1. Background
Transient ischemic attack (TIA) and ischemic stroke are two of the leading causes of death and disability and presents a worldwide health care problem. Although post-traumatic stress disorder (PTSD) commonly occurs due to traumas caused by exposure to natural disasters or violence, [
1,
2], PTSD has also been investigated in patients that suffered from life-threatening medical conditions including ischemic cerebrovascular events, and the prevalence and correlates of PTSD after TIA or ischemic stroke have been investigated in previous studies [
3,
4,
5,
6,
7,
8]. The crude prevalence of PTSD after TIA or ischemic stroke was varied from 12.9–31% [
3,
4,
5,
6,
7,
8]. There are relatively few studies on PTSD after stroke, with conflicting results for many predictors of PTSD after stroke. By comparing the general demographic characteristics (age, sex, marital status, education level, ethnicity, etc.) and the impact degree of stroke between the post-traumatic stress disorder population and the non-post-traumatic stress disorder population, no consistent conclusion has been reached. This may be related to differences in traumatic experience between medical and non-medical PTSD [
9,
10,
11]. Participants with PTSD were more likely to have low compliance to medications than other participants [
4].
Apart from the lack of knowledge about the risk factors for PTSD after TIA and stroke, psychological mechanisms that can prevent PTSD development have not been investigated in TIA and stroke patients until now. There has been increasing research showing a link between attachment and PTSD [
12,
13,
14,
15,
16,
17,
18]. A study has begun to suggest that attachment insecurity is associated with the severity of symptoms of PTSD [
19]. Insecure attachment was also found to mediate PTSD in abused children, [
17] inflammatory bowel disease, [
13] and HIV patients [
15]. Attachment style in therapy may improve the quality of life and prognosis of the patients [
15,
20]. Rumination has also been shown to be associated with traumatic stress and may be a risk factor for PTSD [
20,
21,
22,
23]. Repeated rumination has been linked to PTSD in children after earthquakes, in first time postpartum women, and in employees who have experienced occupational accidents as well as firefighters [
24,
25,
26,
27,
28,
29].
Such research has shown that attachment and rumination were strongly and predictively associated with PTSD. Researchers have further discovered that rumination is a mediator of attachment to physical health and emotional regulation [
