Relationship between Arterial Hypertension with Cognitive Performance in Elderly. Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Strategies
2.2. Eligibility Criteria
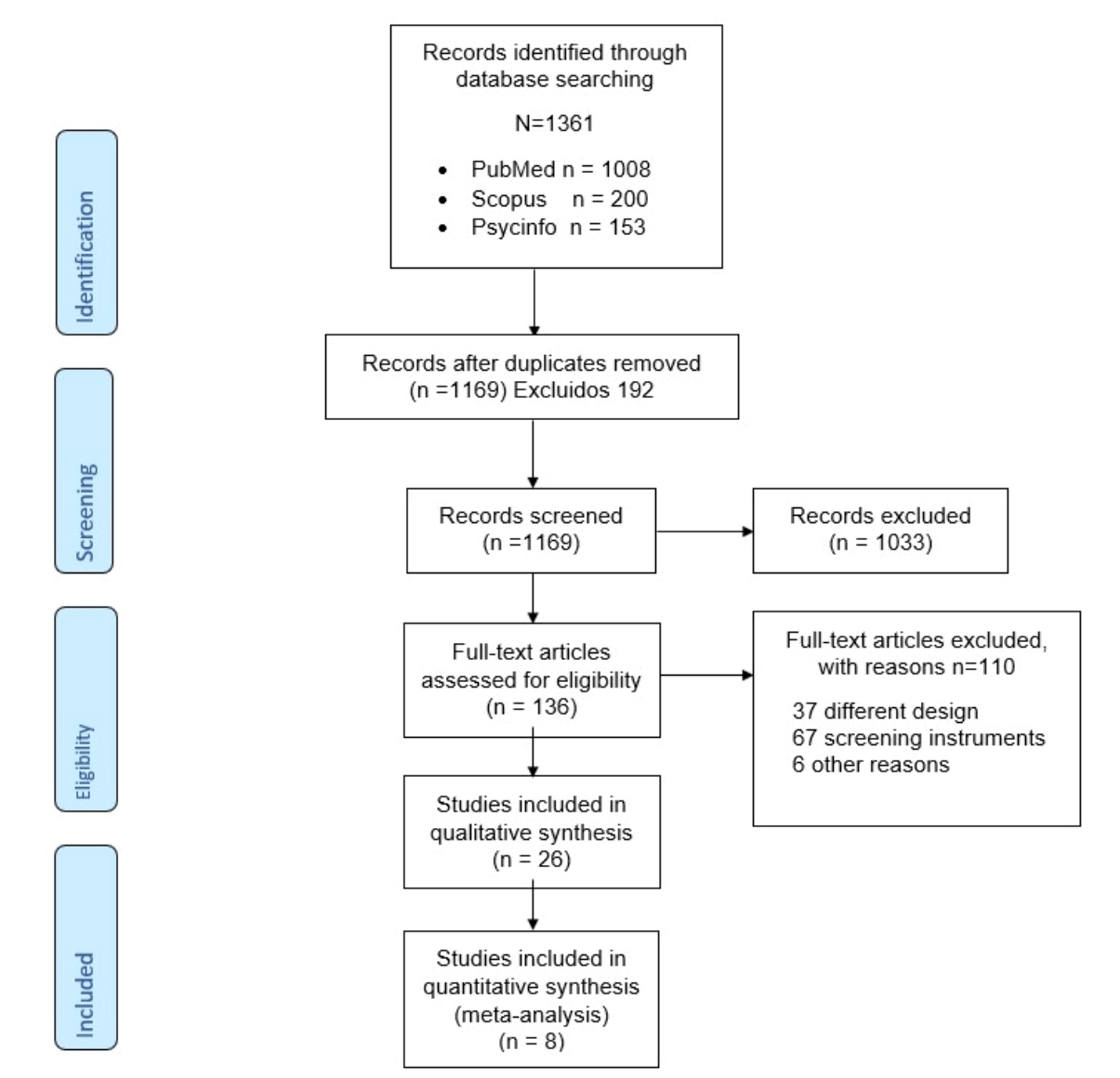
2.3. Article Selection
2.4. Analysis and Data Synthesis
3. Results
3.1. Studies Selection
3.2. Studies Characteristics
3.3. Relationship of Cognitive Performance with Arterial Hypertension
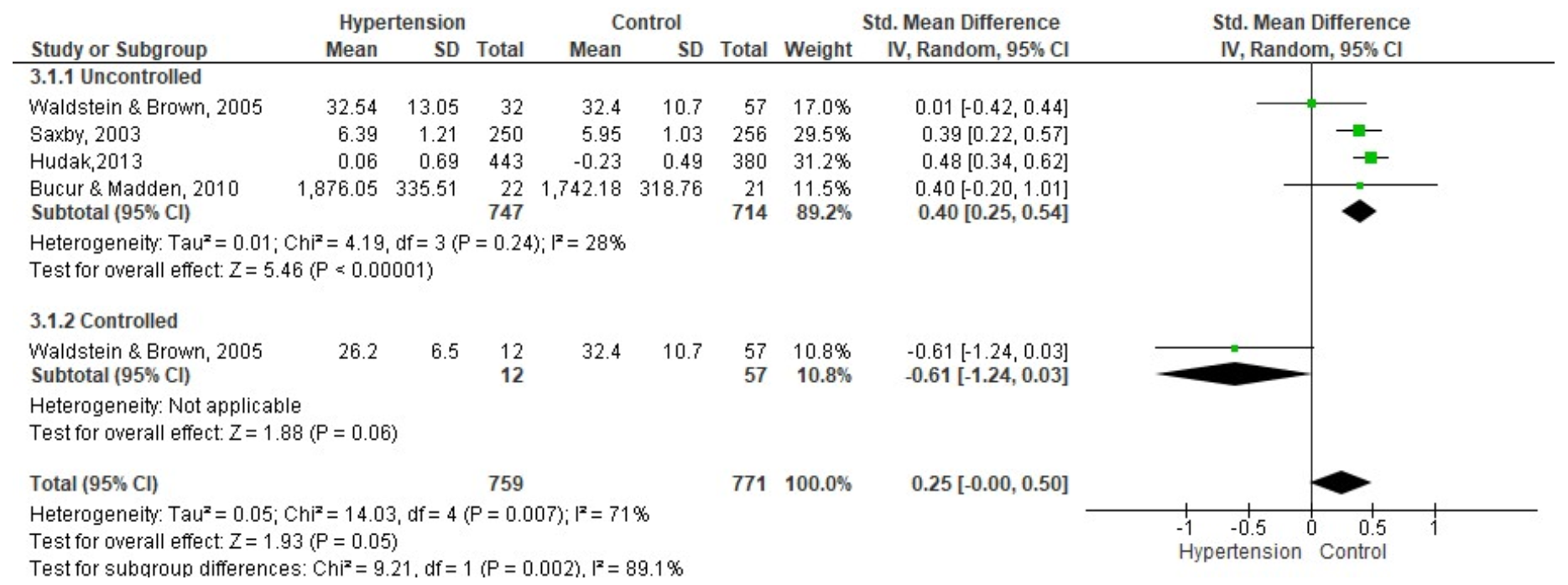
3.3.1. Processing Speed
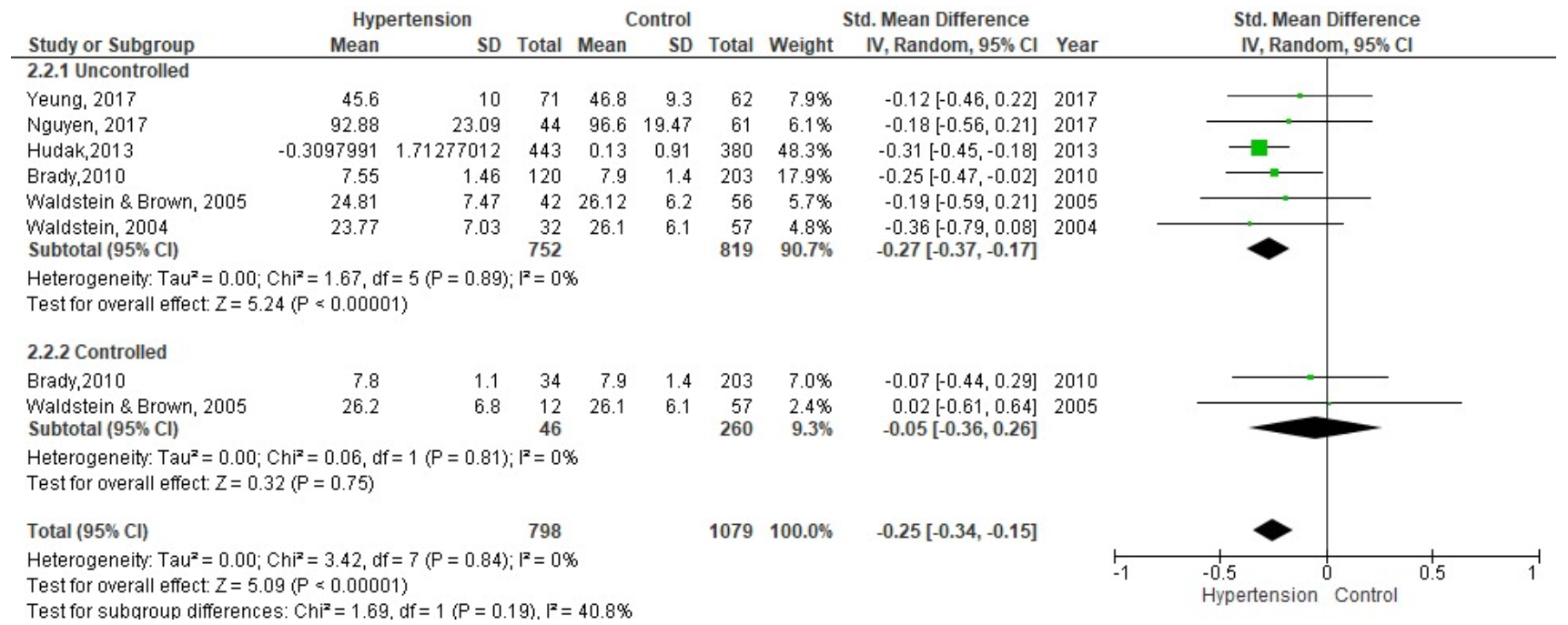
3.3.2. Working Memory
3.3.3. Short-Term Memory and Learning
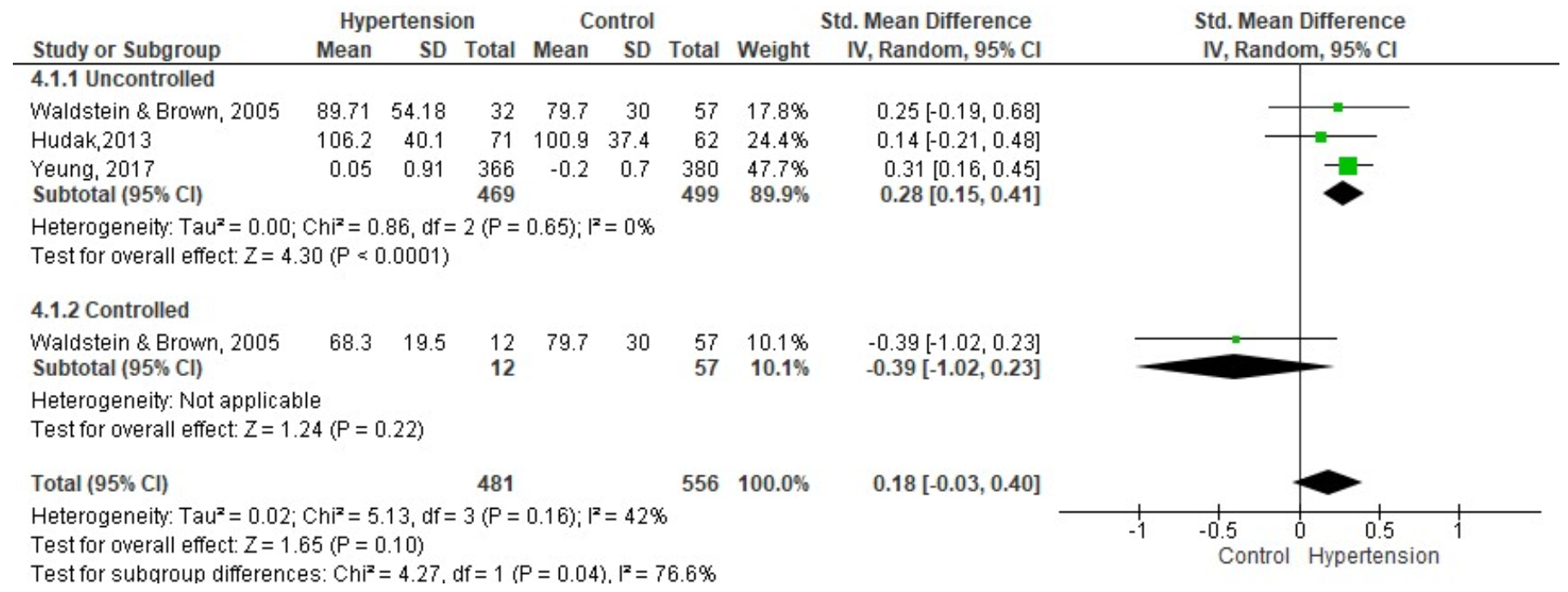
3.3.4. Delayed Memory
3.3.5. Other Cognitive Processes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. PRISMA (Systematic Revision Report Elements and Meta-Analysis Protocols) Verification List, 2009
| Section/Topic | # | Checklist Item | Reported on Page # | |
| TITLE | ||||
| Title | 1 | Identify the report as a systematic review, meta-analysis, or both. | 1 | |
| ABSTRACT | ||||
| Structured summary | 2 | Provide a structured summary including, as applicable: background; objectives; data sources; eligibility study criteria, participants, interventions; study appraisal and synthesis methods; results; limitations; conclusions and key findings implications; systematic review registration number. | 1 | |
| INTRODUCTION | ||||
| Rationale | 3 | Describe the rationale for the review within the context of what is already known. | 2 | |
| Objectives | 4 | Provide an explicit statement of questions being addressed with reference to participants, interventions, comparisons, outcomes, and study design (PICOS). | 3 | |
| METHODS | ||||
| Protocol and registration | 5 | Indicate if a reviewed protocol exists, if and where it can be accessed (e.g., Web address); and, if available, provide registration information including registration number. | NA | |
| Eligibility criteria | 6 | Specify study characteristics (e.g., PICOS, follow-up length) and report characteristics (e.g., years considered, language, publication status) used as criteria for eligibility, giving rationale. | 3 | |
