Natalizumab Treatment for Relapsing Multiple Sclerosis Stabilises Normal-Appearing White Matter Microstructure: A One-Year Prospective Ultra-High-Field Quantitative Imaging Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients and Study Design
2.2. MRI Data Acquisition
- (1)
- To produce T1 maps, seven 3D inversion recovery TFE (IR-TFE, or MPRAGE) images were acquired across the deep grey matter at a range of inversion times (150, 300, 500, 800, 1200, 1800, 2500 ms). The acquisition parameters were as follows: TE = 3.2 ms; TR = 6.9 ms; flip angle of the TFE readout pulse = 8°; TFE factor per inversion = 240; shot-to-shot interval = 8 s; spatial resolution = 1.25 × 1.25 × 1.25 mm3; field of view = 200 × 200 × 72.5 mm3; scan time per TI = 2 min. An adiabatic, phase-modulated pulse with a bandwidth of 1.6 kHz and duration of 13 ms was used for inversion [21].
- (2)
- MT-weighted images were acquired using a 3D MT-prepared turbo field echo (MT-TFE) sequence (0.86 × 0.86 × 1.5 mm voxel size). Three acquisitions were made: one with no presaturation, one with presaturation −1.05 kHz off-resonance from water (MTRNOE: sensitive to MT and NOEs), and one with presaturation +1.05 kHz off-resonance (MTRAPT: sensitivity to MT and to a lesser extent to amide proton transfer) (total scan time = 8 min 22 s for the three acquisitions, further details can be found in a prior publication [14]).
- (3)
- High-resolution (0.6 × 0.6 × 0.6 mm3) MPRAGE (T1-weighted) anatomical images were acquired prior to and post injection of gadolinium (0.1 millilitre Gadovist per kg body weight). Details of the acquisition were as follows: TE = 5.9 ms, TR = 15 ms, shot-to-shot intervals 3000 ms, turbo field echo (TFE) factor = 148, inversion time = 1050 ms, flip angle = 8°, spatial resolution 0.6 mm isotropic, matrix size 320, pseudo-radial k-space sampling for a total acquisition time of 11 min 40 s.
