Abstract
Patients with schizophrenia spectrum disorders (SSD) have an elevated risk of suicidality. The same has been found for people within the penitentiary system, suggesting a cumulative effect for offender patients suffering from SSD. While there appear to be overlapping characteristics, there is little research on factors distinguishing between offenders and non-offenders with SSD regarding suicidality. Our study therefore aimed at evaluating distinguishing such factors through the application of supervised machine learning (ML) algorithms on a dataset of 232 offenders and 167 non-offender patients with SSD and history of suicidality. With an AUC of 0.81, Naïve Bayes outperformed all other ML algorithms. The following factors emerged as most powerful in their interplay in distinguishing between offender and non-offender patients with a history of suicidality: Prior outpatient psychiatric treatment, regular intake of antipsychotic medication, global cognitive deficit, a prescription of antidepressants during the referenced hospitalisation and higher levels of anxiety and a lack of spontaneity and flow of conversation measured by an adapted positive and negative syndrome scale (PANSS). Interestingly, neither aggression nor overall psychopathology emerged as distinguishers between the two groups. The present findings contribute to a better understanding of suicidality in offender and non-offender patients with SSD and their differing characteristics.
1. Introduction
Schizophrenia spectrum disorders (SSD) are severe mental disorders with a substantial burden of disease due to significant impairments in many domains and high excess mortality, with 10 to 25 years less life expectancy than the general population [1,2]. While natural causes, such as respiratory and cardiovascular diseases, account for most deaths in this population, another risk factor for early mortality is the high rates of suicidality among patients with SSD, with a lifetime prevalence of around 30% for suicidal ideations, suicide plans and attempts, and a lifetime risk of suicide between 3–7% [3,4,5,6,7]. Factors known to contribute to the high risk of suicide for patients with SSD are young age, male gender, a high level of education, a history of suicide attempts as well as depressive and delusional symptoms [7]. Further studies suggest an association between violent behaviour and suicidal or self-harming behaviour in general among patients with SSD [8,9]. Results regarding the influence of hallucinations are mixed: while some authors have described them to contribute to an elevated risk, a systematic review by Hawton et al. found an association between a reduced risk of suicide under hallucinatory symptoms [7,10].
Another population at higher risk for suicide than the general population are people who display aggressive and violent behaviour in general, and violent offenders in particular [11,12,13]. In these populations, having a psychiatric disorder, such as depression or substance use disorders, has been found to be associated with higher rates of suicide [14]. A large cohort study among prisoners in the United States found a substantially higher suicide risk if schizophrenia (RR = 7.3) and other non-schizophrenic psychotic disorders (RR = 13.8) were present [8]. A longitudinal Danish study amongst offenders identified custodial sentencing, but, even more so, sentencing to psychiatric treatment to be strongly associated with increased suicide risk (OR = 26.65) [15]. A smaller study comparing prison and forensic psychiatric hospital populations confirmed a higher suicide rate in the latter [9]. These previous findings suggest that, among patients with SSD, the subgroup of offender patients with SSD is at particularly high risk for suicide and suicidal behaviour. Even though offender patients with SSD can be considered a dual-vulnerable population due to the coercive treatment context as well as their often highly impairing mental disorder, little is known about whether this subgroup is influenced by other mediators with respect to suicidality, and whether the known risk factors have similar weights as in general psychiatric patients. Previous literature has either focused mainly on inmates or patients with SSD, but rarely populations with both these features in co-occurrence. In a recent study, our research group evaluated predictors of self-harm in offender patients with SSD and identified the early onset of disorder and higher severity of psychopathology as risk factors [16]. As this had only been an explorative analysis within the offender population, there was no control group.
This research gap cannot be closed by simply applying knowledge gained from general psychiatric patients due to numerous systematic differences between forensic and general psychiatric patients: First of all, OP are known to have a higher rate of comorbidity, especially substance use [17,18]. Secondly, they receive treatment in a compulsory context as it is court-mandated, and the treatment goals may not be in line with the patients’ own ideas [19]. Thirdly, while aggressive behaviour is also common in acute psychiatric wards, OP stand out amongst psychiatric patients due to their history of severe violence [20,21]. They also are more likely to be subjected to disadvantageous social circumstances, such as unemployment and homelessness [20]. Due to the fact that there are several key differences between OP and NOP, it can be assumed that the two groups differ in many domains, including suicidality.
Therefore, and in light of previous research, the first objective of this study now presented was to detect the most distinguishing factors between offender patients with SSD (OP) and non-offender patients with SSD (NOP), both with a history of suicidality. Our second objective was to build a model based on these distinguishing features and to rank them according to their significance, using advanced statistics in the form of machine learning (ML). This study was reviewed and approved by the Ethics Committee Zurich [Kanton Zürich] (committee’s reference number: KEK-ZH-NR 2014–0480).
2. Materials and Methods
The study group comprised 370 offender patients (OP) with an SSD, including schizophrenia, schizoaffective and delusional disorders (F2x according to ICD-10 and ICD-9), who had all been in court-mandated treatment at the Centre for Inpatient Forensic Therapies of the University Hospital of Psychiatry Zurich, Switzerland due to being found not guilty by reason of insanity (NGRI) or for treatment of acute syndromes while being in the penitentiary system [22,23]. This population has been used in previous exploratory analyses of our research group as part of a larger ongoing project studying offender patients with SSD. The comparison group comprised 370 non-offender patients (NOP) with SSD, who had been in inpatient treatment at the Centre for Integrative Psychiatry of the University Hospital of Psychiatry Zurich. This general psychiatric facility focuses on rehabilitative treatment, and its population mostly consists of patients suffering from chronic and/or prolonged courses of disorder. As this is a characteristic shared with the majority of forensic psychiatric patients, we deemed this sample to be particularly suitable as a comparison group. Another reason was that in both groups, initial treatment for acute psychosis had already been established in most cases, either in an acute ward for NOP or in a prison setting for OP.
Data from the files of all patients were retrospectively assessed through directed qualitative content analysis [24]. Data extraction was performed by two experienced psychiatrists according to an adapted rating protocol based on a set of criteria originally described by Seifert and Nedopil [25]. The case files were rather comprehensive and included professionally documented medical histories, psychiatric/psychologic reports of both hospitalisations as well as outpatient treatments, extensive progress reports by clinicians, nursing and care staff, as well as—in the case of the OP population—testimonies, court proceedings and data regarding previous imprisonments and detentions. Data on the following areas were collected from said case files: social-demographic data, childhood/youth events, psychiatric history, past criminal history, social/sexual functioning, prison data, and particularities of the current hospitalisation and psychopathological symptoms defined by an adapted three-tier positive and negative syndrome scale (PANSS) [26,27]. The PANSS was developed as a multidimensional rating scale for assessing positive and negative syndromes as well as overall psychopathology in patients with schizophrenia and is validated and globally well established, with a mean interrater correlation of 0.83–0.87 and internal reliability of 0.73–0.83 (α coefficient) [27]. For this study, we used an adapted three-tier rating scale instead of rating each item on a seven-tier scale. As we wanted to match both groups by gender, no further female patients were included in the NOP sample after having reached the number of female patients in the OP group.
Suicidality was defined as either one of the following before the offence leading to the referenced forensic psychiatric hospitalisation for OP, respectively, before the referenced hospitalisation for NOP: suicidal thoughts and ideations, plans, and attempts. This information was also assessed retrospectively through the patients’ case files (e.g., reports of previous psychiatric hospitalisations). After omitting all cases without a history of suicidality, a total of 399 patients remained, with 232 of them being OP (58.1%) and 167 NOP (41.9%). In the initial step, we calculated the p-value for demographic and psychiatric variables to evaluate basic group characteristics. For this purpose, we performed an independent samples Mann–Whitney-U-Test for all metric variables with non-normal distribution, and a Fisher’s Exact Test for all other variables [28,29].
Predictor variables were selected in accordance with previous findings (see Appendix A for a detailed overview of our selected variables and their reference in previous literature).