30,
31,
32,
33]. However, these associations were estimated in a general population, and whether this association still exists in patients suffering from TIA or stroke was ambiguous.
This study intends to explore the relationship between attachment, rumination, and PTSD in stroke patients as well as the impact on drug compliance, in order to provide some reference for early psychological nursing measures.
2. Methods
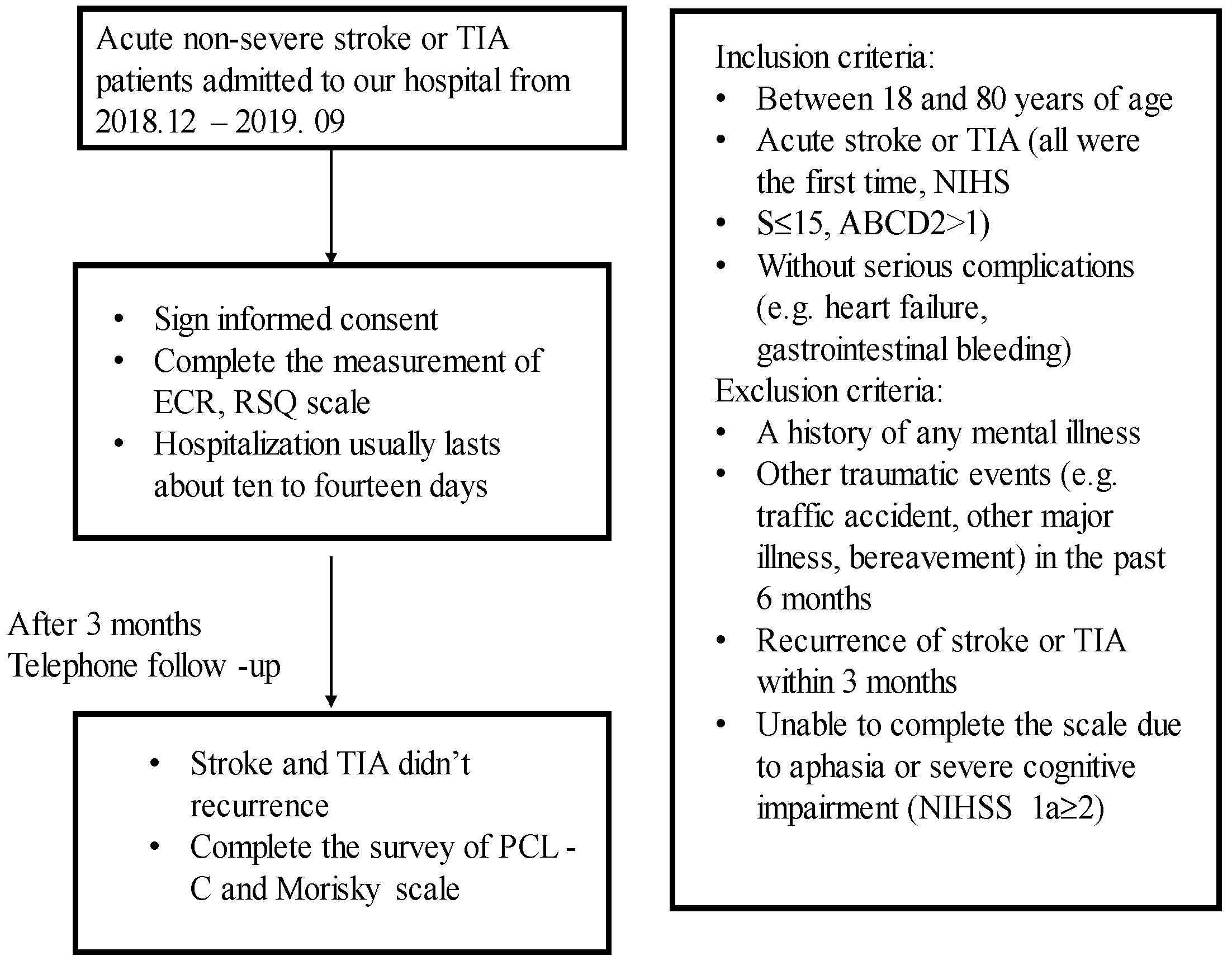
This study was a prospective longitudinal observational study of acute stroke and TIA patients. Three hundred participants were recruited at the Department of Neurology in The Second Hospital of Hebei Medical University, in the period from December 2018 to September 2019. This study was approved by the Research Ethics Committee of the Second Hospital of Hebei Medical University. The procedure of the study is described in
Figure 1. Patients were eligible if they were between 18 and 80 years of age and had acute stroke and TIA (all were first time, NIHSS total score ≤ 15, ABCD total score > 1) and those without serious complications such as heart failure and gastrointestinal bleeding. Key exclusion criteria were a history of any mental illness or other traumatic events (e.g., traffic accident, other major illness, bereavement) in the last 6 months or recurrence of stroke or TIA within 3 months or those who were unable to complete the scale due to aphasia or severe cognitive impairment. Patients and their families were given an oral and written explanation of the study and signed informed consent.
Eligible patients were assessed with either a National Institute of Health Stroke Scale (NIHSS), which assessed the patient for functional impairment, or an ABCD
2 score, which predicted stroke risk in TIA patients. Once included, patients were evaluated for attachment archetypes by the Relationships Scales Questionnaire (RSQ), attachment dimensions were measured by the Experiences in Close Relationships Inventory (ECR), and the Ruminative Responses Scale (RRS), which assessed the rumination dimensions were also measured [
34,
35]. The PTSD symptoms and medicine compliance were measured 3 months after stroke. The grade of PTSD symptomatology was assessed using a civilian version of PCL (PCL-C). It contains 17 items and screens in a variety of clinical settings [
34]. The Morisky Medication Adherence Scale (MMAS) is a 8-item scale, which is a simple and practical tool for evaluating medication compliance for discharged patients [
36].
