Changes in Cortical Activity during Preferred and Fast Speed Walking under Single- and Dual-Tasks in the Young-Old and Old-Old Elderly
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Design and Experimental Protocol
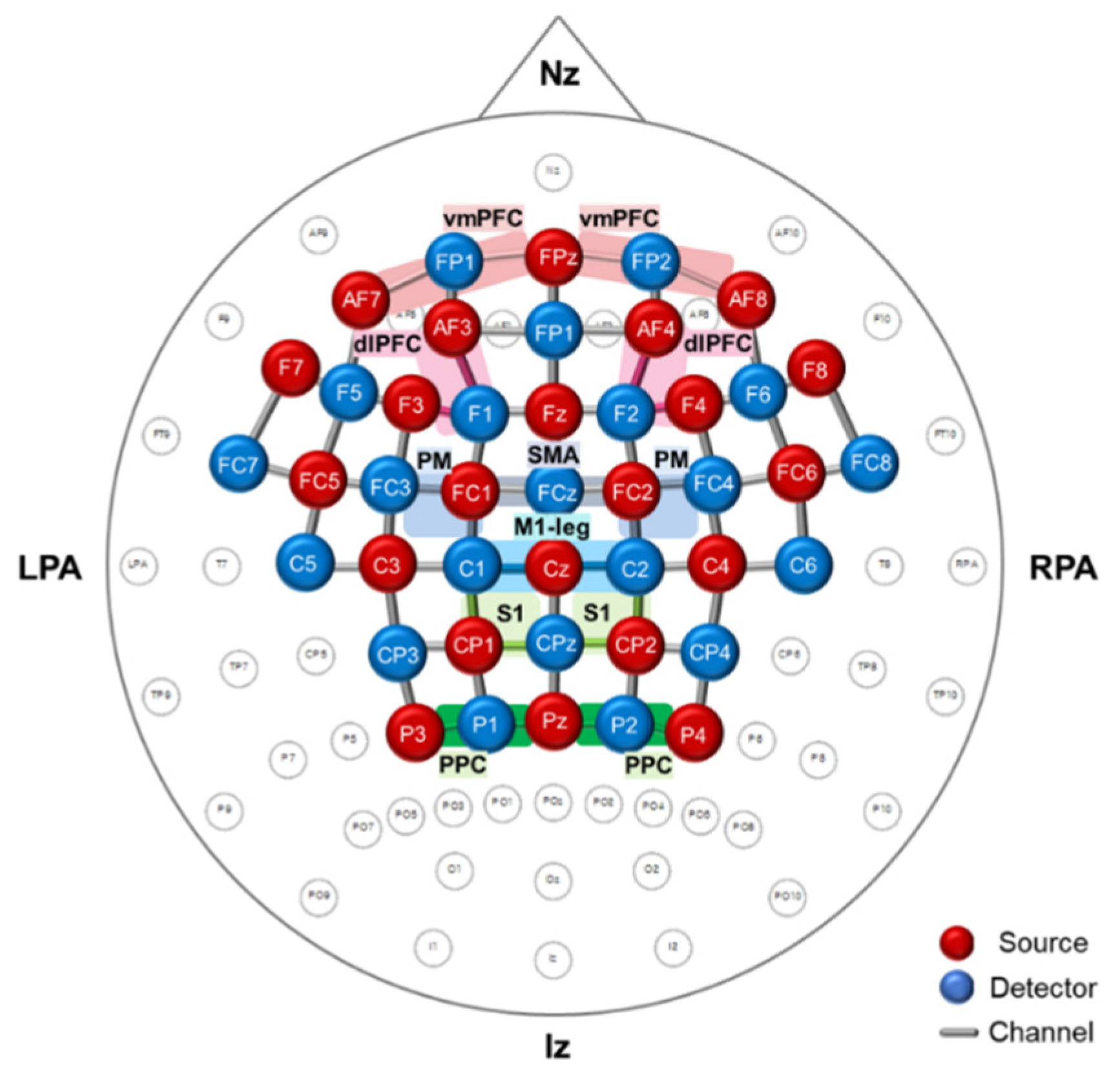
2.3. Measurement of Functional Near-Infrared Spectroscopy
2.4. Data Processing and Analysis of Functional Near-Infrared Spectroscopy
2.5. Statistical Analysis
3. Results
3.1. Characteristics of the Study Population and Functional Differences between the Young-Old and the Old-Old
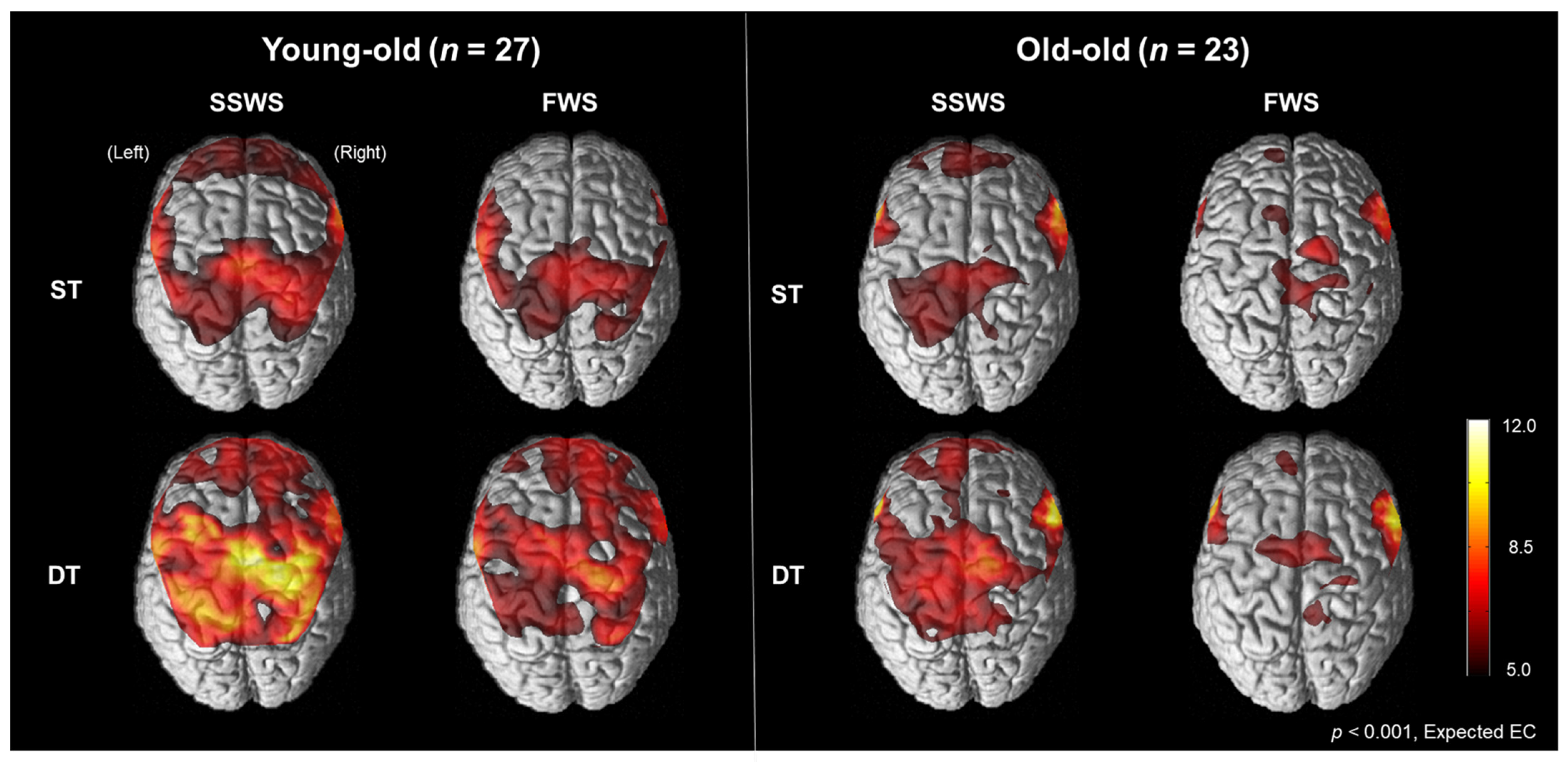
3.2. Cortical Activation Patterns during Walking in the Young-Old and the Old-Old
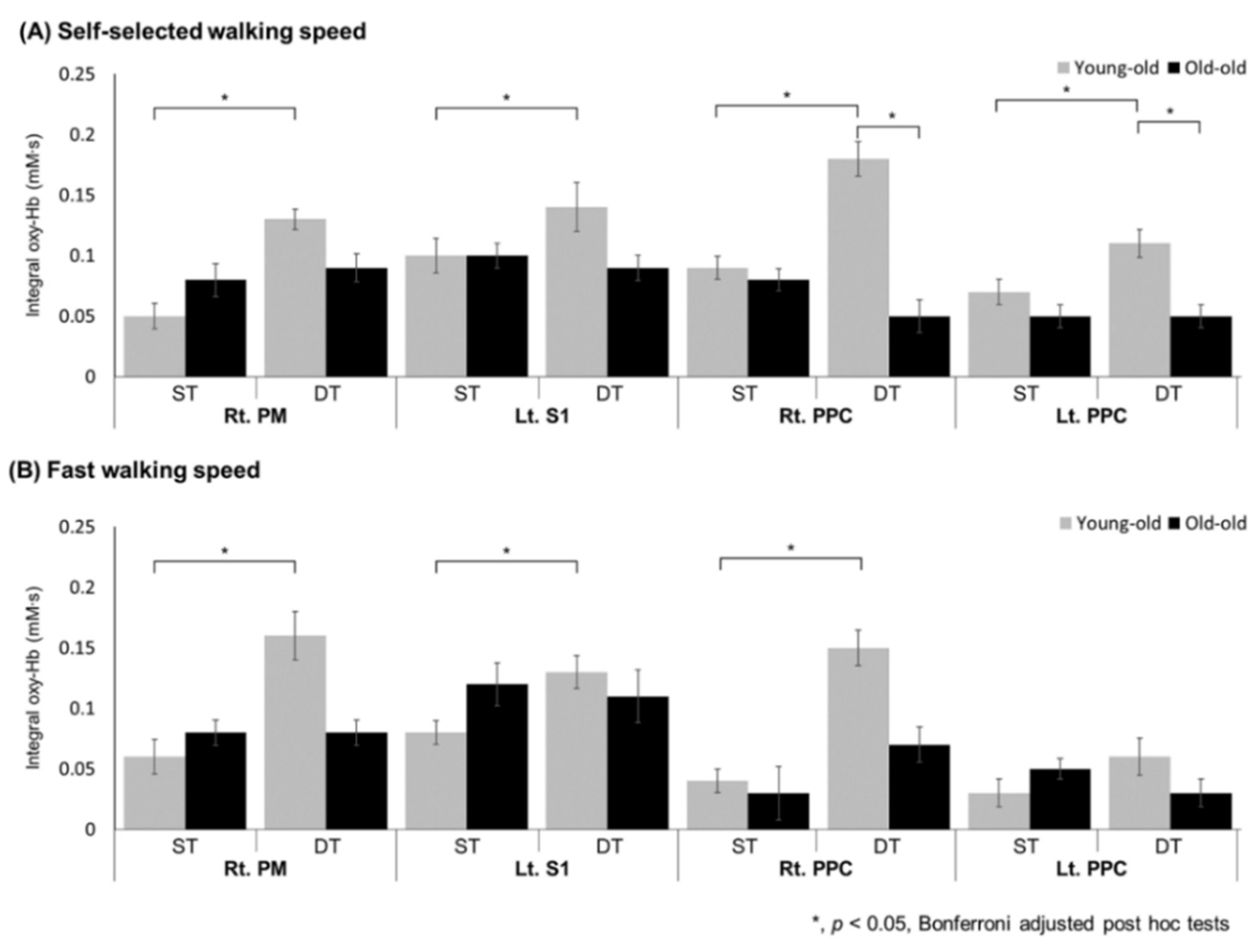
3.3. Regional oxyHb Values during Walking in the Young-Old and the Old-Old
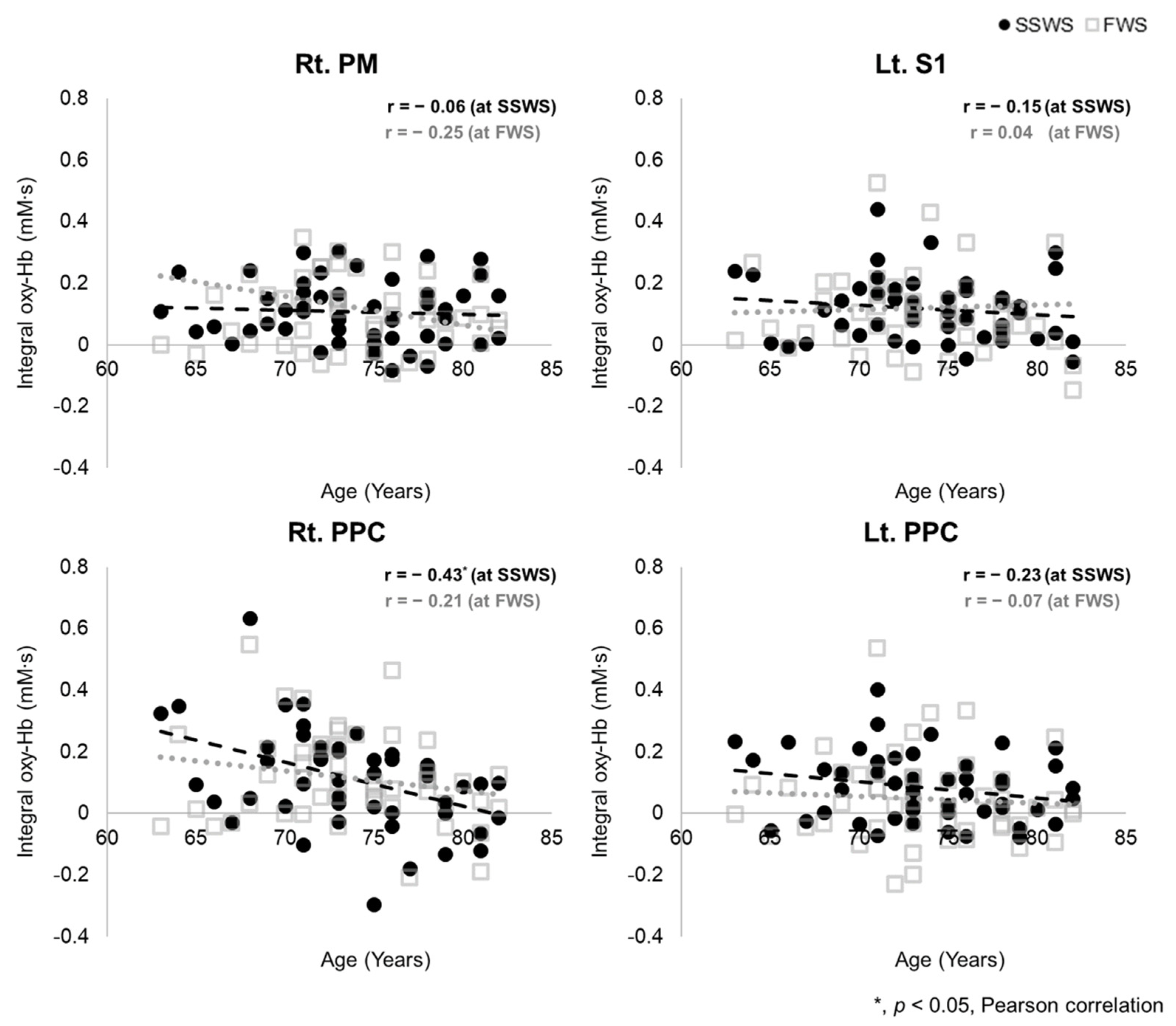
3.4. Association between Age and Regional oxyHb Value during Dual-Task Walking
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shimada, H.; Kim, H.; Yoshida, H.; Suzukawa, M.; Makizako, H.; Yoshida, Y.; Saito, K.; Suzuki, T. Relationship between Age-Associated Changes of Gait and Falls and Life-Space in Elderly People. J. Phys. Ther. Sci. 2010, 22, 419–424. [Google Scholar] [CrossRef] [Green Version]
- Sudarsky, L. Gait Disorders in the Elderly. N. Engl. J. Med. 1990, 322, 1441–1446. [Google Scholar] [PubMed]
- Studenski, S.; Perera, S.; Patel, K.; Rosano, C.; Faulkner, K.; Inzitari, M.; Brach, J.; Chandler, J.; Cawthon, P.; Connor, E.B.; et al. Gait Speed and Survival in Older Adults. JAMA 2011, 305, 50–58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verghese, J.; Ma, A.L.; Hall, C.; Katz, M.J.; Ambrose, A.F.; Lipton, R.B. Epidemiology of Gait Disorders in Community-Residing Older Adults. J. Am. Geriatr. Soc. 2005, 54, 255–261. [Google Scholar] [CrossRef] [Green Version]
- Harada, T.; Miyai, I.; Suzuki, M.; Kubota, K. Gait capacity affects cortical activation patterns related to speed control in the elderly. Exp. Brain Res. 2008, 193, 445–454. [Google Scholar] [CrossRef] [PubMed]
- Mihara, M.; Miyai, I.; Hatakenaka, M.; Kubota, K.; Sakoda, S. Role of the prefrontal cortex in human balance control. NeuroImage 2008, 43, 329–336. [Google Scholar] [CrossRef]
- Wilson, J.; Allcock, L.; Mc Ardle, R.; Taylor, J.-P.; Rochester, L. The neural correlates of discrete gait characteristics in ageing: A structured review. Neurosci. Biobehav. Rev. 2018, 100, 344–369. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.L.; Best, J.R.; Voss, M.W.; Handy, T.C.; Beauchet, O.; Lim, B.C.; Liu-Ambrose, T. Functional Neural Correlates of Slower Gait among Older Adults with Mild Cognitive Impairment. J. Gerontol. Ser. A Boil. Sci. Med Sci. 2018, 74, 513–518. [Google Scholar] [CrossRef]
