The Effect of Acceptance and Commitment Therapy for Improving Psychological Well-Being in Parents of Individuals with Autism Spectrum Disorders: A Randomized Controlled Trial
Abstract
:1. Introduction
1.1. PT Approach
1.2. Acceptance and Commitment Therapy Model
2. Materials and Methods
2.1. Inclusion Criteria
2.2. Ethics
2.3. Study Design
2.4. Intervention
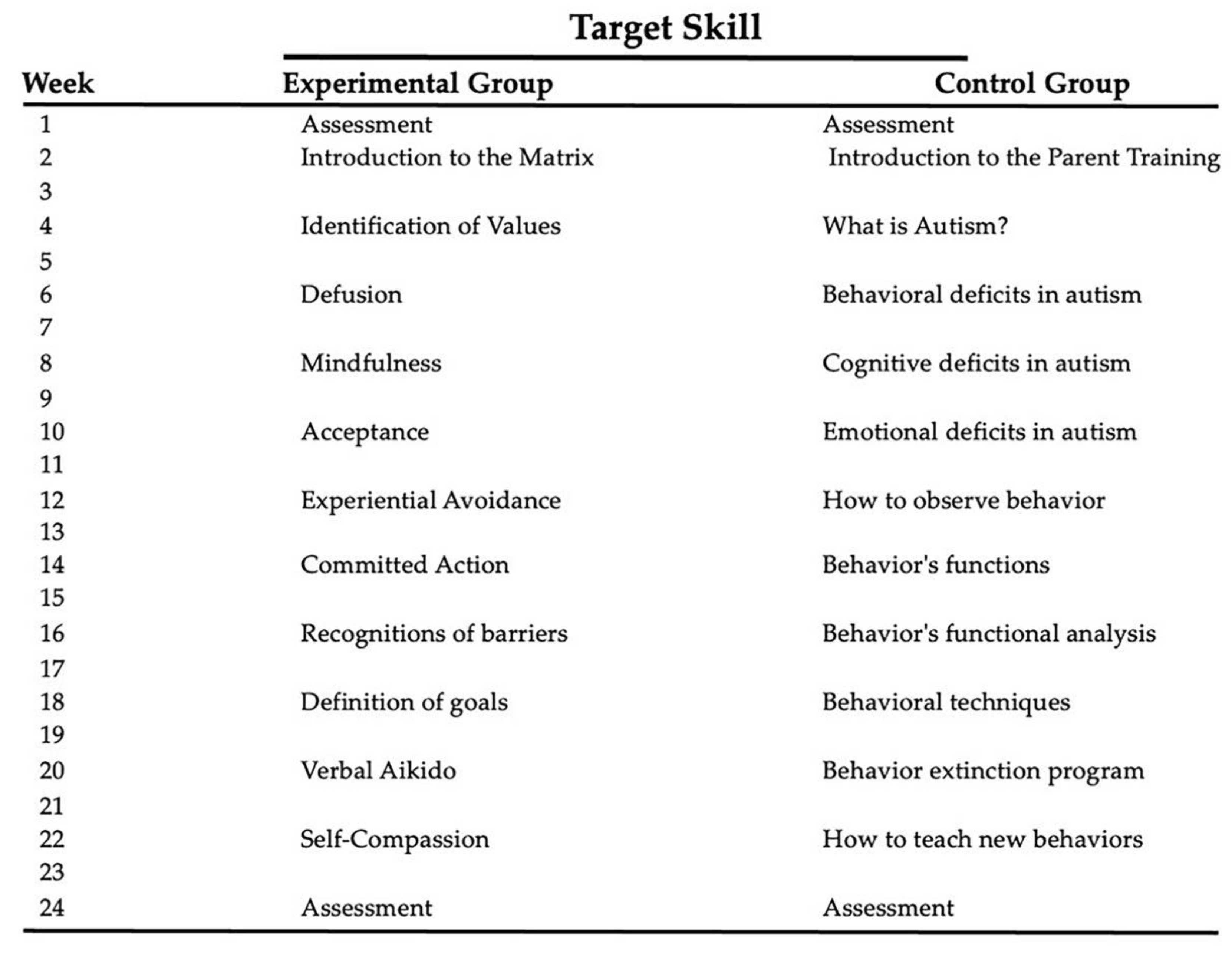
2.5. ACT Matrix
2.6. PT
2.7. Outcome Measures
2.8. Primary Outcome Measures
2.8.1. Acceptance and Action Questionnaire (AAQ-II)
2.8.2. Home Situation Questionnaire (HSQ-ASD)
2.9. Secondary Outcome Measures
2.9.1. Valued Living Questionnaire (VLQ)
2.9.2. Mindful Attention Awareness Scale (MAAS)
2.9.3. Parental Stress Index/Short Form (PSI/SF)
2.10. Statistical Analysis
3. Results
3.1. Clinical Enrollment
3.2. ACT Versus PT Treatments
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Campbell, S.B.; Spieker, S.; Burchinal, M.; Poe, M.D.; The NICHD Early Child Care Research Network. Trajectories of aggression from toddlerhood to age 9 predict academic and social functioning through age 12. J. Child Psychol. Psychiatry 2006, 47, 791–800. [Google Scholar] [CrossRef] [PubMed]
- Merikangas, K.R.; He, J.P.; Burstein, M.; Swanson, S.A.; Avenevoli, S.; Cui, L.; Benjet, C.; Georgiades, K.; Swendsen, J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the national comorbidity survey replication—adolescent supplement (NCS-A). J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 980–989. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eikeseth, S.; Klintwall, L.; Hayward, D.; Gale, C. Stress in parents of children with autism participating in early and intensive behavioral intervention. Eur. J. Behav. Anal. 2015, 16, 112–120. [Google Scholar] [CrossRef]
- Estes, A.; Munson, J.; Dawson, G.; Koehler, E.; Zhou, X.H.; Abbott, R. Parenting stress and psychological functioning among mothers of preschool children with autism and developmental delay. Autism 2009, 13, 375–387. [Google Scholar] [CrossRef]
- Grindle, C.F.; Kovshoff, H.; Hastings, R.P.; Remington, B. Parents’ experiences of home-based applied behavior analysis programs for young children with autism. J. Autism Dev. Disord. 2009, 39, 42–56. [Google Scholar] [CrossRef] [PubMed]
- Hayes, S.A.; Watson, S.L. The impact of parenting stress: A meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. J. Autism Dev. Disord. 2013, 43, 629–642. [Google Scholar] [CrossRef]
