Abstract
Individuals affected by Coronavirus Disease 2019 (COVID-19) may experience psychiatric symptoms, including depression and suicidal ideation, that could lead to chronic impairment and a reduction in quality of life. Specifically, depressive disorder shows high incidence and may lead to chronic impairment and a reduction in the quality of life. To date, no studies on the presence of suicidality and quantitative analysis of depressive symptoms and their risk factors have yet been published. In this study, we aim to assess the prevalence of depressive symptoms and related risk factors at 3 months after discharge to home care following hospitalization for COVID-19 infection. Methods: Participants were contacted three months after hospital discharge from one of the five COVID-19 hospitals in Rome, as part of a larger project on health outcomes in COVID-19 inpatients (Long Term Neuropsychiatric Disorder in COVID-19 Project), and the Patient Health Questionnaire-9 (PHQ-9) was administered by telephone interview. Results: Of 115 participants, 14.8% (N = 17) received a PHQ-9-based diagnosis of depression, and n = 7 of them scored 1 or more on the item on suicidality. A linear regression model showed the predictive role of female sex, pulmonary chronic condition and previous mental disorder in the development of depressive disorder; the latter was confirmed also by binary logistic regression. Severity indexes of disease (length of hospitalization and intensive care treatment) were found not to be associated with the development of depressive symptoms. Conclusions: A small but clinically meaningful number of participants in the current study reported that they experienced symptoms of depression and suicidal ideation 3 months post-discharge from their COVID-19 hospitalization. In particular, given the findings that a history of prior psychiatric disorders was predictive of the development of depression symptoms, clinicians should carefully monitor for the presence of all psychiatric symptoms at follow-up visits.
1. Introduction
Since December 2019, the novel Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), the cause of the Coronavirus Disease 19 (COVID-19), has rapidly spread around the world [1]. In March 2020, Italy was severely affected by the epidemic and has the second-largest number of confirmed COVID-19 cases, after China [2].
Clinical manifestations of COVID-19 range from an asymptomatic disease to acute respiratory distress syndrome (ARDS), multiorgan failure and shock and can lead to death in up to 25–62% of critically ill patients [3,4,5,6]. Evidence has shown that it is crucial to arrange follow-up visits for discharged individuals in order to quickly identify possible organ damages and long-term sequelae [7].
Previous data on severe acute respiratory syndrome (SARS) infection showed that coronavirus is associated with sustained mental disorders and long-lasting neuropsychiatric consequences [8]. Specifically, COVID-19 individuals have shown symptoms of psychological distress that may lead to chronic impairment and a reduction in their quality of life; emerging evidence has also shown that, following hospitalization, these individuals are at high risk of developing Post-Traumatic Stress Disorder [9,10].
A few studies have focused on the relation between COVID-19 and depression during and after hospitalization [11,12,13]. These studies showed that symptoms of depression are highly prevalent during the hospital stay and tend to decrease after discharge. One study has reported data on the long-term prevalence of the subjective presence of depressive symptoms [14]. Although powerful in consideration of the number of participants involved, this study relies on one item, a 0–4 scale indicating the self-reported level of anxiety or depression. To our knowledge, no studies on the presence of suicidality and quantitative analysis of depressive symptoms and their risk factors have yet been published. The aim of this study was to assess the prevalence of depressive symptoms and related risk factors at 3 months after discharge to home care following hospitalization for COVID-19 infection. The study was carried out in a large COVID-19 University Hospital in Rome.
2. Materials and Methods
2.1. Participants
Participants were recruited among those admitted to the Division of Infectious Diseases, at the Department of Public Health and Infectious Diseases of Umberto I “Sapienza” University Hospital of Rome, during the height of the pandemic in Rome. As one of the 5 COVID-19 hospitals of Rome, “Umberto I” is a 1200-bed teaching hospital, with a catchment area of 600,000–1,200,000 people [15]. This study is part of a larger project on health outcomes in COVID-19 inpatients, named “Long Term Neuropsychiatric Disorder in COVID-19 Project”. Inclusion criteria included: age > 18 years, hospitalization for a confirmed case of COVID-19 and discharge to home care. Recruitment was carried out over two months. Individuals with a clinically evident cognitive impairment, active mental disorders or inadequate knowledge of the Italian language were excluded. Participants with non-remitting COVID-19, or unrelated clinical conditions, involving being transferred to other hospital wards or medical facilities, were also excluded.