- Lo, O.-Y.; Halko, M.A.; Zhou, J.; Harrison, R.; Lipsitz, L.A.; Manor, B. Gait Speed and Gait Variability Are Associated with Different Functional Brain Networks. Front. Aging Neurosci. 2017, 9, 390. [Google Scholar] [CrossRef] [Green Version]
- Holtzer, R.; Mahoney, J.R.; Izzetoglu, M.; Wang, C.; England, S.; Verghese, J. Online fronto-cortical control of simple and attention-demanding locomotion in humans. NeuroImage 2015, 112, 152–159. [Google Scholar] [CrossRef] [Green Version]
- Plichta, M.M.; Herrmann, M.J.; Baehne, C.G.; Ehlis, A.C.; Richter, M.M.; Pauli, P.; Fallgatter, A.J. Event-related functional near-infrared spectroscopy (fNIRS): Are the measurements reliable? Neuroimage 2006, 31, 116–124. [Google Scholar] [CrossRef]
- Gramigna, V.; Pellegrino, G.; Cerasa, A.; Cutini, S.; Vasta, R.; Olivadese, G.; Martino, I.; Quattrone, A. Near-Infrared Spectroscopy in Gait Disorders: Is It Time to Begin? Neurorehabil. Neural Repair 2017, 31, 402–412. [Google Scholar] [CrossRef] [Green Version]
- Montero-Odasso, M.; Verghese, J.; Beauchet, O.; Hausdorff, J.M. Gait and Cognition: A Complementary Approach to Understanding Brain Function and the Risk of Falling. J. Am. Geriatr. Soc. 2012, 60, 2127–2136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Yahya, E.; Dawes, H.; Smith, L.; Dennis, A.; Howells, K.; Cockburn, J. Cognitive motor interference while walking: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2010, 35, 715–728. [Google Scholar] [CrossRef] [PubMed]
- Bock, O. Dual-task costs while walking increase in old age for some, but not for other tasks: An experimental study of healthy young and elderly persons. J. Neuroeng. Rehabil. 2008, 5, 27. [Google Scholar] [CrossRef] [Green Version]
- Yogev-Seligmann, G.; Rotem-Galili, Y.; Mirelman, A.; Dickstein, R.; Giladi, N.; Hausdorff, J.M. How Does Explicit Prioritization Alter Walking During Dual-Task Performance? Effects of Age and Sex on Gait Speed and Variability. Phys. Ther. 2010, 90, 177–186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamacher, D.; Herold, F.; Wiegel, P.; Hamacher, D.; Schega, L. Brain activity during walking: A systematic review. Neurosci. Biobehav. Rev. 2015, 57, 310–327. [Google Scholar] [CrossRef]
- Ohsugi, H.; Ohgi, S.; Shigemori, K.; Schneider, E.B. Differences in dual-task performance and prefrontal cortex activation between younger and older adults. BMC Neurosci. 2013, 14, 10. [Google Scholar] [CrossRef] [Green Version]