2.3. Data Analysis and Post-Processing
2.4. Statistical Analysis
3. Results
3.1. Participants and Clinical Course of MS
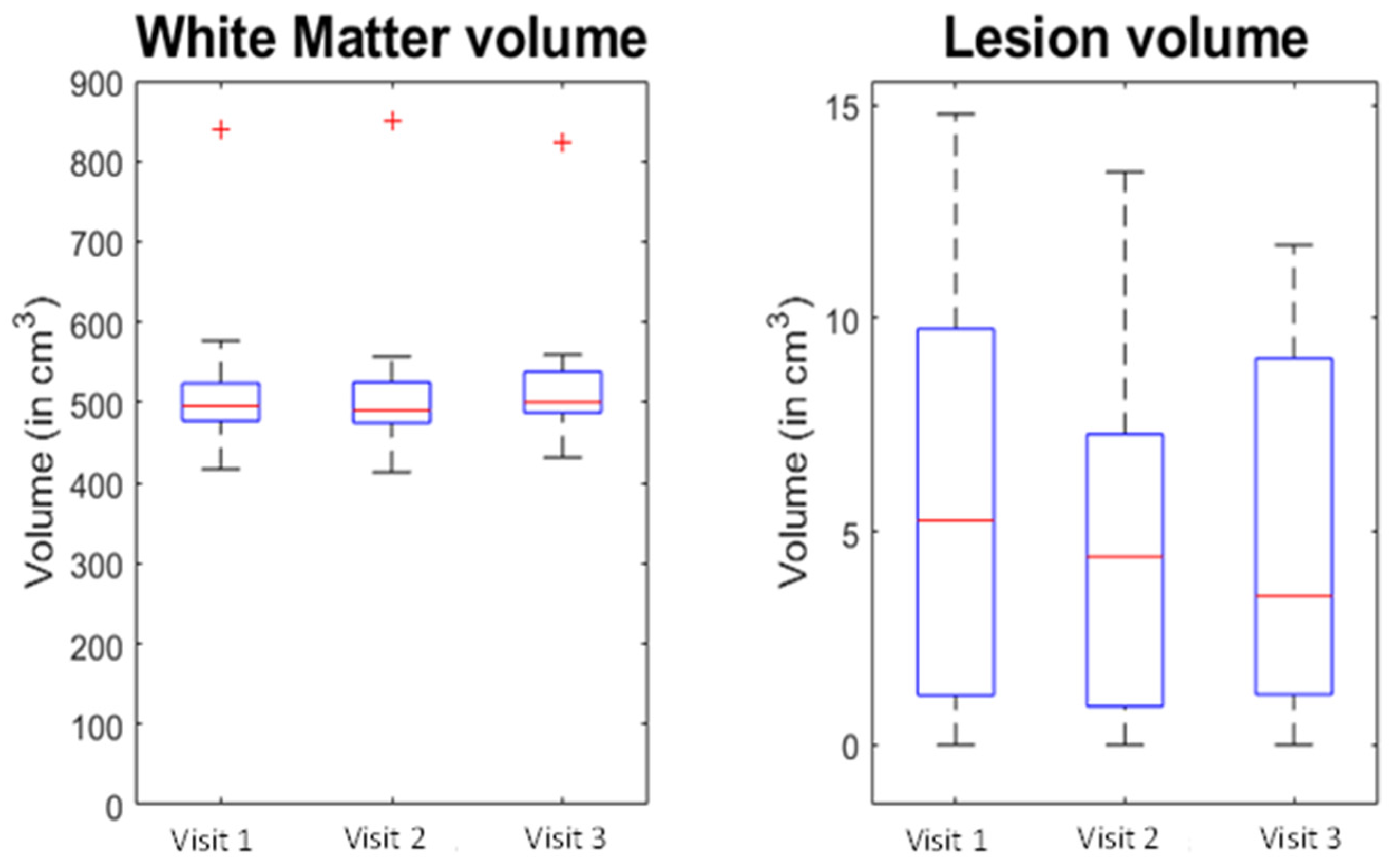
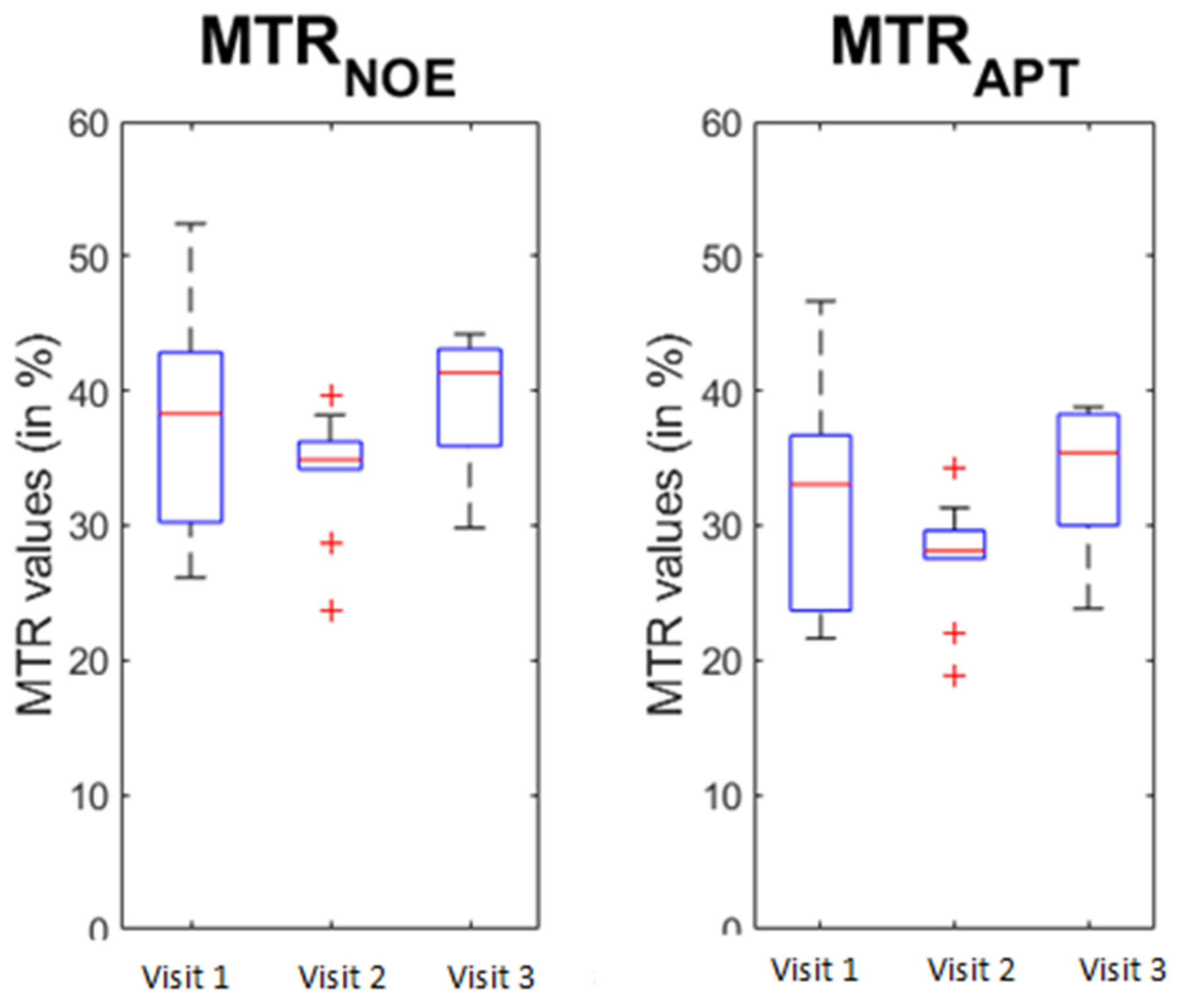
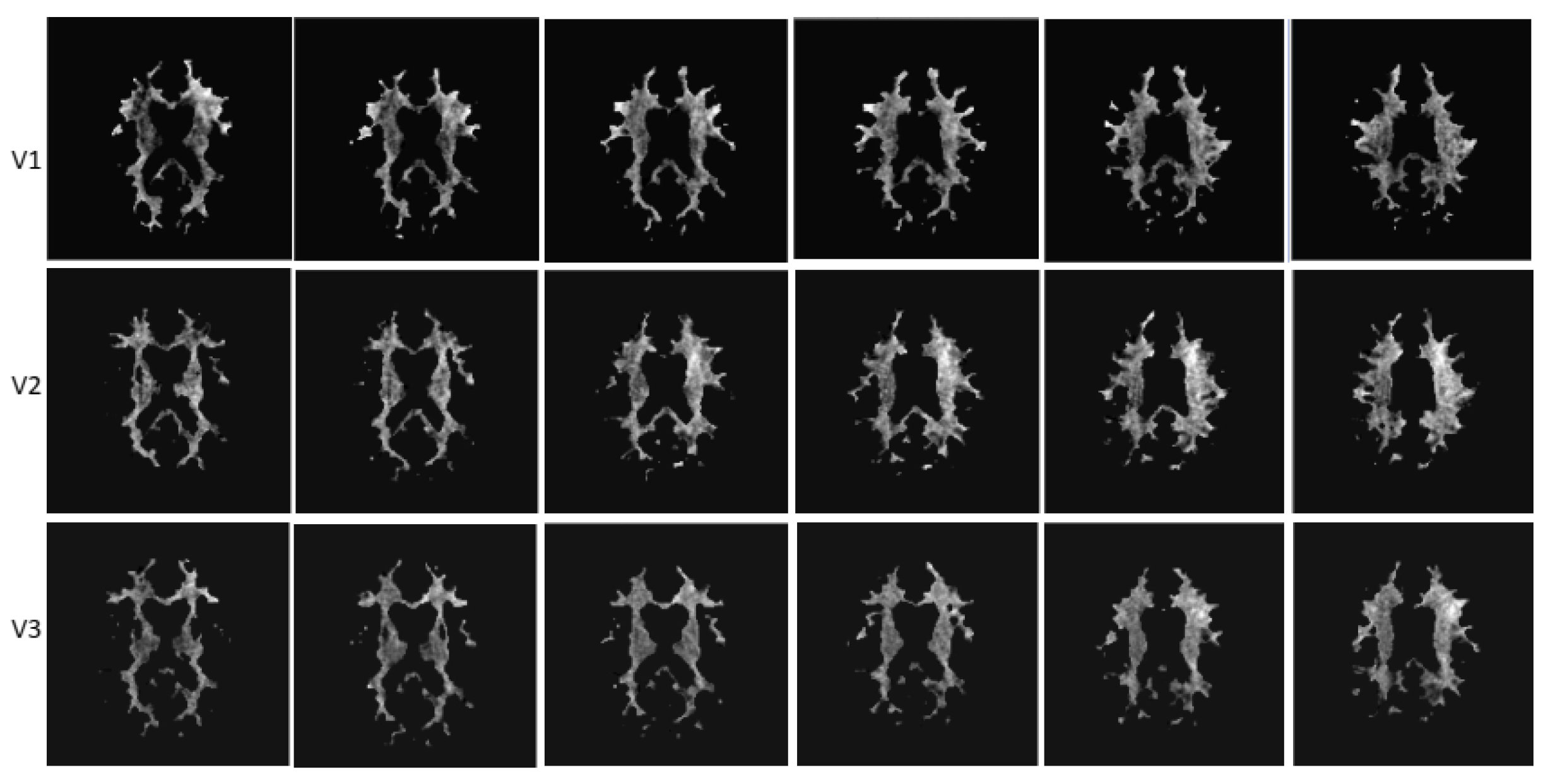
3.2. MRI Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Christensen, J.R.; Ratzer, R.; Bornsen, L.; Lyksborg, M.; Garde, E.; Dyrby, T.B.; Siebner, H.R.; Sorensen, P.S.; Sellebjerg, F. Natalizumab in progressive MS: Results of an open-label, phase 2A, proof-of-concept trial. Neurology 2014, 82, 1499–1507. [Google Scholar] [CrossRef]
- Preziosa, P.; Storelli, L.; Meani, A.; Moiola, L.; Rodegher, M.; Filippi, M.; Rocca, M.A. Effects of Fingolimod and Natalizumab on Brain T1-/T2-Weighted and Magnetization Transfer Ratios: A 2-Year Study. Neurotherapeutics 2021, 18, 878–888. [Google Scholar] [CrossRef]
- Soon, D.; Altmann, D.R.; Fernando, K.T.; Giovannoni, G.; Barkhof, F.; Polman, C.H.; O’Connor, P.; Gray, B.; Panzara, M.; Miller, D.H. A study of subtle blood brain barrier disruption in a placebo-controlled trial of natalizumab in relapsing remitting multiple sclerosis. J. Neurol. 2007, 254, 306–314. [Google Scholar] [CrossRef]
- Sucksdorff, M.; Tuisku, J.; Matilainen, M.; Vuorimaa, A.; Smith, S.; Keitila, J.; Rokka, J.; Parkkola, R.; Nylund, M.; Rinne, J.; et al. Natalizumab treatment reduces microglial activation in the white matter of the MS brain. Neurol. Neuroimmunol. Neuroinflamm. 2019, 6, e574. [Google Scholar] [CrossRef]
- Tallantyre, E.C.; Brookes, M.J.; Dixon, J.E.; Morgan, P.S.; Evangelou, N.; Morris, P.G. Demonstrating the perivascular distribution of MS lesions in vivo with 7-Tesla MRI. Neurology 2008, 70, 2076–2078. [Google Scholar] [CrossRef]