- Abbeduto, L.; Seltzer, M.M.; Shattuck, P.; Krauss, M.W.; Orsmond, G.; Murphy, M.M. Psychological Well-Being and Coping in Mothers of Youths with Autism, Down Syndrome, or Fragile X Syndrome. Am. J. Ment. Retard. 2004, 109, 237–254. [Google Scholar] [CrossRef] [Green Version]
- Kogan, M.D.; Strickland, B.B.; Blumberg, S.J.; Singh, G.K.; Perrin, J.M.; Van Dyck, P.C. A national profile of the health care experiences and family impact of autism spectrum disorder among children in the United States, 2005–2006. Pediatrics 2008, 122, e1149–e1158. [Google Scholar] [CrossRef] [PubMed]
- Rao, P.A.; Beidel, D.C. The impact of children with high-functioning autism on parental stress, sibling adjustment, and family functioning. Behav Modif. 2009, 33, 437–451. [Google Scholar] [CrossRef]
- Dabrowska, A.; Pisula, E. Parenting stress and coping styles in mothers and fathers of pre-school children with autism and Down syndrome. J. Intellect. Disabil. Res. 2010, 54, 266–280. [Google Scholar] [CrossRef]
- Dumas, J.E.; Wolf, L.C.; Fisman, S.N.; Culligan, A. Parenting Stress, Child Behavior Problems, and Dysphoria in Parents of Children with Autism, Down Syndrome, Behavior Disorders, and Normal Development. Exceptionality 1991, 2, 97–110. [Google Scholar] [CrossRef]
- Brobst, J.B.; Clopton, J.R.; Hendrick, S.S. Parenting children with autism spectrum disorders: The couple’s relationship. Focus Autism Other Dev. Disabil. 2009, 24, 38–49. [Google Scholar] [CrossRef]
- Hartley, S.L.; Barker, E.T.; Seltzer, M.M.; Floyd, F.; Greenberg, J.; Orsmond, G.; Bolt, D. The relative risk and timing of divorce in families of children with an autism spectrum disorder. J. Fam. Psychol. 2010, 24, 449–457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Folkman, S.; Moskowitz, J.T. Coping: Pitfalls and promise. Annu. Rev. Psychol. 2004, 55, 745–774. [Google Scholar] [CrossRef]
- Singh, N.N.; Lancioni, G.E.; Winton, A.S.W.; Fisher, B.C.; Wahler, R.G.; McAleavey, K.; Singh, J.; Sabaawi, M. Mindful parenting decreases aggression, noncompliance, and self-injury in children with autism. J. Emot. Behav. Disord. 2006, 14, 169–177. [Google Scholar] [CrossRef]
- Singh, N.N.; Lancioni, G.E.; Winton, A.S.W.; Karazsia, B.T.; Myers, R.E.; Latham, L.L.; Singh, J. Mindfulness-Based Positive Behavior Support (MBPBS) for Mothers of Adolescents with Autism Spectrum Disorder: Effects on Adolescents’ Behavior and Parental Stress. Mindfulness 2014, 5, 646–657. [Google Scholar] [CrossRef]