- Fraser, S.A.; Dupuy, O.; Pouliot, P.; Lesage, F.; Bherer, L. Comparable Cerebral Oxygenation Patterns in Younger and Older Adults during Dual-Task Walking with Increasing Load. Front. Aging Neurosci. 2016, 8, 240. [Google Scholar] [CrossRef]
- Forrest, K.Y.Z.; Zmuda, J.M.; Cauley, J.A. Correlates of Decline in Lower Extremity Performance in Older Women: A 10-Year Follow-Up Study. J. Gerontol. Ser. A Boil. Sci. Med Sci. 2006, 61, 1194–1200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shumway-Cook, A.; Guralnik, J.M.; Ms, C.L.P.; Coppin, A.K.; Ciol, M.; Bandinelli, S.; Ferrucci, L. Age-Associated Declines in Complex Walking Task Performance: The Walking InCHIANTI Toolkit. J. Am. Geriatr. Soc. 2007, 55, 58–65. [Google Scholar] [CrossRef] [Green Version]
- Thaler-Kall, K.; Peters, A.; Thorand, B.; Grill, E.; Autenrieth, C.S.; Horsch, A.; Meisinger, C. Description of spatio-temporal gait parameters in elderly people and their association with history of falls: Results of the population-based cross-sectional KORA-Age study. BMC Geriatr. 2015, 15, 32. [Google Scholar] [CrossRef] [Green Version]
- Magaziner, J. Demographic and epidemiologic considerations for developing preventive strategies in the elderly. Md. Med. J. 1989, 38, 115–120. [Google Scholar]
- Gimmon, Y.; Rashad, H.; Kurz, I.; Plotnik, M.; Riemer, R.; Debi, R.; Shapiro, A.; Melzer, I. Gait Coordination Deteriorates in Independent Old-Old Adults. J. Aging Phys. Act. 2018, 26, 382–389. [Google Scholar] [CrossRef] [PubMed]
- Pothier, K.; Benguigui, N.; Kulpa, R.; Chavoix, C. Multiple Object Tracking While Walking: Similarities and Differences between Young, Young-Old, and Old-Old Adults. J. Gerontol. Ser. B 2014, 70, 840–849. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Na, H.R.; Lee, J.-W.; Lee, S.-H.; Yang, D.W.; Han, I.-W.; Kim, D.H.; Yu, K.-H.; Lee, J.S.; Kim, J.-S.; Kim, S. P3–076: The validity and reliability of the Korean version severe impairment battery. Alzheimer’s Dement. 2006, 2, 70–76. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Simonsick, E.M.; Ferrucci, L.; Glynn, R.J.; Berkman, L.F.; Blazer, D.G.; Scherr, P.A.; Wallace, R.B. A Short Physical Performance Battery Assessing Lower Extremity Function: Association with Self-Reported Disability and Prediction of Mortality and Nursing Home Admission. J. Gerontol. 1994, 49, M85–M94. [Google Scholar] [CrossRef] [PubMed]
