A Computer-Assisted System for Early Mortality Risk Prediction in Patients with Traumatic Brain Injury Using Artificial Intelligence Algorithms in Emergency Room Triage
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics
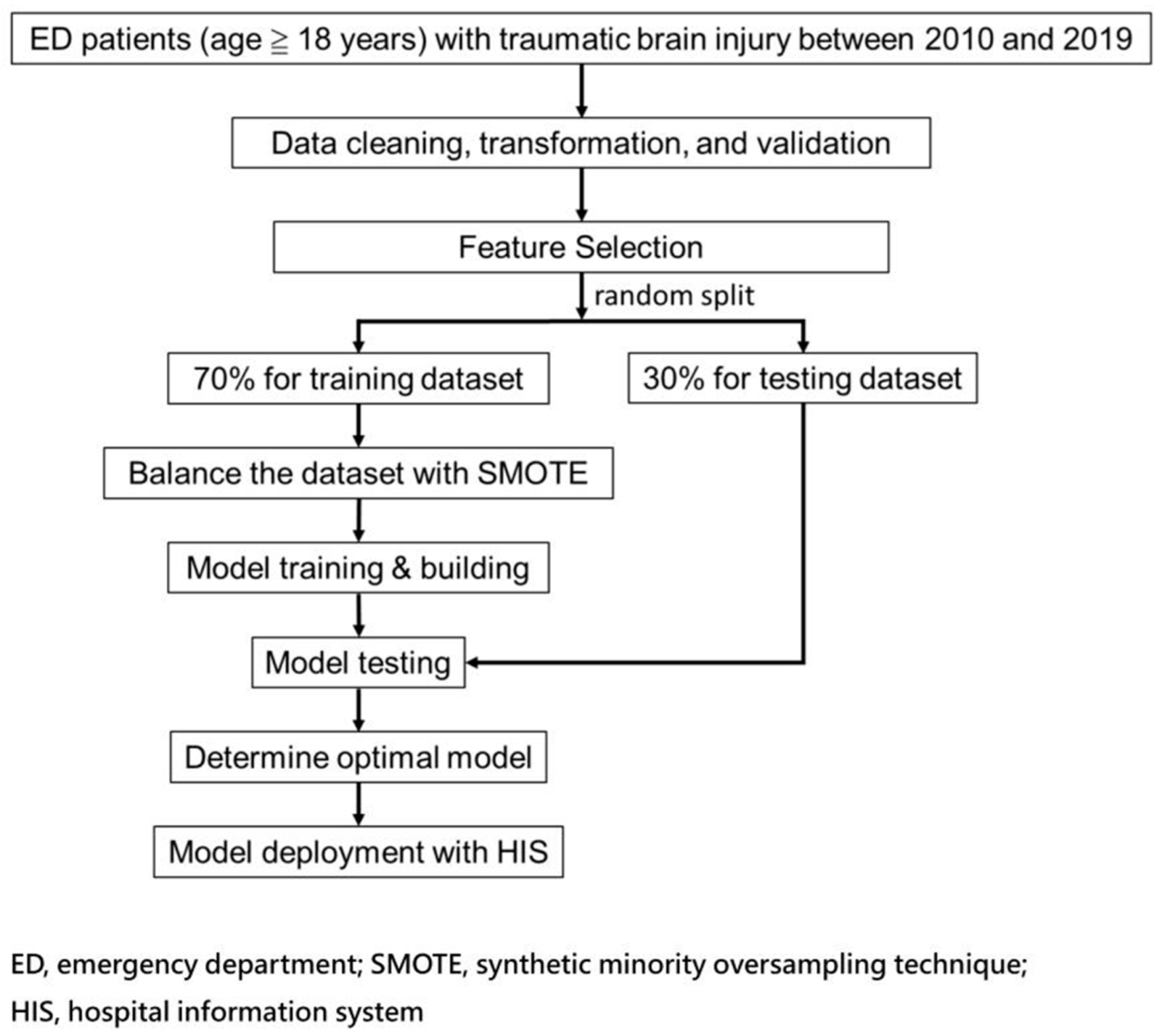
2.2. Flow Chart of Current Study
2.3. Patient Selection
2.4. Features Selection and Model Building
2.5. Model Performance Measurement and Calibration
3. Results
3.1. Demographics and Clinical Pictures in Patients with TBI