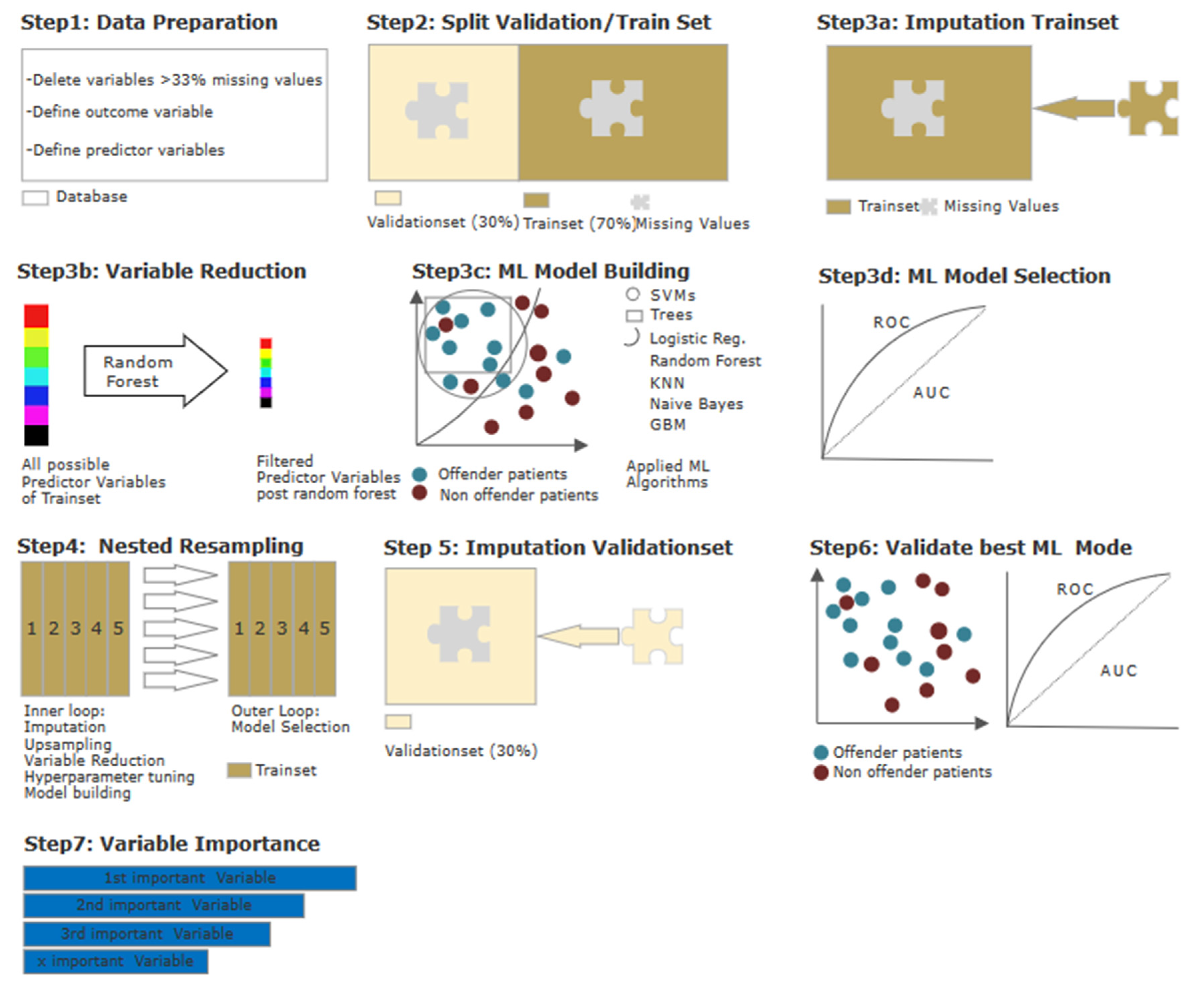
We applied supervised machine learning (ML) to evaluate the interplay of the variables and to rank them according to their contribution to the model. Supervised ML learning is used generally to describe prediction tasks in order to classify a specific outcome of interest—in this case, suicidality—as opposed to unsupervised ML, which can be useful to find relationships in a dataset without having measured an outcome [30]. The performance of said model regarding its ability to differentiate between suicidal OP and NOP should then be quantified. An overview of the statistical steps is shown in Figure 1 provides a first glance at the statistical procedures step-by-step. Due to overlapping methodological approaches, part of the following section has been previously published, e. g. in Hofmann et al. [26], and is therefore partially replicated here.
Figure 1.
Statistical procedures using machine learning (ML). Step 1—Data preparation: Conversion of categorial variables to binary code. Outcome variable OP/NOP and predictor variables were defined. Omission of variables with missing values of 30% or more Step 2—Data splitting: 70% training dataset and 30% validation dataset. Step 3a–d—Model building and selection (a): Imputation by mean; (b) variable reduction via random forest; (c) model building using ML algorithms (d) selection of most suitable ML algorithm via ROC parameters. Step 4—Model building and testing on training subset: Step 5—Imputation by mean on validation set. Step 6—Model building and testing on validation data: Application of the most suitable model identified in Step 3c on imputed validation dataset, evaluation via ROC parameters. Step 7—Test for multicollinearity and ranking of variables.
All the steps were performed using R version 3.6.3. (R Project, Vienna, Austria) and the MLR package v2.171 (Bischl, Munich, Germany). The balanced accuracy was calculated in MATLAB R2019a (MATLAB and Statistics Toolbox Release 2012, The MathWorks, Inc., Natick, MA, USA). Initially, we processed all raw data for ML (see Figure 1, Step 1): Several categorical variables were converted to binary code., while continuous and ordinal variables did not undergo adjustment. The independent variable was dichotomised into (a) “offender patient (OP)” and (b) “non-offender patient (NOP)”, with the latter being defined as the positive class. All variables with missing values of 30% or more were omitted, yielding 107 possible predictor variables (for a detailed variable description, please refer to the material in the Appendix A and Appendix B). In a second step, the database was split into one training subset containing 70% of all cases, and one validation subset containing the remaining 30% (see Figure 1, Step 2). The training subset was used for variable reduction and model building/selection. To avoid the need to omit variables entirely due to missing values in an already small population, we conducted an imputation of missing values (by mean for continuous variables, and by mode for categorical variables). Imputation weights were stored to be later reapplied to the validation subset (see Figure 1, Step 3a). As we wanted to identify the most influential predictors and as a decrease in variables can counter-act overfitting while maintaining practical computing times in initial model building, we performed a variable reduction through random-Forest SRC, down to the point where the AUC did improve by no more than 5% through adding another item (see Figure 1, Step 3b). This led to a variable reduction down to the six most predictive variables. With the database of n = 399 being relatively small for ML purposes, we applied discriminative model building with seven algorithms (see Figure 1, Step 3c). The quality of each model was assessed in terms of established performance parameters. The model with the highest AUC was then chosen for final model validation with the validation subset (see Figure 1, Step 3d). Finally, with the intention to prevent overfitting, we used a nested resampling model with the inner loop performing imputation, variable filtration, and model building within fivefold cross-validation, and the outer loop for performance evaluation also embedded in fivefold cross-validation (see Figure 1, Step 4). This cross-validation artificially created five different subsets of our dataset of equal size so that one subset could serve as the training set for our model, while the remaining four subsets allowed us to evaluate the accuracy of the learned model [31,32]. To evaluate the model selected earlier, we applied it to the validation subset, which included 30% of all cases: The imputation weights from Step 3a were reused on the validation subset (see Figure 1, Step 5). Afterward, the selected model was applied (see Figure 1, Step 6). Lastly, the variables identified as most dominant in the model were finally ranked according to their indicative power (see Figure 1, Step 7).
3. Results
3.1. Demographic and Psychiatric Characteristics
As shown in Table 1, the two groups were well balanced regarding demographics: Around three-quarters of both OP and NOP were diagnosed with schizophrenia, while the remaining one-quarter were admitted under diagnoses of schizoaffective disorder, acute psychotic disorder, and other disorders from the schizophrenia spectrum (F2x. according to ICD-10 and ICD-9). Both groups were predominantly single at the time of their criminal offence (OP), respectively, of their admission to the referenced hospitalisation. NOP, however, had a lower rate of patients whose native country was Switzerland. Around half of the total population had at least one documented suicide attempt prior to their referenced hospitalisation, a rate that was also reflected in the individual groups. Suicide attempts during the referenced hospitalisation were extremely rare, with 2 in the NOP and 10 in the OP group. As expected, OP expressed higher rates of endangerment of others both in the past as well as during the referenced hospitalisation.

Table 1.
Demographic characteristics of the study population.
3.2. Model Calculation Using Machine Learning (ML)
The performance parameters of the seven calculated ML algorithms are provided in Table 2.

Table 2.
Machine learning models and performance in nested cross-validation.
With a balanced accuracy of 76.6% and an AUC of 0.87, the naïve Bayes algorithm showed the best performance parameters. As described above, the model did not improve significantly (>5) by adding another item. Under the inclusion of all initial 107 possible predictor variables, the AUC yielded 0.89 as compared to the AUC of 0.87 under the inclusion of 6 variables. This very small delta between the two AUC demonstrates that the model is mainly dominated by the 6 predictor variables. The absolute and relative distribution of the 6 most predictive variables identified during nested resampling, which were used for the model building, are shown in Table 3.

Table 3.
Absolut and relative distribution of predictor variables most dominant in the model.
The quality of the final naïve Bayes model on the validation subset is provided in Table 4.

Table 4.
Performance measures of naïve Bayes model on the validation set.
While the balanced accuracy of 71.2% and the AUC of 0.81 were a little lower than the results of the initial training model, they were still indicative. With a sensitivity of 61.5% and a specificity of 80.9%, NOP with a history of suicidality were identified correctly in two-thirds of the cases, while four-fifths of cases were identified correctly as being OP with a history of suicidality.