| Information sources | 7 | Describe all information sources (e.g., databases with coverage dates, contact study authors to identify additional studies) in the search and date last searched. | 3 | |
| Search | 8 | Present full electronic search strategy for at least one database, including any limits used, such that it could be repeated. | 3 | |
| Study selection | 9 | State the process for selecting studies (i.e., screening, eligibility, included in systematic review, and, if applicable, included in the meta-analysis). | 3 | |
| Data collection process | 10 | Describe method of data extraction from reports (e.g., piloted forms, independently, in duplicate) and any processes for obtaining and confirming data from investigators. | 3 | |
| Data items | 11 | List and define all variables for which data were sought (e.g., PICOS, funding sources) and any assumptions and simplifications made. | 3 | |
| Risk of bias in individual studies | 12 | Describe methods used for assessing risk of bias of individual studies (including specification of whether this was done at the study or outcome level), and how this information is to be used in any data synthesis. | 3 | |
| Summary measures | 13 | State the principal summary measures (e.g., risk ratio, difference in means). | 3 | |
| Synthesis of results | 14 | Describe the handling data methods and study combining results; if done, including consistency measures (e.g., I2) for each meta-analysis. | 3 | |
| Risk of bias across studies | 15 | Specify any assessment of risk of bias that may affect the cumulative evidence (e.g., publication bias, selective reporting within studies). | NA | |
| Additional analyses | 16 | Describe methods of additional analyses (e.g., sensitivity or subgroup analyses, meta-regression); if done, indicating which were pre-specified. | NA | |
| RESULTS | ||||
| Study selection | 17 | Give numbers of screened studies, assessed for eligibility, included in the review, with reasons for exclusions at each stage, ideally with a flow diagram. | 4 | |
| Study characteristics | 18 | For each study, present characteristics for which data were extracted (e.g., study size, PICOS, follow-up period) and provide the citations. | 4 | |