In November 1994, according to DSM-W, the PTSD Checklist-Civilian Version (PCL-C) was created by the United States. Seventeen items are graded into five levels (not at all, a little, moderately, quite a lot, very much). It is a multi-dimensional observation tool for PTSD including re-experiencing, avoidance, numbing, and hyperarousal [
37]. The higher the cumulative score (17 to 85), the greater the likelihood of PTSD. A score of 17 to 37 indicates no significant PTSD symptoms, 38 to 49 means some degree of PTSD symptoms, and 50 to 85 shows a high level of PTSD symptoms. With respect to the MMAS, the first seven items are yes/no and the last is a 5-point rating [
38]. The scoring criteria are low adherence (<6), medium adherence (6–8), and high adherence (8) [
36]. Moreover, the patients’ age, sex, education, and occupation were also recorded.
Statistics were processed using SPSS version 20 (SPSS, Inc., Chicago, IL, USA). ANOVA was used to observe the differences in various indicators among subjects with different attachment types, PTSD degrees, and medication compliance. To test the mediational model, both the Sobel test and bootstrapping procedure were adopted.
3. Results
Among the 300 patients, 20 patients had cerebral infarction again, two were lost to follow-up, one had fracture surgery, one had cerebrovascular bypass surgery, and two had an incomplete questionnaire due to memory decline after stroke during 3 month follow-up. Therefore, 274 were effective, comprising 185 (67.9%) males (aged mean ± SD, 54.78 ± 10.58) and 88 (32.1%) females (aged mean ± SD, 58.95 ± 9.30). A total of 60% of the patients had an education level above primary school. A total of 253 patients had ischemic stroke, nine patients had hemorrhagic stroke, and 12 patients with TIA were included in the study.
The NIHSS score was the mean ± SD, 2.18 ± 2.47 and the ABCD
2 score was the mean ± SD, 2.58 ± 1.08). A total of 7.7% (21/274) of patients had significant PTSD. In addition, the low medication adherence was 149 (54.4%), the medium adherence was 118 (43.1%), the high adherence was 7 (2.5%). Sociodemographic information of the participants are summarized in
Supplementary Table S1 and Supplementary Figure S1.
3.1. Intercorrelations between Study Variables
The PTSD scores were significantly associated with attachment anxiety (r = 0.225,
p < 0.01), symptom rumination (r = 0.197,
p < 0.01), and obsessive thinking (r = 0.187,
p < 0.01). In addition, attachment anxiety was significantly associated with symptom rumination (r = 0.44,
p < 0.01) and obsessive thinking (r = 0.35,
