Persistent Non-Suicidal Self-Injury and Suicidality in Referred Adolescents: A Longitudinal Study Exploring the Role of Cyclothymic Temperament
Abstract
1. Introduction
2. Materials and Methods
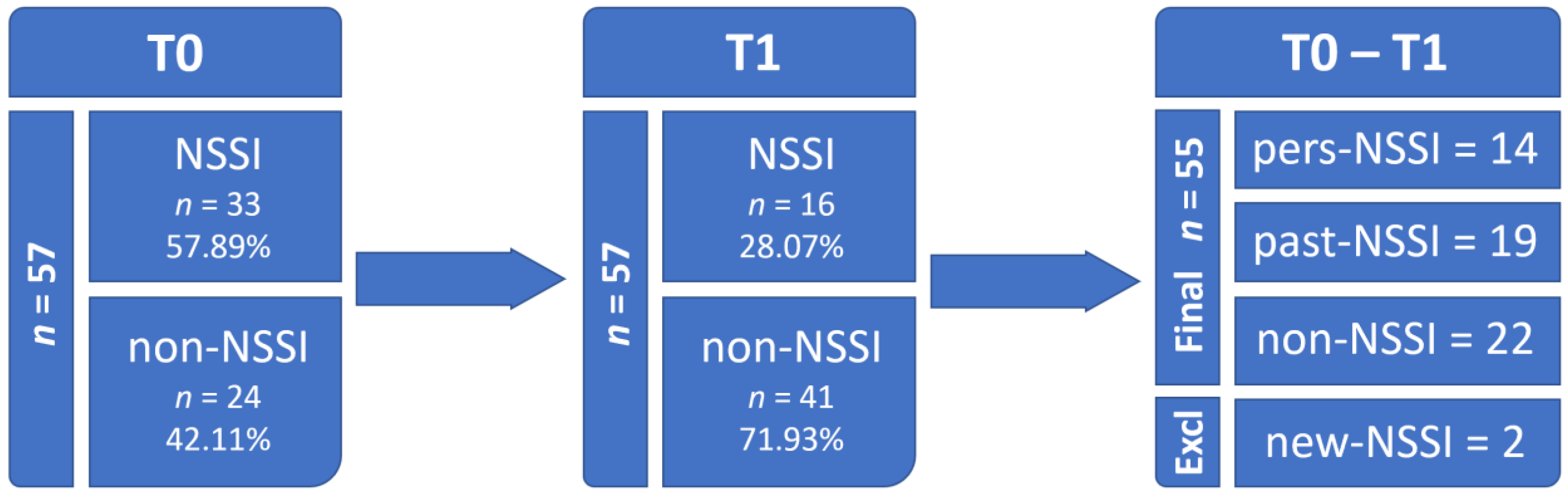
2.1. Participants and Study Design
2.2. Measures
2.3. Statistics
3. Results
3.1. Clinical Assessment at T1
3.2. Longitudinal Assessment
3.3. Suicidal Ideation and Behavior
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nock, M.K. Why do people hurt themselves? New insights into the nature and functions of self-injury. Curr. Dir. Psychol. Sci. 2009, 18, 78–83. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5-TR, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2022. [Google Scholar]
- McManus, S.; Gunnell, D.; Cooper, C.; Bebbington, P.E.; Howard, L.M.; Brugha, T.; Jenkins, R.; Hassiotis, A.; Weich, S.; Appleby, L. Prevalence of non-suicidal self-harm and service contact in England, 2000–2014: Repeated cross-sectional surveys of the general population. Lancet Psychiatry 2019, 6, 573–581. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; CBS Publishers: New Delhi, India, 2013. [Google Scholar]
- World Health Organization. Preventing Suicide: A Global Imperative. World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Klonsky, E.D.; May, A.M.; Glenn, C.R. The relationship between nonsuicidal self-injury and attempted suicide: Converging evidence from four samples. J. Abnorm. Psychol. 2013, 122, 231–237. [Google Scholar] [CrossRef]
- Kapur, N.; Cooper, J.; O’Connor, R.C.; Hawton, K. Non-suicidal self-injury v. attempted suicide: New diagnosis or false dichotomy? Br. J. Psychiatry 2013, 202, 326–328. [Google Scholar] [CrossRef] [PubMed]
- Scott, L.N.; Pilkonis, P.A.; Hipwell, A.E.; Keenan, K.; Stepp, S.D. Non-suicidal self-injury and suicidal ideation as predictors of suicide attempts in adolescent girls: A multi-wave prospective study. Compr. Psychiatry 2015, 58, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Cavanagh, J.T.O.; Carson, A.J.; Sharpe, M.; Lawrie, S.M. Psychological autopsy studies of suicide: A systematic review. Psychol. Med. 2003, 33, 395–405. [Google Scholar] [CrossRef] [PubMed]
- Hamza, C.A.; Stewart, S.L.; Willoughby, T. Examining the link between nonsuicidal self-injury and suicidal behavior: A review of the literature and an integrated model. Clin. Psychol. Rev. 2012, 32, 482–495. [Google Scholar] [CrossRef] [PubMed]
- Victor, S.E.; Klonsky, E.D. Correlates of suicide attempts among self-injurers: A meta-analysis. Clin. Psychol. Rev. 2014, 34, 282–297. [Google Scholar] [CrossRef] [PubMed]
- Lynam, D.R.; Miller, J.D.; Miller, D.J.; Bornovalova, M.A.; Lejuez, C.W. Testing the relations between impulsivity-related traits, suicidality, and nonsuicidal self-injury: A test of the incremental validity of the UPPS model. Personal. Disord. 2011, 2, 151–160. [Google Scholar] [CrossRef]