| Risk of bias within studies | 19 | Present data on risk of bias of each study and, if available, any outcome level assessment (see item 12). | 18 | |
| Results of individual studies | 20 | For all outcomes considered (benefits or disadvantages), present, for each study: (a) simple summary data for each intervention group (b) effect estimates and confidence intervals, ideally with a forest plot. | 4–12 | |
| Synthesis of results | 21 | Present results of each meta-analysis done, including confidence intervals and consistency measures. | 4–12 | |
| Risk of bias across studies | 22 | Present any assessment of risk of bias results across studies (see Item 15). | 18 | |
| Additional analysis | 23 | Give results of additional analyses if done (e.g., sensitivity or subgroup analyses, meta-regression [see Item 16]). | NA | |
| DISCUSSION | ||||
| Summary of evidence | 24 | Summarize the main findings including the strength of evidence for each main outcome; consider their relevance to key groups (e.g., healthcare providers, users, and policy makers). | 14 | |
| Limitations | 25 | Discuss limitations at study and outcome level (e.g., risk of bias), and at review-level (e.g., incomplete retrieval of identified research, reporting bias). | 14 | |
| Conclusions | 26 | Provide a general interpretation of the results in the context of other evidence, and implications for future research. | 14 | |
| FUNDING | ||||
| Funding | 27 | Describe funding sources for the systematic review and other support (e.g., supply of data); role of funders for the systematic review. | 15 | |
Appendix B. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Case-Control Studies in Meta-Analyses
| Study | Selection | Comparability | Exposure | Total Quality Score | |||||
| In the Case Definition | Representativeness of the Cases | Selection of Controls | Definition of Controls | Comparability of Cases and Controls | Ascertainment of Exposure | Same Method of Ascertainment for Cases and Controls | Non-Respose Rate | ||
| Wei et al., 2018 [42] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 7 |
| Yeung et al.,2017 [52] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Nguyen et al., 2017 [55] | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 7 |