Between one and two days before discharge, participants were approached by the unit doctors and received a complete explanation of the purpose and procedures of the study and gave written informed consent to participate. Clinical and demographic variables were retrieved from clinical records. Sociodemographic variables, comorbidities, previous mental health conditions, treatment undergone during hospitalization and length of hospital stay were included in the dataset. Three months after discharge, trained clinical raters contacted the participants by telephone. The telephone call included a renewal of the informed consent and an interview including specific tools. Although a face-to-face assessment with a structured psychiatric interview would have been preferable, this methodology was the only one available during the height of the pandemic. Information about the study and its aims were provided again, and verbal consensus was requested to confirm the informed consent provided during hospitalization. If they consented, information about current clinical state and new medical treatments was retrieved. In order to gather specific data on depressive symptomatology, raters administered the Patient Health Questionnaire-9 (PHQ-9). Individuals with signs of clinically significant mental distress during assessment were offered to be referred to the Psychiatry Outpatient Service of our hospital or other second-level mental health services, as appropriate. The study received the approval of the Sapienza University of Rome Ethical Committee (Ref. 109/2020).
2.2. Instruments
PHQ-9 is a validated screening tool for assessing the presence and severity of depression in the clinical setting [16,17]. Participants are asked to rate, between 0 (never) and 3 (almost every day), how frequently they experience a variety of depressive symptoms as reported by the Diagnostic and Statistical Manual of Mental Disorders fifth edition (DSM-5) (Figure 1) [18]. If any symptom is reported, participants are asked to rate from 0 to 3 how much impact such symptoms have on their daily functioning (i.e., working, taking care of home and getting along with others). For the purpose of this study, we used the continuous variable “total score” and a 10-point cut-off indicating the presence of clinically relevant depressive symptomatology [19].
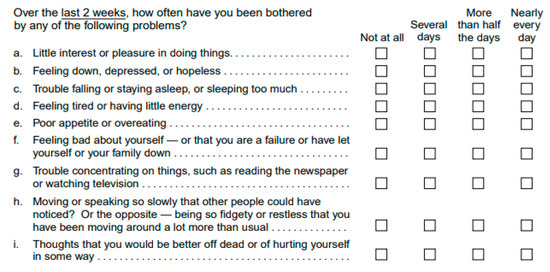
Figure 1.
Patient Health Questionnaire-9 (PHQ-9).
2.3. Statistical Analysis
Analysis was performed using Statistical Package for Social Science (SPSS) version 25 (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY, USA: IBM Corp).
Continuous variables were summarized into either medians with interquartile range (IQR, 25th and 75th percentile) or into means with standard deviation (±SD), as appropriate, along with the related ranges (minimum–maximum). Categorical variables were summarized as frequencies (n), proportions or percentages and rates, as appropriate.
Univariate analyses were conducted for all available sociodemographic and clinical variables. In order to select potentially meaningful organic conditions, we built a stepwise regression model predicting PHQ-9 total score, including all the pre-existing chronic medical conditions as possible predictors of depression (obesity, immunodepression, hypertension, dysthyroidism, cardiopathy, diabetes, cancer, inflammatory bowel diseases and vascular pathologies) [20,21,22,23,24,25,26,27]. Obesity was considered as body mass index (BMI) > 30 (<18.5 underweight range, 18.5–24.9 healthy weight range, 25–29.9 overweight range, >30 obese range) [28]. A multivariate linear regression model was built to analyze possible predictors of the PHQ-9 total score and a binary logistic regression model was built to test for predictors of clinically relevant depressive symptomatology. Odds ratios (ORs) and 95% confidence intervals (95% CIs) were calculated for all associations. p-value < 0.05 was considered statistically significant.
3. Results
A total of 183 consecutive participants discharged to home care during the study time span were assessed for eligibility. Of these, 68 were excluded (n = 25 did not fulfil inclusion criteria, n = 46 were missed, n = 2 declined to participate). A total of n = 115 individuals were recruited.
