Effect of Multisession Progressive Gait-Slip Training on Fall-Resisting Skills of People with Chronic Stroke: Examining Motor Adaptation in Reactive Stability
Abstract
1. Introduction
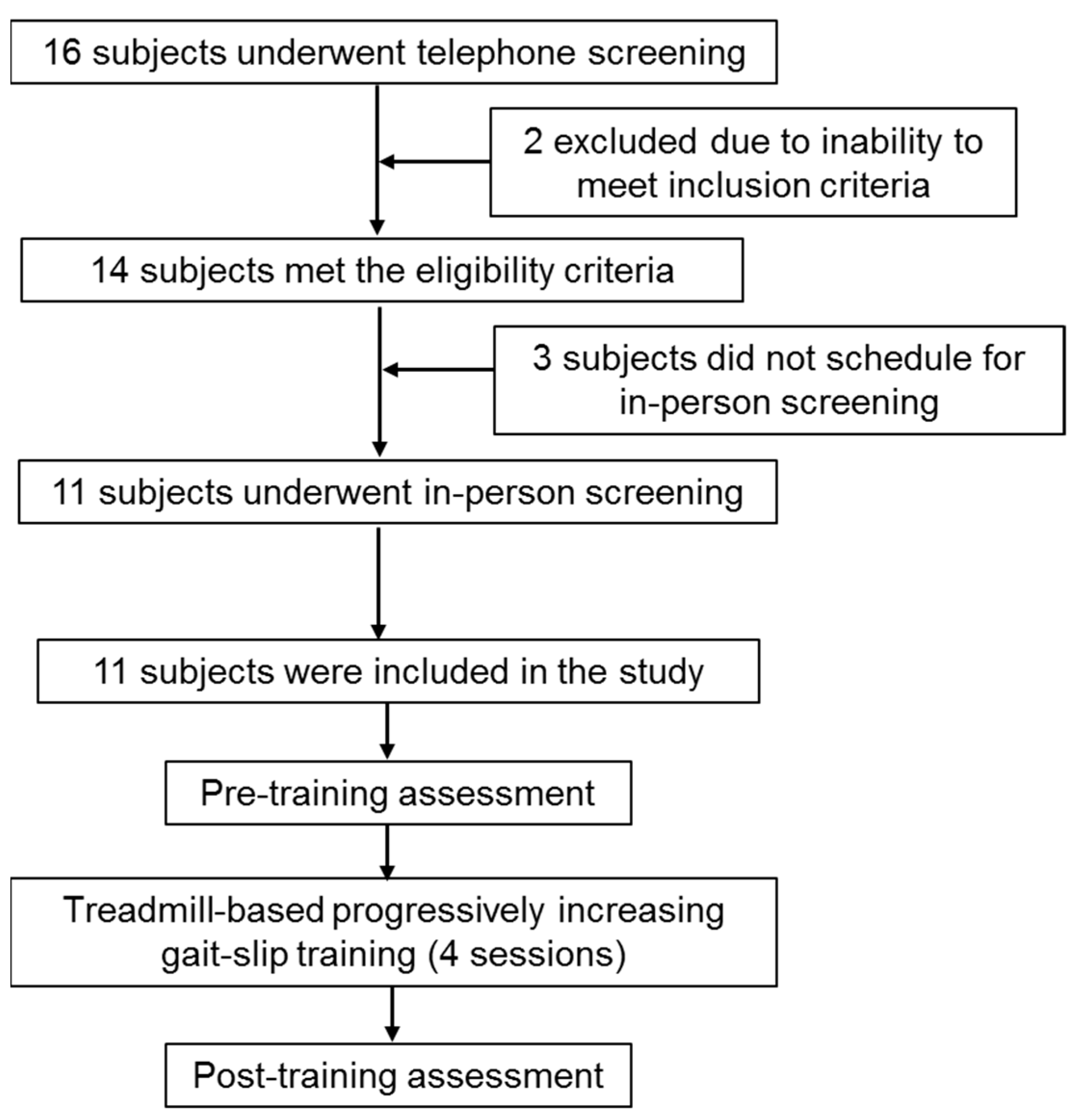
2. Methods
2.1. Participants
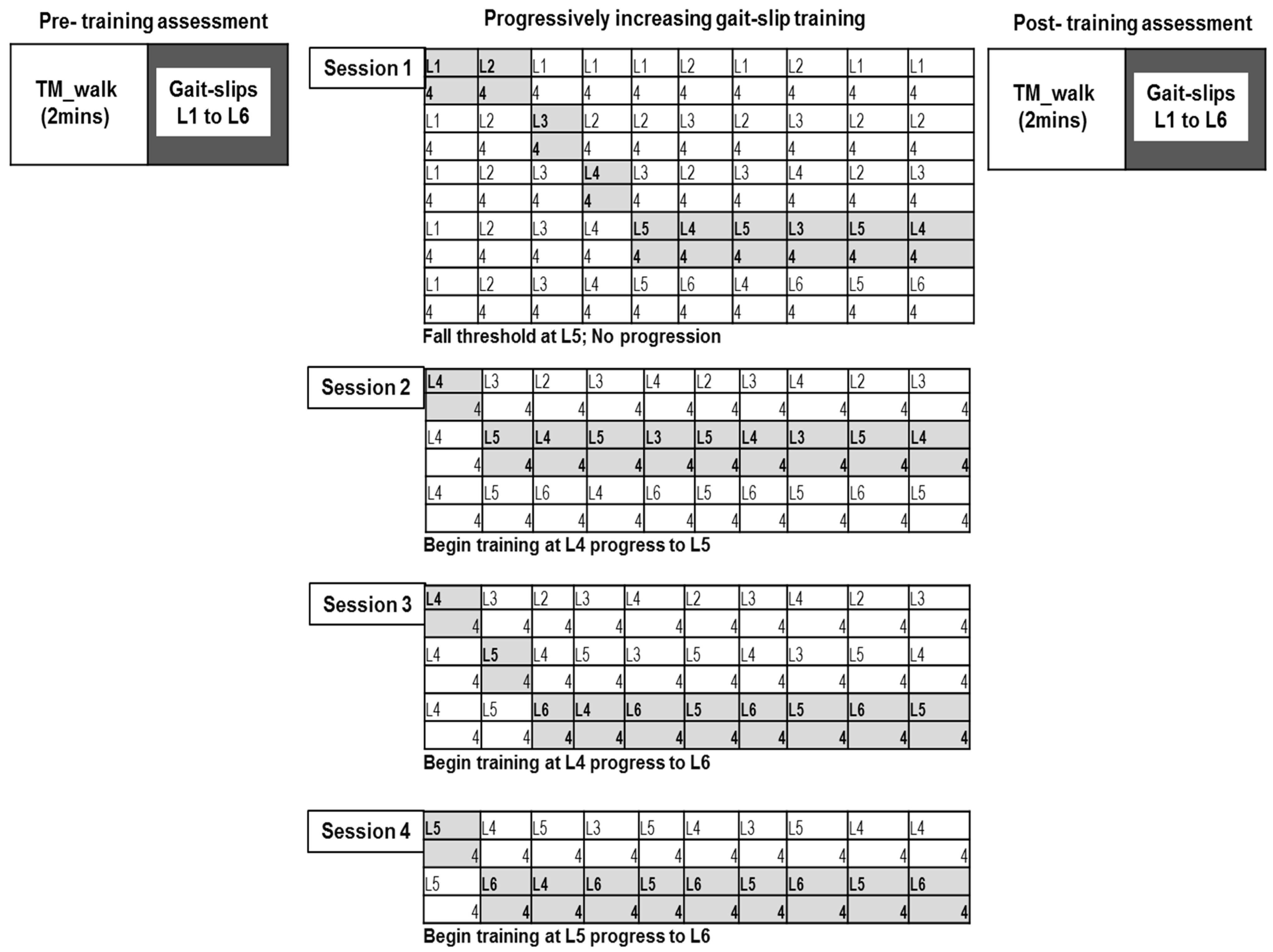
2.2. Training Protocol
2.3. Assessment
2.4. Intervention
2.5. Data Collection
2.6. Outcome Measures
3. Results
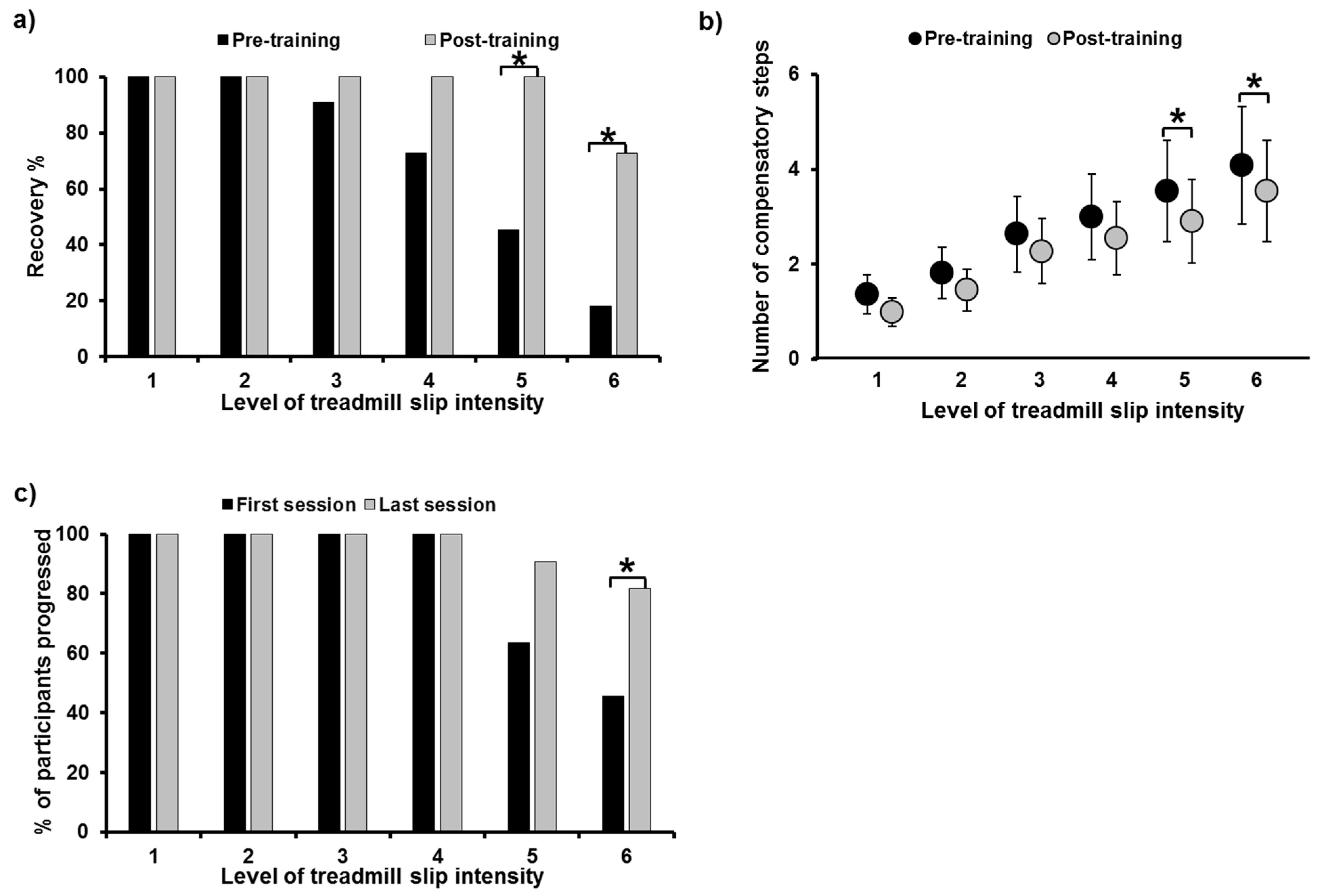
3.1. Effect of Multisession, Treadmill-Based Gait-Slip Training on Gait-Slips
3.2. Number of Compensatory Steps
3.3. Progression in Training Slip Intensity
3.4. Effect of Multisession, Treadmill-Based Gait-Slip Training on Clinical Measures
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics—2020 Update: A Report from the American Heart Association. Circulation 2020, 141, e139–e596. [Google Scholar] [CrossRef]
- Johnson, W.; Onuma, O.; Owolabi, M.; Sachdev, S. Stroke: A global response is needed. Bull. World Health Organ. 2016, 94, 634. [Google Scholar] [CrossRef]
- Weerdesteijn, V.; Niet, M.; Van Duijnhoven, H.; Geurts, A.C. Falls in Individuals with Stroke. J. Rehabil. Res. Dev. 2008, 45, 1195–1214. [Google Scholar] [CrossRef]
- Lamb, S.; Ferrucci, L.; Volapto, S.; Fried, L.; Guralnik, J. Risk Factors for Falling in Home-Dwelling Older Women with Stroke. Stroke 2003, 34, 494–501. [Google Scholar] [CrossRef]
- Hyndman, D.; Ashburn, A.; Stack, E. Fall events among people with stroke living in the community: Circumstances of falls and characteristics of fallers. Arch. Phys. Med. Rehabil. 2002, 83, 165–170. [Google Scholar] [CrossRef]
- Harris, J.; Eng, J.J.; Marigold, D.S.; Tokuno, C.D.; Louis, C.L. Relationship of Balance and Mobility to Fall Incidence in People With Chronic Stroke. Phys. Ther. 2005, 85, 150–158. [Google Scholar] [CrossRef]
- Schmid, A.A.; Yaggi, H.K.; Burrus, N.; McClain, V.; Austin, C.; Ferguson, J.; Fragoso, C.; Sico, J.J.; Miech, E.J.; Matthias, M.S.; et al. Circumstances and consequences of falls among people with chronic stroke. J. Rehabil. Res. Dev. 2013, 50, 1277–1286. [Google Scholar] [CrossRef]
- Jørgensen, L.; Engstad, T.; Jacobsen, B.K. Higher incidence of falls in long-term stroke survivors than in population controls: Depressive symptoms predict falls after stroke. Stroke 2002, 33, 542–547. [Google Scholar] [CrossRef] [PubMed]
- Minet, L.R.; Peterson, E.; von Koch, L.; Ytterberg, C. Occurrence and predictors of falls in people with stroke: Six-year prospective study. Stroke 2015, 46, 2688–2690. [Google Scholar] [CrossRef] [PubMed]