| Hudak et al., 2013 [37] | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 6 |
| Yasar et al., 2011 [38] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Bucur & Madden., 2010 [46] | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 7 |
| Brady et al., 2005 [39] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Waldstein, Brown et al., 2005 [31] | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 7 |
| Waldstein & Katzel, 2004 [36] | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 7 |
| Saxby et al., 2003 [48] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7 |
| Harrington et al., 2000 [49] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7 |
References
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the Management of Arterial Hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E.; Collins, K.J.; Himmelfarb, C.D.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, 1269–1324. [Google Scholar] [CrossRef] [PubMed]
- Gómez, J.F.; Camacho, P.A.; López-López, J.; López-Jaramillo, P. Control y Tratamiento de La Hipertensión Arterial: Programa 20-20. Rev. Colomb. de Cardiol. 2019, 26, 99–106. [Google Scholar] [CrossRef]
- Cloutier, L.; Lamarre-Cliche, M. Hypertension in Adults With Type 2 Diabetes: A Review of Blood Pressure Measurement Methods, Targets and Therapy. Can. J. Diabetes 2018, 42, 188–195. [Google Scholar] [CrossRef]
- Radišauskas, R.; Kuzmickiene, I.; Milinavičiene, E.; Everatt, R. Hypertension, Serum Lipids and Cancer Risk: A Review of Epidemiological Evidence. Medicina 2016, 52, 89–98. [Google Scholar] [CrossRef]
- Liu, M.-Y.; Li, N.; Li, W.A.; Khan, H. Association between Psychosocial Stress and Hypertension: A Systematic Review and Meta-Analysis. Neurol. Res. 2017, 39, 573–580. [Google Scholar] [CrossRef]
- Walker, K.A.; Power, M.C.; Gottesman, R.F. Defining the Relationship Between Hypertension, Cognitive Decline, and Dementia: A Review. Curr. Hypertens. Rep. 2017, 19, 1–16. [Google Scholar] [CrossRef]
- Gorelick, P.B.; Erkinjuntti, T.; Hofman, A.; Rocca, W.A.; Skoog, I.; Winblad, B. Prevention of Vascular Dementia. Alzheimer Dis. Assoc. Disord. 1999, 13, S131–S139. [Google Scholar]