No significant differences in sociodemographic variables were found between participants who were recruited and those lost during recruitment in age (median 57 (IQR 25–75%) 48–66 vs. 60.5 (IQR 25–75%) 48–72, respectively p = 0.200) or sex (male 54% vs. 42%, respectively p = 0.300).
At 3-month follow up, 14.8% of the sample (N = 17) received a PHQ-9-based diagnosis of depression (total score > 9). Mean PHQ-9 total score was 4.82 ± 0.79 (range= 0–25). n = 41 (35.65%) participants scored at least 1 on the item on subjective impairment, with n = 7 scoring 2 or more. A total of n = 7 participants scored 1 or more on the item on suicidality (these individuals were referred to secondary mental health services).
Demographic and clinical characteristics of the sample are presented in Table 1.

Table 1.
Demographic and clinical characteristics of the population.
The stepwise regression model highlighted a potential role of chronic pulmonary conditions, over and above other chronic conditions (B = 4.50; SE = 1.26; p < 0.001). We therefore included anamnesis of chronic pulmonary conditions in the models. The linear regression model predicting PHQ-9 total score (Table 2) highlighted the predictive role of chronic pulmonary conditions, previous mental disorders and sex. On the other hand, the binary logistic regression model predicting a PHQ-9 diagnosis of depression (Table 3) confirmed the predictive role of previous psychiatric diagnosis only.

Table 2.
Linear regression model predicting PHQ-9 total score.

Table 3.
Binary logistic regression model predicting PHQ-9 based diagnosis of depression.
4. Discussion
In this observational study on COVID-19 survivors discharged after hospitalization for COVID-19 during the height of the pandemic in Rome, we analyzed quantitative aspects of depression and the presence of suicidality at a 3-month FU. More than one out of ten participants received a provisional diagnosis of depressive disorder and the average and more than one of three reported some degree of impairment caused by depressive symptoms. Concerningly, 6% of the individuals reported the onset of suicidality. Findings from this study confirm and deepen the emerging evidence from other studies on the topic and are in line with similar reports from past epidemics (e.g., the SARS epidemic in 2002–2004).
The etiology of depression following hospitalization due to infection with coronavirus is likely to be multifactorial, involving organic, psychological and social factors. On an organic level, causes might include the direct effects of the viral infection, cerebrovascular consequences, the immunological response and medical interventions. On a psychological level, we believe that the fear of a novel severe and potentially fatal illness, the following stigma and the isolation have played a role [29,30,31]. This is especially true in consideration of the domino effect that COVID-19 had, spreading rapidly within households and family members [32]. Our data highlight the role of previous psychiatric conditions and female sex, which are commonly known factors in the development of mental disorders in response to a variety of stressors [33]. Although further research is needed to understand the role of chronic pulmonary diseases, considering that chronic pulmonary disease was a widely known risk factor for COVID-19 severity, we hypothesize that it might have worked as a booster of fear (before, during and after hospitalization) and of prophylactic social isolation. This hypothesis would be in line with our data showing how, in our cohort, the presence of depressive symptomatology is not associated with variables indicating a more severe disease (i.e., duration of hospitalization, ICU treatment).
We hypothesize that social factors played a role in the development of depressive symptoms: grief, fears of loss and stigma, as well as the repeated exposure to stressors, such as the restrictive measures implemented nationwide (e.g., full lockdown) and the daily media reports on local and global consequences of COVID-19. Indeed, evidence from different conditions has shown that these factors in their complexity might increase vulnerability to depressive disorder [34]. Moreover, the economical and labor crisis should also be taken into account in consideration of the literature supporting their relation with depression and anxiety [35]. Regarding this hypothesis, it is interesting to note how social support, which, in many cases, was drastically reduced due to restrictions, seems to play a moderating role in the relation between economic stressors and depression [36]. Further research is needed to test these hypotheses and attempt to uncover the complex pathogenesis of depression following severe COVID-19 infection.
Limitations
The telephone interview methodology is the major limitation of our study. Although this method has been used successfully in previous research during the current pandemic and raters were trained in interview skills before this study, a face-to-face assessment with a structured psychiatric interview would have been preferable [37,38]. A face-to-face interview, indeed, would offer the chance to perform cross-checking with visible symptomatology and investigate possible impairments in daily functions. Despite this, the methodology that we used was the only one available during the height of the pandemic and in a setting where part of the population was not able to use a virtual platform.