- Xu, T.; Clemson, L.; O’Loughlin, K.; Lannin, N.; Dean, C.; Koh, G. Risk Factors for Falls in Community Stroke Survivors: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2018, 99, 563–573.e5. [Google Scholar] [CrossRef] [PubMed]
- Shumway-Cook, A.; Woollacott, M.H. Motor Control: Translating Research into Clinical Practice; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2007. [Google Scholar]
- Maki, B.E.; McIlroy, W.E. The role of limb movements in maintaining upright stance: The “change-in-support” strategy. Phys. Ther. 1997, 77, 488–507. [Google Scholar] [CrossRef]
- Runge, C.; Shupert, C.; Horak, F.; Zajac, F. Ankle and hip postural strategies defined by joint torques. Gait Posture 1999, 10, 161–170. [Google Scholar] [CrossRef]
- Lakhani, B.; Mansfield, A.; Inness, E.L.; McIlroy, W. Compensatory stepping responses in individuals with stroke: A pilot study. Physiother. Theory Pr. 2010, 27, 299–309. [Google Scholar] [CrossRef] [PubMed]
- Mansfield, A.; Inness, E.L.; Lakhani, B.; McIlroy, W.E. Determinants of Limb Preference for Initiating Compensatory Stepping Poststroke. Arch. Phys. Med. Rehabil. 2012, 93, 1179–1184. [Google Scholar] [CrossRef] [PubMed]
- Salot, P.; Patel, P.; Bhatt, T. Reactive Balance in Individuals with Chronic Stroke: Biomechanical Factors Related to Perturbation-Induced Backward Falling. Phys. Ther. 2016, 96, 338–347. [Google Scholar] [CrossRef] [PubMed]
- Gerards, M.H.; McCrum, C.; Mansfield, A.; Meijer, K. Perturbation-based balance training for falls reduction among older adults: Current evidence and implications for clinical practice. Geriatr. Gerontol. Int. 2017, 17, 2294–2303. [Google Scholar] [CrossRef] [PubMed]
- Mansfield, A.; Wong, J.S.; Bryce, J.; Knorr, S.; Patterson, K.K. Does Perturbation-Based Balance Training Prevent Falls? Systematic Review and Meta-Analysis of Preliminary Randomized Controlled Trials. Phys. Ther. 2015, 95, 700–709. [Google Scholar] [CrossRef] [PubMed]
- McCrum, C.; Gerards, M.H.G.; Karamanidis, K.; Zijlstra, W.; Meijer, K. A systematic review of gait perturbation paradigms for improving reactive stepping responses and falls risk among healthy older adults. Eur. Rev. Aging Phys. Act. 2017, 14, 1–11. [Google Scholar] [CrossRef]
- Bhatt, T.; Yang, F.; Pai, Y.-C. Learning to Resist Gait-Slip Falls: Long-Term Retention in Community-Dwelling Older Adults. Arch. Phys. Med. Rehabil. 2012, 93, 557–564. [Google Scholar] [CrossRef] [PubMed]