- Nock, M.K.; Joiner, T.E.J.; Gordon, K.H.; Lloyd-Richardson, E.; Prinstein, M.J. Non-suicidal self-injury among adolescents: Diagnostic correlates and relation to suicide attempts. Psychiatry Res. 2006, 144, 65–72. [Google Scholar] [CrossRef]
- Masi, G.; Lupetti, I.; D’Acunto, G.; Milone, A.; Fabiani, D.; Madonia, U.; Berloffa, S.; Lenzi, F.; Mucci, M. A Comparison between Severe Suicidality and Nonsuicidal Self-Injury Behaviors in Bipolar Adolescents Referred to a Psychiatric Emergency Unit. Brain Sci. 2021, 11, 790. [Google Scholar] [CrossRef]
- MacPherson, H.A.; Weinstein, S.M.; West, A.E. Non-Suicidal Self-Injury in Pediatric Bipolar Disorder: Clinical Correlates and Impact on Psychosocial Treatment Outcomes. J. Abnorm. Child Psychol. 2018, 46, 857–870. [Google Scholar] [CrossRef] [PubMed]
- Masi, G.; Milone, A.; Montesanto, A.R.; Valente, E.; Pisano, S. Non suicidal self-injury in referred adolescents with mood disorders and its association with cyclothymic-hypersensitive temperament. J. Affect. Disord. 2018, 227, 477–482. [Google Scholar] [CrossRef] [PubMed]
- Serra, G.; De Crescenzo, F.; Maisto, F.; Galante, J.R.; Iannoni, M.E.; Trasolini, M.; Maglio, G.; Tondo, L.; Baldessarini, R.J.; Vicari, S. Suicidal behavior in juvenile bipolar disorder and major depressive disorder patients: Systematic review and meta-analysis. J. Affect. Disord. 2022, 311, 572–581. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, P.; Kelvin, R.; Roberts, C.; Dubicka, B.; Goodyer, I. Clinical and psychosocial predictors of suicide attempts and nonsuicidal self-injury in the Adolescent Depression Antidepressants and Psychotherapy Trial (ADAPT). Am. J. Psychiatry 2011, 168, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Asarnow, J.R.; Porta, G.; Spirito, A.; Emslie, G.; Clarke, G.; Wagner, K.D.; Vitiello, B.; Keller, M.; Birmaher, B.; McCracken, J.; et al. Suicide attempts and nonsuicidal self-injury in the treatment of resistant depression in adolescents: Findings from the TORDIA study. J. Am. Acad. Child Adolesc. Psychiatry 2011, 50, 772–781. [Google Scholar] [CrossRef]
- Chesin, M.S.; Galfavy, H.; Sonmez, C.C.; Wong, A.; Oquendo, M.A.; Mann, J.J.; Stanley, B. Nonsuicidal Self-Injury Is Predictive of Suicide Attempts among Individuals with Mood Disorders. Suicide Life Threat. Behav. 2017, 47, 567–579. [Google Scholar] [CrossRef]
- Yen, S.; Kuehn, K.; Melvin, C.; Weinstock, L.M.; Andover, M.S.; Selby, E.A.; Solomon, J.B.; Spirito, A. Predicting Persistence of Nonsuicidal Self-Injury in Suicidal Adolescents. Suicide Life Threat. Behav. 2016, 46, 13–22. [Google Scholar] [CrossRef]
- Perugi, G.; Hantouche, E.; Vannucchi, G.; Pinto, O. Cyclothymia reloaded: A reappraisal of the most misconceived affective disorder. J. Affect. Disord. 2015, 183, 119–133. [Google Scholar] [CrossRef]
- Perugi, G.; Hantouche, E.; Vannucchi, G. Diagnosis and Treatment of Cyclothymia: The “Primacy” of Temperament. Curr. Neuropharmacol. 2017, 15, 372–379. [Google Scholar] [CrossRef]