3.3. Ranking of Predictor Variables
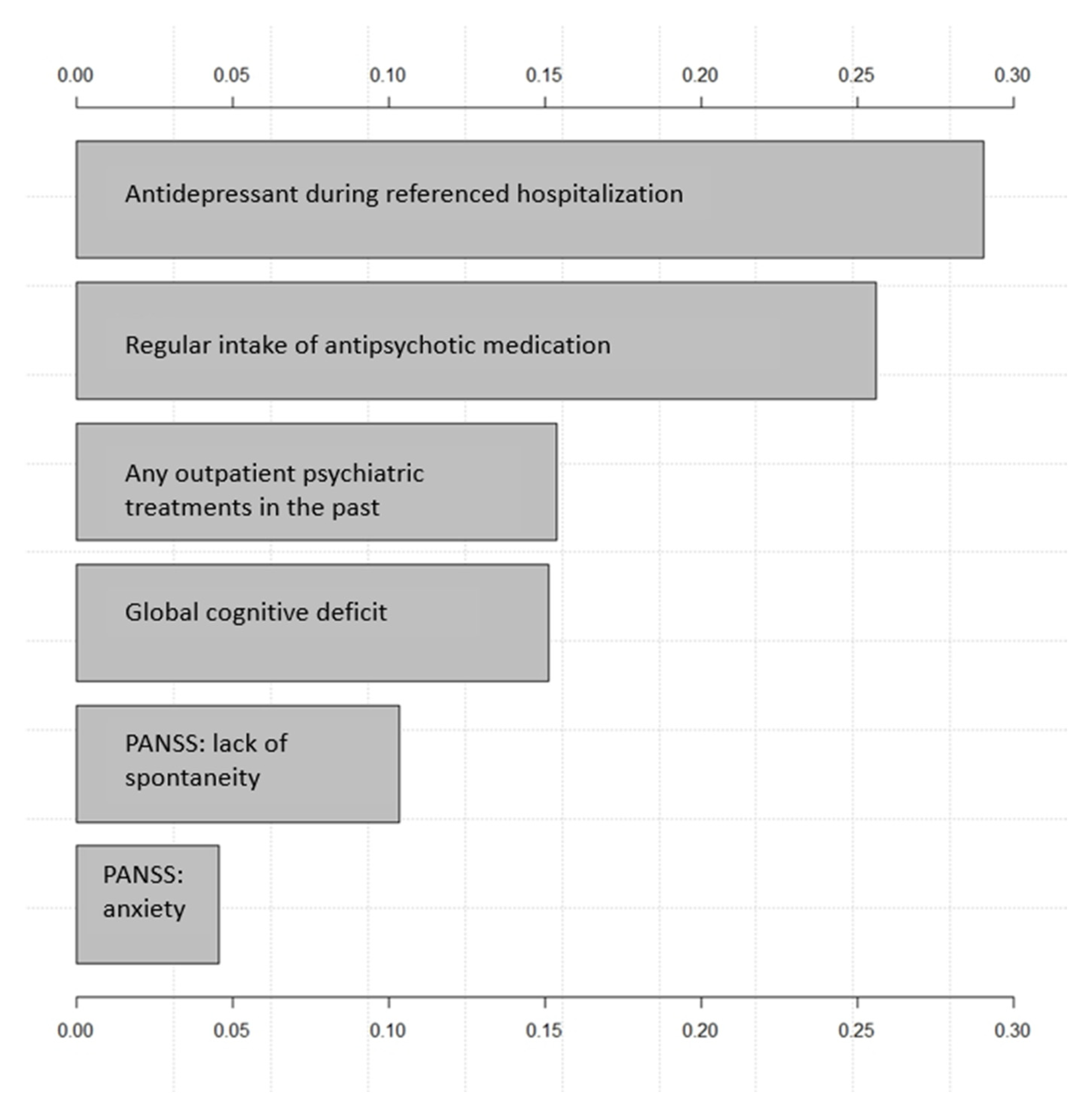
Figure 2 shows the effect on the output variable (NOP/OP) by varying each predictor variable at a time, keeping all the other predictor variables at their initial values. The x-axis represents the relative variable importance, and the y-axis each variable (the wider the bar, the more impact the variable has on the model and the outcome). Consequently, the predictor variables are ranked from the most influential to the least influential within the model.
Figure 2.
Importance of variables by naïve bayes. PANSS refers to adapted PANSS as described in the methodology section.
The two variables most indicative of being a non-offender patient in the model referred to as pharmacotherapy were “antidepressant during referenced hospitalisation” and “regular intake of antipsychotic medication”. Other influential items that set apart NOP from OP were having had “any outpatient psychiatric treatment(s) in the past”, having a “global cognitive deficit” as well as higher scores on the adapted PANSS items “anxiety” and “lack of spontaneity and flow of conversation”.
4. Discussion
The aim of this study was to determine the factors that distinguish between patients with SSD and a history of suicidality who had committed a criminal offence from those who did not. Regarding demographic and psychiatric characteristics, we found that OP were more often from native countries other than Switzerland, and, as expected, showed a significantly higher rate of endangerment of others both in the past and during the referenced hospitalisation. Even though it did not quite reach a satisfying level of significance, NOP had more frequently attempted suicide in the past. Apart from these characteristics, both groups were rather similar, thus allowing optimal comparability.
As there is little research on the matter, thus complicating the generation of null hypotheses, we used and explorative approach, applying ML algorithms to a large database consisting of 399 patients matched for age and gender. In doing so, we were able to create an appropriate model: With a balanced accuracy of 71% and an AUC of 0.81, the model based on the Naïve Bayes algorithm as able to correctly identify non-offenders in two-thirds of the cases. Variables related mostly to integration into the therapeutic support network, pharmacotherapy, and cognition. Results painted a picture of the NOP with a history of suicidality as being more compliant regarding (pharmaco-)therapy—which was more likely to include antidepressants, but more subjected to cognitive deficits and anxiety. They were more likely to have a prescription for antidepressants during the referenced hospitalisation. This observation is not only found when comparing merely the patients with a suicidal history: a higher rate of antidepressant pharmacotherapy in NOP with SSD than OP with SSD has been observed in general [33]. While an adjunctive antidepressant can be beneficial to patients with SSD, especially regarding negative symptoms, it seems to be a less common prescription in OP, possibly due to fear of re-exacerbation of positive psychotic symptoms and an increased risk of side effects [34,35]. This could also prevent clinicians from targeting suicidality with antidepressants. They may rather rely on antipsychotics and mood stabilisers in suicidal offender patients, e. g. clozapine, which is especially recommended for forensic psychiatric populations due to evidence for its efficacy against violent behaviour but has also shown to be effective regarding suicidality [36,37]. As research on prescription practices in offender populations with SSD are scarce, the possible reasons that explain why antidepressant medication is the most influential variable in the model remain hypothetical and cannot be confirmed without data on the clinicians’ decision process in pharmacotherapeutic treatment.
Compared to OP, NOP were also more likely to have been involved in psychiatric treatment prior to the referenced hospitalisation in the form of outpatient treatment and to show a regular intake of their prescribed antipsychotic medication. In the literature, a negative attitude towards therapy or a lack of compliance has been described as a risk factor for the development of suicidality in general, but not for forensic psychiatric patients with SSD [20,38,39]. The question remains as to why this factor emerges as a distinguishing feature between OP and NOP even in a sample exclusively comprising patients who had shown suicidality in the past. Previous research has described an insufficient integration into the mental health care system in offenders with SSD: while there is high utilisation of inpatient treatments, regular outpatient therapies and regular intake of prescribed pharmacotherapeutic substances are observed less frequently [40,41]. It has been hypothesised, that due to a greater risk profile, inpatient care becomes more likely in individuals with violent behaviour [42]. This could largely refer to compulsory admissions, which are indicated and legally permissible in Switzerland in cases of acute danger to the self, but also to others. In summary, the current findings indicate that—while lack of compliance regarding (pharmaco-)therapeutic treatment is a known risk factor of suicidality—the risk factor domain of insufficient treatment is particularly salient in a population that is clustered to show inadequate treatment adherence.
NOP also showed a higher prevalence of global cognitive deficits and scored higher on the PANSS-item “lack of spontaneity and flow of speech”, which seems likely to be interlinked. This was surprising, as previous research comparing OP and NOP with SSD found the former to have worse overall cognitive functioning [43]. However, it has been hypothesised that institutionalised OP may participate in cognitive tests with greater engagement to demonstrate motivation, resulting in better scores when compared to their controls [44]. There is also a possible selection bias to be considered: Data on the NOP group were extracted from patients admitted to a rehabilitative psychiatric institution, focusing on reintegration into social and, if appropriate, working life. Due to this treatment focus, physicians are likely to refer patients who primarily have limited daily living skills rather than impairments in other symptom domains, e. g. positive productive symptoms, as focus of their therapeutic goals. In contrast, admittance to the institution from which the OP data stem is not determined by symptomatology of the individual patient, but by court mandate. The OP sample may therefore not be as subjected to pre-selection of patients corresponding to the NOP sample.
Lastly, NOP were characterised by higher levels of anxiety as measured by an adapted PANSS than their OP counterparts. Anxiety has been identified as a mediator for suicidality in both offender populations and SSD populations [45,46,47,48]. At the same time, anxiety can be difficult to detect in patients with SSD due to obscuring positive psychotic symptoms and impairment regarding the ability to verbalise and express emotions [47]. This could even more be the case in offender populations, as they may tend to externalise anxiety through antisocial and impulsive behaviours as an outward expression of emotional distress, as described by Carragher et al. [49]. Another possible explanation is a potentially reduced openness on the part of the patient in the coercive context of the forensic psychiatric setting: The special role of the forensic psychiatrist as a “dual mandate holder” who not only treats but also controls, orders, and monitors leads to a certain vertical relationship since the patient is not able to simply terminate therapy without consequences [50]. This may consequently have an influence on trust in the treating clinician. Especially in the initial treatment period, a longer phase of therapeutic relationship building is usually necessary to allow the patient to verbalise and show vulnerability. However, as Höfer et al. could demonstrate, the quality of the therapeutic relationship is not associated with the patient’s legal status, but with the severity of hostility as a symptom, thus showing that a coercive setting does not obligatorily lead to an impaired therapeutic basis [51].
Interestingly, variables linked to aggression, although more prevalent in the offender population, were not amongst the most influential variables in the model and were dominated by the items discussed above. Even though over half of the patients in both groups had shown some kind of endangerment of others in the past and OP had a significantly higher expression of aggression towards others both before and during their referenced hospitalisation, the item did not emerge as highly powerful in distinguishing the two groups from another. It can however not be ruled out, that variables regarding aggression could have more impact if a more precise distinction is made between the different manifestations of aggression. When taking previous literature on offenders into account, this seems likely, as the severity of the offence committed has been associated with the risk of suicide [52,53]. The current finding also indicates that aggression against others and suicidality are indeed independent phenomena. While such a linkage has been described in previous literature for adults and adolescents, other characteristics present in patients with a pattern of aggressive behaviour may be the driving forces behind suicidal developments [8,9,54].