- Bearss, K.; Johnson, C.; Smith, T.; Lecavalier, L.; Swiezy, N.; Aman, M.; McAdam, D.B.; Butter, E.; Stillitano, C.; Minshawi, N.; et al. Effect of parent training vs parent education on behavioral problems in children with autism spectrum disorder: A randomized clinical trial. JAMA J. Am. Med. Assoc. 2015, 313, 1524–1533. [Google Scholar] [CrossRef]
- Lecciso, F.; Petrocchi, S.; Savazzi, F.; Marchetti, A.; Nobile, M.; Molteni, M. The association between maternal resolution of the diagnosis of autism, maternal mental representations of the relationship with the child, and children’s attachment. Life Span Disabil 2013, 16, 21–38. [Google Scholar]
- Russell, G.; Norwich, B. Dilemmas, diagnosis and de-stigmatization: Parental perspectives on the diagnosis of autism spectrum disorders. Clin. Child Psychol. Psychiatry 2012, 17, 229–245. [Google Scholar] [CrossRef]
- Hayes, S.C.; Strosahl, K.D.; Wilson, K.G. Acceptance and Commitment Therapy: An Experiential Approach to Behavior Change; The Guilford Press: New York, NY, USA, 2003; ISBN 1572309555. [Google Scholar]
- Blackledge, J.T.; Drake, C.E. Acceptance and Commitment Therapy: Empirical and Theoretical Considerations; New Harbinger Publications, Inc.: Oakland, CA, USA, 2013. [Google Scholar]
- Bond, F.W.; Bunce, D. Mediators of change in emotion-focused and problem-focused worksite stress management interventions. J. Occup. Health Psychol. 2000, 5, 156–163. [Google Scholar] [CrossRef]
- Twohig, M.P.; Woods, D.W. A preliminary investigation of acceptance and commitment therapy and habit reversal as a treatment for trichotillomania. Behav. Ther. 2004, 35, 803–820. [Google Scholar] [CrossRef]
- Dahl, J.; Wilson, K.G.; Nilsson, A. Acceptance and commitment therapy and the treatment of persons at risk for long-term disability resulting from stress and pain symptoms: A preliminary randomized trial. Behav. Ther. 2004, 35, 785–801. [Google Scholar] [CrossRef] [Green Version]
- Gifford, E.V.; Kohlenberg, B.S.; Hayes, S.C.; Antonuccio, D.O.; Piasecki, M.M.; Rasmussen-Hall, M.L.; Palm, K.M. Acceptance-based treatment for smoking cessation. Behav. Ther. 2004, 35, 689–705. [Google Scholar] [CrossRef]
- Hayes, S.C.; Wilson, K.G.; Gifford, E.V.; Bissett, R.; Piasecki, M.; Batten, S.V.; Byrd, M.; Gregg, J. A preliminary trial of twelve-step facilitation and acceptance and commitment therapy with polysubstance-abusing methadone-maintained opiate addicts. Behav. Ther. 2004, 35, 667–688. [Google Scholar] [CrossRef] [Green Version]