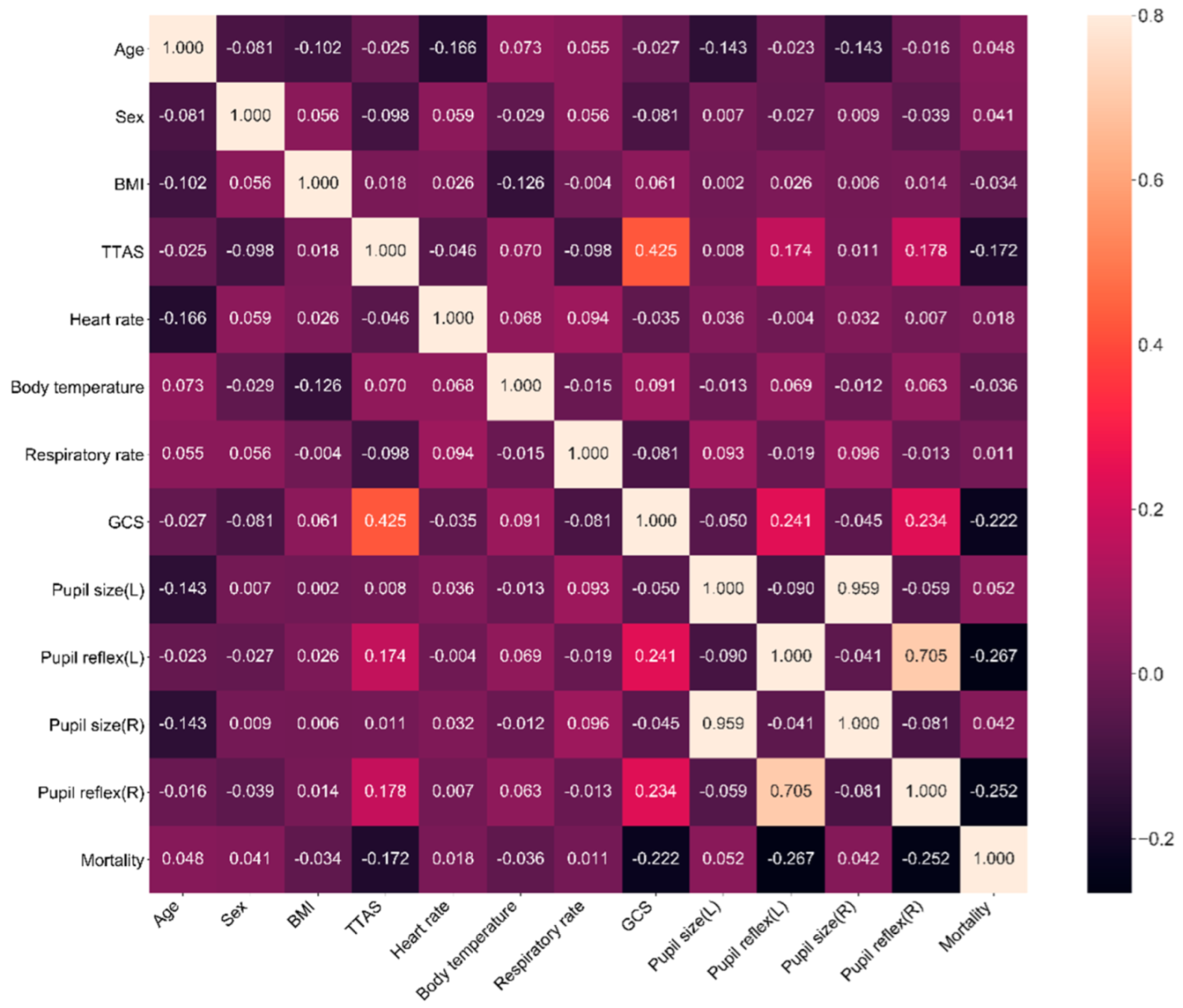
3.2. The Correlation between Feature Variables and Mortality
3.3. The Predictive Model Using the Twelve Feature Variables
3.4. The Predictive Models Using Fewer Feature Variables
3.5. Comparing Model Calibration for the Best Models
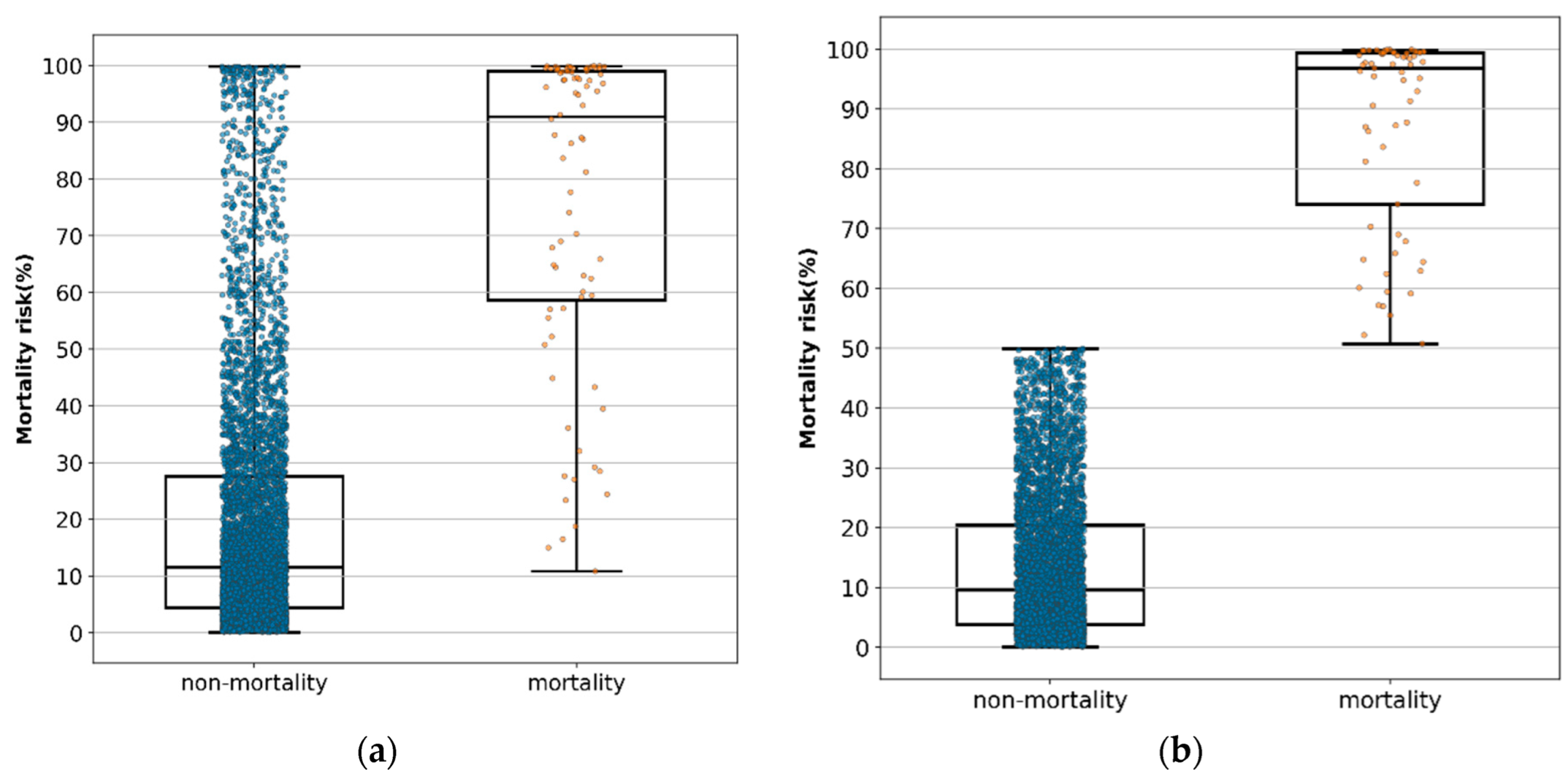
3.6. Distribution of the Predictive Value of Mortality in Each Patient
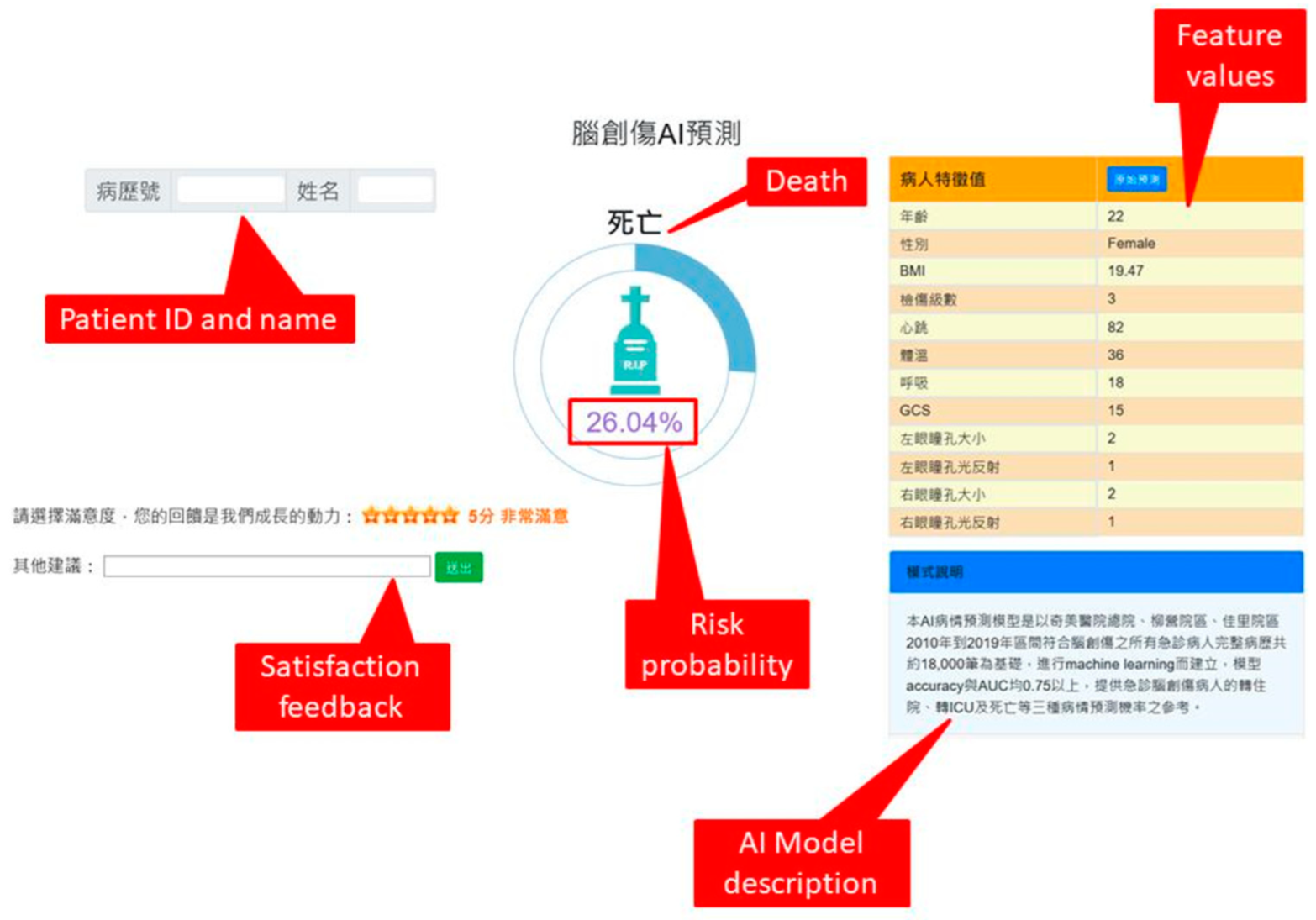
3.7. External Validation and Computer-Assisted System Development
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hsu, I.L.; Li, C.Y.; Chu, D.C.; Chien, L.C. An epidemiological analysis of head injuries in Taiwan. Int. J. Environ. Res. Public Health 2018, 15, 2457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Centers for Disease Control and Prevention. Traumatic Brain Injory & Concussion. Available online: www.cdc.gov/traumaticbraininjury/data/ (accessed on 1 October 2021).