- Tallantyre, E.C.; Morgan, P.S.; Dixon, J.E.; Al-Radaideh, A.; Brookes, M.J.; Morris, P.G.; Evangelou, N. 3 Tesla and 7 Tesla MRI of multiple sclerosis cortical lesions. J. Magn. Reson. Imaging 2010, 32, 971–977. [Google Scholar] [CrossRef]
- Livshits, I.; Hussein, S.; Kennedy, C.; Weinstock-Guttman, B.; Hojnacki, D.; Zivadinov, R. Comparison of a 1.5T standard vs. 3T optimized protocols in multiple sclerosis patients. Minerva Med. 2012, 103, 97–102. [Google Scholar] [CrossRef]
- Tallantyre, E.C.; Morgan, P.S.; Dixon, J.E.; Al-Radaideh, A.; Brookes, M.J.; Evangelou, N.; Morris, P.G. A comparison of 3T and 7T in the detection of small parenchymal veins within MS lesions. Investig. Radiol. 2009, 44, 491–494. [Google Scholar] [CrossRef]
- Sartoretti, E.; Sartoretti, T.; Wyss, M.; Becker, A.S.; Schwenk, A.; van Smoorenburg, L.; Najafi, A.; Binkert, C.; Thoeny, H.C.; Zhou, J.; et al. Amide Proton Transfer Weighted Imaging Shows Differences in Multiple Sclerosis Lesions and White Matter Hyperintensities of Presumed Vascular Origin. Front. Neurol. 2019, 10, 1307. [Google Scholar] [CrossRef]
- Huang, J.; Xu, J.; Lai, J.H.C.; Chen, Z.; Lee, C.Y.; Mak, H.K.F.; Chan, K.H.; Chan, K.W.Y. Relayed nuclear Overhauser effect weighted (rNOEw) imaging identifies multiple sclerosis. Neuroimage Clin. 2021, 32, 102867. [Google Scholar] [CrossRef]
- By, S.; Barry, R.L.; Smith, A.K.; Lyttle, B.D.; Box, B.A.; Bagnato, F.R.; Pawate, S.; Smith, S.A. Amide proton transfer CEST of the cervical spinal cord in multiple sclerosis patients at 3T. Magn. Reson. Med. 2018, 79, 806–814. [Google Scholar] [CrossRef] [PubMed]
- Heo, H.Y.; Zhang, Y.; Burton, T.M.; Jiang, S.; Zhao, Y.; van Zijl, P.C.M.; Leigh, R.; Zhou, J. Improving the detection sensitivity of pH-weighted amide proton transfer MRI in acute stroke patients using extrapolated semisolid magnetization transfer reference signals. Magn. Reson. Med. 2017, 78, 871–880. [Google Scholar] [CrossRef]