- Goshgarian, C.; Gorelick, P.B. Perspectives on the Relation of Blood Pressure and Cognition in the Elderly. Trends Cardiovasc. Med. 2019, 29, 12–18. [Google Scholar] [CrossRef]
- Iadecola, C.; Yaffe, K.; Biller, J.; Bratzke, L.C.; Faraci, F.M.; Gorelick, P.B.; Gulati, M.; Kamel, H.; Knopman, D.S.; Launer, L.J.; et al. Impact of Hypertension on Cognitive Function: A Scientific Statement from the American Heart Association. Hypertension 2016, 68, e67–e94. [Google Scholar] [CrossRef]
- Izzo, J.L.; Shykoff, B.E. Arterial Stiffness: Clinical Relevance, Measurement, and Treatment. Rev. Cardiovasc. Med. 2001, 2, 29–34. [Google Scholar]
- Iadecola, C. The Pathobiology of Vascular Dementia. Neuron 2013, 80, 844–866. [Google Scholar] [CrossRef]
- Yang, E.Y.; Chambless, L.; Sharrett, A.R.; Virani, S.S.; Liu, X.; Tang, Z.; Boerwinkle, E.; Ballantyne, C.M.; Nambi, V. Carotid Arterial Wall Characteristics Are Associated With Incident Ischemic Stroke But Not Coronary Heart Disease in the Atherosclerosis Risk in Communities (ARIC) Study. Stroke 2012, 43, 103–108. [Google Scholar] [CrossRef]
- Madhavan, M.; Graff-Radford, J.; Piccini, J.P.; Gersh, B.J. Cognitive Dysfunction in Atrial Fibrillation. Nat. Rev. Cardiol. 2018, 15, 744–756. [Google Scholar] [CrossRef]
- Gonzalez-Marrero, I.; Hernández-Abad, L.G.; Castañeyra-Ruiz, L.; Carmona-Calero, E.M.; Castañeyra-Perdomo, A. Variaciones de Los Plexos Coroideos y Las Barreras Cerebrales En La Hipertensión Arterial y El Envejecimiento. Neurología 2018. [Google Scholar] [CrossRef]
- Setiadi, A.; Korim, W.S.; Elsaafien, K.; Yao, S.T. The Role of the Blood–Brain Barrier in Hypertension. Exp. Physiol. 2018, 103, 337–342. [Google Scholar] [CrossRef]
- Rensma, S.P.; van Sloten, T.T.; Launer, L.J.; Stehouwer, C.D.A. Cerebral Small Vessel Disease and Risk of Incident Stroke, Dementia and Depression, and All-Cause Mortality: A Systematic Review and Meta-Analysis. Neurosci. Biobehav. Rev. 2018, 90, 164–173. [Google Scholar] [CrossRef]
- Lennon, M.J.; Makkar, S.R.; Crawford, J.D.; Sachdev, P.S. Midlife Hypertension and Alzheimer’s Disease: A Systematic Review and Meta-Analysis. J. Alzheimers Dis. 2019, 71, 307–316. [Google Scholar] [CrossRef]
