Predictive Value of Cough Frequency in Addition to Aspiration Risk for Increased Risk of Pneumonia in Dysphagic Stroke Survivors: A Clinical Pilot Study
Abstract
1. Introduction
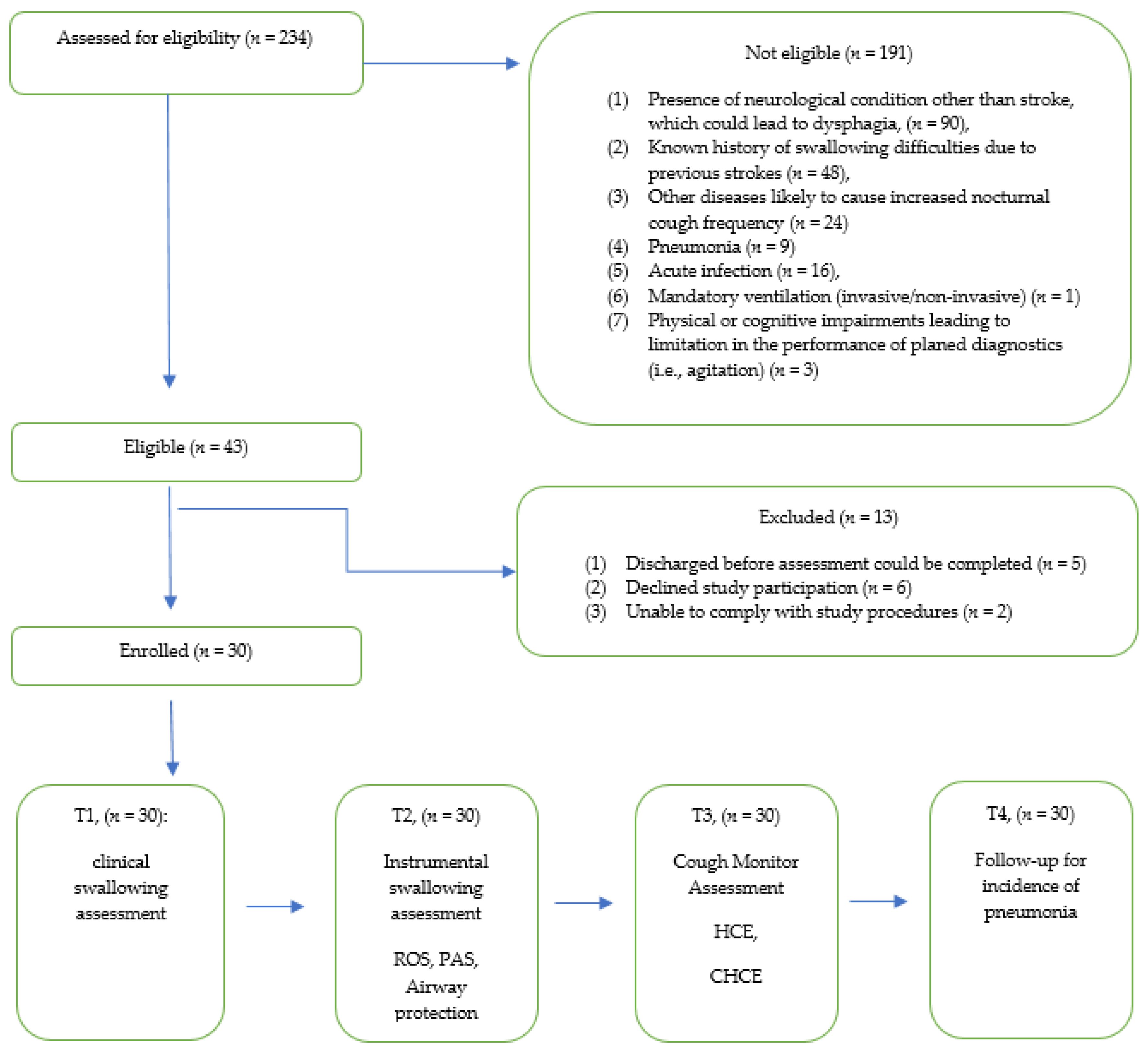
2. Materials and Methods
2.1. Participants
- (1)
- Age between 18–85 years;
- (2)
- First ever stroke (ICD-10-CM Code: Cerebrovascular diseases, I60-I69);
- (3)
- Clinical suspicion of neurogenic swallowing disorder up to 6 weeks post-onset.