- Kochman, F.J.; Hantouche, E.G.; Ferrari, P.; Lancrenon, S.; Bayart, D.; Akiskal, H.S. Cyclothymic temperament as a prospective predictor of bipolarity and suicidality in children and adolescents with major depressive disorder. J. Affect. Disord. 2005, 85, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, J.; Birmaher, B.; Brent, D.; Rao, U.; Flynn, C.; Moreci, P.; Williamson, D.; Ryan, N. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 980–988. [Google Scholar] [CrossRef] [PubMed]
- Achenbach, T.; Rescorla, L. Manual for the ASEBA School-Age Forms and Profiles: An Integrated System of Multi-Informant Assessment; University of Vermont, Research Center for Children, Youth, & Families: Burlington, VT, USA, 2001. [Google Scholar]
- Doelitzsch, C.; Koelch, M.; Fegert, J.M.; Schmeck, K.; Schmid, M. Ability of the Child Behavior Checklist-Dysregulation Profile and the Youth Self Report-Dysregulation Profile to identify serious psychopathology and association with correlated problems in high-risk children and adolescents. J. Affect. Disord. 2016, 205, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Holtmann, M.; Buchmann, A.F.; Esser, G.; Schmidt, M.H.; Banaschewski, T.; Laucht, M. The Child Behavior Checklist-Dysregulation Profile predicts substance use, suicidality, and functional impairment: A longitudinal analysis. J. Child Psychol. Psychiatry 2011, 52, 139–147. [Google Scholar] [CrossRef]
- Pisano, S.; Senese, V.P.; Bravaccio, C.; Santangelo, P.; Milone, A.; Masi, G.; Catone, G. Cyclothymic-hypersensitive temperament in youths: Refining the structure, the way of assessment and the clinical significance in the youth population. J. Affect. Disord. 2020, 271, 272–278. [Google Scholar] [CrossRef] [PubMed]
- Akiskal, H.S.; Akiskal, K.K.; Haykal, R.F.; Manning, J.S.; Connor, P.D. TEMPS-A: Progress towards validation of a self-rated clinical version of the Temperament Evaluation of the Memphis, Pisa, Paris, and San Diego Autoquestionnaire. J. Affect. Disord. 2005, 85, 3–16. [Google Scholar] [CrossRef]
- Posner, K.; Brown, G.K.; Stanley, B.; Brent, D.A.; Yershova, K.V.; Oquendo, M.A.; Currier, G.W.; Melvin, G.A.; Greenhill, L.; Shen, S.; et al. The Columbia-suicide severity rating scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am. J. Psychiatry 2011, 168, 1266–1277. [Google Scholar] [CrossRef]
- Lindh, Å.U.; Dahlin, M.; Beckman, K.; Strömsten, L.; Jokinen, J.; Wiktorsson, S.; Renberg, E.S.; Waern, M.; Runeson, B. A Comparison of Suicide Risk Scales in Predicting Repeat Suicide Attempt and Suicide: A Clinical Cohort Study. J. Clin. Psychiatry 2019, 80, 20485. [Google Scholar] [CrossRef]
- Andrews, T.; Martin, G.; Hasking, P.; Page, A. Predictors of continuation and cessation of nonsuicidal self-injury. J. Adolesc. Health 2013, 53, 40–46. [Google Scholar] [CrossRef]
- Eggart, V.; Cordier, S.; Hasan, A.; Wagner, E. Psychotropic drugs for the treatment of non-suicidal self-injury in children and adolescents: A systematic review and meta-analysis. Eur. Arch. Psychiatry Clin. Neurosci. 2022, 272, 1559–1568. [Google Scholar] [CrossRef]