- Kim, J.W.; Choi, J.; Cho, J.; Lee, C.; Jeon, D.; Park, S.H. Preliminary Observations on Sensitivity and Specificity of Magnetization Transfer Asymmetry for Imaging Myelin of Rat Brain at High Field. Biomed. Res. Int. 2015, 2015, 565391. [Google Scholar] [CrossRef] [PubMed]
- Al-Radaideh, A.; Mougin, O.E.; Lim, S.Y.; Chou, I.J.; Constantinescu, C.S.; Gowland, P. Histogram analysis of quantitative T1 and MT maps from ultrahigh field MRI in clinically isolated syndrome and relapsing-remitting multiple sclerosis. NMR Biomed. 2015, 28, 1374–1382. [Google Scholar] [CrossRef] [PubMed]
- Chou, I.J.; Lim, S.Y.; Tanasescu, R.; Al-Radaideh, A.; Mougin, O.E.; Tench, C.R.; Whitehouse, W.P.; Gowland, P.A.; Constantinescu, C.S. Seven-Tesla Magnetization Transfer Imaging to Detect Multiple Sclerosis White Matter Lesions. J. Neuroimaging 2018, 28, 183–190. [Google Scholar] [CrossRef]
- Elliott, C.; Momayyezsiahkal, P.; Arnold, D.L.; Liu, D.; Ke, J.; Zhu, L.; Zhu, B.; George, I.C.; Bradley, D.P.; Fisher, E.; et al. Abnormalities in normal-appearing white matter from which multiple sclerosis lesions arise. Brain Commun. 2021, 3, fcab176. [Google Scholar] [CrossRef]
- Zivadinov, R.; Dwyer, M.G.; Hussein, S.; Carl, E.; Kennedy, C.; Andrews, M.; Hojnacki, D.; Heininen-Brown, M.; Willis, L.; Cherneva, M.; et al. Voxel-wise magnetization transfer imaging study of effects of natalizumab and IFNbeta-1a in multiple sclerosis. Mult. Scler. 2012, 18, 1125–1134. [Google Scholar] [CrossRef]
- Rocca, M.A.; Preziosa, P.; Filippi, M. Application of advanced MRI techniques to monitor pharmacologic and rehabilitative treatment in multiple sclerosis: Current status and future perspectives. Expert Rev. Neurother. 2019, 19, 835–866. [Google Scholar] [CrossRef]
- Polman, C.H.; Reingold, S.C.; Banwell, B.; Clanet, M.; Cohen, J.A.; Filippi, M.; Fujihara, K.; Havrdova, E.; Hutchinson, M.; Kappos, L.; et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann. Neurol. 2011, 69, 292–302. [Google Scholar] [CrossRef]