Another striking finding was that, while individual symptom domains such as anxiety and cognitive deficits were of great influence in the model, overall clinical impairment as measured by the total PANSS score was not. The few studies directly comparing offender and non-offender patients with SSD reported the former to be more clinically impaired, which seems logical, as court-mandated treatment is mostly intended for highly severe courses of the disorder [20,43,55]. A potential explanation for this contradictive result could be in the selection of our comparison group: As described in the methodology section, we chose patients within a rehabilitative psychiatric institution due to their similar rate of chronically ill patients. It could be that the overall burden of disease had less influence on the model than other items because of similarly severe treatment courses in both study and comparison groups.
When looking into the limitations of this study, the most obvious is retrospective design. While we aimed at ensuring sufficient quality of data by using a structured data extraction protocol, data quality comparable to a prospectively standardised study cannot be assumed. This is especially the case for items that may be subject to high interrater reliability, such as “social isolation”. Such items may have already been scored differently by differing clinicians during documentation, thus resulting in skewed results. For robust variables, such as the number of previous hospitalisations, it is likely that this effect is less pronounced. Additionally, as the data extraction was performed by two psychiatrists rather than one, it cannot be ruled out that biases were introduced through this procedure. When looking at the selection of our comparison group, it should be noted that some of the NOP had also shown aggressive incidents in the past. Nevertheless, those patients were not grouped into the OP sample as their aggressive incidents had remained without the involvement of the judicial system in a sense of court-mandated treatment.
Another limitation was our broad definition of suicidality, including suicidal thoughts and ideations, plans, and attempts. The rationale behind this decision was the intention to cover suicidality as a whole entity. However, it cannot be ruled out that results may present themselves differently when differentiating more between the different manifestations of suicidality. In general, while our sample can be considered rather large for forensic psychiatry as a niche specialty, it has to be acknowledged that the total case number of 399 patients, each group collected from a single institution, can merely serve exploratory purposes. Further application and validation of the model to a larger population are, therefore, recommended, preferably in a multicentric approach to eliminate possible bias through characteristics of the institution. Lastly, as expected in offender populations with matching controls, our sample was predominantly male, thus limiting the applicability of our results to women in forensic psychiatric institutions. Replication of our findings in a larger sample, therefore, seems sensible, preferably in a prospective approach and, if possible, under the inclusion of more female patients.
In summation, the present findings enhance our understanding of suicidality in offender and non-offender patients with SSD and their differing characteristics. Using ML, we identified the 6 factors most distinguishing between the two groups, as well as their complex interplay out of a large dataset with 107 possibly predictive different parameters. The results suggest that even though both OP and NOP have an elevated risk for suicidality, different risk factors could have differing weightings depending on the population. This should raise awareness amongst clinicians when evaluating suicidality: Not all risk factors seem to have the same impact in different patient populations, and certain interventions may therefore be more indicated and profitable for one group than the other. For instance, it seems sensible to further address anxiety in OP with a history of suicidality. In general, the authors propose further research on suicidality in these populations, ideally in prospective trials with a large population as to allow subgroup testing as well as generalizability.
Author Contributions
Conceptualisation, J.K. and L.M.; methodology, J.K.; software, J.K.; validation, J.K. and L.M.; formal analysis, J.K.; investigation, J.K. and L.M.; resources, L.M., J.K., S.L. and E.H.; data curation, L.M., J.K. and E.H.; writing—original draft preparation, L.M.; writing—review and editing, L.M., S.L. and J.K.; visualisation, L.M. and J.K.; supervision, S.L., J.K. and E.H.; project administration, J.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was reviewed and approved by the Ethics Committee Zurich [Kanton Zürich] (committee’s reference number: KEK-ZH-NR 2014–0480). The study complied with the Helsinki Declaration of 1975, revised in 2008.
Informed Consent Statement
Patient consent was waived due to the retrospective design, for which formal consent is not required.
Data Availability Statement
The datasets generated and analysed during the current study as well as a detailed list are of all our variables (including definitions and references) are available from the corresponding author on request.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A. Selected Variables and Reference to Previous Literature
| Variable in Current Study | Previous Literature w. Similar Variable | Population: Description/Sample Size (n) |
| Sociodemographic Data | ||
| Age at admission to referenced hospitalization | [56] | NOP with SSD/510 |
| [57] | NOP with SSD + depression/132 | |
| [58] | NOP with SSD/150 | |
| Gender | [56] | NOP with SSD/510 |
| [57] | NOP with SSD + depression/132 | |
| [58] | NOP with SSD/150 | |
| [59] | OP with SSD/223 | |
| Country of birth: Switzerland | - | - |
| Marital status * | [57] | NOP with SSD + depression/132 |
| [59] | OP with SSD/223 | |
| Living situation * | [57] | NOP with SSD + depression/132 |
| [20] | OP and NOP with schizophrenia/70 | |
| Level of education * | [57] | NOP with SSD + depression/132 |
| [58] | NOP with SSD/150 | |
| Social network * | [60] | NOP with SSD/510 |
| Existent low ability ** | [56] | NOP with SSD/510 |
| [20] | OP and NOP with schizophrenia/70 | |
| Legal supervision 1 | [20] | OP and NOP with schizophrenia/70 |
| Psychiatric Data | ||
| Age of onset of illness | [56] | NOP with SSD/510 |
| [61] | NOP with SSD/156 | |
| [58] | NOP with SSD 150 | |
| [16] | OP with SSD/356 | |
| Comorbid alcohol use disorder | [10] | n.a. (systematic review) |
| [20] | OP and NOP with schizophrenia/70 | |
| [62] | Inmates/1212 | |
| Comorbid substance use disorder | [10] | n.a. (systematic review) |
| [62] | Inmates/1212 | |
| [20] | OP and NOP with schizophrenia/70 | |
| Comorbid personality disorder | [62] | Inmates/1212 |
| Previous psychiatric treatment Inpatient outpatient | [20] | OP and NOP with schizophrenia/70 |
| Previous compulsory measures | - | - |
| Cognitive impairment | [63] | Inmates/254 |
| Delusions | [56] | NOP with SSD/510 |
| Hallucinations | [64] | NOP with psychosis/290 |
| Penetrability of own ego | - | - |
| Disorders of affect/drive | [65] | NOP with SSD/59 |
| [66] | NOP with psychotic disorder/45 | |
| Negative symptoms | [66] | NOP with psychotic disorder/45 |
| [67] | NOP with SSD/332 | |
| PANSS: P1–P7 1 | [64] | NOP with psychosis/290 |
| [38] | NOP with SSD/40 | |
| [58] | NOP with SSD/150 | |
| PANSS: N1–N7 2 | [57] | NOP with SSD + depression/132 |
| [58] | NOP with SSD/150 | |
| PANSS: G1–G16 3 | [68] | NOP with first-episode psychosis/101 |
| [64] | NOP with psychosis/290 | |
| [58] | NOP with SSD/150 | |
| PANSS: total 4 | [64] | NOP with psychosis/290 |
| [57] | NOP with SSD + depression/132 | |
| [16] | OP with SSD/356 | |
| Previous suicide attempts | [64] | NOP with psychosis/290 |
| [57] | NOP with SSD + depression/132 | |
| [69] | NOP with SSD/51 | |
| [20] | OP and NOP with schizophrenia/70 | |
| [59] | OP with SSD/223 | |
| History of self-harm | [70] | NOP with SSD/57 |
| History of endangerment of others | [71] | OP/96 |
| [72] | OP/266 | |
| Data reg. pharmacotherapy | ||
| Regular intake of medication as prescribed | [38] | NOP with SSD/40 |
| Antipsychotic polypharmacy (>2 substances) | [73] | NOP with SSD/1611 |
| Prescription of antidepressants | [73] | NOP with SSD/1611 |
| Other | ||
| Pre-existing physical disorder 1 | [56] | NOP with SSD/510 |
* at the time of the investigated offence resp. at the time of admission to referenced hospitalization. ** later omitted due to missing values ≥ 33%. 1 P1 = delusions, P2 = conceptual disorganization, P3 = hallucinatory behaviour, P4 = excitement, P5 = grandiosity, P6 = suspiciousness, P7 = hostility. 2 N1 = blunted affect, N2 = emotional withdrawal, N3 = poor rapport, N4 = passive-apathetic social withdrawal, N5 = difficulty in abstract thinking, N6 = lack of spontaneity and flow of conversation, N7 = stereotyped thinking. 3 G1 = somatic concern, G2 = anxiety, G3 = guilt feelings, G4 = tension, G5 = mannerism and posturing, G6 = depression, G7 = motor retardation, G8 = uncooperativeness, G9 = unusual thought content, G10 = disorientation, G11 = poor attention, G12 = lack of judgement and insight, G13 = disturbance of volition, G14 = poor impulse control, G15 = preoccupation, G16 = active social avoidance. 4 total score of all P-, N- and G-items, range = 30–210.