- Dite, W.; Temple, V. A clinical test of stepping and change of direction to identify multiple falling older adults. Arch. Phys. Med. Rehabil. 2002, 83, 1566–1571. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, D. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39142–39148. [Google Scholar] [CrossRef]
- Collen, F.M.; Wade, D.T.; Bradshaw, C.M. Mobility after stroke: Reliability of measures of impairment and disability. Int. Disabil. Stud. 1990, 12, 6–9. [Google Scholar] [CrossRef]
- Lee, D.Y.; Lee, K.U.; Lee, J.H.; Kim, K.W.; Jhoo, J.H.; Youn, J.C.; Kim, S.Y.; Woo, S.I.; Woo, J.I. A Normative Study of the Mini-Mental State Examination in the Korean Elderly. J. Korean Neuropsychiatr. Assoc. 2002, 41, 508–525. [Google Scholar]
- Alden, D.; Austin, C.; Sturgeon, R. A Correlation between the Geriatric Depression Scale Long and Short Forms. J. Gerontol. 1989, 44, P124–P125. [Google Scholar] [CrossRef] [PubMed]
- Balestroni, G.; Bertolotti, G. EuroQol-5D (EQ-5D): An instrument for measuring quality of life. Monaldi Arch. Chest Dis. 2012, 78, 155–159. [Google Scholar] [CrossRef]
- Jung, H.Y.; Park, B.K.; Shin, H.S.; Kang, Y.K.; Pyun, S.B.; Paik, N.J.; Kim, S.H.; Kim, T.H.; Han, T.R. Development of the Korean Version of Modified Barthel Index (K-MBI): Multi-center Study for Subjects with Stroke. J. Korean Acad. Rehab. Med. 2007, 31283–31297. [Google Scholar]
- Wass, E.; Taylor, N.F.; Matsas, A. Familiarisation to treadmill walking in unimpaired older people. Gait Posture 2005, 21, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Fukuchi, C.A.; Fukuchi, R.K.; Duarte, M. A public dataset of overground and treadmill walking kinematics and kinetics in healthy individuals. PeerJ 2018, 6, e4640. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dorfman, M.; Herman, T.; Brozgol, M.; Shema, S.; Weiss, A.; Hausdorff, J.M.; Mirelman, A. Dual-Task Training on a Treadmill to Improve Gait and Cognitive Function in Elderly Idiopathic Fallers. J. Neurol. Phys. Ther. 2014, 38, 246–253. [Google Scholar] [CrossRef]
- Tak, S.; Ye, J.C. Statistical analysis of fNIRS data: A comprehensive review. NeuroImage 2013, 85, 72–91. [Google Scholar] [CrossRef]
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Soc. Ser. B Methodol. 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Robbins, D.; Elwell, C.; Jimenez, A.; Goss-Sampson, M. Localised Muscle Tissue Oxygenation during Dynamic Exercise with Whole Body Vibration. J. Sports Sci. Med. 2012, 11, 346–351. [Google Scholar]