- Pai, Y.-C.; Bhatt, T.; Yang, F.; Wang, E. Perturbation Training Can Reduce Community-Dwelling Older Adults’ Annual Fall Risk: A Randomized Controlled Trial. J. Gerontol. Ser. A Boil. Sci. Med. Sci. 2014, 69, 1586–1594. [Google Scholar] [CrossRef]
- Grabiner, M.D.; Bareither, M.L.; Gatts, S.; Marone, J.; Troy, K. Task-Specific Training Reduces Trip-Related Fall Risk in Women. Med. Sci. Sports Exerc. 2012, 44, 2410–2414. [Google Scholar] [CrossRef]
- Parijat, P.; Lockhart, T.E. Effects of Moveable Platform Training in Preventing Slip-Induced Falls in Older Adults. Ann. Biomed. Eng. 2011, 40, 1111–1121. [Google Scholar] [CrossRef] [PubMed]
- Lurie, J.D.; Zagaria, A.B.; Ellis, L.; Pidgeon, D.; Gill-Body, K.M.; Burke, C.; Armbrust, K.; Cass, S.; Spratt, K.F.; McDonough, C.M. Surface Perturbation Training to Prevent Falls in Older Adults: A Highly Pragmatic, Randomized Controlled Trial. Phys. Ther. 2020, 100, 1153–1162. [Google Scholar] [CrossRef]
- Bhatt, T.; Dusane, S.; Patel, P. Does severity of motor impairment affect reactive adaptation and fall-risk in chronic stroke survivors? J. Neuroeng. Rehabil. 2019, 16, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Nevisipour, M.; Grabiner, M.D.; Honeycutt, C.F. A single session of trip-specific training modifies trunk control following treadmill induced balance perturbations in stroke survivors. Gait Posture 2019, 70, 222–228. [Google Scholar] [CrossRef]
- Dusane, S.; Bhatt, T. Mixed slip-trip perturbation training for improving reactive responses in people with chronic stroke. J. Neurophysiol. 2020, 124, 20–31. [Google Scholar] [CrossRef] [PubMed]
- Punt, M.; Bruijn, S.M.; van de Port, I.G.; de Rooij, I.J.; Wittink, H.; van Dieën, J.H. Does a perturbation-based gait intervention enhance gait stability in fall-prone stroke survivors? A pilot study. J. Appl. Biomech. 2019, 35, 173–181. [Google Scholar] [CrossRef]
- Pigman, J.; Reisman, D.S.; Pohlig, R.T.; Jeka, J.J.; Wright, T.R.; Conner, B.C.; Petersen, D.A.; Crenshaw, J.R. Anterior fall-recovery training applied to individuals with chronic stroke. Clin. Biomech. 2019, 69, 205–214. [Google Scholar] [CrossRef]
- Handelzalts, S.; Kenner-Furman, M.; Gray, G.; Soroker, N.; Shani, G.; Melzer, I. Effects of Perturbation-Based Balance Training in Subacute Persons with Stroke: A Randomized Controlled Trial. Neurorehabilit. Neural Repair 2019, 33, 213–224. [Google Scholar] [CrossRef] [PubMed]
- Van Duijnhoven, H.J.R.; Roelofs, J.M.B.; Boer, J.J.D.; Lem, F.C.; Hofman, R.; Van Bon, G.E.A.; Geurts, A.C.H.; Weerdesteyn, V. Perturbation-Based Balance Training to Improve Step Quality in the Chronic Phase After Stroke: A Proof-of-Concept Study. Front. Neurol. 2018, 9, 980. [Google Scholar] [CrossRef]
