COVID-19 Still Surprising Us—A Rare Movement Disorder Induced by Infection
Abstract
1. Background
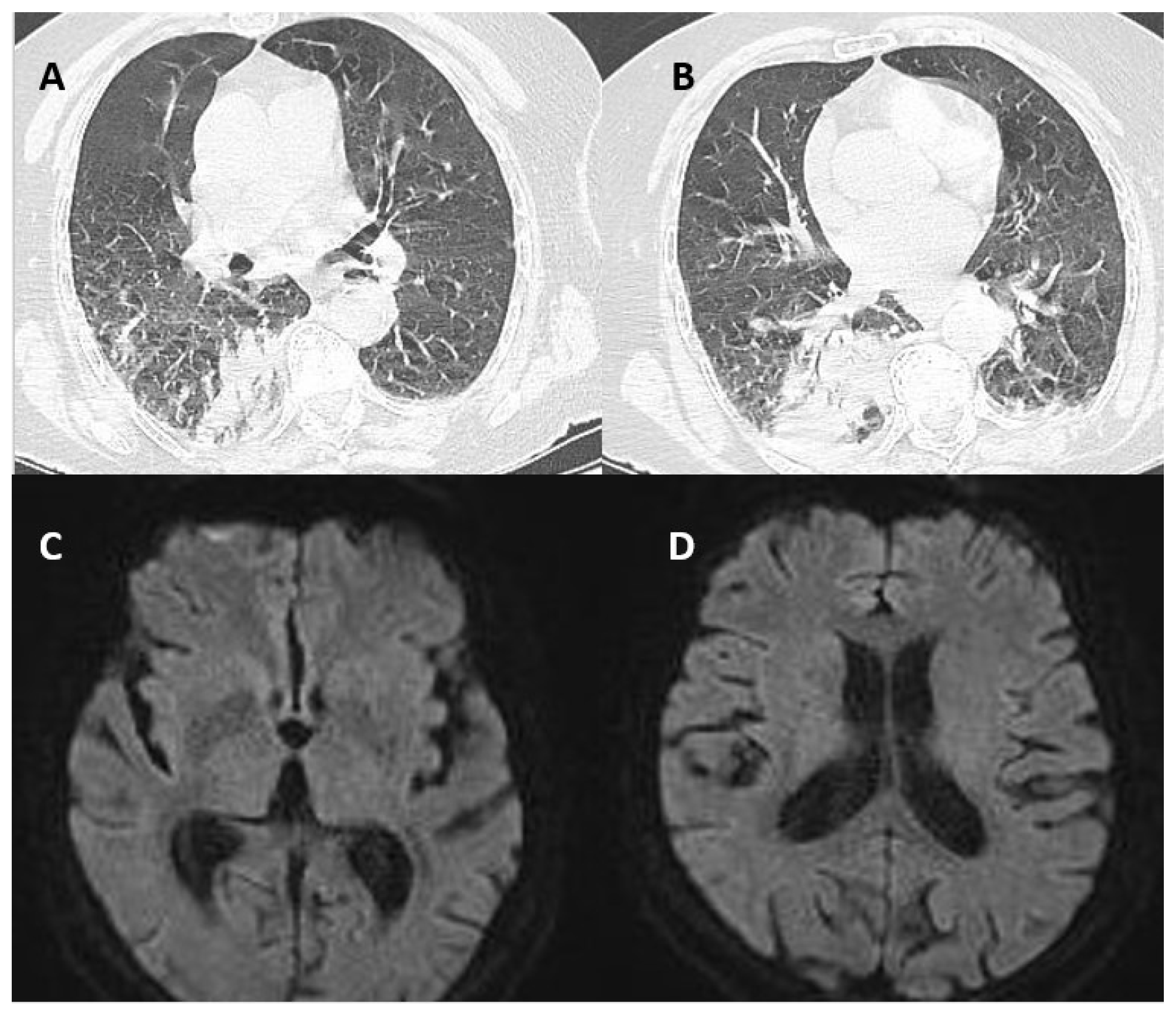
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Paterson, R.W.; Brown, R.L.; Benjamin, L.; Nortley, R.; Wiethoff, S.; Bharucha, T.; Jayaseelan, D.L.; Kumar, G.; Raftopoulos, R.E.; Zambreanu, L.; et al. The emerging spectrum of COVID-19 neurology: Clinical, radiological and laboratory findings. Brain 2020, 143, 3104–3120. [Google Scholar] [CrossRef] [PubMed]
- Florea, A.A.; Sirbu, C.A.; Ghinescu, M.C.; Plesa, C.F.; Sirbu, A.M.; Mitrica, M.; Ionita-Radu, F. SARS-CoV-2, multiple sclerosis, and focal deficit in a postpartum woman: A case report. Exp. Ther. Med. 2021, 21, 92. [Google Scholar] [CrossRef] [PubMed]
- Acar, T.; Demirel, E.A.; Afsar, N.; Akcali, A.; Demir, G.A.; Alagoz, A.N.; Mengi, T.A.; Arsava, E.M.; Ayta, S.; Bebek, N.; et al. The COVID-19 from Neurological Overview. TJN 2020, 26, 58–108. [Google Scholar] [CrossRef]
- Al-Ramadan, A.; Rabab’h, O.; Shah, J.; Gharaibeh, A. Acute and Post-Acute Neurological Complications of COVID-19. Neurol. Int. 2021, 13, 102–119. [Google Scholar] [CrossRef] [PubMed]
- Heidarpour, M.; Vakhshoori, M.; Haghighatpanah, M.A.; Ashrafi, L.; Khorvash, F.; Iraj, B. Rhabdomyolysis plus Hypocalcemia and Diabetic Ketoacidosis as Concurrent Rare COVID-19 Manifestations. J. Med. Case Rep. 2021, 2021, 1–6. [Google Scholar] [CrossRef]
- Tawakul, A.A.; Al-Doboke, A.W.; Altayyar, S.A.; Alsulami, S.A.; Alfahmi, A.M.; Nooh, R.T. Guillain-Barré Syndrome in the COVID-19 Pandemic. Neurol. Int. 2021, 14, 34–48. [Google Scholar] [CrossRef]
- Martinez-Hernandez, E.; Ariño, H.; McKeon, A.; Iizuka, T.; Titulaer, M.J.; Simabukuro, M.M.; Lancaster, E.; Petit-Pedrol, M.; Planagumà, J.; Blanco, Y.; et al. Clinical and Immunologic Investigations in Patients With Stiff-Person Spectrum Disorder. JAMA Neurol. 2016, 73, 714–720. [Google Scholar] [CrossRef]
- Manes, P.K.; Mohammad Aslam, S.; Varghese, M.; Elipulikattu, L. Stiff-Person Syndrome: A Case Report. J. Med. Case Rep. 2016, 7, 426–428. [Google Scholar] [CrossRef]
- Alexopoulos, H.; Dalakas, M.C. A critical update on the immunopathogenesis of Stiff Person Syndrome. Eur. J. Clin. Invest. 2010, 40, 1018–1025. [Google Scholar] [CrossRef] [PubMed]
- Raju, R.; Rakocevic, G.; Chen, Z.; Hoehn, G.; Semino-Mora, C.; Shi, W.; Olsen, R.; Dalakas, M.C. Autoimmunity to GABAA-receptor-associated protein in stiff-person syndrome. Brain 2006, 129 Pt 12, 3270–3276. [Google Scholar] [CrossRef]