- Brickman, L.J.; Ammerman, B.A.; Look, A.E.; Berman, M.E.; McCloskey, M.S. The relationship between non-suicidal self-injury and borderline personality disorder symptoms in a college sample. Bord. Personal. Disord. Emot. Dysregulation 2014, 1, 14. [Google Scholar] [CrossRef]
- Santangelo, P.S.; Koenig, J.; Funke, V.; Parzer, P.; Resch, F.; Ebner-Priemer, U.W.; Kaess, M. Ecological Momentary Assessment of Affective and Interpersonal Instability in Adolescent Non-Suicidal Self-Injury. J. Abnorm. Child Psychol. 2017, 45, 1429–1438. [Google Scholar] [CrossRef] [PubMed]
- Tragesser, S.L.; Solhan, M.; Schwartz-Mette, R.; Trull, T.J. The role of affective instability and impulsivity in predicting future BPD features. J. Pers. Disord. 2007, 21, 603–614. [Google Scholar] [CrossRef] [PubMed]
- Mehlum, L.; Tørmoen, A.J.; Ramberg, M.; Haga, E.; Diep, L.M.; Laberg, S.; Larsson, B.S.; Stanley, B.H.; Miller, A.L.; Sund, A.M.; et al. Dialectical behavior therapy for adolescents with repeated suicidal and self-harming behavior: A randomized trial. J. Am. Acad. Child Adolesc. Psychiatry 2014, 53, 1082–1091. [Google Scholar] [CrossRef] [PubMed]
- Sesso, G.; Milone, A.; Drago, F.; Viglione, V.; Berloffa, S.; Boldrini, S.; Loriaux, N.; Valente, E.; Molesti, A.; Placini, F.; et al. A novel multidimensional questionnaire for the assessment of emotional dysregulation in adolescents: Reactivity, Intensity, Polarity and Stability questionnaire–youth version (RIPoSt–Y). J. Affect. Disord. 2021, 291, 359–367. [Google Scholar] [CrossRef]
- Masi, G.; Sesso, G.; Pfanner, C.; Valente, E.; Molesti, A.; Placini, F.; Boldrini, S.; Loriaux, N.; Drago, F.; Montesanto, A.; et al. An exploratory study of emotional dysregulation dimensions in youth with attention deficit hyperactivity disorder and/or bipolar spectrum disorders. Front. Psychiatry 2021, 12, 619037. [Google Scholar] [CrossRef] [PubMed]
| Variables | pers-NSSI | past-NSSI | non-NSSI | Statistics | p-Value | Post-Hoc Comparisons |
|---|---|---|---|---|---|---|
| CHT cut-off a | 9 (75.00) | 10 (55.56) | 4 (22.22) | 8.7096 | 0.0128 * | pers-NSSI > past-NSSI > non-NSSI |
| CHT score b | 17.17 ± 4.41 | 12.71 ± 7.35 | 8.89 ± 5.21 | 7.0831 | 0.0022 * | pers-NSSI > non-NSSI |
| SCID—avoiding a | 5 (45.45) | 5 (41.67) | 5 (27.78) | 1.1084 | 0.5517 | |
| SCID—dependent a | 2 (18.18) | 3 (25.00) | 2 (11.11) | 0.9940 | 0.5918 | |
| SCID—obsessive compulsive a | 8 (66.67) | 8 (66.67) | 9 (47.37) | 1.6228 | 0.4442 | |
| SCID—oppositional a | 9 (81.82) | 10 (83.33) | 13 (72.22) | 0.6435 | 0.7992 | |
| SCID—depressive a | 6 (54.55) | 6 (50.00) | 6 (33.33) | 1.5034 | 0.5214 | |
| SCID—paranoid a | 7 (63.64) | 8 (66.67) | 6 (33.33) | 4.1296 | 0.1268 | |
| SCID—schizotypal a | 4 (36.36) | 6 (50.00) | 4 (22.22) | 2.5035 | 0.2647 | |
| SCID—schizoid a | 2 (18.18) | 3 (25.00) | 0 (0.00) | 4.7057 | 0.0762 | |
| SCID—histrionic a | 0 (0.00) | 2 (16.67) | 1 (5.56) | 2.4976 | 0.4470 | |