- Mansfield, A.; Aqui, A.; Danells, C.J.; Knorr, S.; Centen, A.; DePaul, V.; Schinkel-Ivy, A.; Brooks, D.; Inness, E.L.; Mochizuki, G. Does perturbation-based balance training prevent falls among individuals with chronic stroke? A randomised controlled trial. BMJ Open 2018, 8, e021510. [Google Scholar] [CrossRef] [PubMed]
- Schinkel-Ivy, A.; Huntley, A.; Aqui, A.; Mansfield, A. Does Perturbation-Based Balance Training Improve Control of Reactive Stepping in Individuals with Chronic Stroke? J. Stroke Cerebrovasc. Dis. 2019, 28, 935–943. [Google Scholar] [CrossRef]
- Dusane, S.; Gangwani, R.; Patel, P.; Bhatt, T. Does stroke-induced sensorimotor impairment and perturbation intensity affect gait-slip outcomes? J. Biomech. 2021, 118, 110255. [Google Scholar] [CrossRef]
- Kajrolkar, T.; Bhatt, T. Falls-risk post-stroke: Examining contributions from paretic versus non paretic limbs to unexpected forward gait slips. J. Biomech. 2016, 49, 2702–2708. [Google Scholar] [CrossRef] [PubMed]
- Kajrolkar, T.; Yang, F.; Pai, Y.-C.; Bhatt, T. Dynamic stability and compensatory stepping responses during anterior gait–slip perturbations in people with chronic hemiparetic stroke. J. Biomech. 2014, 47, 2751–2758. [Google Scholar] [CrossRef] [PubMed]
- Boyne, P.; Scholl, V.; Doren, S.; Carl, D.; Billinger, S.A.; Reisman, D.S.; Gerson, M.; Kissela, B.; Vannest, J.; Dunning, K. Locomotor training intensity after stroke: Effects of interval type and mode. Top. Stroke Rehabil. 2020, 27, 483–493. [Google Scholar] [CrossRef]
- Rose, M.H.; Løkkegaard, A.; Sonne-Holm, S.; Jensen, B.R. Improved clinical status, quality of life, and walking capacity in Parkinson’s disease after body weight-supported high-intensity locomotor training. Arch. Phys. Med. Rehabil. 2013, 94, 687–692. [Google Scholar] [CrossRef]
- Holleran, C.L.; Rodriguez, K.S.; Echauz, A.; Leech, K.A.; Hornby, T.G. Potential Contributions of Training Intensity on Locomotor Performance in Individuals with Chronic Stroke. J. Neurol. Phys. Ther. 2015, 39, 95–102. [Google Scholar] [CrossRef]
- Leech, K.A.; Kinnaird, C.R.; Holleran, C.L.; Kahn, J.; Hornby, T.G. Effects of Locomotor Exercise Intensity on Gait Performance in Individuals with Incomplete Spinal Cord Injury. Phys. Ther. 2016, 96, 1919–1929. [Google Scholar] [CrossRef]
- Liu, X.; Bhatt, T.; Pai, Y.-C. (Clive) Intensity and generalization of treadmill slip training: High or low, progressive increase or decrease? J. Biomech. 2016, 49, 135–140. [Google Scholar] [CrossRef]