- Herold, F.; Wiegel, P.; Scholkmann, F.; Müller, N.G. Applications of Functional Near-Infrared Spectroscopy (fNIRS) Neuroimaging in Exercise–Cognition Science: A Systematic, Methodology-Focused Review. J. Clin. Med. 2018, 7, 466. [Google Scholar] [CrossRef] [Green Version]
- Strangman, G.; Culver, J.P.; Thompson, J.H.; Boas, D.A. A quantitative comparison of simultaneous BOLD fMRI and NIRS recordings during functional brain activation. Neuroimage 2002, 17, 719–731. [Google Scholar] [CrossRef]
- Morais, G.A.Z.; Balardin, J.B.; Sato, J.R. fNIRS Optodes’ Location Decider (fOLD): A toolbox for probe arrangement guided by brain regions-of-interest. Sci. Rep. 2018, 8, 3341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferraro, K. Self-Ratings of Health among the Old and the Old-Old. J. Heal. Soc. Behav. 1980, 21, 377. [Google Scholar] [CrossRef]
- Al-Yahya, E.; Mahmoud, W.; Meester, D.; Esser, P.; Dawes, H. Neural Substrates of Cognitive Motor Interference during Walking; Peripheral and Central Mechanisms. Front. Hum. Neurosci. 2019, 12, 536. [Google Scholar] [CrossRef]
- Abbud, G.; Li, K.; DeMont, R. Attentional requirements of walking according to the gait phase and onset of auditory stimuli. Gait Posture 2009, 30, 227–232. [Google Scholar] [CrossRef] [Green Version]
- Meester, D.; Al-Yahya, E.; Dawes, H.; Martin-Fagg, P.; Piñon, C. Associations between prefrontal cortex activation and H-reflex modulation during dual task gait. Front. Hum. Neurosci. 2014, 8, 78. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.Y.; Kim, E.J.; You, J.S.H. Adaptive locomotor network activation during randomized walking speeds using functional near-infrared spectroscopy. Technol. Heal. Care 2017, 25, 93–98. [Google Scholar] [CrossRef] [Green Version]
- Nordin, A.D.; Hairston, W.D.; Ferris, D.P. Faster Gait Speeds Reduce Alpha and Beta EEG Spectral Power From Human Sensorimotor Cortex. IEEE Trans. Biomed. Eng. 2019, 67, 842–853. [Google Scholar] [CrossRef]
- Marigold, D.S.; Andujar, J.E.; Lajoie, K.; Drew, T. Chapter 6—Motor planning of locomotor adaptations on the basis of vision: The role of the posterior parietal cortex. Prog. Brain Res. 2011, 188, 83–100. [Google Scholar] [CrossRef]
- Young, D.R.; Parikh, P.J.; Layne, C. The Posterior Parietal Cortex is Involved in Gait Adaptation: A Bilateral Transcranial Direct Current Stimulation Study. Front. Hum. Neurosci. 2020, 14, 464. [Google Scholar] [CrossRef]
- An, J.; Yoo, D.; Lee, B.-C. Electrocortical activity changes in response to unpredictable trip perturbations induced by a split-belt treadmill. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019. [Google Scholar] [CrossRef]