- Park, J.-H.; Hong, J.-H.; Lee, S.-W.; Ji, H.D.; Jung, J.-A.; Yoon, K.-W.; Lee, J.-I.; Won, K.S.; Song, B.-I.; Kim, H.W. The Effect of Chronic Cerebral Hypoperfusion on the Pathology of Alzheimer’s Disease: A Positron Emission Tomography Study in Rats. Sci. Rep. 2019, 9, 14102. [Google Scholar] [CrossRef]
- Buford, T.W. Hypertension and Aging. Ageing Res. Rev. 2016, 26, 96–111. [Google Scholar] [CrossRef]
- Sierra, C. Hypertension and the Risk of Dementia. Front. Cardiovasc. Med. 2020, 7, 5. [Google Scholar] [CrossRef]
- Craik, F.I.M.; Bialystok, E. Cognition through the Lifespan: Mechanisms of Change. Trends Cogn. Sci. 2006, 10, 131–138. [Google Scholar] [CrossRef]
- Salthouse, T.A. Major Issues in Cognitive Aging; Oxford University Press: New York, NY, USA, 2010. [Google Scholar]
- Salthouse, T.A. Localizing Age-Related Individual Differences in a Hierarchical Structure. Intelligence 2004, 32, 541–561. [Google Scholar] [CrossRef]
- Salthouse, T.A. Relations between Cognitive Abilities and Measures of Executive Functioning. Neuropsychology 2005, 19, 532–545. [Google Scholar] [CrossRef]
- Tucker-Drob, E.; Johnson, K.; Jones, R. The Cognitive Reserve Hypothesis: A Longitudinal Examination of Age- Associated Declines in Reasoning and Processing Speed. Dev. Psychol. 2011, 45, 431–446. [Google Scholar] [CrossRef]
- van den Berg, E.; Kloppenborg, R.P.; Kessels, R.P.; Jaap Kappelle, L.; Jan Biessels, G. Type 2 Diabetes Mellitus, Hypertension, Dyslipidemia and Obesity: A Systematic Comparison of Their Impact on Cognition. Biochim. Biophys. Acta-Mol. Basis Dis. 2009, 1792, 470–481. [Google Scholar] [CrossRef]
- Birns, J.; Kalra, L. Cognitive Function and Hypertension. J. Hum. Hypertens. 2009, 23, 86–96. [Google Scholar] [CrossRef]
- Forte, G.; de Pascalis, V.; Favieri, F.; Casagrande, M. Effects of Blood Pressure on Cognitive Performance: A Systematic Review. J. Clin. Med. 2019, 9, 34. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.A.; Shea, B.; O´Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality If Nonrandomized Studies in Meta-Analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 14 October 2021).