- Zettle, R.D.; Hayes, S.C. Dysfunctional control by client verbal behavior: The context of reason-giving. Anal. Verbal Behav. 1986, 4, 30–38. [Google Scholar] [CrossRef]
- Zettle, R.D.; Rains, J.C. Group cognitive and contextual therapies in treatment of depression. J. Clin. Psychol. 1989, 45, 436–445. [Google Scholar] [CrossRef]
- Vanzin, L.; Mauri, V.; Valli, A.; Pozzi, M.; Presti, G.; Oppo, A.; Ristallo, A.; Molteni, M.; Nobile, M. Clinical Effects of an ACT-Group Training in Children and Adolescents with Attention-Deficit/Hyperactivity Disorder. J. Child Fam. Stud. 2020, 29, 1070–1080. [Google Scholar] [CrossRef] [Green Version]
- Zemestani, M.; Mozaffari, S. Acceptance and commitment therapy for the treatment of depression in persons with physical disability: A randomized controlled trial. Clin. Rehabil. 2020, 34, 938–947. [Google Scholar] [CrossRef]
- Ingersoll, B.; Wainer, A. Initial efficacy of project ImPACT: A parent-mediated social communication intervention for young children with ASD. J. Autism Dev. Disord. 2013, 43, 2943–2952. [Google Scholar] [CrossRef]
- Plant, K.M.; Sanders, M.R. Predictors of care-giver stress in families of preschool-aged children with developmental disabilities. J. Intellect. Disabil. Res. 2007, 51, 109–124. [Google Scholar] [CrossRef] [Green Version]
- Stahmer, A.C.; Gist, K. The Effects of an Accelerated Parent Education Program on Technique Mastery and Child Outcome. J. Posit. Behav. Interv. 2001, 3, 75–82. [Google Scholar] [CrossRef]
- Steiner, A.M.; Koegel, L.K.; Koegel, R.L.; Ence, W.A. Issues and theoretical constructs regarding parent education for autism spectrum disorders. J. Autism Dev. Disord. 2012, 42, 1218–1227. [Google Scholar] [CrossRef] [Green Version]
- Polk, K.L.; Schoendorff, B.; Webster, M.; Olaz, F.O. The Essential Guide to the ACT Matrix: A Step-by-Step Approach to Using the ACT Matrix Model in Clinical Practice; Star, J., Ed.; Context Press: Reno, NV, USA, 2016; ISBN 5856420187. [Google Scholar]
- Pearl, E.S. Parent management training for reducing oppositional and aggressive behavior in preschoolers. Aggress. Violent Behav. 2009, 14, 295–305. [Google Scholar] [CrossRef]
- Postorino, V.; Sharp, W.G.; McCracken, C.E.; Bearss, K.; Burrell, T.L.; Evans, A.N.; Scahill, L. A Systematic Review and Meta-analysis of Parent Training for Disruptive Behavior in Children with Autism Spectrum Disorder. Clin. Child Fam. Psychol. Rev. 2017, 20, 391–402. [Google Scholar] [CrossRef] [PubMed]