- Hak, L.; Houdijk, H.; Steenbrink, F.; Mert, A.; van der Wurff, P.; Beek, P.J.; van Dieën, J.H. Speeding up or slowing down?: Gait adaptations to preserve gait stability in response to balance perturbations. Gait Posture 2012, 36, 260–264. [Google Scholar] [CrossRef]
- Van Ooijen, M.W.; Roerdink, M.; Trekop, M.; Janssen, T.W.J.; Beek, P.J. The efficacy of treadmill training with and without projected visual context for improving walking ability and reducing fall incidence and fear of falling in older adults with fall-related hip fracture: A randomized controlled trial. BMC Geriatr. 2016, 16, 215. [Google Scholar] [CrossRef]
- Schmidt, R.A.; Wrisberg, C.A. Motor Learning and Performance: A Situation-Based Learning Approach; Human kinetics: Champaign, IL, USA, 2008. [Google Scholar]
- Savin, D.N.; Tseng, S.-C.; Whitall, J.; Morton, S.M. Poststroke Hemiparesis Impairs the Rate but not Magnitude of Adaptation of Spatial and Temporal Locomotor Features. Neurorehabilit. Neural Repair 2012, 27, 24–34. [Google Scholar] [CrossRef][Green Version]
- Lee, A.; Bhatt, T.; Liu, X.; Wang, Y.; Wang, S.; Pai, Y.-C. (Clive) Can Treadmill Slip-Perturbation Training Reduce Longer-Term Fall Risk Upon Overground Slip Exposure? J. Appl. Biomech. 2020, 36, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Melnick, M.J. Effects of Overlearning on the Retention of a Gross Motor Skill. Res. Q. Am. Assoc. Health Phys. Educ. Recreat. 1971, 42, 60–69. [Google Scholar] [CrossRef]
- Driskell, J.E.; Willis, R.P.; Copper, C. Effect of overlearning on retention. J. Appl. Psychol. 1992, 77, 615. [Google Scholar] [CrossRef]
- Davis, R.B.; Õunpuu, S.; Tyburski, D.; Gage, J.R. A gait analysis data collection and reduction technique. Hum. Mov. Sci. 1991, 10, 575–587. [Google Scholar] [CrossRef]
- Yang, F.; Pai, Y.-C. Automatic recognition of falls in gait-slip training: Harness load cell based criteria. J. Biomech. 2011, 44, 2243–2249. [Google Scholar] [CrossRef]
- Patel, P.; Bhatt, T. Adaptation to large-magnitude treadmill-based perturbations: Improvements in reactive balance response. Physiol. Rep. 2015, 3, e12247. [Google Scholar] [CrossRef] [PubMed]
- Hof, A.; Gazendam, M.; Sinke, W. The condition for dynamic stability. J. Biomech. 2005, 38, 1–8. [Google Scholar] [CrossRef]
- Pai, Y.-C.; Patton, J. Center of mass velocity-position predictions for balance control. J. Biomech. 1997, 30, 347–354. [Google Scholar] [CrossRef]