| SCID—narcissistic a | 2 (18.18) | 6 (50.00) | 7 (38.89) | 2.5778 | 0.2979 | |
| SCID—borderline a | 9 (75.00) | 12 (100.00) | 11 (57.89) | 6.8522 | 0.0292 * | past-NSSI > pers-NSSI > non-NSSI |
| SCID—antisocial a | 4 (36.36) | 6 (50.00) | 5 (27.78) | 1.5329 | 0.4576 | |
| K-SADS-PL—depression a | 11 (78.57) | 16 (88.89) | 16 (94.12) | 1.7608 | 0.4794 | |
| K-SADS-PL—mania a | 5 (35.71) | 11 (61.11) | 5 (29.41) | 3.9956 | 0.1356 | |
| K-SADS-PL—panic disorder a | 3 (23.08) | 6 (42.86) | 2 (11.76) | 3.9948 | 0.1574 | |
| K-SADS-PL—separation anxiety a | 2 (15.38) | 1 (6.67) | 1 (5.88) | 0.9585 | 0.6663 | |
| K-SADS-PL—generalized anxiety a | 9 (69.23) | 7 (46.67) | 6 (35.29) | 3.4398 | 0.1791 | |
| K-SADS-PL—social anxiety a | 4 (30.77) | 1 (6.67) | 3 (17.65) | 2.7681 | 0.2984 | |
| K-SADS-PL—specific phobias a | 4 (30.77) | 1 (6.67) | 3 (17.65) | 2.7681 | 0.2984 | |
| K-SADS-PL—obsessive compulsive a | 0 (0.00) | 0 (0.00) | 2 (11.76) | 3.4473 | 0.3222 | |
| K-SADS-PL—ADHD a | 3 (23.08) | 5 (33.33) | 6 (35.29) | 0.5649 | 0.7829 | |
| K-SADS-PL—oppositional defiant a | 4 (30.77) | 4 (26.67) | 8 (47.06) | 1.6290 | 0.4973 | |
| K-SADS-PL—conduct disorder a | 2 (15.38) | 2 (13.33) | 0 (0.00) | 2.7017 | 0.2379 | |
| K-SADS-PL—eating disorder a | 1 (7.69) | 2 (13.33) | 2 (11.76) | 0.2362 | 1.0000 | |
| K-SADS-PL—psychosis a | 1 (7.69) | 0 (0.00) | 0 (0.00) | 2.5175 | 0.2889 | |
| CGAS b | 46.83 ± 8.86 | 50.19 ± 9.72 | 57.64 ± 6.73 | 5.5405 | 0.0076 * | non-NSSI > past-NSSI and pers-NSSI |
| C-SSRS—ideation b | 1.92 ± 2.11 | 1.83 ± 1.89 | 0.38 ± 0.92 | 5.1881 | 0.0091 * | pers-NSSI and past-NSSI > non-NSSI |
| C-SSRS—behavior b | 1.33 ± 1.87 | 0.56 ± 1.29 | 0.05 ± 0.22 | 4.4579 | 0.0168 * | pers-NSSI > non-NSSI |
| CBCL—anxious/depressed b | 71.00 ± 11.47 | 67.11 ± 12.30 | 61.67 ± 13.20 | 2.1886 | 0.1234 | |
| CBCL—withdrawn/depressed b | 66.36 ± 13.43 | 64.89 ± 13.83 | 62.48 ± 11.91 | 0.3646 | 0.6964 | |
| CBCL—somatic problems b | 65.64 ± 9.64 | 62.56 ± 8.13 | 57.67 ± 10.12 | 2.9333 | 0.0630 | |
| CBCL—social problems b | 62.00 ± 11.75 | 62.61 ± 9.99 | 56.57 ± 8.35 | 2.1727 | 0.1252 | |
| CBCL—thought problems b | 69.64 ± 12.40 | 61.28 ± 7.31 | 59.76 ± 10.05 | 3.9159 | 0.0267 * | pers-NSSI > non-NSSI |
| CBCL—attentive problems b | 62.55 ± 5.07 | 65.50 ± 14.70 | 60.33 ± 9.50 | 1.0611 | 0.3542 | |
| CBCL—antisocial behaviors b | 62.36 ± 5.37 | 58.17 ± 6.96 | 59.48 ± 9.31 | 1.0010 | 0.3752 | |
| CBCL—aggressive behaviors b | 59.55 ± 7.24 | 59.44 ± 8.85 | 61.33 ± 9.80 | 0.2600 | 0.7721 | |
| CBCL—dysregulation profile b | 193.09 ± 19.71 | 191.44 ± 29.48 | 183.33 ± 28.59 | 0.6365 | 0.5337 | |
| CBCL—internalizing problems b | 69.91 ± 11.04 | 64.50 ± 14.99 | 49.43 ± 14.20 | 2.1177 | 0.1316 | |
| CBCL—externalizing problems b | 61.45 ± 7.16 | 57.56 ± 10.33 | 58.86 ± 12.50 | 0.4491 | 0.6409 | |
| CBCL—total problems b | 67.00 ± 8.80 | 62.56 ± 12.08 | 58.62 ± 14.06 | 1.6946 | 0.1947 |