- Balint, B.; Meinck, H.M. Pragmatic Treatment of Stiff Person Spectrum Disorders. Mov. Disord. Clin. 2018, 5, 394–401. [Google Scholar] [CrossRef] [PubMed]
- Kasperek, S.; Zebrowski, S. Stiff-Man Syndrome and Encephalomyelitis: Report of a Case. Arch. Neurol. 1971, 24, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Ortiz, J.F.; Ghani, M.R.; Cox, Á.M.; Tambo, W.; Bashir, F.; Wirth, M.; Moya, G. Stiff-Person Syndrome: A Treatment Update and New Directions. Cureus 2020, 12, e11995. [Google Scholar] [CrossRef]
- Levy, L.M.; Levy-Reis, I.; Fujii, M.; Dalakas, M.C. Brain γ-Aminobutyric Acid Changes in Stiff-Person Syndrome. Arch. Neurol. 2005, 62, 970–974. [Google Scholar] [CrossRef]
- Hassin-Baer, S.; Kirson, E.D.; Shulman, L.; Buchman, A.S.; Bin, H.; Hindiyeh, M.; Markevich, L.; Mendelson, E. Stiff-Person Syndrome Following West Nile Fever. Arch. Neurol. 2004, 61, 938. [Google Scholar] [CrossRef]
- Martin, R.; Meinck, H.M.; Schulte-Mattler, W.; Ricker, K.; Mertens, H.G. Borrelia burgdorferi myelitis presenting as a partial stiff man syndrome. J. Neurol. 1990, 237, 51–54. [Google Scholar] [CrossRef]
- Requena, I.; Arias, M.; Pardo, J.; Portela, M.; Alvarez, J.A. Syndromes of continuous muscular activity: Report of a central case (stiff-man) and a peripheral case (neuromyotonia) associated with neuroborreliosis. Rev. Neurol. 1995, 23, 129–133. [Google Scholar]
- Bolay, H.; Söylemezoǧlu, F.; Nurlu, G.; Tuncer, S.; Vari, K. PCR detected hepatitis C virus genome in the brain of a case with progressive encephalomyelitis with rigidity. Clin. Neurol. Neurosurg. 1996, 98, 305–308. [Google Scholar] [CrossRef]
- Magira, E.E.; Alexopoulos, H.; Charitatos, E.; Michas, D.; Dalakas, M.C. Progressive encephalomyelitis with rigidity and myoclonus (PERM): Brucellosis as a possible triggering factor and long-term follow-up therapy with rituximab. Ther. Adv. Neurol. Disord. 2016, 9, 69–73. [Google Scholar] [CrossRef]
- Chmiela, T.; Rzepka, M.; Krzystanek, E.; Gorzkowska, A. A 50-Year-Old Patient with Guillain–Barré Syndrome after COVID-19: A Case Report. Medicina 2021, 57, 775. [Google Scholar] [CrossRef]
- Chroni, E.; Papadimitriou, A.; Avramidis, T.; Terentiou, A.E.; Tzioras, C.; Divari, R. Stiff-person like syndrome in a patient with multiple pituitary hormone deficiencies. Acta Neurol. Scand. 2000, 102, 403–405. [Google Scholar] [CrossRef]
- Goh, K.G.; Yusof Khan, A.H.K.; Nasruddin, A. Stiff Person-Like Syndrome: An Unusual Presentation of Pituitary Macroadenoma with Panhypopituitarism. Case Rep. Neurol 2022, 14, 157–161. [Google Scholar] [CrossRef]