- Pai, Y.-C.; Iqbal, K. Simulated movement termination for balance recovery: Can movement strategies be sought to maintain stability in the presence of slipping or forced sliding? J. Biomech. 1999, 32, 779–786. [Google Scholar] [CrossRef]
- Yang, F.; Anderson, F.C.; Pai, Y.-C. Predicted threshold against backward balance loss in gait. J. Biomech. 2007, 40, 804–811. [Google Scholar] [CrossRef]
- Pai, Y.-C. Movement Termination and Stability in Standing. Exerc. Sport Sci. Rev. 2003, 31, 19–25. [Google Scholar] [CrossRef]
- Ishige, S.; Wakui, S.; Miyazawa, Y.; Naito, H. Reliability and validity of the Activities-specific Balance Confidence scale-Japanese (ABC-J) in community-dwelling stroke survivors. Phys. Ther. Res. 2020, 23, 15–22. [Google Scholar] [CrossRef]
- Botner, E.M.; Miller, W.C.; Eng, J.J. Measurement properties of the Activities-specific Balance Confidence Scale among individuals with stroke. Disabil. Rehabil. 2005, 27, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Salbach, N.M.; Mayo, N.E.; Hanley, J.A.; Richards, C.L.; Wood-Dauphinee, S. Psychometric Evaluation of the Original and Canadian French Version of the Activities-Specific Balance Confidence Scale Among People With Stroke. Arch. Phys. Med. Rehabil. 2006, 87, 1597–1604. [Google Scholar] [CrossRef]
- Tsang, C.S.; Liao, L.-R.; Chung, R.C.; Pang, M.Y. Psychometric Properties of the Mini-Balance Evaluation Systems Test (Mini-BESTest) in Community-Dwelling Individuals with Chronic Stroke. Phys. Ther. 2013, 93, 1102–1115. [Google Scholar] [CrossRef] [PubMed]
- Lampropoulou, S.I.; Billis, E.; Gedikoglou, I.A.; Michailidou, C.; Nowicky, A.V.; Skrinou, D.; Michailidi, F.; Chandrinou, D.; Meligkoni, M. Reliability, validity and minimal detectable change of the Mini-BESTest in Greek participants with chronic stroke. Physiother. Theory Pract. 2019, 35, 171–182. [Google Scholar] [CrossRef]
- Alghadir, A.H.; Al-Eisa, E.S.; Anwer, S.; Sarkar, B. Reliability, validity, and responsiveness of three scales for measuring balance in patients with chronic stroke. BMC Neurol. 2018, 18, 141. [Google Scholar] [CrossRef]
- Moore, J.; Raad, J. Measurement Characteristics and Clinical Utility of the Berg Balance Scale Among Individuals with Stroke. Arch. Phys. Med. Rehabil. 2013, 94, 217–218. [Google Scholar] [CrossRef]
- Patel, P.J.; Bhatt, T. Does aging with a cortical lesion increase fall-risk: Examining effect of age versus stroke on intensity modulation of reactive balance responses from slip-like perturbations. Neuroscience 2016, 333, 252–263. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.D.; Schmidt, R. Motor Control and Learning; Human kinetics: Champaign, IL, USA, 2005. [Google Scholar]