- Scahill, L.; Bearss, K.; Lecavalier, L.; Smith, T.; Swiezy, N.; Aman, M.G.; Sukhodolsky, D.G.; McCracken, C.; Minshawi, N.; Turner, K.; et al. Effect of Parent Training on Adaptive Behavior in Children With Autism Spectrum Disorder and Disruptive Behavior: Results of a Randomized Trial. J. Am. Acad. Child Adolesc. Psychiatry 2016, 55, 602–609. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hastings, R.P.; Johnson, E. Stress in UK families conducting intensive home-based behavioral intervention for their young child with autism. J Autism Dev Disord. 2001, 31, 327–336. [Google Scholar] [CrossRef] [PubMed]
- Bond, F.W.; Hayes, S.C.; Baer, R.A.; Carpenter, K.M.; Guenole, N.; Orcutt, H.K.; Waltz, T.; Zettle, R.D. Preliminary Psychometric Properties of the Acceptance and Action Questionnaire-II: A Revised Measure of Psychological Inflexibility and Experiential Avoidance. Behav. Ther. 2011, 42, 676–688. [Google Scholar] [CrossRef] [Green Version]
- Chowdhury, M.; Aman, M.G.; Lecavalier, L.; Smith, T.; Johnson, C.; Swiezy, N.; McCracken, J.T.; King, B.; McDougle, C.J.; Bearss, K.; et al. Factor structure and psychometric properties of the revised home situations questionnaire for autism spectrum disorder: The home situations questionnaire-autism spectrum disorder. Autism 2016, 20, 528–537. [Google Scholar] [CrossRef] [Green Version]
- Wilson, K.G.; Sandoz, E.K.; Kitchens, J.; Roberts, M. The Valued Living Questionnaire: Defining and Measuring Valued Action. Psychol. Rec. 2010, 60, 249–272. [Google Scholar] [CrossRef] [Green Version]
- Brown, K.W.; Ryan, R.M. The Benefits of Being Present: Mindfulness and Its Role in Psychological Well-Being. J. Pers. Soc. Psychol. 2003, 84, 822–848. [Google Scholar] [CrossRef] [Green Version]
- Abidin, R.R. Parenting Stress Index; Psychological Assessment Resources, Inc.: Odessa, FL, USA, 1995. [Google Scholar]
- Blackledge, J.T.; Hayes, S.C. Using acceptance and commitment training in the support of parents of children diagnosed with autism. Child Fam. Behav. Ther. 2006, 28, 1–18. [Google Scholar] [CrossRef]
- Kowalkowski, J.D. The Impact of a Group-Based Acceptance and Commitment Therapy Intervention on Parents of Children Diagnosed with an Autism Spectrum Disorder. Master’s Theses and Doctoral Dissertations. 512. 2013. Available online: https://commons.emich.edu/theses/512 (accessed on 29 June 2021).