Appendix B. Detailed List of Investigated Predictor Variables
| Variable Code | Label | Definition |
| SD1 | Age at admission? | Age (in years and months) at the date of admission to the referenced hospital |
| SD2 | Gender? | As indicated in the file |
| SD3a | Country of birth: Switzerland? | As indicated in the file |
| SD5b | Marital Status: single | Yes, if he/she was unmarried at the time of the offence, respectively, the admission to the referenced hospitalization |
| SD6a | Living situation: psychiatric living measure | Yes, if, at the time of the offence, respectively, the admission to the referenced hospitalization, he/she was an inpatient or a semi-inpatient in a mental health care institution |
| SD6b | Living situation: complementary facility | Yes, if, at the time of the offence, respectively, the admission to the referenced hospitalization, he/she lived in any type of community-based dwelling equipped with support staff which provided at least a minimum housing standard (does not include homeless shelters) |
| SD6c | Living situation: home alone | Yes, if, at the time of the offence, respectively, the admission to the referenced hospitalization, he/she lived on his/her own in any type of community-based dwelling without support staff which provided at least the minimum housing standard |
| SD6d | Living situation: home with others | Yes, if item SD6e and/or SD6f applies AND/OR if, at the time of the offence, respectively, the admission to the referenced hospitalization, he/she lived with one or more person(s) in any type of community-based dwelling without support staff which provided at least the minimum housing standard |
| SD6e | Living situation: at parents | Yes, if, at the time of the offence, respectively, the admission to the referenced hospitalization, he/she lived with one or both legal parent(s) in any type of community-based dwelling which provided at least the minimum housing standard |
| SD6f | Living situation: with relatives | Yes, if item SD6e applies AND/OR if, at the time of the offence, respectively, the admission to the referenced hospitalization, he/she lived with one or more relative(s)/person(s) in law in any type of community-based dwelling which provided at least the minimum housing standard |
| SD6g | Living situation: homeless | Yes, if, at the time of the offence, respectively the admission to the referenced hospitalization, he/she lived in a place which was below the minimum housing standard AND had no access to an adequate dwelling |
| SD6i | Living situation: other | Yes, if, at the time of the offence, respectively, the admission to the referenced hospitalization, none of the items SD6a-SD6g applies |
| SD7a | Highest graduation: no compulsory school | Yes, if he/she had not completed primary or (lower) secondary school education (school period from about age 6 to about age 16) at the time of the investigated offence, respectively, the admission to the referenced hospitalization |
| SD7b | Highest graduation: compulsory school | Yes, if he/she had completed primary AND (lower) secondary school education (school period from about age 6 to about age 16) at the time of the investigated offence, respectively, the admission to the referenced hospitalization |
| SD7c | Type of graduation | His/her highest completed level of education at the time of the investigated offence, respectively, the admission to the referenced hospitalization: (1) no graduation (2) primary school (3) secondary school (4) gymnasium (5) vocational school (6) “Fachmittelschule” (technical school) (7) college (8) university degree (9) other |
| SD7d | Highest graduation: college/university | Yes, if he/she had graduated from college and/or university and/or another higher education institution (e.g., university of applied sciences) at the time of the investigated offence, respectively, the admission to the referenced hospitalization |
| PH1 | Age at which the F2x diagnosis was given? | Age (in years) at which the patient was diagnosed with any schizophrenia spectrum disorder for the first time (ICD-10: F2x.x) |
| PH2 | Age at which the patient showed first symptoms of the F2x diagnosis? | Age (in years) at which he/she showed any of the symptoms that are described in the ICD-10 under the corresponding F2x.x diagnosis (see item PH1) for the first time; unless the symptoms can be better explained by other causes (e. g. substance consumption) |
| PH3 | History of delusions | Yes, if he/she (had) experienced any type of delusion (persecutory delusions, delusions of grandeur). ‘Delusion’ was defined as “a false belief based on incorrect inference about external reality that is firmly sustained despite what almost everybody else believes and despite what constitutes incontrovertible and obvious proof or evidence to the contrary. The belief is not one ordinarily accepted by other members of the person’s culture or subculture (e.g., it is not an article of religious faith)” |
| PH4 | History of hallucinations | Yes, if he/she (had) experienced any visual, auditory, olfactory, tactile, and/or gustatory hallucinations. |
| PH5 | History of penetrability of the own ego | Yes, if he/she (had) experienced any of the following: thought insertion, thought withdrawal, thought broadcasting, thought echo, depersonalisation, derealisation and/or delusions of control |
| PH6 | History of disorders of affect or drive | Yes, if he/she (had) experienced any mania- and/or depression-like symptoms with the consequence of any type of functional impairment (distress and/or disability) |
| PH7 | History of negative symptoms | Yes, if he/she (had) experienced any types of negative symptoms which are listed in the positive and negative syndrome scale (PANSS), which cannot be better explained by other causes (such as another mental illness) |
| PH10a | History of suicide attempts | Yes, if he/she had harmed himself/herself intentionally with suicidal intent at any one time before the investigated offence, respectively, the time of the referenced hospitalization |
| PH11a | History of endangerment of others | Yes, if, at any one time before the investigated offence, respectively, the referenced hospitalization, he/she had deliberately or negligently put one or more person(s) at any type of risk (e.g., by the exertion of violence), which entailed the potential or actual consequence of a substantial mental and/or physical impairment of the corresponding person(s) |
| PH12a | Was there ever any compulsory measure during a hospitalization used? | Yes, if one or more of the following measures had been forced upon the patient in a psychiatric hospital at any one time before the investigated offence, respectively, the referenced hospitalization:
|
| PH13 | Alcohol abuse | Yes, if he/she (had) had an alcohol consumption pattern corresponding to the ICD-10 diagnosis “Harmful use (F10.1)” or “Dependence syndrome (F10.2x)” at the time of or at any one time before the investigated offence, respectively, the referenced hospitalization |
| PH14a | Drug abuse | Yes, if he/she did not have and had not had a substance consumption pattern corresponding to the ICD-10 diagnosis “Harmful use (F1x.1)” or “Dependence syndrome (F1x.2x)” at the time of and at any one time before the investigated offence, respectively, the referenced hospitalization. In this item, the term ‘substance’ refers to illicit drugs and prescription medications but not to alcohol. |
| PH14b | Cannabis abuse/-dependence? | Yes, if he/she (had) had a cannabinoid consumption pattern corresponding to the ICD-10 diagnosis “Harmful use (F12.1)” or “Dependence syndrome (F12.2x)” at the time of or at any one time before the investigated offence, respectively, the referenced hospitalization |
| PH15a | Presence of a personality disorder (PD)? | Yes, if he/she had ever been diagnosed with any personality disorder listed in the ICD-10 (F60.x, F61) and/or the DSM-V |
| PH18a | Any outpatient psychiatric treatment(s)? | Yes, if he/she had visited a mental health care provider (psychologist and/or psychiatrist) as an outpatient at any time before the investigated offence, respectively, the referenced hospitalization, regardless of the duration of said treatment |
| PH19a | Any inpatient psychiatric treatment(s)? | Yes, if he/she had been an inpatient and/or a semi-inpatient in a mental health care institution at any time before the investigated offence, respectively, the referenced hospitalization, regardless of the duration of said treatment |
| PH22a | Was the patient ever compulsorily admitted? | Yes, if he/she had been involuntarily admitted to any mental health care institution by order of an authorised person (such as a physician) at any one time before the investigated offence, respectively, the referenced hospitalization. Compulsory admission is defined as application of the Swiss “Fürsorgerische Unterbringung (FU)” OR “Fürsorgerischer Freiheitsentzug (FFE)” according to the Swiss child and adult protection law (KESR). |
| PH23p | Regular intake of antipsychotic medication | Yes, if he/she, mental health professionals and trusted private persons (e.g., close family members) had not reported/documented a lack of compliance/adherence to any antipsychotic medications at any time before the investigated offence AND if mental health professionals and trusted private persons (e.g., close family members) had not had reasonable grounds for suspecting that the patient lacked medication compliance/adherence to any antipsychotic medications at any time before the investigated offence, respectively, the referenced hospitalization. |