- Wolpert, D.; Kawato, M. Multiple paired forward and inverse models for motor control. Neural Netw. 1998, 11, 1317–1329. [Google Scholar] [CrossRef]
- Mihara, M.; Miyai, I.; Hattori, N.; Hatakenaka, M.; Yagura, H.; Kawano, T.; Kubota, K. Cortical control of postural balance in patients with hemiplegic stroke. Neuro Rep. 2012, 23, 314–319. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, J.V.; Horak, F.B. Cortical control of postural responses. J. Neural Transm. 2007, 114, 1339–1348. [Google Scholar] [CrossRef]
- Varghese, J.P.; McIlroy, R.E.; Barnett-Cowan, M. Perturbation-evoked potentials: Significance and application in balance control research. Neurosci. Biobehav. Rev. 2017, 83, 267–280. [Google Scholar] [CrossRef]
- Peterson, S.M.; Ferris, D.P. Differentiation in Theta and Beta Electrocortical Activity between Visual and Physical Perturbations to Walking and Standing Balance. Eneuro 2018, 5, 5. [Google Scholar] [CrossRef]
- Bhatt, T.; Wening, J.D.; Pai, Y.-C. Adaptive control of gait stability in reducing slip-related backward loss of balance. Exp. Brain Res. 2005, 170, 61–73. [Google Scholar] [CrossRef]
- Cham, R.; Redfern, M.S. Changes in gait when anticipating slippery floors. Gait Posture 2002, 15, 159–171. [Google Scholar] [CrossRef]
- Lockhart, T.E.; Woldstad, J.C.; Smith, J.L. Effects of age-related gait changes on the biomechanics of slips and falls. Ergonomics 2003, 46, 1136–1160. [Google Scholar] [CrossRef]
- Marigold, D.S.; Patla, A.E. Strategies for Dynamic Stability during Locomotion on a Slippery Surface: Effects of Prior Experience and Knowledge. J. Neurophysiol. 2002, 88, 339–353. [Google Scholar] [CrossRef] [PubMed]
- Bhushan, N.; Shadmehr, R. Computational nature of human adaptive control during learning of reaching movements in force fields. Biol. Cybern. 1999, 81, 39–60. [Google Scholar] [CrossRef] [PubMed]
- Kawato, M.; Gomi, H. A computational model of four regions of the cerebellum based on feedback-error learning. Biol. Cybern. 1992, 68, 95–103. [Google Scholar] [CrossRef] [PubMed]

| Variable | n = 11 |
|---|---|
| Age (years) | 63.27 ± 8.2 |
| Height (meters) | 1.71 ± 0.08 |
| Weight (kilograms) | 83.62 ± 9.54 |
| Gender (Male/Female) | 9/2 |
| Chronicity of stroke (years) | 6.82 ± 6.49 |
| Impairment level | |
| CMSA (Leg) | 4.91 ± 0.79 |
| CMSA (Foot) | 3.64 ± 1.37 |
| AFO/No AFO | 7/4 |
| Stroke type (Hemorrhagic/Ischemic) | 3/6 * |
| Balance (BBS) | 49.18 ± 3.59 |
| Gait speed (10 m test)(m/s) | 0.76 ± 0.24 |