- (1)
- The presence of neurological condition other than stroke, which could lead to dysphagia;
- (2)
- Known history of swallowing difficulties due to previous stroke;
- (3)
- Any other diseases correlating with increased risk of coughing during night-time measurement (i.e., COPD, asthma);
- (4)
- Pneumonia;
- (5)
- Acute infection;
- (6)
- Requirement for invasive or non-invasive ventilation;
- (7)
- Physical or cognitive impairments leading to limitation in the performance of planed diagnostics (i.e., agitation);
- (8)
- Discharged before assessments could be completed.
2.2. Procedures
2.2.1. Functional Independence Measurement (FIM)
2.2.2. Dysphagia Screening and Clinical Swallowing Evaluation
2.2.3. Instrumental Diagnostics of Dysphagia
Penetration–Aspiration-Scale (PAS)
- (1)
- PAS I–II: Normal–mild (no aspiration, penetration with clearing);
- (2)
- PAS III–V: Moderate (penetrations);
- (3)
- PAS VI–VIII: Severe (aspirations), with PAS VIII defined as silent aspiration.
Rating of Secretion (ROS)
- (1)
- ROS 0: Normal rating;
- (2)
- ROS 1: Any secretions evident upon entry in the protective structures surrounding the laryngeal vestibule that were bilaterally represented or deeply pooled;
- (3)
- ROS 2: Any secretions that changed from a “1” rating to a “3” rating during the observation period;
- (4)
- ROS 3: Any secretions seen in the area defined as the laryngeal vestibule, where pulmonary secretions were included if they were not cleared by swallowing or coughing by the close of the segment.
Airway Protection
- (1)
- PTBH 1: Breath holding not achieved;
- (2)
- PTBH 2: Transient breath holding with glottis open;
- (3)
- PTBH 3: Sustained breath holding with glottis open;
- (4)
- PTBH 4: Transient true vocal fold closure;
- (5)
- PTBH 5: Sustained true vocal fold closure;
- (6)
- PTBH 6: Transient true and ventricular fold closure;
- (7)
- PTBH 7: Sustained true and ventricular fold closure.
2.2.4. Cough Monitor Assessment
Hourly Cough Rate (HCR)
Categorized Hourly Cough Events (CHCE)
- (1)
- None: 0 average HCRs;
- (2)
- Minor: 1–2 average HCRs;
- (3)
- Moderate: 3–5 average HCRs;
- (4)
- Distinct: 6 or more average HCRs.
2.2.5. Follow-Up for Incidence of Pneumonia
- (1)
- New lung infiltrates on chest imaging;
- (2)
- Respiratory decline;
- (3)
- Fever;
- (4)
- Productive cough.
2.3. Statistical Analysis
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Clinical Trial Registration Information
References
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef] [PubMed]
- Martino, R.; Foley, N.; Bhogal, S.; Diamant, N.; Speechley, M.; Teasell, R. Dysphagia after stroke: Incidence, diagnosis, and pulmonary complications. Stroke 2005, 36, 2756–2763. [Google Scholar] [CrossRef] [PubMed]
- Hinchey, J.A.; Shephard, T.; Furie, K.; Smith, D.; Wang, D.; Tonn, S. Formal Dysphagia Screening Protocols Prevent Pneumonia. Stroke 2005, 36, 1972–1976. [Google Scholar] [CrossRef]
- Gomes, F.; Emery, P.W.; Weekes, C.E. Risk of Malnutrition Is an Independent Predictor of Mortality, Length of Hospital Stay, and Hospitalization Costs in Stroke Patients. J. Stroke Cerebrovasc. Dis. 2016, 25, 799–806. [Google Scholar] [CrossRef] [PubMed]
- Deutsche Gesellschaft für Neurologie. Available online: www.dgn.org/leitlinien (accessed on 8 February 2021).