p < 0.01). As for medication compliance, none of the measures were significantly correlated with it (
Table 1).
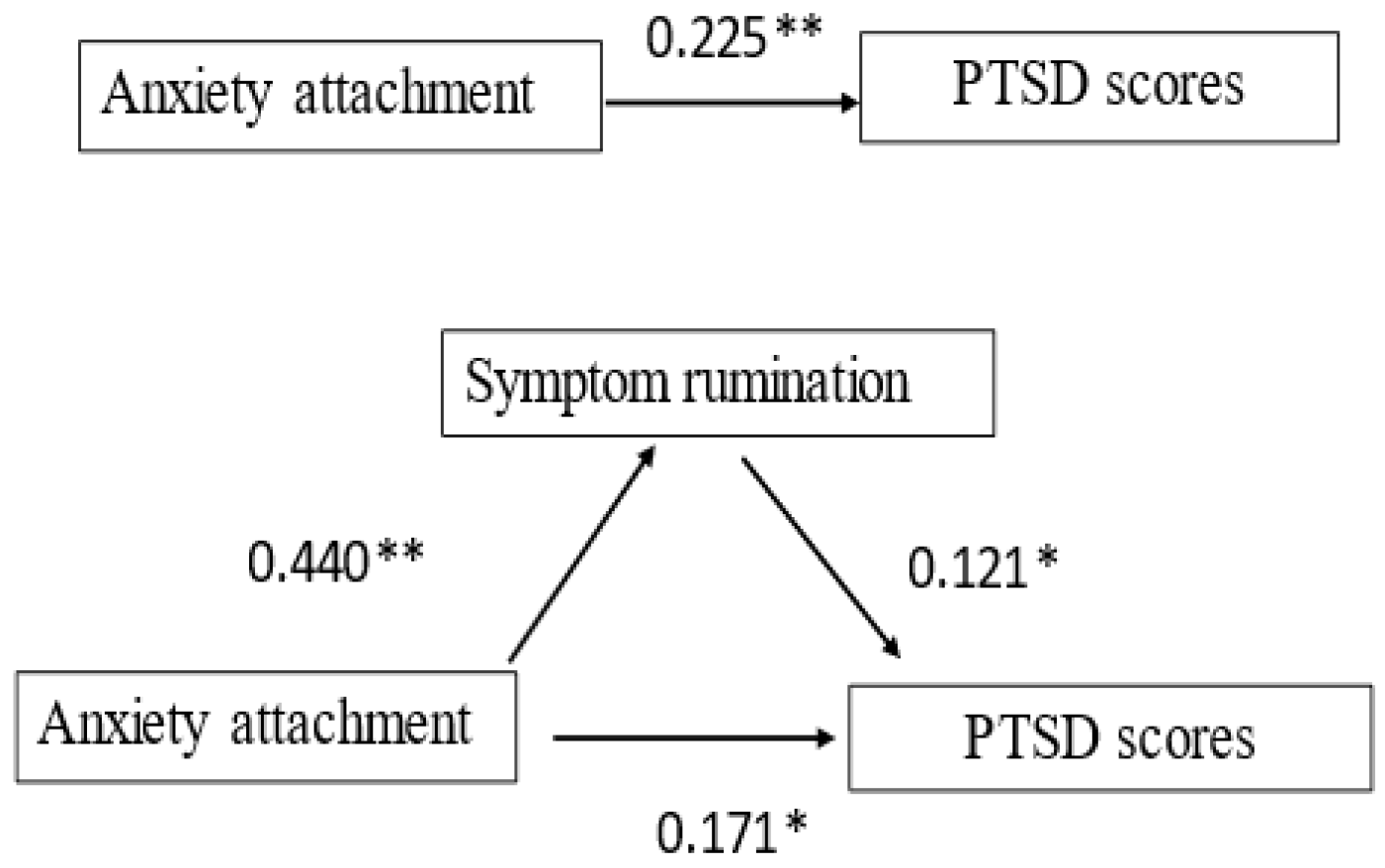
3.2. Mediation Analysis
To test the mediating effect, we employed the stepwise test regression coefficient method (Sobel test). In Model 1, attachment anxiety had a positive predictive effect on the PTSD scores (β = 0.225,
p < 0.01) (i.e., the higher the degree of attachment anxiety, the higher the PTSD score). In addition, attachment anxiety had a significant positive predictive effect on the mediating factor (symptom rumination) (Model 2, β = 0.440,
p < 0.01). From Model 3, it was found that the positive predictive effect of attachment anxiety on the PTSD scores decreased from β = 0.225 (
p < 0.01) to β = 0.171 (
p < 0.05) after the addition of symptomatic ruminant (
Table 2). According to the method of Baron and Kenny (1986) [
39], symptomatic ruminant mediates the relationship between attachment anxiety and PTSD (
Figure 2).
In Model 4 and Model 5, attachment anxiety had a positive predictive effect on the PTSD scores (β = 0.225,
p < 0.01) and the mediating factor (obsessive thinking) (Model 5, β = 0.281,
p < 0.01). From Model 6, it was found that the positive predictive effect of attachment anxiety on the PTSD scores decreased from β = 0.225 (
p < 0.01) to β = 0.215 (
p < 0.05) after the addition of obsessive thinking (
Table 3). According to the method by Baron and Kenny (1986) [
39], obsessive thinking mediates the relationship between attachment anxiety and PTSD (
Figure 3).
Bootstrap was used to test the mediating effect (Wen Zhonglin and Ye Baojuan, 2014) [
40]. The estimated mediating effect of symptom rumination between attachment anxiety and PTSD scores was 23.66% with a 95% confidence interval [0.279,3.074], indicating a significant mediating effect. In the meantime, the estimated mediating effect of the obsessive thinking between attachment anxiety and PTSD scores was 4.12%, with a 95% confidence interval [0.786,3.091], indicating a significant mediating effect.
4. Discussion
This study contributes to verification between attachment, rumination, and PTSD and, more explicitly, to examine the mediation where in the different dimensions of attachment could predict PTSD in stroke or TIA patients directly and indirectly through the role of specific ruminant regulatory processes. Furthermore, there have been no studies using mediating and moderating models of these variables in patients with stroke or TIA. Our findings provide areas for intervention in the clinical practice of stroke or TIA patients with PTSD.
