1. Introduction
The value and potential for music interventions, including neurologic music therapy (NMT), within multidisciplinary neurorehabilitation have been recognised and discussed [
1,
2,
3,
4,
5,
6,
7]. However, few music therapists are currently working in neurorehabilitation internationally [
8,
9]. There is a lack of implementation research looking at the feasibility and acceptability of music interventions within existing multidisciplinary services, which traditionally include physiotherapists, occupational therapists, and speech and language therapists. One study on an acute stroke ward found a two-day-per-week NMT service to be feasible and helpful for mood and motivation while simultaneously supporting functional recovery [
10].
Music interventions with brain-injured populations may help to improve gait parameters, timing of arm movements, aphasia, and quality of life [
11]. Studies have shown music interventions in subacute neurorehabilitation to support gait training [
12,
13], upper extremity [
14,
15,
16], speech [
17], and cognitive recovery [
18].
Previous research on NMT indicates a positive effect on mood, quality of life, and well-being, and a reduction in symptoms of depression and anxiety, while addressing functional goals [
19,
20,
21,
22]. Music interventions may be less fatiguing than traditional therapies [
16,
23,
24], possibly due to neurochemical changes induced by music [
25], enhanced levels of neuroplasticity [
15,
26], and the activation of neural mechanisms involved in emotion regulation, motivation, reward, and arousal [
6]. This could support adherence to rehabilitation programmes and so help patients meet dosage requirements, which is crucial for effective recovery [
27,
28,
29].
This study looked at the feasibility and acceptability of a one-day-per-week NMT post in a subacute neurorehabilitation centre over a 15-month period.
2. Materials and Methods
2.1. Setting
The NMT worked within the multidisciplinary team (MDT) for 7.5 h per week. The centre also hosted a music therapy master of arts (MA) student on placement for 10 h per week across eight months of the service evaluation. Two MA students were hosted at the centre, one of whom had completed NMT training. Both were supported to use NMT techniques through weekly supervision with NMT trained music therapists.
During the setup of the post, a presentation outlining the mechanisms of NMT, including video demonstrations and clarifying referral criteria, was delivered to the MDT. A therapy assistant working at the centre was assigned to liaise between the MDT and the music therapist. Members of the MDT regularly attended a sensorimotor group run by the music therapist as well as conjoint working in individual sessions.
2.2. Data Collection
Data were collected as part of usual care, including: age, sex, reason for referral to NMT, number of sessions offered and attended, reasons for non-attendance, type of session, interventions used, and who the referral was from. Patients were referred verbally or by e-mail for NMT by members of the MDT. Data on attendance, alongside feedback from the questionnaires, were used to evaluate the feasibility of delivering NMT in a one-day-per-week post. There was no control group as the study aimed to evaluate the feasibility of NMT as part of MDT subacute neurorehabilitation.
All data collection tools were approved by the centre manager and clinical lead, and permission to collect data as part of standard care and for publishing was granted by the rehabilitation centre. The music therapist and MA student explained the reason and purpose of data collection to each patient, including that data would be anonymised, used for a service evaluation, and possibly published. Each patient then provided verbal consent.
The data collection tools comprised three questionnaires (staff, patients, patients’ relatives) and the Visual Analog Mood Scales (VAMS) [
30]. These were chosen to align with tools used in a recent study evaluating the feasibility of NMT in an acute stroke ward [
10]. A version of the patient questionnaire for those with aphasia was co-designed with the speech and language therapist. The questionnaire was administered to patients after they had attended one or more sessions by other members of staff, not the music therapist, to reduce bias. Members of the MDT and relatives were asked to complete a questionnaire after they had attended a session. The questionnaires asked respondents to rate whether they thought NMT was 1. Not Helpful, 2. Quite Helpful, 3. Helpful, 4. Very Helpful, or 5. Not Applicable towards five therapeutic aims: ‘speech and communication’, ‘walking and mobility’, ‘concentration’, ‘arm and hand movement’, and ‘motivation and mood’. There was space for additional comments with prompting questions.
VAMS [
31] data were collected by the music therapist and other staff pre and post a single NMT session. The lead music therapist was qualified to deliver VAMS per the required standard and supervised students and other staff in its use. Eight mood states are included in the VAMS: six negative (afraid, confused, sad, angry, tired, tense) and two positive (energetic, happy). Data were not collected in the first session to allow the patient to adjust to the new therapy input.