- Pizzamiglio, S.; Abdalla, H.; Naeem, U.; Turner, D.L. Neural predictors of gait stability when walking freely in the real-world. J. Neuroeng. Rehabil. 2018, 15, 11. [Google Scholar] [CrossRef] [PubMed]
- Rosano, C.; Aizenstein, H.; Brach, J.; Longenberger, A.; Studenski, S.; Newman, A.B. Special Article: Gait Measures Indicate Underlying Focal Gray Matter Atrophy in the Brain of Older Adults. J. Gerontol. Ser. A Boil. Sci. Med Sci. 2008, 63, 1380–1388. [Google Scholar] [CrossRef] [Green Version]
- Rubino, A.; Assogna, F.; Piras, F.; Di Battista, M.E.; Imperiale, F.; Chiapponi, C.; Spalletta, G.; Meco, G. Does a volume reduction of the parietal lobe contribute to freezing of gait in Parkinson’s disease? Parkinsonism Relat. Disord. 2014, 20, 1101–1103. [Google Scholar] [CrossRef] [PubMed]
- Daffner, K.R.; Sun, X.; Tarbi, E.C.; Rentz, D.M.; Holcomb, P.J.; Riis, J.L. Does compensatory neural activity survive old-old age? NeuroImage 2011, 54, 427–438. [Google Scholar] [CrossRef] [Green Version]
- Roeder, L.; Boonstra, T.W.; Smith, S.S.; Kerr, G.K. Dynamics of corticospinal motor control during overground and treadmill walking in humans. J. Neurophysiol. 2018, 120, 1017–1031. [Google Scholar] [CrossRef] [PubMed]
- Scholkmann, F.; Gerber, U.; Wolf, M.; Wolf, U. End-tidal CO2: An important parameter for a correct interpretation in functional brain studies using speech tasks. NeuroImage 2013, 66, 71–79. [Google Scholar] [CrossRef]
| All Participants (n = 50) | Young-Old (65–74 Years) (n = 27) | Old-Old (75–84 Years) (n = 23) | p Value | |
|---|---|---|---|---|
| Age (years, mean ± SD, range) | 73.80 ± 4.79 (65-82) | 70.19 ± 3.03 (65–74) | 78.04 ± 2.33 (75–82) | <0.001 * |
| Sex (Male:Female) | 19:31 | 10:17 | 9:14 | 0.555 |
| Height (cm, mean ± SD, range) | 158.64 ± 7.67 (141–179) | 160.22 ± 7.64 (148–179) | 156.77 ± 7.45 (141–170) | 0.114 |
| Weight (kg, mean ± SD, range) | 61.16 ± 9.23 (42–86) | 63.19 ± 10.10 (42–86) | 58.78 ± 7.64 (43–75) | 0.093 |
| BMI (kg/m2, mean ± SD, range) | 24.22 ± 2.99 (16.2–31.2) | 24.54 ± 2.93 (19.2–31.2) | 23.85 ± 3.10 (16.2–28.4) | 0.419 |
| Education (years, mean ± SD, range) | 8.31 ± 5.07 (0–16) | 9.42 ± 3.09 (6–16) | 7.65 ± 5.93 (0–16) | 0.278 |
| Medical History (N, %) | ||||
| Neck pain | 5 (10.0) | 4 (14.8) | 1 (4.3) | 0.229 |
| Low back pain | 9 (18.0) | 5 (18.5) | 4 (17.4) | 0.606 |
| Rheumatoid arthritis | 2 (4.0) | 1 (3.7) | 1 (4.3) | 0.713 |
| Osteoarthritis | 8 (16.0) | 3 (11.1) | 5 (21.7) | 0.263 |
| High blood pressure | 28 (56.0) | 14 (51.9) | 14 (60.9) | 0.362 |
| Diabetes | 9 (18.0) | 5 (18.5) | 4 (17.4) | 0.606 |