- Pottie, C.G.; Ingram, K.M. Daily Stress, Coping, and Well-Being in Parents of Children with Autism: A Multilevel Modeling Approach. J. Fam. Psychol. 2008, 22, 855–864. [Google Scholar] [CrossRef] [PubMed]
- Rezendes, D.L.; Scarpa, A. Associations between Parental Anxiety/Depression and Child Behavior Problems Related to Autism Spectrum Disorders: The Roles of Parenting Stress and Parenting Self-Efficacy. Autism Res. Treat. 2011, 2011, 395190. [Google Scholar] [CrossRef] [Green Version]
- Boström, P.K.; Broberg, M.; Bodin, L. Child’s positive and negative impacts on parents—A person-oriented approach to understanding temperament in preschool children with intellectual disabilities. Res. Dev. Disabil. 2011, 32, 1860–1871. [Google Scholar] [CrossRef] [PubMed]
- Vasilopoulou, E.; Nisbet, J. The quality of life of parents of children with autism spectrum disorder: A systematic review. Res. Autism Spectr. Disord. 2016, 23, 36–49. [Google Scholar] [CrossRef]
- Hastings, R.P.; Kovshoff, H.; Brown, T.; Ward, N.J.; Espinosa, F.D.; Remington, B. Coping strategies in mothers and fathers of preschool and school-age children with autism. Autism 2005, 9, 377–391. [Google Scholar] [CrossRef] [Green Version]
- Lecavalier, L. Behavioral and emotional problems in young people with pervasive developmental disorders: Relative prevalence, effects of subject characteristics, and empirical classification. J. Autism Dev. Disord. 2006, 36, 1101–1114. [Google Scholar] [CrossRef]
- Ferraioli, S.J.; Harris, S.L. Comparative Effects of Mindfulness and Skills-Based Parent Training Programs for Parents of Children with Autism: Feasibility and Preliminary Outcome Data. Mindfulness 2013, 4, 89–101. [Google Scholar] [CrossRef]
- Jones, L.; Totsika, V.; Hastings, R.P.; Petalas, M.A. Gender differences when parenting children with autism spectrum disorders: A multilevel modeling approach. J. Autism Dev. Disord. 2013, 43, 2090–2098. [Google Scholar] [CrossRef]
- Marino, F.; Chilà, P.; Failla, C.; Crimi, I.; Minutoli, R.; Puglisi, A.; Arnao, A.A.; Tartarisco, G.; Ruta, L.; Vagni, D.; et al. Tele-assisted behavioral intervention for families with children with autism spectrum disorders: A randomized control trial. Brain Sci. 2020, 10, 649. [Google Scholar] [CrossRef] [PubMed]


| Variable | Matrix Group (n = 20) | PT Group (n = 20) | Comparison between Groups | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mdn | Full Range | Mean | SD | Mdn | Full Range | U | W | Z | p-Value | |
| Child Age * | 6.90 | 1.66 | 6.50 | 5–10 | 5.80 | 2.39 | 5.00 | 4–10 | 28.0 | 83.0 | −1.69 | 0.105 |
| Child DQ *,$ | 88.6 | 11.6 | 91.0 | 72.4–111 | 86.1 | 10.6 | 85.4 | 70.0–107 | 43.0 | 98.0 | −0.529 | 0.631 |
| Parental Age | 40.6 | 5.34 | 40.5 | 31–49 | 42.0 | 5.71 | 41.0 | 37–58 | 182 | 392 | −0.489 | 0.640 |
| Parental Education $ | 16.0 | 2.99 | 18.0 | 8–18 | 15.8 | 2.55 | 18.0 | 13–18 | 215 | 425 | 0.490 | 0.678 |