- Anton, E. Hipopituitarism due to primary empty sella and uncommon muscular symptoms. Rheumatology 2012, 32, 565–566. [Google Scholar] [CrossRef]
- Borku Uysal, B.; Ikitimur, H.; Yavuzer, S.; Islamoglu, M.S.; Cengiz, M. Case Report: A COVID-19 Patient Presenting with Mild Rhabdomyolysis. Am. J. Trop. Med. 2020, 103, 847–850. [Google Scholar] [CrossRef]
- Paliwal, V.K.; Garg, R.K.; Gupta, A.; Tejan, N. Neuromuscular presentations in patients with COVID-19. Neurol. Sci. 2020, 41, 3039–3056. [Google Scholar] [CrossRef]
- Meegada, S.; Muppidi, V.; Wilkinson, D.C.; Siddamreddy, S.; Katta, S.K. Coronavirus Disease 2019-Induced Rhabdomyolysis. Cureus 2020, 12, e10123. [Google Scholar] [CrossRef]
- Piscitelli, D.; Perin, C.; Tremolizzo, L.; Peroni, F.; Cerri, C.G.; Cornaggia, C.M. Functional movement disorders in a patient with COVID-19. Neurol. Sci. 2020, 41, 2343–2344. [Google Scholar] [CrossRef]
- Ercoli, T.; Lutzoni, L.; Orofino, G.; Muroni, A.; Defazio, G. Functional neurological disorder after COVID-19 vaccination. Neurol. Sci. 2021, 42, 3989–3990. [Google Scholar] [CrossRef]
- Stone, J.; Carson, A.; Duncan, R.; Roberts, R.; Warlow, C.; Hibberd, C.; Coleman, R.; Cull, R.; Murray, G.; Pelosi, A.; et al. Who is referred to neurology clinics?--the diagnoses made in 3781 new patients. Clin. Neurol. Neurosurg. 2010, 112, 747–751. [Google Scholar] [CrossRef]
- Lidstone, S.C.; Costa-Parke, M.; Robinson, E.J.; Ercoli, T.; Stone, J. FMD GAP Study Group. Functional movement disorder gender, age and phenotype study: A systematic review and individual patient meta-analysis of 4905 cases. J. Neurol. Neurosurg. Psychiatry 2022, 93, 609–616. [Google Scholar] [CrossRef]
| Day of Hospitalization | CK Value | Grade of Rigidity |
|---|---|---|
| Day 1 | 253 U/L | + |
| Day 3 | 597 U/L | ++ |
| Day 4 | 12,030 U/L | ++ |
| Day 5 | 9797 U/L | + |
| Day 8 | 457 U/L | No rigidity |
| Associated Pathogen | Clinical Manifestation | Paraclinical Findings | Evolution |
|---|---|---|---|
| West Nile Virus | Increased muscle tone in left arm and legs (stiffness particularly in the arms and shoulder girdle area) Stiff appearance when walking Bradykinesia Hyperreflexia Plantar response extension bilaterally | Positive IgM and IgG antibodies to WNV in serum and CSF Positive serum anti-GAD antibodies Elevated Creatin-Kinase values CSF biochemistry, cellular count, and cultures Oligoclonal IgG antibodies in CSF Cervical and Brain MRI were normal Nerve conduction studies, repetitive nerve stimulation, and electromyography were normal | Complete resolution of a clinical picture after 3 months |