2.3. Statistical Analysis
T scores were generated from the VAMS raw scores and used for statistical analysis. For identifying mood disorders, a
T-score of <60 for negative emotions or >40 for positive emotions is considered significant [
31]. When tracking changes in mood, differences between the pre- and post-
T scores above 20
T are considered reliable, and differences over 30
T are considered clinically significant. SPSS 26 was used to generate means for pre- and post-session
T scores along with standard deviation and confidence intervals. As the data were not normally distributed, a Wilcoxon signed ranks test was conducted, as well as an effect size calculation (Cohen’s d). A significance level of 0.05 was used with 95% confidence intervals.
The questionnaire generated both quantitative and qualitative data. A thematic analysis was conducted on additional comments with written responses coded using inductive coding and grouped into themes.
2.4. Intervention
Many of the interventions used were standardised NMT exercises to achieve motor, cognitive, and speech and communication goals in line with those set by the MDT [
32]. These included a weekly sensorimotor group using therapeutical instrumental music performance (TIMP), where patients played instruments in time with music provided by the music therapist to target specific movements. This took place in a private lounge at the centre. Individual sessions also used TIMP, as well as other NMT techniques such as patterned sensory enhancement (PSE), melodic intonation therapy (MIT), rhythmic speech cueing (RSC), vocal intonation therapy (VIT), musical neglect training (MNT), and musical attentional control training (MACT). Additionally, the music therapist and MA student supported the psychological and emotional well-being of patients through techniques such as improvising music, singing meaningful familiar songs, and songwriting. Individual sessions took place in a private lounge or in patient rooms.
4. Discussion
Over the period reported, based on the number of referrals, sessions offered and completed, and questionnaire data, the service was feasible with the additional input from the MA student and the liaison person. The exercises were acceptable and considered helpful within neurorehabilitation, in particular, toward goals relating to concentration, arm and hand movement, motivation, and mood. VAMS scores showed positive changes in seven of eight mood variables after a single session, with a statistically significant increase in ‘happiness’ and a decrease in ‘confusion’.
This study looked at the feasibility and acceptability of delivering NMT one-day-per-week in one neurorehabilitation centre. Results cannot be generalised to other services; however, there are similarities with previous research in acute stroke rehabilitation in regard to patient engagement and perceived benefit of the interventions [
10].
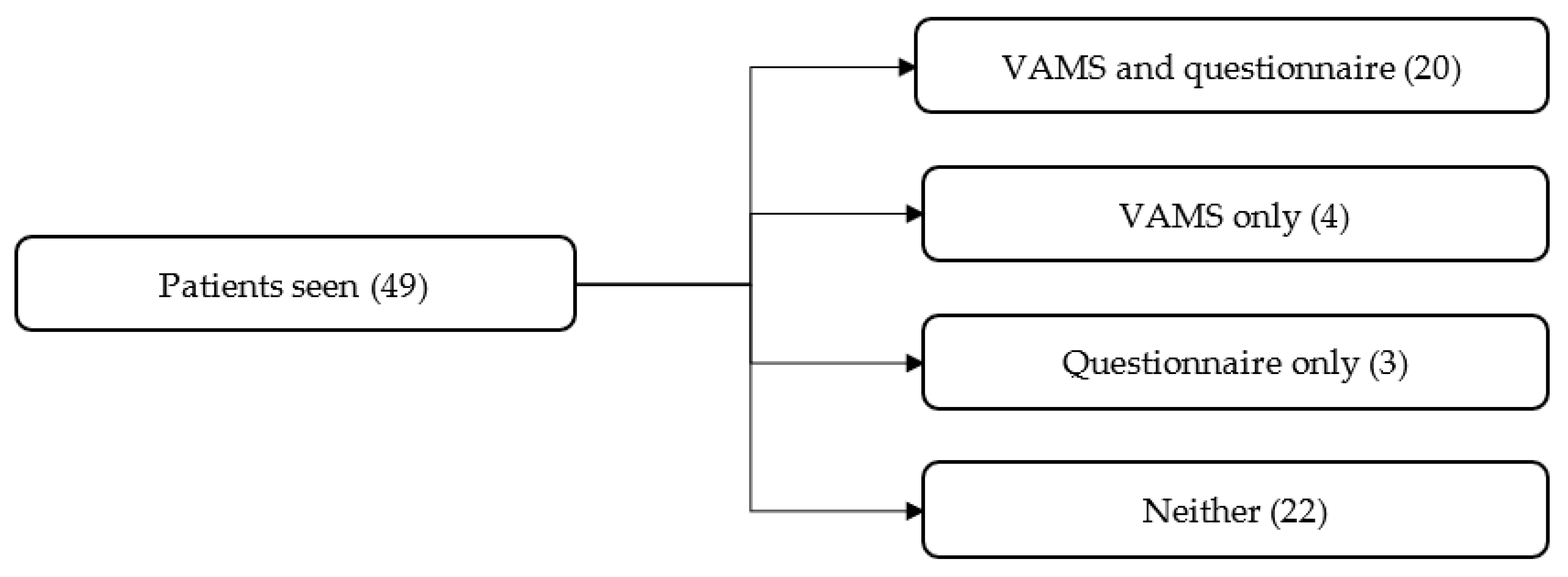
As data were collected as a service evaluation, there are several limitations. No comparison data were collected, so it is not possible to say whether a similar questionnaire and VAMS data would have resulted from other MDT sessions. Of a total of 49 patients who received NMT, 24 completed the mood scale, and 22 completed the questionnaire. All members of the MDT who jointly ran NMT sessions completed the staff questionnaires, totalling 9 of 10 members of staff. One member of the MDT, a psychologist, worked on a different day to the NMT, so it was not possible to do conjoint work. There may have been some bias in the data collection, as data were collected by clinicians working at the centre. However, in an attempt to mitigate this, staff other than the NMT collected all patient questionnaire data and some VAMS data. The questionnaire data show participants’ perception of the benefits of functional goals, but no data were collected on functional outcomes using validated measures.