- McCurtin, A.; Boland, P.; Kavanagh, M.; Lisiecka, D.; Roche, C.; Galvin, R. Do stroke clinical practice guideline recommendations for the intervention of thickened liquids for aspiration support evidence based decision making? A systematic review and narrative synthesis. J. Eval. Clin. Pract. 2020, 26, 1744–1760. [Google Scholar] [CrossRef]
- Smithard, D.G.; Fairfield, C.; Roffe, C.; Enderby, P. European Society for Swallowing Disorders Position Statements and Meeting Abstracts 2012: Dysphagia management in the acute phase of stroke. Dysphagia 2013, 28, 307. [Google Scholar]
- Cichero, J. Respiration and swallowing. In Dysphagia: Foundation, Theory and Practice; Cichero, J., Murdoch, B., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2006; pp. 92–111. [Google Scholar]
- Farneti, D.; Turroni, V.; Genovese, E. Aspiration: Diagnostic contributions from bedside swallowing evaluation and endoscopy. Acta Otorhinolaryngol. Ital. 2018, 38, 511–516. [Google Scholar]
- Virvidaki, I.E.; Nasios, G.; Kosmidou, M.; Giannopoulos, S.; Milionis, H. Swallowing and Aspiration Risk: A Critical Review of Non Instrumental Bedside Screening Tests. J. Clin. Neurol. 2018, 14, 265–274. [Google Scholar] [CrossRef]
- McCullough, G.H.; Rosenbek, J.C.; Wertz, R.T.; McCoy, S.; Mann, G.; McCullough, K. Utility of Clinical Swallowing Examination Measures for Detecting Aspiration Post-Stroke. J. Speech Lang. Hear. Res. 2005, 48, 1280–1293. [Google Scholar] [CrossRef]
- Carnaby-Mann, G.; Lenius, K. The Bedside Examination in Dysphagia. Phys. Med. Rehabil. Clin. N. Am. 2008, 19, 747–768. [Google Scholar] [CrossRef]
- Leder, S.B. A comment on “Modified barium swallow: Clinical and radiographic correlation and relation to feeding recommendations”. Dysphagia 1997, 12, 52–56. [Google Scholar] [PubMed]
- Langmore, S.E. Evaluation of oropharyngeal dysphagia: Which diagnostic tool is superior? Curr. Opin. Otolaryngol. Head Neck Surg. 2003, 11, 485–489. [Google Scholar] [CrossRef]
- Kelly, A.M.; Drinnan, M.; Leslie, P. Assessing Penetration and Aspiration: How Do Videofluoroscopy and Fiberoptic Endoscopic Evaluation of Swallowing Compare? Laryngoscope 2007, 117, 1723–1727. [Google Scholar] [CrossRef] [PubMed]
- Kelly, A.; Leslie, P.; Beale, T.; Payten, C.L.; Drinnan, M. Fibreoptic endoscopic evaluation of swallowing and videofluoroscopy: Does examination type influence perception of pharyngeal residue severity? Clin. Otolaryngol. 2006, 31, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Daniels, S.K.; Brailey, K.; Priestly, D.H.; Herrington, L.R.; Weisberg, L.A.; Foundas, A.L. Aspiration in patients with acute stroke. Arch. Phys. Med. Rehabil. 1998, 79, 14–19. [Google Scholar] [CrossRef]
- Pikus, L.; Levine, M.; Yang, Y.; Rubesin, S.; Katzka, D.; Laufer, I.; Gefter, W.B. Videofluroscopic studies of swallowing dysfunction and the relative risk of pneumonia. Am. J. Roentgenol. 2003, 180, 1613–1616. [Google Scholar] [CrossRef] [PubMed]
- Kulnik, S.T.; Birring, S.S.; Hodsoll, J.; Moxham, J.; Rafferty, G.; Kalra, L. Higher cough flow is associated with lower risk of pneumonia in acute stroke. Thorax 2016, 71, 474–475. [Google Scholar] [CrossRef]
- Cho, P.S.P.; Birring, S.S.; Fletcher, H.V.; Turner, R.D. Methods of Cough Assessment. J. Allergy Clin. Immunol. Pract. 2019, 7, 1715–1723. [Google Scholar] [CrossRef]
- Spinou, A.; Birring, S.S. An update on measurement and monitoring of cough: What are the important study endpoints? J. Thorac. Dis. 2014, 6 (Suppl. S7), S728–S734. [Google Scholar] [CrossRef]