- Tanasescu, R.; Frakich, N.; Chou, I.J.; Filippini, P.; Podda, G.; Xin, G.; Muraleedharan, R.; Jerca, O.; Onion, D.; Constantinescu, C.S. Natalizumab Treatment of Relapsing Remitting Multiple Sclerosis Has No Long-Term Effects on the Proportion of Circulating Regulatory T Cells. Neurol. Ther. 2023. [Google Scholar] [CrossRef]
- Hurley, A.C.; Al-Radaideh, A.; Bai, L.; Aickelin, U.; Coxon, R.; Glover, P.; Gowland, P.A. Tailored RF pulse for magnetization inversion at ultrahigh field. Magn. Reson. Med. 2010, 63, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Wright, P.J.; Mougin, O.E.; Totman, J.J.; Peters, A.M.; Brookes, M.J.; Coxon, R.; Morris, P.E.; Clemence, M.; Francis, S.T.; Bowtell, R.W.; et al. Water proton T1 measurements in brain tissue at 7, 3, and 1.5 T using IR-EPI, IR-TSE, and MPRAGE: Results and optimization. Magn. Reson. Mater. Phys. Biol. Med. 2008, 21, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Ropele, S.; Filippi, M.; Valsasina, P.; Korteweg, T.; Barkhof, F.; Tofts, P.S.; Samson, R.; Miller, D.H.; Fazekas, F. Assessment and correction of B1-induced errors in magnetization transfer ratio measurements. Magn. Reson. Med. 2005, 53, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Fox, R.J.; Cronin, T.; Lin, J.; Wang, X.; Sakaie, K.; Ontaneda, D.; Mahmoud, S.Y.; Lowe, M.J.; Phillips, M.D. Measuring myelin repair and axonal loss with diffusion tensor imaging. AJNR Am. J. Neuroradiol. 2011, 32, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Wiebenga, O.T.; Schoonheim, M.M.; Hulst, H.E.; Nagtegaal, G.J.; Strijbis, E.M.; Steenwijk, M.D.; Polman, C.H.; Pouwels, P.J.; Barkhof, F.; Geurts, J.J. White Matter Diffusion Changes during the First Year of Natalizumab Treatment in Relapsing-Remitting Multiple Sclerosis. AJNR Am. J. Neuroradiol. 2016, 37, 1030–1037. [Google Scholar] [CrossRef]