- Kuo, J.R.; Lo, C.J.; Lu, C.L.; Chio, C.C.; Wang, C.C.; Lin, K.C. Prognostic predictors of outcome in an operative series in traumatic brain injury patients. J. Formos. Med. Assoc. 2011, 110, 258–264. [Google Scholar] [CrossRef]
- Farace, E.; Alves, W.M. Do women fare worse? A metaanalysis of gender differences in outcome after traumatic brain injury. Neurosurg. Focus. 2000, 8, e6. [Google Scholar] [CrossRef] [PubMed]
- Czorlich, P.; Dreimann, M.; Emami, P.; Westphal, M.; Lefering, R.; Hoffmann, M. Body Mass Index > 35 as independent predictor of mortality in severe traumatic brain injury. World Neurosurg. 2017, 107, 515–521. [Google Scholar] [CrossRef] [PubMed]
- Cone, J.T.; Benjamin, E.R.; Alfson, D.B.; Demetriades, D. Isolated severe blunt traumatic brain injury: Effect of obesity on outcomes. J. Neurosurg. 2020, 134, 1667–1674. [Google Scholar] [CrossRef]
- Ng, C.J.; Yen, Z.S.; Tsai, J.C.; Chen, L.C.; Lin, S.J.; Sang, Y.Y.; Chen, J.C. TTAS national working group. Validation of the Taiwan triage and acuity scale: A new computerised five-level triage system. Emerg. Med. J. 2011, 28, 1026–1231. [Google Scholar] [CrossRef]
- Nyam, T.E.; Ao, K.H.; Hung, S.Y.; Shen, M.L.; Yu, T.C.; Kuo, J.R. FOUR Score predicts early outcome in patients after traumatic brain injury. Neurocrit. Care 2017, 26, 225–231. [Google Scholar] [CrossRef]
- Brain Trauma Foundation, American Association of Neurological Surgery. Joint section in Neurotrauma and Critical care: Pupillary diameter and light reflex. J. Neurotrauma. 2000, 17, 583–590. [Google Scholar] [CrossRef]
- Eisenberg, H.M.; Gary, H.E.; Aldrich, E.; Saydjari, C.; Turner, B.; Foulkes, M.A.; Jane, J.A.; Marmarou, A.; Marshall, L.F.; Young, H.F. Initial CT findings in 753 patients with severe head injury. A report from the NIH Traumatic Coma Data Bank. J. Neurosurg. 1990, 73, 688–698. [Google Scholar] [CrossRef]
- Li, Z.; Wu, X.; Wu, X.; Yu, J.; Yuan, Q.; Du, Z. Admission circulating monocytes level is an independent predictor of outcome in traumatic brain injury. Brain Inj. 2018, 32, 515–522. [Google Scholar] [CrossRef]
- Kuo, J.; Chou, T.; Chio, C. Coagulopathy as a parameter to predict the outcome in head injury patients--analysis of 61 cases. J. Clin. Neurosci. 2004, 11, 710–714. [Google Scholar] [CrossRef] [PubMed]
- Liao, J.; Ho, C.; Liang, F.; Wang, J.; Lin, K.; Chio, C.; Kuo, J.R. One-year mortality associations in hemodialysis patients after traumatic brain injury—An eight-year population-based study. PLoS ONE 2014, 9, e93956. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.; Ho, C.; Wang, C.; Liang, F.; Wang, J.; Chio, C.; Chang, C.; Kuo, J.R. One-year mortality after traumatic brain injury in liver cirrhosis patients—A ten-year population-based study. Medicine 2015, 94, e1468. [Google Scholar] [CrossRef] [PubMed]
- Steyerberg, E.W.; Mushkudiani, N.; Perel, P.; Butcher, I.; Lu, J.; Mchugh, G.S.; Murray, G.D.; Marmarou, A.; Roberts, I.; Habbema, J.D.F.; et al. Predicting outcome after traumatic brain injury: Development and international validation of prognostic scores based on admission characteristics. PLoS Med. 2008, 5, e165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hosmer, D.W.; Lemeshow, S., Jr.; Sturdivant, R.X. Applied Logistic Regression; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2013. [Google Scholar]
- Breiman, L. Random forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef] [Green Version]
- Cortes, C.; Vapnik, V. Support-vector networks. Mach. Learn. 1995, 20, 273–297. [Google Scholar] [CrossRef]
- Ke, G.; Meng, Q.; Finley, T.; Wang, T.F.; Chen, W.; Ma, W.D.; Ye, Q.; Liu, T.Y. LightGBM: A highly efficient gradient boosting decision tree. In Proceedings of the 31st Conference on Neural Information Processing Systems, Long Beach, CA, USA, 4–9 December 2017. [Google Scholar]