| AAQ-II | 34.6 | 5.35 | 34.5 | 20–46 | 36.9 | 3.06 | 36.0 | 33–44 | 257 | 467 | 1.56 | 0.121 |
| HSQ-ASD | 4.12 | 1.50 | 3.80 | 1.4–6.9 | 3.29 | 1.68 | 2.90 | 1.1–6.7 | 129 | 339 | −1.90 | 0.056 |
| VLQ | 84.4 | 7.14 | 87.0 | 69–91 | 83.4 | 7.55 | 85.0 | 64–91 | 181 | 391 | −0.520 | 0.620 |
| MAAS | 42.1 | 4.63 | 41.5 | 35–55 | 40.0 | 3.22 | 39.5 | 35–48 | 139 | 349 | −1.65 | 0.102 |
| PSI/SF | 30.8 | 10.8 | 31.0 | 12–55 | 29.4 | 8.87 | 27.0 | 15–43 | 149 | 359 | −1.38 | 0.174 |
| Matrix Group (n = 20) | Control Group (n = 20) | Intervention Outcome Comparison between Groups | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Post- Pre- Difference | Baseline | Post- Pre- Difference | ||||||||||||||||||
| Test | Factor | Mean | SD | Mdn | Full Range | Mean | SD | Mdn | Full Range | Mean | SD | Mdn | Full Range | Mean | SD | Mdn | Full Range | U | W | Z | p-Value |
| AAQ-II | Total | 34.6 | 5.35 | 34.5 | 20–46 | 22.3 | 4.77 | 21.5 | 16.0–32.0 | 36.9 | 3.06 | 36.0 | 33–44 | .250 | 1.25 | 0.000 | −4.00–2.00 | .000 | 210 | −5.51 | <0.001 * |
| HSQ-ASD | SI | 4.12 | 1.50 | 3.80 | 1.4–6.9 | −1.18 | 1.64 | −0.950 | −4.40–1.90 | 3.29 | 1.68 | 2.90 | 1.1–6.7 | −0.020 | 0.900 | 0.300 | −2.30–1.00 | 302 | 512 | 2.78 | 0.005 * |
| DA | 3.37 | 1.84 | 3.55 | 0.5–7.2 | −1.18 | 1.49 | −0.650 | −4.60–0.50 | 2.42 | 1.68 | 1.55 | 0.5–5.8 | 0.320 | 0.640 | 0.400 | −1.20–1.40 | 345 | 555 | 3.92 | <0.001 * | |
| Total | 3.65 | 1.52 | 3.75 | 0.9–6.3 | −1.16 | 1.41 | −0.700 | −4.50–0.80 | 2.74 | 1.49 | 2.40 | 0.8–5.5 | 0.140 | 0.590 | 0.200 | −1.30–1.00 | 337 | 547 | 3.72 | <0.001 * | |
| VLQ | I | 84.4 | 7.14 | 87.0 | 69–91 | 3.00 | 4.23 | 2.00 | −7.00–14.0 | 83.4 | 7.55 | 85.0 | 64–91 | 0.250 | 5.38 | 0.000 | −8.00–20.0 | 78.5 | 288 | −3.37 | 0.001 * |
| C | 47.8 | 3.68 | 47.5 | 42–55 | 22.1 | 6.27 | 22.5 | 9.00–35.0 | 38.9 | 5.14 | 47.5 | 42–60 | −0.150 | 1.66 | 0.000 | −4.00–3.00 | 0.000 | 210 | −5.51 | <0.001 * | |
| Total | 40.1 | 4.16 | 40.4 | 34–49 | 21.3 | 6.79 | 20.95 | 4.20–38.0 | 41.8 | 3.68 | 42.0 | 35–49 | −0.100 | 1.30 | 0.000 | −2.70–2.70 | 0.000 | 210 | −5.45 | <0.001 * | |
| MAAS | Total | 42.1 | 4.63 | 41.5 | 35–55 | 22.8 | 4.38 | 22.5 | 13.0–31.0 | 40.0 | 3.22 | 39.5 | 35–48 | 0.150 | 1.53 | 0.000 | −4.00–3.00 | 0.000 | 210 | −0.545 | <0.001 * |
| PSI/SF | PD | 30.8 | 10.8 | 31.0 | 12–55 | −2.55 | 9.34 | −4.00 | −20.0–19.0 | 29.4 | 8.87 | 27.0 | 15–43 | 2.30 | 8.26 | 0.000 | −15.0–20.0 | 277 | 487 | 2.08 | 0.038 $ |
| CDI | 29.8 | 7.42 | 28.0 | 16–49 | −4.35 | 5.64 | −3.00 | −15.0–5.00 | 27.8 | 8.10 | 26.5 | 16–44 | −0.600 | 7.82 | −0.500 | −21.0–13.0 | 269 | 479 | 1.88 | 0.063 | |
| DC | 37.5 | 7.94 | 36.0 | 25–53 | 0.000 | 12.5 | −0.500 | −24.0–26.0 | 38.8 | 7.06 | 37.5 | 26–52 | 0.050 | 7.77 | 1.00 | −17.0–12.0 | 213 | 423 | 0.352 | 0.738 | |