As noted earlier, the results indicated that symptom rumination and obsessive thinking mediated the relationship between attachment anxiety and PTSD. In other words, stroke or TIA patients who tended to attachment anxiety also suffer more from PTSD, which was connected to symptom rumination and obsessive thinking. The occurrence of stroke and TIA caused more ineffective and problematic thinking among patients with higher attachment anxiety. In addition, anxious people tend to over activate their emotions and pain, and are more likely to be ruminating [
41]. Sudden neurological dysfunction is a physical and psychological trauma that may activate the patient’s attachment system. Differences in attachment styles affect how patients solve and express problems. Secure attachment can increase resilience, and patients will take the initiative to talk to others and seek help to protect themselves from the negative effects of trauma. However, patients with attachment anxiety repeatedly think about the experience of stroke or the impact of sequelae of stroke on life, which brings physical and mental discomfort to patients. Lias Bishop et al. suggested that rumination caused PTSD, and the underlying mechanism may be experiential avoidance [
23]. In conclusion, these results suggest that high attachment anxiety may be a risk factor for PTSD. When stroke and TIA occur suddenly, patients with attachment anxiety seem to experience symptom rumination and obsessive thinking, trying to cope with illness in an unhealthy way.
The results of this study indicated that neither adult attachment style nor rumination had a predictive effect on medication compliance, which was not consistent with other studies. It may be that medication compliance is more likely to be related to the patient’s age, underlying disease status, financial status, social support, disease level, disease awareness, and other factors.
This study has clear clinical implications. Since this study discovers that attachment style and rumination play a role in how individuals cope with PTSD following stroke or TIA, clinicians should focus on the patients’ attachment style and rumination and use them to guide treatment. Clinicians can provide patients with specific psychological education to reduce ruminative thoughts. Clinicians can provide patients with specific psychological education to reduce their ruminative thoughts. For example, medical staff should improve education work to make patients correctly understand the occurrence and prognosis of stroke. Second, mindful attention is an important modulator of the relationship between rumination and all aspects of PTSD symptoms. Therefore, mindfulness meditation is a promising basis for interventions. In recent years, there have been many efforts to prevent PTSD in the general population [
42,
43]. However, the prevention of PTSD after stroke is rare and there is no expert consensus on it. We still need to explore it in large samples.
We acknowledge several limitations inherent in this study. First, there is the fact that attachment styles vary with age. Then, the subjects included were mild and moderate stroke patients, while the patients with severe stroke were unable to complete the questionnaire. Our cohort was represented by patients with mild to moderate stroke, so was only a small proportion of patients with apparent PTSD. Findings require cautious interpretation. The correlations between the PTSD scores and the other variables is thus probably mostly influenced by the scores of the large number of patients with mild PTSD. This makes it difficult to make inferences about the small number of patients with significant PTSD symptoms. Therefore, the results of the study may not be generalizable to patients with severe stroke. Our results deserve further evaluation in a larger prospective cohort study. Additionally, the title of the adult attachment scale used in this study was translated from the English version, which is indeed difficult for elderly patients with stroke and TIA to understand. Meanwhile, there was no further search for the reason that each indicator was not correlated with drug compliance. These variations must be considered when interpreting the results of studies of PTSD after stroke.
5. Conclusions
In the stroke or TIA patients, the incidents of PTSD was 7.7%; Our study supports the underlying role of that symptom rumination and obsessive thinking mediated attachment anxiety plays in PTSD after TIA and stroke. Therefore, attention should be paid to the mental state of stroke patients in the early stage.
Author Contributions
K.Z. and L.Z. wrote the manuscript and prepared the tables. L.Z. modified the manuscript. T.L. and W.W. designed the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by the Beijing–Tianjin–Hebei Project (No. H2018206435) and the National Natural Science Foundation of China (82101490).
Institutional Review Board Statement
This study was approved by the ethics committee of The Second Hospital of Hebei Medical University, Shijiazhuang, China (Approval Code: 2018-P053; Approval Date: 22 August 2018).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The original contributions presented in the study are included in the article.
Acknowledgments
We thank all of the investigators and participants who contributed to these studies.
Conflicts of Interest
The authors declare that they have no competing interests.
