336. [Google Scholar]
- Sudhakar, V.; Gersey, Z.; Polster, S.P.; Mantica, M.; Zenonos, G. Supratentorial Lymphocytic Inflammation with Parenchymal Perivascular Enhancement Responsive to Steroids: A Case Report and Literature Review. Surg. Neurol. Int. 2021, 12, 327. [Google Scholar] [CrossRef] [PubMed]
- Picarelli, H.; Yamaki, V.N.; Casal, Y.R.; de Brito, M.H.; de Lima, L.G.C.A.; Ayres, A.S.; de Oliveira, M.C.B. CLIPPERS With Exclusive Extra Pontine Involvement. Neurol. Neuroimmunol. Neuroinflamm. 2021, 8, 989. [Google Scholar] [CrossRef] [PubMed]
- Vattoth, S.; Aker, L.; Abdelhady, M.; El Beltagi, A.H. Case 302: Supratentorial Lymphocytic Inflammation with Parenchymal Perivascular Enhancement Responsive to Steroids. Radiology 2022, 303, 726–730. [Google Scholar] [CrossRef] [PubMed]
- Al-Chalabi, M.; DelCimmuto, N.R.; Beran, A.; Devarasetty, P.P.; Mhanna, A.; Mahfooz, N.; Sheikh, A. Clinical Characteristics, Management, and Outcomes of CLIPPERS: A Comprehensive Systematic Review of 140 Patients from 100 Studies. Mult. Scler. Relat. Disord. 2022, 68, 104112. [Google Scholar] [CrossRef] [PubMed]
- Fang, B.; McKeon, A.; Hinson, S.R.; Kryzer, T.J.; Pittock, S.J.; Aksamit, A.J.; Lennon, V.A. Autoimmune Glial Fibrillary Acidic Protein Astrocytopathy: A Novel Meningoencephalomyelitis. JAMA Neurol. 2016, 73, 1297–1307. [Google Scholar] [CrossRef] [PubMed]
- Long, Y.; Liang, J.; Xu, H.; Huang, Q.; Yang, J.; Gao, C.; Qiu, W.; Lin, S.; Chen, X. Autoimmune Glial Fibrillary Acidic Protein Astrocytopathy in Chinese Patients: A Retrospective Study. Eur. J. Neurol. 2018, 25, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Adams Waldorf, K.M.; Nelson, J.L. Autoimmune Disease during Pregnancy and the Microchimerism Legacy of Pregnancy. Immunol. Investig. 2008, 37, 631–644. [Google Scholar] [CrossRef] [PubMed]

| (Armand et al., 2015 [3]) (n = 2) | (Horng et al., 2017 [9]) (n = 1) | (Sudhakar et al., 2021 [10]) (n = 1) | (Picarelli et al., 2021 [11]) (n = 1) | (Vattoth et al., 2022 [12]) (n = 1) | |
|---|---|---|---|---|---|
| Age | N/A 1 | 56 | 71 | 39 | 21 |
| Sex | N/A 1 | Male | Male | Female | Male |
| Clinical presentation | Seizures, headache and hemiparesis | Cognitive impairment | Cognitive impairment and hemiparesis | Headache and seizures | Seizure, dizziness and left homonymous hemianopia |
| Location | N/A 1 | Bilateral PVWM lesions, including the amygdala and hippocampus | Right occipital lobe, right precentral gyrus, and multiple small lesions in PVWM | Subcortical and PVWM lesions in the right frontoparietal and insular lobes | Right parieto-occipital subcortical and PVWM, extending to the splenium |
| Follow up of more than 2 years | No | No | No | No | No |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Freua, F.; Mahler, J.V.; Lima, P.L.G.d.S.B.; Neville, I.S.; Portella, L.B.; Marussi, V.H.R.; Lancellotti, C.L.P.; Nobrega, P.R.; Silva, G.D. Supratentorial Lymphocytic Inflammation with Parenchymal Perivascular Enhancement Responsive to Steroids (SLIPPERS)—Does it Really Exist? Brain Sci. 2023, 13, 1191. https://doi.org/10.3390/brainsci13081191
Freua F, Mahler JV, Lima PLGdSB, Neville IS, Portella LB, Marussi VHR, Lancellotti CLP, Nobrega PR, Silva GD. Supratentorial Lymphocytic Inflammation with Parenchymal Perivascular Enhancement Responsive to Steroids (SLIPPERS)—Does it Really Exist? Brain Sciences. 2023; 13(8):1191. https://doi.org/10.3390/brainsci13081191
Chicago/Turabian StyleFreua, Fernando, João Vitor Mahler, Pedro Lucas Grangeiro de Sá Barreto Lima, Iuri Santana Neville, Leonardo Barreira Portella, Victor Hugo Rocha Marussi, Carmen Lucia Penteado Lancellotti, Paulo Ribeiro Nobrega, and Guilherme Diogo Silva. 2023. "Supratentorial Lymphocytic Inflammation with Parenchymal Perivascular Enhancement Responsive to Steroids (SLIPPERS)—Does it Really Exist?" Brain Sciences 13, no. 8: 1191. https://doi.org/10.3390/brainsci13081191
APA StyleFreua, F., Mahler, J. V., Lima, P. L. G. d. S. B., Neville, I. S., Portella, L. B., Marussi, V. H. R., Lancellotti, C. L. P., Nobrega, P. R., & Silva, G. D. (2023). Supratentorial Lymphocytic Inflammation with Parenchymal Perivascular Enhancement Responsive to Steroids (SLIPPERS)—Does it Really Exist? Brain Sciences, 13(8), 1191. https://doi.org/10.3390/brainsci13081191