The questionnaire data suggest that NMT was considered most helpful for ‘concentration’, ‘arm and hand rehabilitation’, and ‘motivation and mood’. Although ‘speech and communication’ or ‘walking and mobility’ were reported as not applicable for 15 (34%) patients, NMT was still reported as helpful or very helpful for addressing these goals for 24 (55%) patients. This pattern was seen in a previous study [
10], which used the same feedback forms in an acute stroke setting. Although exercises for lower limb and walking phases were included in the sensorimotor group, patients may not have comprehended that these were linked to gait. Thematic analysis of the additional questionnaire comments showed that NMT raised patient mood and provided an opportunity for social interaction as well as supporting sensorimotor rehabilitation, which is supported by previous study findings [
16,
22].
There was more variety in questionnaire ratings from patients than from their relatives and staff. This could be due to patients being more focused on the applicability to their own goals, while their relatives and clinicians might consider the potential effectiveness across more domains and recognise the importance of motivation for patients to engage sufficiently in rehabilitation. Additionally, clinicians would have a greater understanding of the mechanisms underlying the interventions through their own clinical knowledge, the initial presentation given to the MDT prior to the NMT commencing, and additional informal communications with the music therapist. However, patients may have an initial preconception of music as a recreational activity. Future research could explore the role awareness of the mechanisms underlying NMT has in clinician and patient perceptions of the helpfulness of the interventions.
The VAMS scores support the subjective questionnaire results showing positive changes in mood states pre and post a single session. The significant reduction in levels of confusion could suggest that engaging in music interventions improves cognitive functioning and orientation, as suggested in the literature [
16,
18,
19]. The increase in ‘energetic’, despite the nature of the exercises, supports the suggestion that engaging in music-based exercises is less fatiguing [
16,
23,
24].
5. Conclusions
Data suggest that NMT was feasible within the subacute setting at one-day-per-week. It was considered helpful, especially for movement, concentration and motivation, and mood, with the latter supported by changes in mood scores (VAMS). Integrating the music therapist into the MDT through conjoint working and having a named, full-time member of staff to facilitate the service was invaluable to the referral system setup for a one day post. This also helped staff to quickly understand the mechanisms of the interventions. Future research should be conducted to determine whether music-based interventions increase patient engagement in other MDT interventions due to the social and mood benefits and whether this improves clinical outcomes, reduces inpatient length of stay, and increases patient flow.