| Borrelia Burgdorferi | Pain and stiffness in the left leg; Spasmodic jerks and painful cramps in the left leg provoked by touch or loud noises; Difficulty walking with frequent falls; Reflex myoclonus in lower extremities which could be induced by touch, loud noises, touching or tapping the leg tendons or the bed | High CK values CSF analysis showed elevated proteins and elevated cell count Borrelia Burgdorferi-specific antibodies were found in serum and CSF Electromyography showed continuous motor activity in the muscles of the left leg Normal brain and spine MRI | Resolution of symptoms after 3 months |
| Hepatitis C Virus | Abnormal posture Motor and sensory deficits in upper and lower limbs Sphincter incontinence Diffuse painful muscle spasms in the extremities which could be induced emotional factors, noise and touch Hyporeflexia | HCV-RNA positive in serum Mild pleocytosis and elevated proteins at CSF analysis; Nerve conduction studies were normal Electromyography showed continuous muscle unit activity of agonist and antagonist muscles in the extremities; Normal brain and spine MRI | Unfavorable clinical outcome |
| Brucella spp. | Restricted vertical gaze movements; bilateral horizontal gaze-evoked nystagmus; diffuse spontaneous myoclonic spasms | Positive PCR test for Brucella in CSF Antiglycine receptor antibodies in serum and CSF; Normal brain and spine MRI; Continuous muscular activity on electromyography | Clinical improvement after 12 months |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sirbu, C.A.; Popescu, D.; Stefan, I.; Stefani, C.; Mitrica, M.; Anghel, D. COVID-19 Still Surprising Us—A Rare Movement Disorder Induced by Infection. Brain Sci. 2022, 12, 1733. https://doi.org/10.3390/brainsci12121733
Sirbu CA, Popescu D, Stefan I, Stefani C, Mitrica M, Anghel D. COVID-19 Still Surprising Us—A Rare Movement Disorder Induced by Infection. Brain Sciences. 2022; 12(12):1733. https://doi.org/10.3390/brainsci12121733
Chicago/Turabian StyleSirbu, Carmen Adella, Diana Popescu, Ion Stefan, Constantin Stefani, Marian Mitrica, and Daniela Anghel. 2022. "COVID-19 Still Surprising Us—A Rare Movement Disorder Induced by Infection" Brain Sciences 12, no. 12: 1733. https://doi.org/10.3390/brainsci12121733
APA StyleSirbu, C. A., Popescu, D., Stefan, I., Stefani, C., Mitrica, M., & Anghel, D. (2022). COVID-19 Still Surprising Us—A Rare Movement Disorder Induced by Infection. Brain Sciences, 12(12), 1733. https://doi.org/10.3390/brainsci12121733