| Variables | pers-NSSI | past-NSSI | non-NSSI | Statistics | p-Value | Post-Hoc Comparisons |
|---|---|---|---|---|---|---|
| Gender (boys) a | 1 (7.14) | 2 (10.53) | 13 (59.09) | 16.0423 | 0.0004 * | non-NSSI > past-NSSI > pers-NSSI |
| Age b | 14.73 ± 1.71 | 15.19 ± 1.28 | 14.09 ± 2.05 | 0.0329 | 0.0550 | |
| Medications a | 12 (100.00) | 15 (83.33) | 14 (73.68) | 3.7308 | 0.1593 | |
| Mood stabilizers a | 12 (100.00) | 15 (83.33) | 10 (52.63) | 9.8656 | 0.0065 * | pers-NSSI > past-NSSI > non-NSSI |
| SSRI antidepressants a | 0 (0.00) | 2 (11.11) | 5 (26.32) | 4.3938 | 0.1395 | |
| Antipsychotics a | 2 (16.67) | 4 (22.22) | 4 (21.05) | 0.1447 | 1.0000 | |
| Individual psychotherapy a | 10 (83.33) | 18 (100.00) | 13 (68.42) | 6.7488 | 0.0204 * | past-NSSI > pers-NSSI > non-NSSI |
| Group psychotherapy a | 4 (33.33) | 5 (27.78) | 5 (26.32) | 0.1863 | 0.9243 | |
| CGAS b | 38.71 ± 2.95 | 39.37 ± 5.59 | 41.41 ± 6.84 | −0.0653 | 0.2612 | |
| CHT cut-off a | 10 (83.33) | 10 (55.56) | 10 (52.63) | 3.3054 | 0.2241 | |
| CHT score b | 16.00 ± 7.14 | 12.39 ± 7.08 | 13.53 ± 5.91 | −0.0251 | 0.6299 | |
| K-SADS-PL—depression a | 11 (78.57) | 19 (100.00) | 16 (94.12) | 5.1859 | 0.0584 | |
| K-SADS-PL—mania a | 6 (42.86) | 10 (52.63) | 7 (41.18) | 0.5513 | 0.7591 | |
| K-SADS-PL—panic disorder a | 4 (28.57) | 5 (29.41) | 2 (11.76) | 1.8563 | 0.4702 | |
| K-SADS-PL—separation anxiety a | 6 (42.86) | 3 (17.65) | 3 (17.65) | 3.3613 | 0.2392 | |
| K-SADS-PL—generalized anxiety a | 9 (64.29) | 9 (52.94) | 8 (47.06) | 0.9337 | 0.6270 | |
| K-SADS-PL—social anxiety a | 5 (35.71) | 4 (23.53) | 4 (23.53) | 0.7456 | 0.7749 | |
| K-SADS-PL—specific phobias a | 3 (21.43) | 1 (5.88) | 3 (17.65) | 1.6879 | 0.4690 | |
| K-SADS-PL—obsessive compulsive a | 1 (7.14) | 0 (0.00) | 4 (23.53) | 5.2700 | 0.0672 | |
| K-SADS-PL—tics a | 0 (0.00) | 0 (0.00) | 1 (5.88) | 1.8623 | 1.0000 | |
| K-SADS-PL—ADHD a | 5 (35.71) | 6 (35.29) | 5 (29.41) | 0.1828 | 1.0000 | |
| K-SADS-PL—oppositional defiant a | 7 (50.00) | 7 (41.18) | 8 (47.06) | 0.2567 | 0.8796 | |
| K-SADS-PL—conduct disorder a | 4 (28.57) | 2 (11.76) | 0 (0.00) | 5.7431 | 0.0613 | |
| K-SADS-PL—elimination disorder a | 1 (7.14) | 1 (5.88) | 0 (0.00) | 1.1750 | 0.7438 | |
| K-SADS-PL—eating disorder a | 0 (0.00) | 3 (17.65) | 1 (5.88) | 3.3369 | 0.3099 | |
| K-SADS-PL—psychosis a | 2 (14.29) | 1 (5.88) | 1 (5.88) | 0.9167 | 0.6673 | |
| CBCL—anxious/depressed b | 69.71 ± 10.66 | 66.00 ± 11.58 | 71.86 ± 8.36 | −0.0596 | 0.0737 | |
| CBCL—withdrawn/depressed b | 70.07 ± 12.29 | 66.00 ± 11.78 | 71.86 ± 12.23 | −0.0436 | 0.1256 | |
| CBCL—somatic problems b | 65.29 ± 9.32 | 62.89 ± 11.66 | 66.77 ± 8.82 | -0.0408 | 0.2148 | |
| CBCL—social problems b | 64.00 ± 10.15 | 65.11 ±9.76 | 65.95 ± 9.49 | −0.0094 | 0.7763 | |
| CBCL—thought problems b | 69.57 ± 9.77 | 64.37 ± 9.04 | 66.95 ± 9.66 | −0.0319 | 0.3665 | |
| CBCL—attentive problems b | 63.14 ± 5.96 | 67.21 ± 11.59 | 68.09 ± 9.57 | −0.0093 | 0.7736 | |