- Ontaneda, D.; Sakaie, K.; Lin, J.; Wang, X.F.; Lowe, M.J.; Phillips, M.D.; Fox, R.J. Measuring Brain Tissue Integrity during 4 Years Using Diffusion Tensor Imaging. AJNR Am. J. Neuroradiol. 2017, 38, 31–38. [Google Scholar] [CrossRef]
- Sinnecker, T.; Granziera, C.; Wuerfel, J.; Schlaeger, R. Future Brain and Spinal Cord Volumetric Imaging in the Clinic for Monitoring Treatment Response in MS. Curr. Treat. Options Neurol. 2018, 20, 17. [Google Scholar] [CrossRef]
- Wu, B.; Warnock, G.; Zaiss, M.; Lin, C.; Chen, M.; Zhou, Z.; Mu, L.; Nanz, D.; Tuura, R.; Delso, G. An overview of CEST MRI for non-MR physicists. EJNMMI Phys. 2016, 3, 19. [Google Scholar] [CrossRef]
- Zhou, J.; Payen, J.F.; Wilson, D.A.; Traystman, R.J.; van Zijl, P.C. Using the amide proton signals of intracellular proteins and peptides to detect pH effects in MRI. Nat. Med. 2003, 9, 1085–1090. [Google Scholar] [CrossRef]
- Mougin, O.; Clemence, M.; Peters, A.; Pitiot, A.; Gowland, P. High-resolution imaging of magnetisation transfer and nuclear Overhauser effect in the human visual cortex at 7 T. NMR Biomed. 2013, 26, 1508–1517. [Google Scholar] [CrossRef]
- O’Grady, K.P.; Satish, S.; Owen, Q.R.; Box, B.A.; Bagnato, F.; Combes, A.J.E.; Cook, S.R.; Westervelt, H.J.; Feiler, H.R.; Lawless, R.D.; et al. Relaxation-Compensated Chemical Exchange Saturation Transfer MRI in the Brain at 7T: Application in Relapsing-Remitting Multiple Sclerosis. Front. Neurol. 2022, 13, 764690. [Google Scholar] [CrossRef] [PubMed]

| Patient Demographics (n = 12) | |
|---|---|
| Age (years, standard deviation) | 34.2 (7.2) |
| Sex (no. of subjects, %) | |
| Female | 7 (58%) |
| Male | 5 (42%) |
| Ethnicity | |
| White British | 10 |
| Asian British | 1 |
| African British | 1 |
| Clinical characteristics | |