Abbreviations
| TIA | Transient ischemic attack |
| PTSD | Post-traumatic stress disorder |
| NIHSS | National institute of Health Stroke Scale |
| RSQ | Relationships Scales Questionnaire |
| ECR | Experiences in Close Relationships Inventory |
| RRS | Ruminative Responses Scale |
| MMAS | Morisky Medication Adherence Scale |
| PCL-C | PTSD Checklist-Civilian Version |
References
- Boden, J.M.; Fergusson, D.M.; Horwood, L.J.; Mulder, R.T. The role of peri-traumatic stress and disruption distress in predicting post-traumatic stress disorder symptoms following exposure to a natural disaster. BJPsych Open 2015, 1, 81–86. [Google Scholar] [CrossRef]
- Birkley, E.L.; Eckhardt, C.I.; Dykstra, R.E. Posttraumatic Stress Disorder Symptoms, Intimate Partner Violence, and Relationship Functioning: A Meta-Analytic Review. J. Trauma. Stress 2016, 29, 397–405. [Google Scholar] [CrossRef]
- Goldfinger, J.Z.; Edmondson, D.; Kronish, I.M.; Fei, K.; Balakrishnan, R.; Tuhrim, S.; Horowitz, C.R. Correlates of Post-Traumatic Stress Disorder in Stroke Survivors. J. Stroke Cerebrovasc. Dis. 2014, 23, 1099–1105. [Google Scholar] [CrossRef]
- Kronish, I.M.; Edmondson, D.; Goldfinger, J.Z.; Fei, K.; Horowitz, C.R. Posttraumatic stress disorder and adherence to medications in survivors of strokes and transient ischemic attacks. Stroke 2012, 43, 2192–2197. [Google Scholar] [CrossRef]
- Favrole, P.; Jehel, L.; Levy, P.; Descombes, S.; Muresan, I.-P.; Manifacier, M.J.; Alamowitch, S. Frequency and predictors of post-traumatic stress disorder after stroke: A pilot study. J. Neurol. Sci. 2013, 327, 35–40. [Google Scholar] [CrossRef]
- Bruggimann, L.; Annoni, J.M.; Staub, F.; von Steinbüchel, N.; Van der Linden, M.; Bogousslavsky, J. Chronic posttraumatic stress symptoms after nonsevere stroke. Neurology 2006, 66, 513–516. [Google Scholar] [CrossRef]
- Rosman, L.; Sico, J.J.; Lampert, R.; Gaffey, A.E.; Ramsey, C.M.; Dziura, J.; Chui, P.W.; Cavanagh, C.E.; Brandt, C.; Haskell, S.; et al. Posttraumatic Stress Disorder and Risk for Stroke in Young and Middle-Aged Adults: A 13-Year Cohort Study. Stroke 2019, 50, 2996–3003. [Google Scholar] [CrossRef]
- Edmondson, D.; Richardson, S.; Fausett, J.K.; Falzon, L.; Howard, V.J.; Kronish, I.M. Prevalence of PTSD in Survivors of Stroke and Transient Ischemic Attack: A Meta-Analytic Review. PLoS ONE 2013, 8, e66435. [Google Scholar] [CrossRef]
- Garton, A.L.; Sisti, J.A.; Gupta, V.P.; Christophe, B.R.; Connolly, E.S., Jr. Poststroke Post-Traumatic Stress Disorder: A Review. Stroke 2017, 48, 507–512. [Google Scholar] [CrossRef]
- Perkins, J.D.; Wilkins, S.S.; Kamran, S.; Shuaib, A. Post-traumatic stress disorder and its association with stroke and stroke risk factors: A literature review. Neurobiol. Stress 2021, 14, 100332. [Google Scholar] [CrossRef]
- Rutovic, S.; Kadojic, D.; Dikanovic, M.; Solic, K.; Malojcic, B. Prevalence and correlates of post-traumatic stress disorder after ischaemic stroke. Acta Neurol. Belg. 2021, 121, 437–442. [Google Scholar] [CrossRef] [PubMed]
- Gick, M.L.; Sirois, F.M. Insecure attachment moderates women's adjustment to inflammatory bowel disease severity. Rehabil. Psychol. 2010, 55, 170–179. [Google Scholar] [CrossRef] [PubMed]