- Chen, T.; Guestrin, C. XGBoost: A scalable tree boosting system. In Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–17 August 2016; pp. 785–794. [Google Scholar]
- Murtagh, F. Multilayer perceptrons for classification and regression. Neurocomputing 1991, 2, 183–197. [Google Scholar] [CrossRef]
- Azarkhish, I.; Raoufy, M.R.; Gharibzadeh, S. Artificial intelligence models for predicting iron deficiency anemia and iron serum level based on accessible laboratory data. J. Med. Syst. 2011, 36, 2057–2061. [Google Scholar] [CrossRef]
- Liu, N.; Koh, Z.X.; Goh, J.; Lin, Z.; Haaland, B.; Ting, B.P.; Ong, M.E. Prediction of adverse cardiac events in emergency department patients with chest pain using machine learning for variable selection. BMC Med. Inform. Decis. Mak. 2014, 14, 75. [Google Scholar] [CrossRef] [Green Version]
- Arvind, V.; Kim, J.S.; Oermann, E.K.; Kaji, D.; Cho, S.K. Predicting surgical complications in adult patients undergoing anterior cervical discectomy and fusion using machine learning. Neurospine 2018, 15, 329–337. [Google Scholar] [CrossRef]
- Du, X.; Min, J.; Shah, C.P.; Bishnoi, R.; Hogan, W.R.; Lemas, D.J. Predicting in-hospital mortality of patients with febrile neutropenia using machine learning models. Int. J. Med. Inform. 2020, 139, 104140. [Google Scholar] [CrossRef] [PubMed]
- Awad, A.; Bader-El-Den, M.B.; McNicholas, J.; Briggs, J.S. Early hospital mortality prediction of intensive care unit patients using an ensemble learning approach. Int. J. Med. Inform. 2017, 108, 185–195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, K.; Hu, Y.; Kong, G. Predicting in-hospital mortality of patients with acute kidney injury in the ICU using random forest model. Int. J. Med. Inf. 2019, 125, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Citi, L.; Barbieri, R. PhysioNet 2012 Challenge: Predicting mortality of ICU patients using a cascaded SVM-GLM paradigm. In Proceedings of the 2012 Computing in Cardiology, Krakow, Poland, 9–12 September 2012; pp. 257–260. [Google Scholar]
- Yera, A.; Muguerza, J.; Arbelaitz, O.; Perona, I.; Keers, R.N.; Ashcroft, D.M.; Williams, R.; Peek, N.; Jay, C.; Vigo, M. Modelling the interactive behaviour of users with a medication safety dashboard in a primary care setting. Int. J. Med. Inform. 2019, 129, 395–403. [Google Scholar] [CrossRef] [PubMed]
- Matsuo, K.; Aihara, H.; Nakai, T.; Morishita, A.; Tohma, Y.; Kohmura, E. Machine learning to predict in-hospital morbidity and mortality after traumatic brain injury. J. Neurotrauma 2019, 37, 202–210. [Google Scholar] [CrossRef]
- Amorim, R.L.; Oliveira, L.M.; Malbouisson, L.M.; Nagumo, M.M.; Simões, M.; Miranda, L.C.; Bor-Seng-Shu, E.; Beer-Furlan, A.; de Andrade, A.F.; Rubiano, A.M.; et al. Prediction of early TBI Mortality using a machine learning approach in a LMIC population. Front. Neurol. 2019, 10, 1366. [Google Scholar] [CrossRef] [Green Version]
- Shi, H.Y.; Hwang, S.L.; Lee, K.T.; Lin, C.L. In-hospital mortality after traumatic brain injury surgery: A nationwide population-based comparison of mortality predictors used in artificial neural network and logistic regression models. J. Neurosurg. 2013, 118, 746–752. [Google Scholar] [CrossRef] [Green Version]
- Serviá, L.; Montserrat, N.; Badia, M.; Llompart-Pou, J.A.; Barea-Mendoza, J.A.; Chico-Fernández, M.; Sánchez-Casado, M.; Jiménez, J.M.; Mayor, D.M.; Trujillano, J. Machine learning techniques for mortality prediction in critical traumatic patients: Anatomic and physiologic variables from the RETRAUCI study. BMC Med. Res. Methodol. 2020, 20, 262. [Google Scholar] [CrossRef]
- Warman, P.; Seas, A.; Satyadev, N.; Adil, S.M.; Kolls, B.J.; Haglund, M.M.; Dunn, T.W.; Fuller, A.T. Machine learning for predicting in-hospital mortality after traumatic brain injury in both high-income and low- and middle-income countries. Neurosurgery 2022, 90, 605–612. [Google Scholar] [CrossRef]