| N2 | Global cognitive deficits | Yes, if any report in the file states that he/she had shown deficits in any of the domains “general intelligence” (N1b), “attention”, “verbal memory”, “verbal fluency”, “verbal learning and memory” or “executive functioning” (adopted from Bowie and Harvey, 2006, p.532–533) for a period of at least 1 year before admission to the referenced hospitalization |
| S1 | Does/did the patient have satisfying friendships? | Yes, if, at the time of admission to the referenced hospital, he/she reported to have had AND to still have at least one good friend who is not related to him/her Note: relationships with intimate partners were excluded in this item |
| S2 | Does/did the patient have a satisfying relationship with his parents? | Yes, if, at the time of admission to the referenced hospital, he/she reported to have had AND to still have a good relationship with at least one of his/her parents OR, if the corresponding parent(s) had passed away, to have had a good relationship with the deceased parent(s) |
| S5 | Does/did the patient suffer from social isolation? | Yes, if he/she had suffered from social isolation for a period of at least 1 year before admission to the referenced hospital Note: Signs of social isolation include “small social networks, infrequent social contacts, absence of confidante connections, living alone, and lack of participation in social activities” |
| R9b | Polypharmacy at admission | Yes, if his/her prescription schedule included two or more different antipsychotics on the date of admission to the referenced hospital (does not include antipsychotics which were prescribed on the date of admission itself) |
| R9f | Polypharmacy at discharge | Yes, if his/her prescription schedule included two or more different antipsychotics at the time of discharge from the referenced hospital |
| R9l | Additional Antidepressant prescribed | Yes, if his/her prescription schedule included two or more different antipsychotics at the time of discharge from the referenced hospital AND if his/her prescription schedule included any antidepressant at the time of discharge from the referenced hospital Note: Herbal and homeopathic remedies are not considered in this item |
| R10 | Was the patient ever suicidal during the referenced hospitalization? | Yes, if he/she reported that he/she has experienced active suicidal ideation at any one time during the referenced hospitalisation AND/OR if he/she attempted suicide during the current hospitalisation (see item R12) |
| R11 | Did the patient ever show any self-harming behaviour during the referenced hospitalization? | Yes, if he/she intentionally harmed himself/herself (by cutting, burning, or other means) at any one time during the referenced hospitalisation (including self-harming behaviour with suicidal intent (see item R12)) |
| R12 | Did the patient ever attempt suicide during the referenced hospitalization? | Yes, if he/she intentionally harmed himself/herself with suicidal intent at any one time during the referenced hospitalisation |
| R20b/c | Did the patient ever show any endangerment of others during the referenced hospitalization? | Yes, if he/she showed any physical or verbal aggressions towards one or more staff member(s) or one or more patient(s) at any one time during the referenced hospitalization Note: Aggression is defined as “a behaviour that is intended to harm another person who Is motivated to avoid that harm” |
| PA1 | PANSS at admission: Scale Delusion | Score in the PANSS item ‘delusion’ at the time of admission to the referenced hospital |
| PA2 | PANSS at admission: Scale Conceptual disorganization | Score in the PANSS item ‘conceptual disorganisation’ at the time of admission to the referenced hospital |
| PA3 | PANSS at admission: Scale Hallucinations | Score in the PANSS item ‘hallucinations’ at the time of admission to the referenced hospital |
| PA4 | PANSS at admission: Scale Hyperactivity | Score in the PANSS item ‘hyperactivity’ at the time of admission to the referenced hospital |
| PA5 | PANSS at admission: Scale Grandiosity | Score in the PANSS item ‘grandiosity’ at the time of admission to the referenced hospital |
| PA6 | PANSS at admission: Scale suspiciousness/persecution | Score in the PANSS item ‘suspiciousness/persecution’ at the time of admission to the referenced hospital |
| PA7 | PANSS at admission: Scale Hostility | Score in the PANSS item ‘hostility’ at the time of admission to the referenced hospital |
| PA8 | PANSS at admission: Scale Blunted affect | Score in the PANSS item ‘blunted affect’ at the time of admission to the referenced hospital |
| PA9 | PANSS at admission: Scale Emotional withdrawal | Score in the PANSS item ‘emotional withdrawal’ at the time of admission to the referenced hospital |
| PA10 | PANSS at admission: Scale Poor rapport | Score in the PANSS item ‘poor rapport’ at the time of admission to the referenced hospital |
| PA11 | PANSS at admission: Scale Passive/apathetic social withdrawal | Score in the PANSS item ‘passive/apathetic social withdrawal’ at the time of admission to the referenced hospital |
| PA12 | PANSS at admission: Scale Difficulty in abstract thinking | Score in the PANSS item ‘difficulty in abstract thinking’ at the time of admission to the referenced hospital |
| PA13 | PANSS at admission: Scale Lack of spontaneity and flow of conversation | Score in the PANSS item ‘lack of spontaneity and flow of conversation’ at the time of admission to the referenced hospital |
| PA14 | PANSS at admission: Scale Stereotyped thinking | Score in the PANSS item ‘stereotyped thinking’ at the time of admission to the referenced hospital |
| PA15 | PANSS at admission: Scale Somatic concern | Score in the PANSS item ‘somatic concern’ at the time of admission to the referenced hospital |
| PA16 | PANSS at admission: Scale Anxiety | Score in the PANSS item ‘anxiety’ at the time of admission to the referenced hospital |
| PA17 | PANSS at admission: Scale Guilt feelings | Score in the PANSS item ‘guilt feelings’ at the time of admission to the referenced hospital |
| PA18 | PANSS at admission: Scale Tension | Score in the PANSS item ‘tension’ at the time of admission to the referenced hospital |
| PA19 | PANSS at admission: Scale Mannerisms and posturing | Score in the PANSS item ‘mannerism and posturing’ at the time of admission to the referenced hospital |
| PA20 | PANSS at admission: Scale Depression | Score in the PANSS item ‘depression’ at the time of admission to the referenced hospital |
| PA21 | PANSS at admission: Scale Motor retardation | Score in the PANSS item ‘motor retardation’ at the time of admission to the referenced hospital |
| PA22 | PANSS at admission: Scale Uncooperativeness | Score in the PANSS item ‘uncooperativeness’ at the time of admission to the referenced hospital |
| PA23 | PANSS at admission: Scale Unusual thought content | Score in the PANSS item ‘unusual thought content’ at the time of admission to the referenced hospital |
| PA24 | PANSS at admission: Scale Disorientation | Score in the PANSS item ‘disorientation’ at the time of admission to the referenced hospital |
| PA25 | PANSS at admission: Scale Poor attention | Score in the PANSS item ‘poor attention’ at the time of admission to the referenced hospital |
| PA26 | PANSS at admission: Scale Lack of judgement and insight | Score in the PANSS item ‘lack of judgement and insight’ at the time of admission to the referenced hospital |
| PA27 | PANSS at admission: Scale Disturbance of volition | Score in the PANSS item ‘disturbance of volition’ at the time of admission to the referenced hospital |
| PA28 | PANSS at admission: Scale Poor impulse control | Score in the PANSS item ‘poor impulse control’ at the time of admission to the referenced hospital |
| PA29 | PANSS at admission: Scale Preoccupation | Score in the PANSS item ‘preoccupation’ at the time of admission to the referenced hospital |
| PA30 | PANSS at admission: Scale Active social avoidance | Score in the PANSS item ‘active social avoidance’ at the time of admission to the referenced hospital |
| PA_A | PANNS Score at admission | PANSS total score at the time of admission to the referenced hospital |
| PA32 | PANSS at discharge: Scale Delusion | Score in the PANSS item ‘delusion’ at the time of discharge from the referenced hospital |
| PA33 | PANSS at discharge: Scale Conceptual disorganization | Score in the PANSS item ‘conceptual disorganisation’ at the time of discharge from the referenced hospital |
| PA34 | PANSS at discharge: Scale Hallucinations | Score in the PANSS item ‘hallucinations’ at the time of discharge from the referenced hospital |
| PA35 | PANSS at discharge: Scale Hyperactivity | Score in the PANSS item ‘hyperactivity’ at the time of discharge from the referenced hospital |
| PA36 | PANSS at discharge: Scale Grandiosity | Score in the PANSS item ‘grandiosity’ at the time of discharge from the referenced hospital |
| PA37 | PANSS at discharge: Scale Suspiciousness/persecution | Score in the PANSS item ‘suspiciousness/persecution’ at the time of discharge from the referenced hospital |
| PA38 | PANSS at discharge: Scale Hostility | Score in the PANSS item ‘hostility’ at the time of discharge from the referenced hospital |
| PA39 | PANSS at discharge: Scale Blunted affect | Score in the PANSS item ‘blunted affect’ at the time of discharge from the referenced hospital |
| PA40 | PANSS at discharge: Scale Emotional withdrawal | Score in the PANSS item ‘emotional withdrawal’ at the time of discharge from the referenced hospital |