| Heart disease | 5 (10.0) | 1 (3.7) | 4 (17.4) | 0.129 |
| SPPB (mean ± SD, range) | 11.18 ± 0.98 (8–12) | 11.59 ± 0.69 (10–12) | 10.70 ± 1.06 (8–12) | <0.001 * |
| FSST (sec, mean ± SD, range) | 8.10 ± 1.25 (4.48–10.94) | 7.52 ± 1.12 (4.48–9.57) | 8.78 ± 1.04 (6.85–10.94) | <0.001 * |
| TUG (sec, mean ± SD, range) | 8.11 ± 1.20 (5.92–10.97) | 7.66 ± 0.92 (5.92–9.50) | 8.63 ± 1.28 (6.48–10.97) | 0.003 * |
| 10MWT (m/s, mean ± SD, range) | 1.41 ± 0.20 (0.85–1.80) | 1.48 ± 0.17 (1.22–1.80) | 1.33 ± 0.21 (0.85–1.74) | 0.006 * |
| K-MMSE (mean ± SD, range) | 25.74 ± 3.50 (13–30) | 26.63 ± 2.44 (22–30) | 24.70 ± 4.26 (13–30) | 0.063 |
| K-MBI (mean ± SD, range) | 100.0 ± 0.0 (100) | 100.0 ± 0.0 (100) | 100.0 ± 0.0 (100) | 1.000 |
| EQ-5D (mean ± SD, range) | 0.89 ± 0.09 (0.56–0.95) | 0.91 ± 0.08 (0.56–0.95) | 0.86 ± 0.09 (0.67–0.95) | 0.029 * |
| GDS-SF (mean ± SD, range) | 3.58 ± 3.76 (0–13) | 2.3 ± 3.34 (0–12) | 5.09 ± 3.75 (0–13) | 0.008 * |
| All Participants (n = 50) | Young-Old (65–74 Years) (n = 27) | Old-Old (75–84 Years) (n = 23) | p Value | |
|---|---|---|---|---|
| Treadmill speed (km/h, mean ± SD, range) | ||||
| Self-selected walking | 3.31 ± 0.45 (2.4–4.2) | 3.41 ± 0.44 (2.4–4.2) | 3.19 ± 0.44 (2.4–4.2) | 0.035 * |
| Fast walking | 4.31 ± 0.59 (3.1–5.5) | 4.46 ± 0.57 (3.1–5.5) | 4.14 ± 0.59 (3.1–5.5) | 0.032 * |
| Verbal fluency performance (mean ± SD, range) | ||||
| Self–selected walking | 29.79 ± 12.22 (9–61) | 34.85 ± 15.24 (23–61) | 26.83 ± 9.58 (9–45) | 0.019 * |
| Fast walking | 27.37 ± 9.95 (15–50) | 33.43 ± 10.36 (25–50) | 23.83 ± 8.14 (15–39) | 0.037 * |
| Self-Selected Walking Speed | Fast Walking Speed | Main Effect | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Single-Task | Dual-Task | Single-Task | Dual-Task | Task | Task × Group | Speed | Speed × Group | ||||||
| ROI | Young-Old | Old-Old | Young-Old | Old-Old | Young-Old | Old-Old | Young-Old | Old-Old | |||||
| M1-leg | Rt. | 0.08 (0.02) | 0.11 (0.02) | 0.12 (0.02) | 0.13 (0.02) | 0.07 (0.02) | 0.12 (0.03) | 0.11 (0.02) | 0.12 (0.04) | 0.033 * | 0.106 | 0.882 | 0.762 |
| Lt. | 0.09 (0.02) | 0.09 (0.02) | 0.10 (0.02) | 0.09 (0.02) | 0.08 (0.02) | 0.11 (0.03) | 0.09 (0.03) | 0.11 (0.04) | 0.413 | 0.566 | 0.712 | 0.193 | |
| PM | Rt. | 0.05 (0.02) | 0.08 (0.03) | 0.13 (0.02) | 0.09 (0.02) | 0.06 (0.03) | 0.08 (0.02) | 0.16 (0.05) | 0.08 (0.02) | 0.003 * | 0.004 * | 0.578 | 0.454 |
| Lt. | 0.10 (0.03) | 0.08 (0.03) | 0.28 (0.07) | 0.20 (0.07) | 0.09 (0.03) | 0.06 (0.03) | 0.19 (0.03) | 0.14 (0.04) | <0.001 * | 0.436 | 0.079 | 0.878 | |