- Zhang, P.; Hsu, C.; Kao, Y.; Chen, C.; Kuo, Y.; Hsu, S.; Liu, T.; Lin, H.; Wang, J.; Liu, C.; et al. Real-time AI prediction for major adverse cardiac events in emergency department patients with chest pain. Scand. J. Trauma Resusc. Emerg. Med. 2020, 28, 93. [Google Scholar] [CrossRef]
- Liu, C.L.; Xu, Y.; Wu, H.; Chen, S.; Guo, J.J. Correlation and interaction visualization of altmetric indicators extracted from scholarly social network activities: Dimensions and structure. J. Med. Internet Res. 2013, 15, e259–e277. [Google Scholar] [CrossRef] [PubMed]
- Chawla, N.V.; Bowyer, K.W.; Hall, L.O.; Kegelmeyer, W.P. SMOTE: Synthetic minority over-sampling technique. J. Artif. Intell. Res. 2002, 16, 321–357. [Google Scholar] [CrossRef]
- Zweig, M.H.; Campbell, G. Receiver-operating characteristic (ROC) plots: A fundamental evaluation tool in clinical medicine. Clin. Chem. 1993, 39, 561–567. [Google Scholar] [CrossRef] [PubMed]
- Bradley, A.P. The use of the area under the ROC curve in the evaluation of machine learning algorithms. Pattern Recognit. 1997, 30, 1145–1159. [Google Scholar] [CrossRef] [Green Version]
- Amarasingham, R.; Patzer, R.E.; Huesch, M.D.; Nguyen, N.Q.; Xie, B. Implementing electronic health care predictive analytics: Considerations and challenges. Health Aff. 2014, 33, 1148–1154. [Google Scholar] [CrossRef]
- Nishida, C. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004, 363, 157–163. [Google Scholar]
- DeLong, E.; DeLong, D.; Clarke-Pearson, D. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics 1998, 44, 837–845. [Google Scholar] [CrossRef]
- Edward, N.; Nan, C.; Hecht, L.; Nelson, E.; Ross, J.; Fiddler, L. Correlation and regression. In SPSS for Windows Version 11.0: A Basic Tutorial; McGraw-Hill, Inc.: New York, NY, USA, 2000. [Google Scholar]
- Bullard, M.J.; Musgrave, E.; Warren, D.; Unger, B.; Skeldon, T.; Grierson, R.; van der Linde, E.; Swain, J. Revisions to the Canadian Emergency Department Triage and Acuity Scale (CTAS) Guidelines 2016. CJEM 2017, 19, S18–S27. [Google Scholar] [CrossRef] [Green Version]
- MRC CRASH Trial Collaborators; Perel, P.; Arango, M.; Clayton, T.; Edwards, P.; Komolafe, E.; Poccock, S.; Roberts, I.; Shakur, H.; Steyerberg, E.; et al. Predicting outcome after traumatic brain injury: Practical prognostic models based on large cohort of international patients. BMJ 2008, 336, 425–429. [Google Scholar] [CrossRef] [Green Version]

| Variable | Overall n = 18,249 | Mortality n = 266 | Non-Mortality n = 17,983 | p-Value |
|---|---|---|---|---|
| Age, mean (SD) | 57.85 (19.44) | 65.59 (17.74) | 57.73 (19.45) | <0.001 |
| Sex, n (%) | ||||
| Female | 8341 (45.71) | 77 (28.95) | 8264 (45.95) | <0.001 |
| Male | 9908 (54.29) | 189 (71.05) | 9719 (54.05) | |
| BMI, mean (SD) | 23.93 (4.45) | 22.68 (3.78) | 23.95 (4.46) | <0.001 |
| TTAS, n (%) | ||||
| Level I | 669 (3.67) | 147 (55.26) | 522 (2.90) | <0.001 |
| Level II | 5246 (28.75) | 85 (31.95) | 5161 (28.70) | |
| Level III-V | 12,334 (67.59) | 34 (12.78) | 12,300 (68.40) | |
| Heart rate, mean (SD) | 86.59 (18.74) | 89.75 (29.66) | 86.54 (18.53) | 0.080 |
| Body temperature, mean (SD) | 36.43 (0.50) | 36.30 (0.70) | 36.43 (0.49) | 0.002 |
| Respiratory rate, mean (SD) | 17.65 (2.51) | 17.44 (5.12) | 17.66 (2.45) | 0.502 |
| GCS, mean (SD) | 14.35 (1.94) | 8.58 (4.68) | 14.44 (1.73) | <0.001 |
| Pupil size(L), mean (SD) | 2.48 (0.57) | 3.05 (1.24) | 2.47 (0.55) | <0.001 |
| Pupil reflex (L), n (%) | ||||
| − | 450 (2.47) | 97 (36.47) | 353 (1.96) | <0.001 |
| + | 17,799 (97.53) | 169 (63.53) | 17,630 (98.04) | |
| Pupil size(R), mean (SD) | 2.47 (0.57) | 2.97 (1.23) | 2.47 (0.55) | <0.001 |
| Pupil reflex(R), n (%) | ||||