| CBCL—antisocial behaviors b | 61.86 ± 8.22 | 63.26 ± 10.62 | 63.95 ± 6.54 | −0.0099 | 0.7915 | |
| CBCL—aggressive behaviors b | 60.57 ± 7.44 | 64.42 ± 10.75 | 67.14 ± 10.31 | −0.0378 | 0.2509 | |
| CBCL—dysregulation profile b | 189.79 ± 22.02 | 194.68 ± 23.18 | 208.59 ± 21.16 | −0.0301 | 0.0562 | |
| CBCL—internalizing problems b | 70.07 ± 8.90 | 65.89 ± 11.84 | 70.73 ± 8.60 | −0.0506 | 0.1384 | |
| CBCL—externalizing problems b | 61.36 ± 8.28 | 64.00 ± 10.24 | 66.36 ± 7.72 | −0.0335 | 0.3754 | |
| CBCL—total problems b | 67.71 ± 6.16 | 67.84 ± 8.36 | 69.86 ± 7.21 | −0.0410 | 0.3684 |
| CGAS | |||
|---|---|---|---|
| Model Variables | Statistics | p-Value | Effect Size |
| NSSI group | 6.3990 | 0.0040 * | 0.2570 |
| Time (T0 − T1) | 100.1830 | 0.0000 * | 0.7300 |
| NSSI group × Time | 4.5800 | 0.0170 * | 0.1980 |
| post-hoc comparisons | statistics | p-value | effect size |
| non-NSSI × (T0 versus T1) | −8.6170 | 0.0000 * | −3.3730 |
| past-NSSI × (T0 versus T1) | −6.4662 | 0.0000 * | −1.3648 |
| pers-NSSI × (T0 versus T1) | −3.1033 | 0.0100 * | −1.2296 |
| T0 × (non-NSSI versus past-NSSI) | 0.7439 | 1.0000 | 0.2381 |
| T0 × (non-NSSI versus pers-NSSI) | 1.3073 | 0.6030 | 0.4303 |
| T0 × (past-NSSI versus pers-NSSI) | 0.4347 | 1.0000 | 0.1464 |
| T1 × (non-NSSI versus past-NSSI) | 3.1816 | 0.0120 * | 1.1610 |
| T1 × (non-NSSI versus pers-NSSI) | 4.2119 | 0.0020 * | 1.7195 |
| T1 × (past-NSSI versus pers-NSSI) | 0.9508 | 1.0000 | 0.3607 |
| CHT score | |||
| model variables | statistics | p-value | effect size |
| NSSI group | 4.8320 | 0.0130 * | 0.2030 |
| Time (T0 − T1) | 3.8270 | 0.0580 | 0.0910 |
| NSSI group × Time | 1.8240 | 0.1750 | 0.0880 |
| post-hoc comparisons | statistics | p-value | effect size |
| non-NSSI versus past-NSSI | −0.9734 | 1.0000 | −0.2356 |
| non-NSSI versus pers-NSSI | −5.0866 | 0.0000 * | −1.3651 |
| past-NSSI versus pers-NSSI | −3.5744 | 0.0020 * | −0.9227 |
| CBCL dysregulation profile | |||
| model variables | statistics | p-value | effect size |
| NSSI group | 0.3050 | 0.7390 | 0.0130 |
| Time (T0 − T1) | 3.5030 | 0.0680 | 0.0720 |
| NSSI group × Time | 4.0360 | 0.0240 * | 0.1520 |
| post-hoc comparisons | statistics | p-value | effect size |
| non-NSSI × (T0 versus T1) | 4.1009 | 0.0006 * | 1.0043 |
| past-NSSI × (T0 versus T1) | 0.0579 | 0.9550 | 0.0213 |
| pers-NSSI × (T0 versus T1) | −0.0179 | 0.9860 | 0.0772 |
| T0 × (non-NSSI versus past-NSSI) | 2.5986 | 0.0400 * | 0.8232 |
| T0 × (non-NSSI versus pers-NSSI) | 2.2884 | 0.0880 | 0.7756 |
| T0 × (past-NSSI versus pers-NSSI) | −0.3241 | 1.0000 | −0.1163 |
| T1 × (non-NSSI versus past-NSSI) | −0.8127 | 1.0000 | −0.2660 |
| T1 × (non-NSSI versus pers-NSSI) | −1.0043 | 0.9750 | −0.3637 |
| T1 × (past-NSSI versus pers-NSSI) | −0.1244 | 1.0000 | −0.0471 |
| CBCL internalizing problems | |||
| model variables | statistics | p-value | effect size |
| NSSI group | 0.4620 | 0.6340 | 0.0220 |
| Time (T0 − T1) | 2.5400 | 0.1190 | 0.0580 |
| NSSI group × Time | 5.7780 | 0.0060 * | 0.2200 |