5. Conclusions
A small but meaningful number of COVID-19 individuals experience some discomfort due to depressive symptoms and clinically relevant depressive symptomatology after hospitalization, developing, in some cases, suicidal ideation. Further research, including more complete assessment and face-to-face psychiatric interviews, is needed to understand the complex etiology of this long-term consequence. Clinicians should consider evaluating the presence of depression and of suicidal ideation in follow-up control visits for COVID-19 individuals.
Author Contributions
Conceptualization, P.V., R.S., G.d. and L.T.; methodology, A.E.K., P.V. and G.d.; software, C.B., C.T.; formal analysis, C.B., P.V. and R.S.; investigation, P.V., C.D.N., C.T. and F.A. (Francesco Alessandri); resources, C.T., F.A. (Federica Alessi), C.D.N. and G.C.; data curation, G.d, G.C., P.V., C.M.M., C.B., L.T. and R.S.; writing—original draft preparation, F.A. (Francesco Alessandri), R.S. and P.V.; writing—review and editing, C.M.M., G.d., G.C., A.E.K. and L.T.; project administration, G.d. and L.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Sapienza, University of Rome.
Institutional Review Board Statement
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethical Committee of Sapienza University of Rome (Ref. 109/2020).
Informed Consent Statement
Written informed consent was collected from each participant prior to study inclusion.
Data Availability Statement
The raw data and materials used for this study are available upon request.
Acknowledgments
We would like to acknowledge the staff of the Department of Public Health and Infectious Diseases of Sapienza University of Rome—Policlinico “Umberto I” for their efforts to combat the COVID-19 pandemic, and all the patients for their kind participation in this project.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef]
- Remuzzi, A.; Remuzzi, G. COVID-19 and Italy: What next? Lancet 2020, 395, 1225–1228. [Google Scholar] [CrossRef]
- Pan, X.; Chen, D.; Xia, Y.; Wu, X.; Li, T.; Ou, X.; Zhou, L.; Liu, J. Asymptomatic cases in a family cluster with SARS-CoV-2 infection. Lancet Infect. Dis. 2020, 20, 410–411. [Google Scholar] [CrossRef]
- Richardson, S.; Hirsch, J.S.; Narasimhan, M.; Crawford, J.M.; McGinn, T.; Davidson, K.W.; Northwell COVID-19 Research Consortium. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized with COVID-19 in the New York City Area. JAMA 2020, 323, 2052–2059. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Yu, Y.; Xu, J.; Shu, H.; Xia, J.; Liu, H.; Wu, Y.; Zhang, L.; Yu, Z.; Fang, M.; et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir. Med. 2020, 8, 475–481. [Google Scholar] [CrossRef] [Green Version]
- Auld, S.; Caridi-Scheible, M.; Blum, J.M.; Robichaux, C.J.; Kraft, C.S.; Jacob, J.T.; Jabaley, C.S.; Carpenter, D.; Kaplow, R.; Hernandez, A.C.; et al. ICU and Ventilator Mortality among Critically Ill Adults with COVID-19. medRxiv 2020. Update in: Crit. Care Med. 2020, 48, e799–e804. [Google Scholar] [CrossRef] [Green Version]
- Balachandar, V.; Mahalaxmi, I.; Subramaniam, M.; Kaavya, J.; Kumar, N.S.; Laldinmawii, G.; Narayanasamy, A.; Reddy, P.J.K.; Sivaprakash, P.; Kanchana, S.; et al. Follow-up studies in COVID-19 recovered patients - is it mandatory? Sci. Total Environ. 2020, 729, 139021. [Google Scholar] [CrossRef] [PubMed]