| PA41 | PANSS at discharge: Scale Poor rapport | Score in the PANSS item ‘poor rapport’ at the time of discharge from the referenced hospital |
| PA42 | PANSS at discharge: Passive/apathetic social withdrawal | Score in the PANSS item ‘passive/apathetic social withdrawal’ at the time of discharge from the referenced hospital |
| PA43 | PANSS at discharge: Scale Difficulty in abstract thinking | Score in the PANSS item ‘difficulty in abstract thinking’ at the time of discharge from the referenced hospital |
| PA44 | PANSS at discharge: Scale Lack of spontaneity and flow of conversation | Score in the PANSS item ‘spontaneity and flow of conversation’ at the time of discharge from the referenced hospital |
| PA45 | PANSS at discharge: Scale Stereotyped thinking | Score in the PANSS item ‘stereotyped thinking’ at the time of discharge from the referenced hospital |
| PA46 | PANSS at discharge: Scale Somatic concern | Score in the PANSS item ‘somatic concern’ at the time of discharge from the referenced hospital |
| PA47 | PANSS at discharge: Scale Anxiety | Score in the PANSS item ‘anxiety’ at the time of discharge from the referenced hospital |
| PA48 | PANSS at discharge: Scale Guilt feelings | Score in the PANSS item ‘guilt feelings’ at the time of discharge from the referenced hospital |
| PA49 | PANSS at discharge: Scale Tension | Score in the PANSS item ‘tension’ at the time of discharge from the referenced hospital |
| PA50 | PANSS at discharge: Scale Mannerisms and posturing | Score in the PANSS item ‘mannerisms and posturing’ at the time of discharge from the referenced hospital |
| PA51 | PANSS at discharge: Scale Depression | Score in the PANSS item ‘depression’ at the time of discharge from the referenced hospital |
| PA52 | PANSS at discharge: Scale Motor retardation | Score in the PANSS item ‘motor retardation’ at the time of discharge from the referenced hospital |
| PA53 | PANSS at discharge: Scale Uncooperativeness | Score in the PANSS item ‘uncooperativeness’ at the time of discharge from the referenced hospital |
| PA54 | PANSS at discharge: Scale Unusual thought content | Score in the PANSS item ‘unusual thought content’ at the time of discharge from the referenced hospital |
| PA55 | PANSS at discharge: Scale Disorientation | Score in the PANSS item ‘disorientation’ at the time of discharge from the referenced hospital |
| PA56 | PANSS at discharge: Scale Poor attention | Score in the PANSS item ‘poor attention’ at the time of discharge from the referenced hospital |
| PA57 | PANSS at discharge: Scale Lack of judgement and insight | Score in the PANSS item ‘lack of judgement and insight’ at the time of discharge from the referenced hospital |
| PA58 | PANSS at discharge: Scale Disturbance of volition | Score in the PANSS item ‘disturbance of volition’ at the time of discharge from the referenced hospital |
| PA59 | PANSS at discharge: Scale Poor impulse control | Score in the PANSS item ‘poor impulse control’ at the time of discharge from the referenced hospital |
| PA60 | PANSS at discharge: Scale Preoccupation | Score in the PANSS item ‘Preoccupation’ at the time of discharge from the referenced hospital |
| PA61 | PANSS at discharge: Scale Active social avoidance | Score in the PANSS item ‘active social avoidance’ at the time of discharge from the referenced hospital |
| PAS62 | PANNS Score at discharge | PANSS total score at the time of discharge from the referenced hospital |
References
- Charlson, F.J.; Ferrari, A.J.; Santomauro, D.F.; Diminic, S.; Stockings, E.; Scott, J.G.; McGrath, J.J.; Whiteford, H.A. Global Epidemiology and Burden of Schizophrenia: Findings from the Global Burden of Disease Study 2016. Schizophr. Bull. 2018, 44, 1195–1203. [Google Scholar] [CrossRef] [PubMed]
- Laursen, T.M.; Nordentoft, M.; Mortensen, P.B. Excess early mortality in schizophrenia. Annu. Rev. Clin. Psychol. 2014, 10, 425–448. [Google Scholar] [CrossRef] [PubMed]
- Yung, N.C.L.; Wong, C.S.M.; Chan, J.K.N.; Chen, E.Y.H.; Chang, W.C. Excess Mortality and Life-Years Lost in People with Schizophrenia and Other Non-affective Psychoses: An 11-Year Population-Based Cohort Study. Schizophr. Bull. 2021, 47, 474–484. [Google Scholar] [CrossRef] [PubMed]
- Olfson, M.; Gerhard, T.; Huang, C.; Crystal, S.; Stroup, T.S. Premature Mortality Among Adults with Schizophrenia in the United States. JAMA Psychiatry 2015, 72, 1172–1181. [Google Scholar] [CrossRef]
- Bai, W.; Liu, Z.H.; Jiang, Y.Y.; Zhang, Q.E.; Rao, W.W.; Cheung, T.; Hall, B.J.; Xiang, Y.T. Worldwide prevalence of suicidal ideation and suicide plan among people with schizophrenia: A meta-analysis and systematic review of epidemiological surveys. Transl. Psychiatry 2021, 11, 552. [Google Scholar] [CrossRef]
- Dutta, R.; Murray, R.M.; Hotopf, M.; Allardyce, J.; Jones, P.B.; Boydell, J. Reassessing the long-term risk of suicide after a first episode of psychosis. Arch. Gen. Psychiatry 2010, 67, 1230–1237. [Google Scholar] [CrossRef]
- Hor, K.; Taylor, M. Suicide and schizophrenia: A systematic review of rates and risk factors. J. Psychopharmacol. 2010, 24 (Suppl. S4), 81–90. [Google Scholar] [CrossRef]
- Baillargeon, J.; Binswanger, I.A.; Penn, J.V.; Williams, B.A.; Murray, O.J. Psychiatric disorders and repeat incarcerations: The revolving prison door. Am. J. Psychiatry 2009, 166, 103–109. [Google Scholar] [CrossRef]
- Voulgaris, A.; Kielisch, S.; Konrad, N.; Opitz-Welke, A. Suizide im Gefängnis und im Maßregelvollzug-eine Berliner Vergleichsstudie. Recht. Psychiatr. 2018, 36, 15–20. [Google Scholar]
- Hawton, K.; Sutton, L.; Haw, C.; Sinclair, J.; Deeks, J.J. Schizophrenia and suicide: Systematic review of risk factors. Br. J. Psychiatry 2005, 187, 9–20. [Google Scholar] [CrossRef]
- Fazel, S.; Cartwright, J.; Norman-Nott, A.; Hawton, K. Suicide in prisoners: A systematic review of risk factors. J. Clin. Psychiatry 2008, 69, 1721–1731. [Google Scholar] [CrossRef]
- Conner, K.R.; Cox, C.; Duberstein, P.R.; Tian, L.; Nisbet, P.A.; Conwell, Y. Violence, alcohol, and completed suicide: A case-control study. Am. J. Psychiatry 2001, 158, 1701–1705. [Google Scholar] [CrossRef] [PubMed]
- Gvion, Y.; Apter, A. Aggression, impulsivity, and suicide behavior: A review of the literature. Arch. Suicide Res. 2011, 15, 93–112. [Google Scholar] [CrossRef] [PubMed]
- Zhong, S.; Senior, M.; Yu, R.; Perry, A.; Hawton, K.; Shaw, J.; Fazel, S. Risk factors for suicide in prisons: A systematic review and meta-analysis. Lancet Public Health 2021, 6, e164–e174. [Google Scholar] [CrossRef] [PubMed]
- Webb, R.T.; Qin, P.; Stevens, H.; Mortensen, P.B.; Appleby, L.; Shaw, J. National study of suicide in all people with a criminal justice history. Arch. Gen. Psychiatry 2011, 68, 591–599. [Google Scholar] [CrossRef] [PubMed]
- Kappes, J.R.; Huber, D.A.; Kirchebner, J.; Sonnweber, M.; Günther, M.P.; Lau, S. Self-Harm Among Forensic Psychiatric Inpatients with Schizophrenia Spectrum Disorders: An Explorative Analysis. Int J. Offender Comp. Criminol. 2021, 306624x211062139. [Google Scholar] [CrossRef] [PubMed]
- Žarkovic Palijan, T.; Mužinić, L.; Radeljak, S. Psychiatric comorbidity in forensic psychiatry. Psychiatr. Danub. 2009, 21, 429–436. [Google Scholar]
- Goethals, K.R.; Vorstenbosch, E.C.; van Marle, H.J. Diagnostic comorbidity in psychotic offenders and their criminal history: A review of the literature. Int. J. Forensic. Ment. Health 2008, 7, 147–156. [Google Scholar] [CrossRef]
- Gunn, J.; Taylor, P.; Hutcheon, I.D. Forensic Psychiatry: Clinical, Legal and Ethical Issues; CRC Press: Boca Raton, FL, USA, 2014. [Google Scholar]
- Landgraf, S.; Blumenauer, K.; Osterheider, M.; Eisenbarth, H. A clinical and demographic comparison between a forensic and a general sample of female patients with schizophrenia. Psychiatry Res. 2013, 210, 1176–1183. [Google Scholar] [CrossRef]
- Fazel, S.; Gulati, G.; Linsell, L.; Geddes, J.R.; Grann, M. Schizophrenia and violence: Systematic review and meta-analysis. PLoS Med. 2009, 6, e1000120. [Google Scholar] [CrossRef]
- World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems: Tenth Revision; World Health Organization: Geneva, Switzerland, 2004.
- Slee, V.N. The International Classification of Diseases: Ninth Revision (ICD-9); American College of Physicians: Philadelphia, PA, USA, 1978; pp. 424–426. [Google Scholar]
- Hsieh, H.-F.; Shannon, S.E. Three approaches to qualitative content analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef] [PubMed]
- Seifert, D. Die entwicklung des psychiatrischen massregelvollzzugs (§ 63StGB) in Nordrhein-Wesfalen. Psychiat Prax. 1997, 24, 237–244. [Google Scholar]
- Hofmann, L.A.; Lau, S.; Kirchebner, J. Advantages of Machine Learning in Forensic Psychiatric Research— Uncovering the Complexities of Aggressive Behavior in Schizophrenia. Appl. Sci. 2022, 12, 819. [Google Scholar]
- Kay, S.R.; Fiszbein, A.; Opler, L.A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 1987, 13, 261–276. [Google Scholar] [CrossRef] [PubMed]
- McKnight, P.E.; Najab, J. Mann-Whitney U Test. In The Corsini Encyclopedia of Psychology; Wiley Online Library: Hoboken, NY, USA, 2010; p. 1. [Google Scholar] [CrossRef]
- Bower, K.M. When to Use Fisher’s Exact Test; American Society for Quality: Milwaukee, WI, USA, 2003; Volume 2, pp. 35–37. [Google Scholar]
- Jiang, T.; Gradus, J.L.; Rosellini, A.J. Supervised Machine Learning: A Brief Primer. Behav. Ther. 2020, 51, 675–687. [Google Scholar] [CrossRef]
- Yarkoni, T.; Westfall, J. Choosing Prediction Over Explanation in Psychology: Lessons from Machine Learning. Perspect. Psychol. Sci. 2017, 12, 1100–1122. [Google Scholar] [CrossRef]
- Browne, M.W. Cross-Validation Methods. J. Math. Psychol. 2000, 44, 108–132. [Google Scholar] [CrossRef]