| post-hoc comparisons | statistics | p-value | effect size |
| non-NSSI × (T0 versus T1) | 3.8196 | 0.0010 * | 1.0833 |
| past-NSSI × (T0 versus T1) | −0.1167 | 0.9090 | −0.1130 |
| pers-NSSI × (T0 versus T1) | −0.6452 | 0.5370 | −0.2440 |
| T0 × (non-NSSI versus past-NSSI) | 1.9596 | 0.1800 | 0.6555 |
| T0 × (non-NSSI versus pers-NSSI) | 1.4972 | 0.4500 | 0.5606 |
| T0 × (past-NSSI versus pers-NSSI) | −0.3681 | 1.0000 | −0.1369 |
| T1 × (non-NSSI versus past-NSSI) | −1.9264 | 0.1890 | −0.6438 |
| T1 × (non-NSSI versus pers-NSSI) | −2.4964 | 0.0580 | −0.8804 |
| T1 × (past-NSSI versus pers-NSSI) | −0.5560 | 1.0000 | −0.2175 |
| CBCL externalizing problems | |||
| model variables | statistics | p-value | effect size |
| NSSI group | 1.0640 | 0.3530 | 0.0440 |
| Time (T0 − T1) | 5.1860 | 0.0270 * | 0.1010 |
| NSSI group × Time | 2.9150 | 0.0640 | 0.1120 |
| post-hoc comparisons | statistics | p-value | effect size |
| T0 versus T1 | 2.8798 | 0.0060 * | 0.5447 |
| C-SSRS—Ideation | |||
|---|---|---|---|
| Model Variables | F Stat | p-Value | Post-Hoc Comparisons |
| NSSI group | 5.0392 | 0.0105 * | pers-NSSI > non-NSSI; past-NSSI > non-NSSI |
| Age | 0.6217 | 0.4344 | |
| Gender | 0.0007 | 0.9792 | |
| C-SSRS—behavior | |||
| model variables | F stat | p-value | post-hoc comparisons |
| NSSI group | 4.3919 | 0.0180 * | pers-NSSI > non-NSSI |
| Age | 1.1326 | 0.2928 | |
| Gender | 0.1572 | 0.6936 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Masi, G.; Pisano, S.; Sesso, G.; Mazzullo, C.; Berloffa, S.; Fantozzi, P.; Narzisi, A.; Placini, F.; Valente, E.; Viglione, V.; et al. Persistent Non-Suicidal Self-Injury and Suicidality in Referred Adolescents: A Longitudinal Study Exploring the Role of Cyclothymic Temperament. Brain Sci. 2023, 13, 755. https://doi.org/10.3390/brainsci13050755
Masi G, Pisano S, Sesso G, Mazzullo C, Berloffa S, Fantozzi P, Narzisi A, Placini F, Valente E, Viglione V, et al. Persistent Non-Suicidal Self-Injury and Suicidality in Referred Adolescents: A Longitudinal Study Exploring the Role of Cyclothymic Temperament. Brain Sciences. 2023; 13(5):755. https://doi.org/10.3390/brainsci13050755
Chicago/Turabian StyleMasi, Gabriele, Simone Pisano, Gianluca Sesso, Cristina Mazzullo, Stefano Berloffa, Pamela Fantozzi, Antonio Narzisi, Francesca Placini, Elena Valente, Valentina Viglione, and et al. 2023. "Persistent Non-Suicidal Self-Injury and Suicidality in Referred Adolescents: A Longitudinal Study Exploring the Role of Cyclothymic Temperament" Brain Sciences 13, no. 5: 755. https://doi.org/10.3390/brainsci13050755
APA StyleMasi, G., Pisano, S., Sesso, G., Mazzullo, C., Berloffa, S., Fantozzi, P., Narzisi, A., Placini, F., Valente, E., Viglione, V., & Milone, A. (2023). Persistent Non-Suicidal Self-Injury and Suicidality in Referred Adolescents: A Longitudinal Study Exploring the Role of Cyclothymic Temperament. Brain Sciences, 13(5), 755. https://doi.org/10.3390/brainsci13050755