- Ercolani, M.; Farinelli, M.; Agostini, A.; Baldoni, F.; Baracchini, F.; Ravegnani, G.; Bortolotti, M. Gastroesophageal reflux disease (GERD) and inflammatory bowel disease (IBD): Attachment styles and parental bonding. Percept. Mot. Skills 2010, 111, 625–630. [Google Scholar] [CrossRef] [PubMed]
- Caplan, R.A.; Maunder, R.G.; Stempak, J.M.; Silverberg, M.S.; Hart, T.L. Attachment, childhood abuse, and IBD-related quality of life and disease activity outcomes. Inflamm. Bowel. Dis. 2014, 20, 909–915. [Google Scholar] [CrossRef] [PubMed]
- Farias, O.O.; Alexandre, H.O.; Lima, I.C.V.; Galvao, M.T.G.; Hanley-Dafoe, R.; Santos, V.D.F. Attachment styles of People Living with HIV/AIDS. Cien. Saude Colet. 2020, 25, 495–504. [Google Scholar] [CrossRef]
- Rajkumar, R.P. Attachment Theory and Psychological Responses to the COVID-19 Pandemic: A Narrative Review. Psychiatr. Danub. 2020, 32, 256–261. [Google Scholar] [CrossRef]
- Owen, C. Obscure Dichotomy of Early Childhood Trauma in PTSD Versus Attachment Disorders. Trauma Violence Abus. 2020, 21, 83–96. [Google Scholar] [CrossRef]
- Zerach, G.; Elklit, A. Attachment and social support mediate associations between Polyvictimization and psychological distress in early adolescence. Int. J. Psychol. 2020, 55, 380–391. [Google Scholar] [CrossRef]
- Barazzone, N.; Santos, I.; McGowan, J.; Donaghay-Spire, E. The links between adult attachment and post-traumatic stress: A systematic review. Psychol. Psychother. 2019, 92, 131–147. [Google Scholar] [CrossRef]
- Weiner, I.B. Psychotherapy relationships that work: Therapist contributions and responsiveness to patients. Psychother. Res. 2003, 13, 529–532. [Google Scholar] [CrossRef]
- Spinhoven, P.; Penninx, B.W.; Krempeniou, A.; van Hemert, A.M.; Elzinga, B. Trait rumination predicts onset of Post-Traumatic Stress Disorder through trauma-related cognitive appraisals: A 4-year longitudinal study. Behav. Res. Ther. 2015, 71, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Vanderveren, E.; Bijttebier, P.; Hermans, D. Autobiographical memory coherence in emotional disorders: The role of rumination, cognitive avoidance, executive functioning, and meaning making. PLoS ONE 2020, 15, e0231862. [Google Scholar] [CrossRef]
- Bishop, L.S.; Ameral, V.E.; Palm Reed, K.M. The Impact of Experiential Avoidance and Event Centrality in Trauma-Related Rumination and Posttraumatic Stress. Behav. Modif. 2018, 42, 815–837. [Google Scholar] [CrossRef]
- Nolen-Hoeksema, S.; Morrow, J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: The 1989 Loma Prieta Earthquake. J. Pers. Soc. Psychol. 1991, 61, 115–121. [Google Scholar] [CrossRef]
- Alamdar, S.; Lv, Y.; Guo, J.; Lu, J.; Zhang, Y. Attentional bias effect on post-traumatic outcomes in children after earthquake: Mediation role of rumination. PsyCh J. 2020, 9, 738–748. [Google Scholar] [CrossRef]
- Jasielska, A.; Ziarko, M. General and specific individual post-traumatic stress disorder-related mechanisms among paramedics. Med. Pr. 2019, 70, 53–66. [Google Scholar] [CrossRef]
- Garcia, F.E.; Vazquez, C.; Inostroza, C. Predictors of post-traumatic stress symptoms following occupational accidents: A longitudinal study. Anxiety Stress Coping 2019, 32, 168–178. [Google Scholar] [CrossRef]
- Lee, J.S. Perceived social support functions as a resilience in buffering the impact of trauma exposure on PTSD symptoms via intrusive rumination and entrapment in firefighters. PLoS ONE 2019, 14, e0220454. [Google Scholar] [CrossRef]