| 6 min walk test (meters) | 283 ± 83.76 |
| Repeated Measures ANOVA Results | |||
|---|---|---|---|
| Main Effect of Trial | Effect of Intensity | Trial × Intensity Interaction | |
| Pre-slip CoM stability at Touch down (TD) | F(1, 59) = 11.84, p < 0.001 * | F (1, 59) = 0.55, p = 0.73 | F(1, 59) = 0.40, p = 0.84 |
| Post-slip CoM stability at Lift-off (LO) | F(1, 59) = 16.83, p < 0.001 * | F(1, 59) = 5.4, p < 0.001 * | F(1, 59) = 0.85, p = 0.51 |
| Post-slip minimum stability | F(1, 58) = 12.15, p < 0.001 * | F (1, 58) = 15.23, p < 0.001 * | F(1, 58) = 0.42, p = 0.83 |
| Pre-Training vs. Post-Training Results at Each Intensity | |||
|---|---|---|---|
| Intensity | Pre-Slip CoM Stability at TD | Post-Slip CoM Stability at LO | Post-Slip Minimum Stability |
| Level 1 | p = 0.15, 95% CI = −0.12, 0.02 | p = 0.78, 95% CI = −0.17, 0.13 | p = 0.15, 95% CI = −0.24, 0.06 |
| Level 2 | p = 0.06, 95% CI = −0.09, −0.001 | p = 0.03, 95% CI = −0.19, −0.008 * | p = 0.22, 95% CI = −0.17, 0.04 |
| Level 3 | p = 0.42, 95% CI = −0.14, 0.06 | p = 0.03, 95% CI = −0.36, −0.01 * | p = 0.13, 95% CI = −0.31, 0.04 |
| Level 4 | p = 0.43, 95% CI = −0.07, 0.03 | p = 0.16, 95% CI = −0.23, 0.04 | p = 0.75, 95% CI = −0.2, 0.15 |
| Level 5 | p = 0.27, 95% CI = −0.14, 0.04 | p = 0.05, 95% CI = −0.44, 0.01 * | p = 0.05, 95% CI = −0.22, 0.004 * |
| Level 6 | p = 0.03, 95% CI = −0.16, −0.007 * | p = 0.12, 95% CI = −0.42, 0.06 | p = 0.03, 95% CI = −0.27, −0.01 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dusane, S.; Bhatt, T. Effect of Multisession Progressive Gait-Slip Training on Fall-Resisting Skills of People with Chronic Stroke: Examining Motor Adaptation in Reactive Stability. Brain Sci. 2021, 11, 894. https://doi.org/10.3390/brainsci11070894
Dusane S, Bhatt T. Effect of Multisession Progressive Gait-Slip Training on Fall-Resisting Skills of People with Chronic Stroke: Examining Motor Adaptation in Reactive Stability. Brain Sciences. 2021; 11(7):894. https://doi.org/10.3390/brainsci11070894
Chicago/Turabian StyleDusane, Shamali, and Tanvi Bhatt. 2021. "Effect of Multisession Progressive Gait-Slip Training on Fall-Resisting Skills of People with Chronic Stroke: Examining Motor Adaptation in Reactive Stability" Brain Sciences 11, no. 7: 894. https://doi.org/10.3390/brainsci11070894
APA StyleDusane, S., & Bhatt, T. (2021). Effect of Multisession Progressive Gait-Slip Training on Fall-Resisting Skills of People with Chronic Stroke: Examining Motor Adaptation in Reactive Stability. Brain Sciences, 11(7), 894. https://doi.org/10.3390/brainsci11070894