- Machetanz, L.; Günther, M.; Lau, S.; Kirchebner, J. High risk, high dose?—Pharmacotherapeutic prescription patterns of offender and non-offender patients with schizophrenia spectrum disorder. Biomedicines 2022, 10, 3243. [Google Scholar] [CrossRef]
- Kramer, M.S.; Vogel, W.H.; DiJohnson, C.; Dewey, D.A.; Sheves, P.; Cavicchia, S.; Little, P.; Schmidt, R.; Kimes, I. Antidepressants in ‘depressed’ schizophrenic inpatients. A controlled trial. Arch. Gen. Psychiatry 1989, 46, 922–928. [Google Scholar] [CrossRef]
- Mao, Y.M.; Zhang, M.D. Augmentation with antidepressants in schizophrenia treatment: Benefit or risk. Neuropsychiatr. Dis. Treat 2015, 11, 701–713. [Google Scholar] [CrossRef]
- Patchan, K.; Vyas, G.; Hackman, A.L.; Mackowick, M.; Richardson, C.M.; Love, R.C.; Wonodi, I.; Sayer, M.A.; Glassman, M.; Feldman, S.; et al. Clozapine in Reducing Aggression and Violence in Forensic Populations. Psychiatr. Q. 2018, 89, 157–168. [Google Scholar] [CrossRef]
- Hennen, J.; Baldessarini, R.J. Suicidal risk during treatment with clozapine: A meta-analysis. Schizophr. Res. 2005, 73, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Pompili, M.; Lester, D.; Grispini, A.; Innamorati, M.; Calandro, F.; Iliceto, P.; De Pisa, E.; Tatarelli, R.; Girardi, P. Completed suicide in schizophrenia: Evidence from a case-control study. Psychiatry Res. 2009, 167, 251–257. [Google Scholar] [CrossRef]
- Sher, L.; Kahn, R.S. Suicide in Schizophrenia: An Educational Overview. Medicina 2019, 55, 361. [Google Scholar] [CrossRef] [PubMed]
- Haller, R.; Kemmler, G.; Kocsis, E.; Maetzler, W.; Prunlechner, R.; Hinterhuber, H. Schizophrenia and violence. Results of a comprehensive inquiry in an Austrian providence. Nervenarzt 2001, 72, 859–866. [Google Scholar] [CrossRef]
- Habermeyer, E.; Wolff, R.; Gillner, M.; Strohm, R.; Kutscher, S. Patienten mit schizophrenen Störungen im psychiatrischen Maßregelvollzug. Der. Nervenarzt 2010, 81, 1117–1124. [Google Scholar] [CrossRef] [PubMed]
- Hachtel, H.; Harries, C.; Luebbers, S.; Ogloff, J.R. Violent offending in schizophrenia spectrum disorders preceding and following diagnosis. Aust. N. Z. J. Psychiatry 2018, 52, 782–792. [Google Scholar] [CrossRef]
- Barlati, S.; Nibbio, G.; Stanga, V.; Giovannoli, G.; Calzavara-Pinton, I.; Necchini, N.; Lisoni, J.; Deste, G.; Vita, A. Cognitive and clinical characteristics of offenders and non-offenders diagnosed with schizophrenia spectrum disorders: Results of the Recoviwel observational study. Eur. Arch. Psychiatry Clin. Neurosci. 2022, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Slotboom, J.; Hoppenbrouwers, S.S.; Bouman, Y.H.A.; in ’t Hout, W.; Sergiou, C.; van der Stigchel, S.; Theeuwes, J. Visual attention in violent offenders: Susceptibility to distraction. Psychiatry Res. 2017, 251, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Pennington, C.R.; Cramer, R.J.; Miller, H.A.; Anastasi, J.S. Psychopathy, depression, and anxiety as predictors of suicidal ideation in offenders. Death Stud. 2015, 39, 288–295. [Google Scholar] [CrossRef] [PubMed]
- Harmer, B.; Lee, S.; Duong, T.V.H.; Saadabadi, A. Suicidal Ideation. In StatPearls; StatPearls Publishing: Tampa, FL, USA, 2022. [Google Scholar]
- Temmingh, H.; Stein, D.J. Anxiety in Patients with Schizophrenia: Epidemiology and Management. CNS Drugs 2015, 29, 819–832. [Google Scholar] [CrossRef] [PubMed]
- Jovanović, N.; Podlesek, A.; Medved, V.; Grubišin, J.; Mihaljevic-Peleš, A.; Goran, T.; Lovretić, V. Association between psychopathology and suicidal behavior in schizophrenia. A cross-sectional study of 509 participants. Crisis 2013, 34, 374–381. [Google Scholar] [CrossRef] [PubMed]
- Carragher, N.; Krueger, R.F.; Eaton, N.R.; Slade, T. Disorders without borders: Current and future directions in the meta-structure of mental disorders. Soc. Psychiatry Psychiatr. Epidemiol. 2015, 50, 339–350. [Google Scholar] [CrossRef] [PubMed]
- Kröber, H.-L. Selbstbestimmung und Zwang in der Behandlung; Springer: Berlin/Heidelberg, Germany, 2019; Volume 13, pp. 1–3. [Google Scholar]
- Höfer, F.X.; Habermeyer, E.; Mokros, A.; Lau, S.; Gairing, S.K. The impact of legal coercion on the therapeutic relationship in adult schizophrenia patients. PLoS ONE 2015, 10, e0124043. [Google Scholar] [CrossRef]
- Bukten, A.; Stavseth, M.R. Suicide in prison and after release: A 17-year national cohort study. Eur. J. Epidemiol. 2021, 36, 1075–1083. [Google Scholar] [CrossRef]
- Radeloff, D.; Stoeber, F.; Lempp, T.; Kettner, M.; Bennefeld-Kersten, K. Murderers or thieves at risk? Offence-related suicide rates in adolescent and adult prison populations. PLoS ONE 2019, 14, e0214936. [Google Scholar] [CrossRef]
- Hartley, C.M.; Pettit, J.W.; Castellanos, D. Reactive Aggression and Suicide-Related Behaviors in Children and Adolescents: A Review and Preliminary Meta-Analysis. Suicide Life Threat. Behav. 2018, 48, 38–51. [Google Scholar] [CrossRef]
- Stratton, J.; Cobia, D.J.; Reilly, J.; Brook, M.; Hanlon, R.E. Differences in Neuropsychological Functioning Between Homicidal and Nonviolent Schizophrenia Samples. J. Forensic. Sci. 2018, 63, 1435–1443. [Google Scholar] [CrossRef]
- Ran, M.S.; Chen, E.Y.; Conwell, Y.; Chan, C.L.; Yip, P.S.; Xiang, M.Z.; Caine, E.D. Mortality in people with schizophrenia in rural China: 10-year cohort study. Br. J. Psychiatry 2007, 190, 237–242. [Google Scholar] [CrossRef]
- Montross, L.P.; Kasckow, J.; Golshan, S.; Solorzano, E.; Lehman, D.; Zisook, S. Suicidal ideation and suicide attempts among middle-aged and older patients with schizophrenia spectrum disorders and concurrent subsyndromal depression. J. Nerv. Ment. Dis. 2008, 196, 884–890. [Google Scholar] [CrossRef]
- Loas, G.; Azi, A.; Noisette, C.; Legrand, A.; Yon, V. Fourteen-year prospective follow-up study of positive and negative symptoms in chronic schizophrenic patients dying from suicide compared to other causes of death. Psychopathology 2009, 42, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Gazdag, G.; Belán, E.; Szabó, F.A.; Ungvari, G.S.; Czobor, P.; Baran, B. Predictors of suicide attempts after violent offences in schizophrenia spectrum disorders. Psychiatry Res. 2015, 230, 728–731. [Google Scholar] [CrossRef] [PubMed]
- Ran, M.S.; Chan, C.L.; Chen, E.Y.; Tang, C.P.; Lin, F.R.; Li, L.; Li, S.G.; Mao, W.J.; Hu, S.H.; Schwab, G.; et al. Mortality of geriatric and younger patients with schizophrenia in the community. Suicide Life Threat. Behav. 2008, 38, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Kuo, C.J.; Tsai, S.Y.; Lo, C.H.; Wang, Y.P.; Chen, C.C. Risk factors for completed suicide in schizophrenia. J. Clin. Psychiatry 2005, 66, 579–585. [Google Scholar] [CrossRef] [PubMed]
- Favril, L.; Indig, D.; Gear, C.; Wilhelm, K. Mental disorders and risk of suicide attempt in prisoners. Soc. Psychiatry Psychiatr. Epidemiol. 2020, 55, 1145–1155. [Google Scholar] [CrossRef]
- Vadini, F.; Calella, G.; Pieri, A.; Ricci, E.; Fulcheri, M.; Verrocchio, M.C.; De Risio, A.; Sciacca, A.; Santilli, F.; Parruti, G. Neurocognitive impairment and suicide risk among prison inmates. J. Affect Disord. 2018, 225, 273–277. [Google Scholar] [CrossRef] [PubMed]
- Fialko, L.; Freeman, D.; Bebbington, P.E.; Kuipers, E.; Garety, P.A.; Dunn, G.; Fowler, D. Understanding suicidal ideation in psychosis: Findings from the Psychological Prevention of Relapse in Psychosis (PRP) trial. Acta. Psychiatr. Scand. 2006, 114, 177–186. [Google Scholar] [CrossRef]
- Johnson, J.; Gooding, P.; Tarrier, N. Suicide risk in schizophrenia: Explanatory models and clinical implications, The Schematic Appraisal Model of Suicide (SAMS). Psychol. Psychother. Theory Res. Pract. 2008, 81, 55–77. [Google Scholar] [CrossRef]
- Jarbin, H.; von Knorring, A.-L. Suicide and suicide attempts in adolescent-onset psychotic disorders. Nord. J. Psychiatry 2004, 58, 115–123. [Google Scholar] [CrossRef]
- Fenton, W.S.; McGlashan, T.H.; Victor, B.J.; Blyler, C.R. Symptoms, subtype, and suicidality in patients with schizophrenia spectrum disorders. Am. J. Psychiatry 1997, 154, 199–204. [Google Scholar]
- Crumlish, N.; Whitty, P.; Kamali, M.; Clarke, M.; Browne, S.; McTigue, O.; Lane, A.; Kinsella, A.; Larkin, C.; O’Callaghan, E. Early insight predicts depression and attempted suicide after 4 years in first-episode schizophrenia and schizophreniform disorder. Acta Psychiatr. Scand. 2005, 112, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, J.M.; Mullee, M.A.; King, E.A.; Baldwin, D.S. Suicide in schizophrenia: A retrospective case-control study of 51 suicides. Schizophr. Bull. 2004, 30, 803–811. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pluck, G.; Lekka, N.P.; Sarkar, S.; Lee, K.H.; Bath, P.A.; Sharif, O.; Woodruff, P.W. Clinical and neuropsychological aspects of non-fatal self-harm in schizophrenia. Eur. Psychiatry 2013, 28, 344–348. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Swogger, M.T.; Walsh, Z.; Maisto, S.A.; Conner, K.R. Reactive and proactive aggression and suicide attempts among criminal offenders. Crim. Justice Behav. 2014, 41, 337–344. [Google Scholar] [CrossRef]
- Swogger, M.T.; You, S.; Cashman-Brown, S.; Conner, K.R. Childhood physical abuse, aggression, and suicide attempts among criminal offenders. Psychiatry Res. 2011, 185, 363–367. [Google Scholar] [CrossRef]
- Haukka, J.; Tiihonen, J.; Härkänen, T.; Lönnqvist, J. Association between medication and risk of suicide, attempted suicide and death in nationwide cohort of suicidal patients with schizophrenia. Pharmacoepidemiol. Drug Saf. 2008, 17, 686–696. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).