- Tomsis, Y.; Gelkopf, M.; Yerushalmi, H.; Zipori, Y. Different coping strategies influence the development of PTSD among first-time mothers. J. Matern. Fetal Neonatal Med. 2018, 31, 1304–1310. [Google Scholar] [CrossRef]
- Quickert, R.E.; MacDonald, T.K. Being in the Moment So You Can Keep Moving Forward: Mindfulness and Rumination Mediate the Relationship between Attachment Orientations and Negative Conflict Styles. Int. J. Environ. Res. Public Health 2020, 17, 6472. [Google Scholar] [CrossRef]
- Huh, H.J.; Kim, K.H.; Lee, H.K.; Chae, J.H. Attachment Style, Complicated Grief and Post-Traumatic Growth in Traumatic Loss: The Role of Intrusive and Deliberate Rumination. Psychiatry Investig. 2020, 17, 636–644. [Google Scholar] [CrossRef] [PubMed]
- Avila, M.; Brandao, T.; Teixeira, J.; Coimbra, J.L.; Matos, P.M. Attachment, emotion regulation, and adaptation to breast cancer: Assessment of a mediational hypothesis. Psychooncology 2015, 24, 1514–1520. [Google Scholar] [CrossRef] [PubMed]
- Van Durme, K.; Goossens, L.; Bosmans, G.; Braet, C. The Role of Attachment and Maladaptive Emotion Regulation Strategies in the Development of Bulimic Symptoms in Adolescents. J. Abnorm. Child Psychol. 2018, 46, 881–893. [Google Scholar] [CrossRef] [PubMed]
- Zortea, T.C.; Gray, C.M.; O'Connor, R.C. Adult attachment: Investigating the factor structure of the Relationship Scales Questionnaire. J. Clin. Psychol. 2019, 75, 2169–2187. [Google Scholar] [CrossRef]
- Nolen-Hoeksema, S.; Wisco, B.E.; Lyubomirsky, S. Rethinking Rumination. Perspect. Psychol. Sci. 2008, 3, 400–424. [Google Scholar] [CrossRef]
- Morisky, D.E.; Ang, A.; Krousel-Wood, M.; Ward, H.J. Predictive validity of a medication adherence measure in an outpatient setting. J. Clin. Hypertens. (Greenwich) 2008, 10, 348–354. [Google Scholar] [CrossRef]
- Reichenheim, M.E.; Oliveira, A.G.; Moraes, C.L.; Coutinho, E.S.; Figueira, I.; Lobato, G. Reappraising the dimensional structure of the PTSD Checklist: Lessons from the DSM-IV-based PCL-C. Braz. J. Psychiatry 2018, 40, 154–162. [Google Scholar] [CrossRef]
- Moon, S.J.; Lee, W.Y.; Hwang, J.S.; Hong, Y.P.; Morisky, D.E. Accuracy of a screening tool for medication adherence: A systematic review and meta-analysis of the Morisky Medication Adherence Scale-8. PLoS ONE 2017, 12, e0187139. [Google Scholar] [CrossRef]
- Baron, R.M.; Kenny, D.A. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986, 6, 117–1182. [Google Scholar] [CrossRef]
- Wen, Z.L.; Ye, B.J. Analyses of Mediating Effects: The Development of Methods and Models. Adv. Psychol. Sci. 2014, 22, 731–745. [Google Scholar] [CrossRef]
- Schmitt, A.P.; Hart, E.; Chow, C.M. Attachment, rumination, and disordered eating among adolescent girls: The moderating role of stress. Eat. Weight Disord. 2021, 26, 2271–2279. [Google Scholar] [CrossRef] [PubMed]
- Viana, A.G.; Paulus, D.J.; Garza, M.; Lemaire, C.; Bakhshaie, J.; Cardoso, J.B.; Ochoa-Perez, M.; Valdivieso, J.; Zvolensky, M.J. Rumination and PTSD symptoms among trauma-exposed Latinos in primary care: Is mindful attention helpful? Psychiatry Res. 2017, 258, 244–249. [Google Scholar] [CrossRef] [PubMed]
- Wielgosz, J.; Goldberg, S.B.; Kral, T.R.A.; Dunne, J.D.; Davidson, R.J. Mindfulness Meditation and Psychopathology. Annu. Rev. Clin. Psychol. 2019, 15, 285–316. [Google Scholar] [CrossRef] [PubMed]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).