| − | 460 (2.52) | 93 (34.96) | 367 (2.04) | <0.001 |
| + | 17,789 (97.48) | 173 (65.04) | 17,616 (97.96) |
| Algorithm | Accuracy | Sensitivity | Specificity | PPV | NPV | AUC (95% CI) |
|---|---|---|---|---|---|---|
| Logistic regression | 0.893 | 0.812 | 0.894 | 0.102 | 0.997 | 0.925 (0.901–0.950) |
| Random forest | 0.800 | 0.800 | 0.800 | 0.056 | 0.996 | 0.870 (0.824–0.916) |
| SVM | 0.865 | 0.862 | 0.865 | 0.087 | 0.998 | 0.920 (0.891–0.948) |
| LightGBM | 0.708 | 0.825 | 0.706 | 0.040 | 0.996 | 0.851 (0.807–0.895) |
| MLP | 0.825 | 0.825 | 0.825 | 0.065 | 0.997 | 0.893 (0.854–0.933) |
| XGBoost | 0.717 | 0.838 | 0.715 | 0.042 | 0.997 | 0.871 (0.829–0.914) |
| Algorithm | Accuracy | Sensitivity | Specificity | PPV | NPV | AUC (95% CI) |
|---|---|---|---|---|---|---|
| (TTAS + 6 feature variables) | ||||||
| Logistic regression | 0.84 | 0.875 | 0.839 | 0.075 | 0.998 | 0.909 (0.876–0.943) |
| Random forest | 0.812 | 0.812 | 0.812 | 0.06 | 0.997 | 0.885 (0.844–0.925) |
| SVM | 0.806 | 0.812 | 0.806 | 0.059 | 0.997 | 0.889 (0.848–0.931) |
| LightGBM | 0.724 | 0.825 | 0.722 | 0.042 | 0.996 | 0.884 (0.848–0.920) |
| MLP | 0.808 | 0.875 | 0.807 | 0.063 | 0.998 | 0.905 (0.869–0.941) |
| XGBoost | 0.812 | 0.838 | 0.812 | 0.062 | 0.997 | 0.897 (0.863–0.931) |
| (TTAS + 5 feature variables) | ||||||
| Logistic regression | 0.823 | 0.825 | 0.823 | 0.065 | 0.997 | 0.907 (0.875–0.939) |
| Random forest | 0.812 | 0.812 | 0.812 | 0.06 | 0.997 | 0.876 (0.840–0.913) |
| SVM | 0.824 | 0.825 | 0.824 | 0.063 | 0.997 | 0.904 (0.872–0.937) |
| LightGBM | 0.826 | 0.825 | 0.826 | 0.073 | 0.997 | 0.883 (0.845–0.921) |
| MLP | 0.814 | 0.838 | 0.814 | 0.062 | 0.997 | 0.902 (0.871–0.937) |
| XGBoost | 0.806 | 0.85 | 0.806 | 0.061 | 0.997 | 0.887 (0.851–0.923) |
| (TTAS + 4 feature variables) | ||||||
| Logistic regression | 0.925 | 0.688 | 0.928 | 0.125 | 0.995 | 0.891 (0.850–0.931) |
| Random forest | 0.876 | 0.75 | 0.878 | 0.084 | 0.996 | 0.855 (0.800–0.911) |
| SVM | 0.81 | 0.788 | 0.811 | 0.058 | 0.996 | 0.869 (0.824–0.915) |
| LightGBM | 0.871 | 0.762 | 0.873 | 0.082 | 0.996 | 0.866 (0.814–0.917) |
| MLP | 0.868 | 0.788 | 0.869 | 0.082 | 0.996 | 0.893 (0.855–0.931) |
| XGBoost | 0.876 | 0.762 | 0.877 | 0.084 | 0.996 | 0.866 (0.815–0.918) |
| (TTAS) | ||||||
| Logistic regression | 0.696 | 0.9 | 0.693 | 0.042 | 0.998 | 0.872 (0.832–0.912) |
| Random forest | 0.696 | 0.9 | 0.693 | 0.042 | 0.998 | 0.872 (0.832–0.912) |
| SVM | 0.696 | 0.9 | 0.693 | 0.042 | 0.998 | 0.872 (0.832–0.912) |
| LightGBM | 0.696 | 0.9 | 0.693 | 0.042 | 0.998 | 0.872 (0.832–0.912) |
| MLP | 0.696 | 0.9 | 0.693 | 0.042 | 0.998 | 0.869 (0.828–0.911) |
| XGBoost | 0.696 | 0.9 | 0.693 | 0.042 | 0.998 | 0.872 (0.832–0.912) |
| TTAS + 11 Features | TTAS + 6 Features | TTAS + 5 Features | TTAS + 4 Features | TTAS | |
|---|---|---|---|---|---|
| TTAS + 11 features | 1 | 0.103 | 0.127 | 0.043 | 0.003 |
| TTAS + 6 features | 0.103 | 1 | 0.777 | 0.174 | 0.013 |
| TTAS + 5 features | 0.127 | 0.777 | 1 | 0.146 | 0.001 |
| TTAS + 4 features | 0.043 | 0.174 | 0.146 | 1 | 0.007 |
| TTAS | 0.003 | 0.013 | 0.001 | 0.007 | 1 |
| Model | Accuracy | Sensitivity | Specificity | PPV | NPV | AUC (95% CI) |
|---|---|---|---|---|---|---|
| TTAS + 11 feature variables | 0.891 | 0.812 | 0.892 | 0.101 | 0.997 | 0.926 (0.901–0.950) |
| TTAS + 6 feature variables | 0.843 | 0.838 | 0.843 | 0.073 | 0.997 | 0.910 (0.876–0.943) |
| TTAS + 5 feature variables | 0.822 | 0.825 | 0.822 | 0.064 | 0.997 | 0.907 (0.875–0.939) |
| TTAS + 4 feature variables | 0.908 | 0.713 | 0.911 | 0.106 | 0.995 | 0.891 (0.851–0.932) |
| TTAS | 0.696 | 0.900 | 0.693 | 0.042 | 0.998 | 0.872 (0.832–0.912) |
| All Cases without Exclusion | Excluding False-Positive and False-Negative Cases | ||||
|---|---|---|---|---|---|