- Lam, M.H.-B.; Wing, Y.-K.; Yu, M.W.-M.; Leung, C.-M.; Ma, R.C.W.; Kong, A.P.S.; So, W.; Fong, S.Y.-Y.; Lam, S.-P. Mental Morbidities and Chronic Fatigue in Severe Acute Respiratory Syndrome Survivors: Long-term Follow-up. Arch. Intern. Med. 2009, 169, 2142–2147. [Google Scholar] [CrossRef] [Green Version]
- Rogers, J.P.; Chesney, E.; Oliver, D.; Pollak, T.A.; McGuire, P.; Fusar-Poli, P.; Zandi, M.; Lewis, G.; David, A. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 2020, 7, 611–627. [Google Scholar] [CrossRef]
- Tarsitani, L.; Vassalini, P.; Koukopoulos, A.; Borrazzo, C.; Alessi, F.; Di Nicolantonio, C.; Serra, R.; Alessandri, F.; Ceccarelli, G.; Mastroianni, C.M.; et al. Post-traumatic Stress Disorder among COVID-19 Survivors at 3-Month Follow-up After Hospital Discharge. J. Gen. Intern. Med. 2021, 36, 1702–1707. [Google Scholar] [CrossRef] [PubMed]
- Garrigues, E.; Janvier, P.; Kherabi, Y.; Le Bot, A.; Hamon, A.; Gouze, H.; Doucet, L.; Berkani, S.; Oliosi, E.; Mallart, E.; et al. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J. Infect. 2020, 81, e4–e6. [Google Scholar] [CrossRef]
- Zandifar, A.; Badrfam, R.; Yazdani, S.; Arzaghi, S.M.; Rahimi, F.; Ghasemi, S.; Khamisabadi, S.; Khonsari, N.M.; Qorbani, M. Prevalence and severity of depression, anxiety, stress and perceived stress in hospitalized patients with COVID-19. J. Diabetes Metab. Disord. 2020, 19, 1431–1438. [Google Scholar] [CrossRef]
- Matalon, N.; Dorman-Ilan, S.; Hasson-Ohayon, I.; Hertz-Palmor, N.; Shani, S.; Basel, D.; Gross, R.; Chen, W.; Abramovich, A.; Afek, A.; et al. Trajectories of post-traumatic stress symptoms, anxiety, and depression in hospitalized COVID-19 patients: A one-month follow-up. J. Psychosom. Res. 2021, 143, 110399. [Google Scholar] [CrossRef]
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; Cook, J.R.; Nordvig, A.S.; Shalev, D.; Sehrawat, T.S.; et al. Post-acute COVID-19 syndrome. Nat. Med. 2021, 27, 601–615. [Google Scholar] [CrossRef] [PubMed]
- Ceccarelli, G.; Spagnolello, O.; Borrazzo, C.; Vullo, F.; Cuomo, M.R.; Milocco, M.; Angeletti, S.; Ciccozzi, M.; Mastroianni, C.M.; D’Ettorre, G.; et al. Impact of the 2017 measles outbreak on the emergency care system of a large tertiary-care teaching hospital in Italy: A retrospective analysis. Eur. J. Public Health 2019, 29, 966–971. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Janet, B.W. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. JAMA 1999, 282, 1737–1744. [Google Scholar] [CrossRef] [Green Version]
- Levis, B.; Benedetti, A.; Thombs, B.D. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: Individual participant data meta-analysis. BMJ 2019, 365, l1476. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; (DSM-5); American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Alexopoulos, G.S.; Buckwalter, K.; Olin, J.; Martinez, R.; Wainscott, C.; Krishnan, K.R. Comorbidity of late life depression: An opportunity for research on mechanisms and treatment. Biol. Psychiatry 2002, 52, 543–558. [Google Scholar] [CrossRef]
- Carney, R.M.; Freedland, K.E. Depression, mortality, and medical morbidity in patients with coronary heart disease. Biol. Psychiatry 2003, 54, 241–247. [Google Scholar] [CrossRef]
- McEwen, B.S. Mood disorders and allostatic load. Biol. Psychiatry 2003, 54, 200–207. [Google Scholar] [CrossRef]
- Gorkhali, B.; Sharma, S.; Amatya, M.; Acharya, D.; Sharma, M. Anxiety and Depression among Patients with Thyroid Function Disorders. J. Nepal Health Res. Counc. 2020, 18, 373–378. [Google Scholar] [CrossRef] [PubMed]