| Total | 98.1 | 11.9 | 97.5 | 80–132 | −6.90 | 6.12 | −6.00 | −19.0–3.00 | 92.9 | 11.1 | 90.0 | 77–113 | 1.80 | 7.19 | 1.50 | −10.0–17.0 | 328 | 538 | 3.47 | <0.001 * | |
| Matrix Group (n = 20) | Parent Training Group (n = 20) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Test | Factor | U | W | Z | p-Value | U | W | Z | p-Value |
| AAQ-II | Total | 400 | 610 | 5.42 | <0.001 * | 221 | 431 | 0.577 | 0.583 |
| HSQ-ASD | SI | 124 | 334 | −2.06 | 0.040 | 208 | 418 | 0.217 | 0.841 |
| DA | 122 | 332 | −2.10 | 0.035 | 232 | 442 | 0.881 | 0.383 | |
| Total | 119 | 329 | −2.18 | 0.028 $ | 218 | 428 | 0.488 | 0.640 | |
| VLQ | I | 260 | 470 | 1.64 | 0.102 | 186 | 396 | −0.369 | 0.718 |
| C | 400 | 610 | 5.42 | <0.001 * | 198 | 408 | 0.055 | 0.968 | |
| Total | 398 | 608 | 5.36 | <0.001 * | 199 | 409 | 0.014 | 0.989 | |
| MAAS | Total | 400 | 610 | 5.42 | <0.001 * | 204 | 414 | 0.110 | 0.925 |
| PSI/SF | PD | 173 | 383 | −0.718 | 0.478 | 229 | 439 | 0.787 | 0.445 |
| CDI | 135 | 345 | −1.78 | 0.081 | 198 | 408 | −0.041 | 0.968 | |
| DC | 195 | 405 | −0.136 | 0.904 | 199 | 409 | 0.027 | 0.989 | |
| Total | 126 | 336 | −2.01 | 0.046 $ | 226 | 436 | 0.718 | 0.478 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marino, F.; Failla, C.; Chilà, P.; Minutoli, R.; Puglisi, A.; Arnao, A.A.; Pignolo, L.; Presti, G.; Pergolizzi, F.; Moderato, P.; et al. The Effect of Acceptance and Commitment Therapy for Improving Psychological Well-Being in Parents of Individuals with Autism Spectrum Disorders: A Randomized Controlled Trial. Brain Sci. 2021, 11, 880. https://doi.org/10.3390/brainsci11070880
Marino F, Failla C, Chilà P, Minutoli R, Puglisi A, Arnao AA, Pignolo L, Presti G, Pergolizzi F, Moderato P, et al. The Effect of Acceptance and Commitment Therapy for Improving Psychological Well-Being in Parents of Individuals with Autism Spectrum Disorders: A Randomized Controlled Trial. Brain Sciences. 2021; 11(7):880. https://doi.org/10.3390/brainsci11070880
Chicago/Turabian StyleMarino, Flavia, Chiara Failla, Paola Chilà, Roberta Minutoli, Alfio Puglisi, Antonino A. Arnao, Loris Pignolo, Giovambattista Presti, Francesca Pergolizzi, Paolo Moderato, and et al. 2021. "The Effect of Acceptance and Commitment Therapy for Improving Psychological Well-Being in Parents of Individuals with Autism Spectrum Disorders: A Randomized Controlled Trial" Brain Sciences 11, no. 7: 880. https://doi.org/10.3390/brainsci11070880
APA StyleMarino, F., Failla, C., Chilà, P., Minutoli, R., Puglisi, A., Arnao, A. A., Pignolo, L., Presti, G., Pergolizzi, F., Moderato, P., Tartarisco, G., Ruta, L., Vagni, D., Cerasa, A., & Pioggia, G. (2021). The Effect of Acceptance and Commitment Therapy for Improving Psychological Well-Being in Parents of Individuals with Autism Spectrum Disorders: A Randomized Controlled Trial. Brain Sciences, 11(7), 880. https://doi.org/10.3390/brainsci11070880