- Hall, J.I.; Lozano, M.; Estrada-Petrocelli, L.; Birring, S.; Turner, R. The present and future of cough counting tools. J. Thorac. Dis. 2020, 12, 5207–5223. [Google Scholar] [CrossRef] [PubMed]
- Irwin, R.S.; Baumann, M.H.; Bolser, D.C.; Boulet, L.-P.; Braman, S.S.; Brightling, C.E.; Brown, K.K.; Canning, B.J.; Chang, A.B.; Dicpinigaitis, P.V.; et al. Diagnosis and Management of Cough Executive Summary. Chest 2006, 129, 1S–23S. [Google Scholar] [CrossRef]
- Hadjikoutis, S.; Eccles, R.; Wiles, C.M. Coughing and choking in motor neuron disease. J. Neurol. Neurosurg. Psychiatry 2000, 68, 601–604. [Google Scholar] [CrossRef][Green Version]
- Kulnik, S.; Birring, S.; Rafferty, G.; Moxham, J.; Kalra, L. P237 Cough frequency in acute stroke. Thorax 2015, 70, A196. [Google Scholar] [CrossRef]
- Koehler, U.; Weissflog, A.; Nikolaizik, W.; Hildebrandt, O.; Scholtes, M.; Sohrabi, K.; Gross, V. Objektives Monitoring von chronischem Husten mit dem ambulanten Lung-Sound-Monitoring-System LEOSound. Pneumologie 2016, 70, 191. [Google Scholar] [CrossRef]
- Linacre, J.M.; Heinemann, A.W.; Wright, B.D.; Granger, C.V.; Hamilton, B.B. The structure and stability of the Functional Independence Measure. Arch. Phys. Med. Rehabil. 1994, 75, 127–132. [Google Scholar] [CrossRef]
- Perry, L.; Love, C.P. Screening for Dysphagia and Aspiration in Acute Stroke: A Systematic Review. Dysphagia 2001, 16, 7–18. [Google Scholar] [CrossRef]
- Suiter, D.M.; Leder, S.B. Clinical Utility of the 3-ounce Water Swallow Test. Dysphagia 2007, 23, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Pekacka-Egli, A.M.; Kazmierski, R.; Lutz, D.; Pekacka-Falkowska, K.; Maszczyk, A.; Windisch, W.; Spielmanns, M. Reassessment of Poststroke Dysphagia in Rehabilitation Facility Results in Reduction in Diet Restrictions. J. Clin. Med. 2021, 10, 1714. [Google Scholar] [CrossRef]
- Langmore, S.E. Endoscopic Evaluation and Treatment of Swallowing Disorders, 2nd ed.; Thieme Medical Publishers: New York, NY, USA, 2001. [Google Scholar]
- Rosenbek, J.C.; Robbins, J.A.; Roecker, E.B.; Coyle, J.L.; Wood, J.L. A penetration-aspiration scale. Dysphagia 1996, 11, 93–98. [Google Scholar] [CrossRef]
- Pluschinski, P.; Zaretsky, Y.; Almahameed, A.; Koseki, J.-C.; Leinung, M.; Girth, L.; Wagenblast, J.; Sader, R.; Stöver, T.; Hey, C. Sekretbeurteilungsskala nach Murray et al. für FEES®: Comparison of reliability and validity of the German long and short version. Nervenarzt 2014, 85, 1582–1587. [Google Scholar] [CrossRef]
- Murray, J. The laryngoscopic evaluation of swallowing or FEES. In Manual of Dysphagia Assessment in Adults; Singular Publishing Company: San Diego, CA, USA, 1999. [Google Scholar]
- Modi, A.R.; Kovacs, C.S. Hospital-acquired and ventilator-associated pneumonia: Diagnosis, management, and prevention. Clevel. Clin. J. Med. 2020, 87, 633–639. [Google Scholar] [CrossRef] [PubMed]
- Kulnik, S.T.; Williams, N.M.; Kalra, L.; Moxham, J.; Birring, S.S. Cough frequency monitors: Can they discriminate patient from environmental coughs? J. Thorac. Dis. 2016, 8, 3152–3159. [Google Scholar] [CrossRef] [PubMed]
- Shim, J.-S.; Song, W.-J.; Morice, A. Drug-Induced Cough. Physiol. Res. 2020, 69 (Suppl. S1), S81–S92. [Google Scholar] [CrossRef] [PubMed]
- Rameau, A.; Young, V.N.; Amin, M.R.; Sulica, L. Flexible Laryngoscopy and COVID-19. Otolaryngol. Neck Surg. 2020, 162, 813–815. [Google Scholar] [CrossRef]
- Bolton, L.; Mills, C.; Wallace, S.; Brady, M.C. Royal College of Speech and Language Therapists (RCSLT) COVID-19 Advisory Group Aerosol generating procedures, dysphagia assessment and COVID-19: A rapid review. Int. J. Lang. Commun. Disord. 2020, 55, 629–636. [Google Scholar] [CrossRef]