- McElroy, S.L.; Keck, P.E. Metabolic Syndrome in Bipolar Disorder. J. Clin. Psychiatry 2014, 75, 46–61. [Google Scholar] [CrossRef]
- Jonas, B.S.; Lando, J.F. Negative Affect as a Prospective Risk Factor for Hypertension. Psychosom. Med. 2000, 62, 188–196. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neuendorf, R.; Harding, A.; Stello, N.; Hanes, D.; Wahbeh, H. Depression and anxiety in patients with Inflammatory Bowel Disease: A systematic review. J. Psychosom. Res. 2016, 87, 70–80. [Google Scholar] [CrossRef]
- Pinquart, M.; Duberstein, P. Depression and cancer mortality: A meta-analysis. Psychol. Med. 2010, 40, 1797–1810. [Google Scholar] [CrossRef]
- Nuttall, F.Q. Body Mass Index. Nutr. Today 2015, 50, 117–128. [Google Scholar] [CrossRef] [Green Version]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [Green Version]
- Yeh, E.A.; Collins, A.; Cohen, M.E.; Duffner, P.K.; Faden, H. Detection of Coronavirus in the Central Nervous System of a Child With Acute Disseminated Encephalomyelitis. Pediatrics 2003, 113, e73–e76. [Google Scholar] [CrossRef] [Green Version]
- Tan, Y.-K.; Goh, C.; Leow, A.S.T.; Tambyah, P.A.; Ang, A.; Yap, E.-S.; Tu, T.-M.; Sharma, V.K.; Yeo, L.L.L.; Chan, B.P.L.; et al. COVID-19 and ischemic stroke: A systematic review and meta-summary of the literature. J. Thromb. Thrombolysis 2020, 50, 587–595. [Google Scholar] [CrossRef]
- Grijalva, C.G.; Rolfes, M.A.; Zhu, Y.; McLean, H.Q.; Hanson, K.E.; Belongia, E.A.; Halasa, N.B.; Kim, A.; Reed, C.; Fry, A.M.; et al. Transmission of SARS-COV-2 Infections in Households—Tennessee and Wisconsin, April–September 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1631–1634. [Google Scholar] [CrossRef]
- Sacks, D.; Baxter, B.; Campbell, B.C.; Carpenter, J.S.; Cognard, C.; Dippel, D.; Eesa, M.; Fischer, U.; Hausegger, K.; Hirsch, J.A. Multisociety Consensus Quality Improvement Revised Consensus Statement for Endovascular Therapy of Acute Ischemic Stroke. Int. J. Stroke 2018, 13, 612–632. [Google Scholar] [CrossRef] [Green Version]
- Gilman, S.E.; Trinh, N.-H.; Smoller, J.W.; Fava, M.; Murphy, J.M.; Breslau, J. Psychosocial stressors and the prognosis of major depression: A test of Axis IV. Psychol. Med. 2013, 43, 303–316. [Google Scholar] [CrossRef] [Green Version]
- Aihara, H.; Iki, M. An Ecological Study of the Relations between the Recent High Suicide Rates and Economic and Demographic Factors in Japan. J. Epidemiol. 2003, 13, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Viseu, J.; Leal, R.; de Jesus, S.N.; Pinto, P.; Pechorro, P.; Greenglass, E. Relationship between economic stress factors and stress, anxiety, and depression: Moderating role of social support. Psychiatry Res. 2018, 268, 102–107. [Google Scholar] [CrossRef] [PubMed]
- Antoun, J.; Brown, D.; Jones, D.; Sangala, N.; Lewis, R.; Shepherd, A.; McNarry, M.; Mackintosh, K.; Mason, L.; Corbett, J.; et al. Understanding the Impact of Initial COVID-19 Restrictions on Physical Activity, Wellbeing and Quality of Life in Shielding Adults with End-Stage Renal Disease in the United Kingdom Dialysing at Home versus In-Centre and Their Experiences with Telemedicine. Int. J. Environ. Res. Public Health 2021, 18, 3144. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Luo, D.; Haase, J.E.; Guo, Q.; Wang, X.Q.; Liu, S.; Xia, L.; Liu, Z.; Yang, J.; Yang, B.X. The experiences of health-care providers during the COVID-19 crisis in China: A qualitative study. Lancet Glob. Health 2020, 8, e790–e798. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).