| Type of MS | |
| (no. of subjects, %) | |
| RR | 12 (100%) |
| SP | 0 (0%) |
| Time from last clinical relapse | >90 days |
| Annualised relapse rate (95% CI) | 1.99 (1.93–2.02) |
| Mean EDSS score (range) | 3.5 (1–7) |
| Lesion volume mm3 | |
| (average, standard deviation) | 6639.7 ± 4632.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanasescu, R.; Mougin, O.; Chou, I.-J.; Al-Radaideh, A.; Jerca, O.P.; Lim, S.-Y.; Gowland, P.; Constantinescu, C.S. Natalizumab Treatment for Relapsing Multiple Sclerosis Stabilises Normal-Appearing White Matter Microstructure: A One-Year Prospective Ultra-High-Field Quantitative Imaging Study. Brain Sci. 2023, 13, 1464. https://doi.org/10.3390/brainsci13101464
Tanasescu R, Mougin O, Chou I-J, Al-Radaideh A, Jerca OP, Lim S-Y, Gowland P, Constantinescu CS. Natalizumab Treatment for Relapsing Multiple Sclerosis Stabilises Normal-Appearing White Matter Microstructure: A One-Year Prospective Ultra-High-Field Quantitative Imaging Study. Brain Sciences. 2023; 13(10):1464. https://doi.org/10.3390/brainsci13101464
Chicago/Turabian StyleTanasescu, Radu, Olivier Mougin, I-Jun Chou, Ali Al-Radaideh, Oltita P. Jerca, Su-Yin Lim, Penny Gowland, and Cris S. Constantinescu. 2023. "Natalizumab Treatment for Relapsing Multiple Sclerosis Stabilises Normal-Appearing White Matter Microstructure: A One-Year Prospective Ultra-High-Field Quantitative Imaging Study" Brain Sciences 13, no. 10: 1464. https://doi.org/10.3390/brainsci13101464
APA StyleTanasescu, R., Mougin, O., Chou, I.-J., Al-Radaideh, A., Jerca, O. P., Lim, S.-Y., Gowland, P., & Constantinescu, C. S. (2023). Natalizumab Treatment for Relapsing Multiple Sclerosis Stabilises Normal-Appearing White Matter Microstructure: A One-Year Prospective Ultra-High-Field Quantitative Imaging Study. Brain Sciences, 13(10), 1464. https://doi.org/10.3390/brainsci13101464