| Non-Mortality | Mortality | Non-Mortality | Mortality | ||
| count | 5395 | 80 | count | 4822 | 65 |
| mean | 20.27 | 76.02 | Mean | 13.73 | 87.15 |
| SD | 22.81 | 27.80 | SD | 12.40 | 16.15 |
| min | 0.09 | 10.84 | min | 0.09 | 50.77 |
| 25% | 4.38 | 58.67 | 25% | 3.79 | 74.10 |
| 50% | 11.57 | 90.96 | 50% | 9.60 | 96.85 |
| 75% | 27.61 | 99.07 | 75% | 20.46 | 99.41 |
| max | 99.86 | 99.94 | max | 49.96 | 99.94 |
| Variable | Survivaln = 197 | Mortalityn = 3 | p-Value |
|---|---|---|---|
| Gender, n (%) | 0.247 | ||
| male | 97 (49.2) | 0 (0) | |
| female | 100 (50.8) | 3 (100) | |
| Age, median (IQR) | 51 (32–67) | 72 (29–95) | 0.280 |
| GCS, median (IQR) | 15 (15–15) | 3 (3–6) | <0.001 |
| Pupil size (L), median (IQR) | 2.5 (2.0–2.5) | 4.0 (2.0–5.0) | 0.137 |
| Pupil size (R), median (IQR) | 2.5 (2.0–2.5) | 2.5 (2.0–4.0) | 0.510 |
| light reflex (L), n (%) | <0.001 | ||
| − | 1 (0.5) | 2 (66.7) | |
| + | 196 (99.5) | 1 (33.3) | |
| light reflex (R), n (%) | <0.001 | ||
| − | 1 (0.5) | 2 (66.7) | |
| + | 196 (99.5) | 1 (33.3) | |
| TTAS, n (%) | <0.001 | ||
| Level I | 4 (2.0) | 3 (100) | |
| Level II | 39 (19.8) | 0 (0) | |
| Levels III–V | 154(78.2) | 0 (0) | |
| BMI, median (IQR) | 24.6 (22.8–24.6) | 19.5 (17.3–19.5) | 0.008 |
| BT, median (IQR) | 36.4 (36.2–36.7) | 36.6 (35.0–37.2) | 0.778 |
| HR, median (IQR) | 86 (75–97) | 98 (86–105) | 0.183 |
| RR, median (IQR) | 16 (16–18) | 18 (10–24) | 0.632 |
| predictive value, median (IQR) | 28.3 (26.0–35.9) | 85.8 (85.7–85.8) | 0.003 |
| Study | This Study | Shi et al., 2013 [32] | Matssuo et al., 2019 [30] | Serviá et al., 2020 [33] |
|---|---|---|---|---|
| Setting | In the emergency room triage | In-hospital | In-hospital | Intensive care unit |
| Patient number | 18,249 | 3206 | 232 | 9625 |
| Study method | Six ML methods | Two ML methods | Nine ML methods | Nine ML methods |
| Feature variables | 12 feature variables | 7 feature variables | 11 feature variables | 11 variables |
| Outcome | Mortality | Mortality | Mortality | Mortality |
| Testing results | 0.925 | 0.896 | 0.875 | 0.915 |
| (AUC 95% CI) | (0.901–0.950) | (0.871–0.921) | (0.869–0.882) | (N/A) |
| Best predicting model | Logistic regression | Artificial neural network | Ridge regression | Bayesian network |
| Real world implementation | Yes | N/A | N/A | N/A. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tu, K.-C.; Eric Nyam, T.-T.; Wang, C.-C.; Chen, N.-C.; Chen, K.-T.; Chen, C.-J.; Liu, C.-F.; Kuo, J.-R. A Computer-Assisted System for Early Mortality Risk Prediction in Patients with Traumatic Brain Injury Using Artificial Intelligence Algorithms in Emergency Room Triage. Brain Sci. 2022, 12, 612. https://doi.org/10.3390/brainsci12050612
Tu K-C, Eric Nyam T-T, Wang C-C, Chen N-C, Chen K-T, Chen C-J, Liu C-F, Kuo J-R. A Computer-Assisted System for Early Mortality Risk Prediction in Patients with Traumatic Brain Injury Using Artificial Intelligence Algorithms in Emergency Room Triage. Brain Sciences. 2022; 12(5):612. https://doi.org/10.3390/brainsci12050612
Chicago/Turabian StyleTu, Kuan-Chi, Tee-Tau Eric Nyam, Che-Chuan Wang, Nai-Ching Chen, Kuo-Tai Chen, Chia-Jung Chen, Chung-Feng Liu, and Jinn-Rung Kuo. 2022. "A Computer-Assisted System for Early Mortality Risk Prediction in Patients with Traumatic Brain Injury Using Artificial Intelligence Algorithms in Emergency Room Triage" Brain Sciences 12, no. 5: 612. https://doi.org/10.3390/brainsci12050612
APA StyleTu, K.-C., Eric Nyam, T.-T., Wang, C.-C., Chen, N.-C., Chen, K.-T., Chen, C.-J., Liu, C.-F., & Kuo, J.-R. (2022). A Computer-Assisted System for Early Mortality Risk Prediction in Patients with Traumatic Brain Injury Using Artificial Intelligence Algorithms in Emergency Room Triage. Brain Sciences, 12(5), 612. https://doi.org/10.3390/brainsci12050612