| Characteristic | Sample (n = 30) |
|---|---|
| Sex (n, %) | |
| Female | 11 (36.7) |
| Male | 19 (63.3) |
| Age, years (mean, SD) | 70.3 (10.6) |
| Height, cm (mean, SD) | 170.4 (10.6) |
| Weight, kg (mean, SD) | 70.8 (13.2) |
| BMI (mean, SD) | 24.3 (3.7) |
| Stroke etiology (n, %) | |
| Ischemic | 26 (86.7) |
| Hemorrhagic | 4 (13.3) |
| Stroke lesion site (n, %) | |
| Left | 14 (46.7) |
| Right | 13 (43.3) |
| Bilateral | 1 (3.3) |
| Medulla | 2 (6.7) |
| FIM (mean, SD) | |
| Total score | 64.7 (23.7) |
| Cognitive sub-score | 22.8 (10.9) |
| Motor sub-score | 41.9 (17.6) |
| Aphasia (n, %) | 12 (40.0) |
| ACE inhibitors (n, %) | 3 (10.0) |
| Nasogastric tube (n, %) | 5 (16.7) |
| PEG/PEJ tube (n, %) | 7 (23.3) |
| Length of stay, days (median, range) | 38 (5, 86) |
| Pneumonia incidence during rehabilitation stay (n, %) | 10 (33.3) |
| Admission to SSA, days (median, range) | 0 (0, 1) |
| SSA to CSE, days (median, range) | 0 (0, 3) |
| CSE to FEES, days (median, range) | 2 (0, 5) |
| FEES to overnight cough monitor (LEOSound), | |
| days (median, range) | 0 (0, 2) |
| Variables | Sample (n = 30) |
|---|---|
| PAS (n)—(mean, SD) | 6 (2.300) |
| ROS (n)—(mean, SD) | 0 (0.681) |
| PTBH (n)—(mean, SD) | 5 (1.545) |
| HCR (n)—(mean, SD) | 4 (7.718) |
| CHCE (des)—(mean, SD) | 2 (2.355) |
| Pneumonia (bi)—(mean, SD) | 0 (0.479) |
| Variables | Pneumonia (r-Value) |
|---|---|
| PAS | 0.521 |
| ROS | 0.352 |
| PTBH | −0.186 |
| HCR | 0.441 |
| CHCE | 0.428 |
| Variables in Model | Beta | OR | p * | −95% CL | 95% CL |
|---|---|---|---|---|---|
| Constant | −4.916 | 0.007 | 0.011 | 0.000 | 0.332 |
| PAS | 0.687 | 1.987 | 0.014 | 1.146 | 3.445 |
| HCR | 0.239 | 1.270 | 0.041 | 1.011 | 1.595 |
| Variables Outside Model | Beta | OR | p | −95% CL | 95% CL |
|---|---|---|---|---|---|
| ROS | 0.052 | 0.487 | 0.303 | 0.118 | 2.843 |
| PTBH | 0.082 | 0.157 | 0.411 | 0.776 | 2.631 |
| CHCE | 0.105 | 0.740 | 0.102 | 0.457 | 1.133 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pekacka-Egli, A.M.; Kazmierski, R.; Lutz, D.; Kulnik, S.T.; Pekacka-Falkowska, K.; Maszczyk, A.; Windisch, W.; Boeselt, T.; Spielmanns, M. Predictive Value of Cough Frequency in Addition to Aspiration Risk for Increased Risk of Pneumonia in Dysphagic Stroke Survivors: A Clinical Pilot Study. Brain Sci. 2021, 11, 847. https://doi.org/10.3390/brainsci11070847
Pekacka-Egli AM, Kazmierski R, Lutz D, Kulnik ST, Pekacka-Falkowska K, Maszczyk A, Windisch W, Boeselt T, Spielmanns M. Predictive Value of Cough Frequency in Addition to Aspiration Risk for Increased Risk of Pneumonia in Dysphagic Stroke Survivors: A Clinical Pilot Study. Brain Sciences. 2021; 11(7):847. https://doi.org/10.3390/brainsci11070847
Chicago/Turabian StylePekacka-Egli, Anna Maria, Radoslaw Kazmierski, Dietmar Lutz, Stefan Tino Kulnik, Katarzyna Pekacka-Falkowska, Adam Maszczyk, Wolfram Windisch, Tobias Boeselt, and Marc Spielmanns. 2021. "Predictive Value of Cough Frequency in Addition to Aspiration Risk for Increased Risk of Pneumonia in Dysphagic Stroke Survivors: A Clinical Pilot Study" Brain Sciences 11, no. 7: 847. https://doi.org/10.3390/brainsci11070847
APA StylePekacka-Egli, A. M., Kazmierski, R., Lutz, D., Kulnik, S. T., Pekacka-Falkowska, K., Maszczyk, A., Windisch, W., Boeselt, T., & Spielmanns, M. (2021). Predictive Value of Cough Frequency in Addition to Aspiration Risk for Increased Risk of Pneumonia in Dysphagic Stroke Survivors: A Clinical Pilot Study. Brain Sciences, 11(7), 847. https://doi.org/10.3390/brainsci11070847