| SMA | 0.05 (0.02) | 0.08 (0.03) | 0.11 (0.02) | 0.09 (0.03) | 0.04 (0.03) | 0.06 (0.02) | 0.09 (0.02) | 0.10 (0.03) | <0.001 * | 0.111 | 0.448 | 0.663 | |
| S1 | Rt. | 0.08 (0.02) | 0.09 (0.02) | 0.18 (0.03) | 0.05 (0.03) | 0.04 (0.02) | 0.03 (0.05) | 0.15 (0.03) | 0.07 (0.03) | 0.136 | 0.192 | 0.490 | 0.635 |
| Lt. | 0.10 (0.02) | 0.10 (0.02) | 0.14 (0.02) | 0.09 (0.02) | 0.08 (0.02) | 0.12 (0.03) | 0.13 (0.03) | 0.11 (0.05) | 0.121 | 0.020 * | 0.761 | 0.905 | |
| PPC | Rt. | 0.09 (0.02) | 0.08 (0.02) | 0.18 (0.03) | 0.05 (0.03) | 0.04 (0.02) | 0.03 (0.04) | 0.15 (0.03) | 0.07 (0.03) | 0.006 * | 0.008 * | 0.110 | 0.510 |
| Lt. | 0.07 (0.02) | 0.05 (0.02) | 0.11 (0.03) | 0.05 (0.02) | 0.03 (0.03) | 0.05 (0.02) | 0.06 (0.03) | 0.03 (0.02) | 0.333 | 0.045 * | 0.001 * | 0.127 | |
| dlPFC | Rt. | 0.04 (0.02) | 0.05 (0.02) | 0.09 (0.02) | 0.08 (0.02) | 0.03 (0.02) | 0.05 (0.02) | 0.09 (0.02) | 0.07 (0.03) | <0.001 * | 0.118 | 0.656 | 0.773 |
| Lt. | 0.04 (0.02) | 0.05 (0.02) | 0.06 (0.03) | 0.07 (0.02) | 0.03 (0.02) | 0.03 (0.02) | 0.06 (0.03) | 0.07 (0.02) | 0.014 * | 0.859 | 0.070 | 0.102 | |
| vmPFC | Rt. | 0.10 (0.03) | 0.10 (0.04) | 0.17 (0.03) | 0.19 (0.05) | 0.09 (0.03) | 0.07 (0.02) | 0.16 (0.03) | 0.30 (0.08) | 0.003 * | 0.244 | 0.524 | 0.198 |
| Lt. | 0.11 (0.02) | 0.10 (0.02) | 0.17 (0.03) | 0.17 (0.03) | 0.07 (0.03) | 0.07 (0.02) | 0.17 (0.03) | 0.16 (0.04) | <0.001 * | 0.889 | 0.008 * | 0.145 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.; Lee, G.; Lee, J.; Kim, Y.-H. Changes in Cortical Activity during Preferred and Fast Speed Walking under Single- and Dual-Tasks in the Young-Old and Old-Old Elderly. Brain Sci. 2021, 11, 1551. https://doi.org/10.3390/brainsci11121551
Kim J, Lee G, Lee J, Kim Y-H. Changes in Cortical Activity during Preferred and Fast Speed Walking under Single- and Dual-Tasks in the Young-Old and Old-Old Elderly. Brain Sciences. 2021; 11(12):1551. https://doi.org/10.3390/brainsci11121551
Chicago/Turabian StyleKim, Jinuk, Gihyoun Lee, Jungsoo Lee, and Yun-Hee Kim. 2021. "Changes in Cortical Activity during Preferred and Fast Speed Walking under Single- and Dual-Tasks in the Young-Old and Old-Old Elderly" Brain Sciences 11, no. 12: 1551. https://doi.org/10.3390/brainsci11121551
APA StyleKim, J., Lee, G., Lee, J., & Kim, Y.-H. (2021). Changes in Cortical Activity during Preferred and Fast Speed Walking under Single- and Dual-Tasks in the Young-Old and Old-Old Elderly. Brain Sciences, 11(12), 1551. https://doi.org/10.3390/brainsci11121551