- Waldstein, S.R.; Brown, J.R.P.; Maier, K.J.; Katzel, L.I. Diagnosis of Hypertension and High. Blood Pressure Levels Negatively Affect. Cognitive Function in Older Adults. Ann. Behav. Med. 2005, 29, 174–180. [Google Scholar] [CrossRef]
- Morris, M.C.; Scherr, P.A.; Hebert, L.E.; Bennett, D.A.; Wilson, D.-F.R.S.; Glynn, R.J.; Evans, D.A. Association between Blood Pressure and Cognitive Function in a Biracial Community Population of Older Persons. Neuroepidemiology 2002, 21, 123–130. [Google Scholar] [CrossRef]
- Izquierdo-Porrera, A.M.; Waldstein, S.R. Cardiovascular Risk Factors and Cognitive Function in African Americans. J. Gerontol. Ser. B 2002, 57, P377–P380. [Google Scholar] [CrossRef] [PubMed]
- Fischer, A.L.; O’Rourke, N.; Loken Thornton, W. Age Differences in Cognitive and Affective Theory of Mind: Concurrent Contributions of Neurocognitive Performance, Sex, and Pulse Pressure. J. Gerontol. Ser. B 2017, 72, 71–81. [Google Scholar] [CrossRef] [PubMed]
- Singh-Manoux, A.; Marmot, M. High Blood Pressure Was Associated with Cognitive Function in Middle-Age in the Whitehall II Study. J. Clin. Epidemiol. 2005, 58, 1308–1315. [Google Scholar] [CrossRef] [PubMed]
- Waldstein, S.R.; Katzel, L.I. Gender Differences in the Relation of Hypertension to Cognitive Function in Older Adults. Neurol. Res. 2004, 26, 502–506. [Google Scholar] [CrossRef]
- Hudak, E.M.; Edwards, J.D.; Athilingam, P.; McEvoy, C.L. A Comparison of Cognitive and Everyday Functional Performance Among Older Adults With and Without Hypertension. Clin. Gerontol. 2013, 36, 113–131. [Google Scholar] [CrossRef][Green Version]
- Yasar, S.; Ko, J.Y.; Nothelle, S.; Mielke, M.M.; Carlson, M.C. Evaluation of the Effect of Systolic Blood Pressure and Pulse Pressure on Cognitive Function: The Women’s Health and Aging Study II. PLoS ONE 2011, 6, e27976. [Google Scholar] [CrossRef]
- Brady, C.B.; Spiro, A.; Gaziano, J.M. Effects of Age and Hypertension Status on Cognition: The Veterans Affairs Normative Aging Study. Neuropsychology 2005, 19, 770–777. [Google Scholar] [CrossRef]
- Kritz-Silverstein, D.; Laughlin, G.A.; McEvoy, L.K.; Barrett-Connor, E. Sex and Age Differences in the Association of Blood Pressure and Hypertension with Cognitive Function in the Elderly: The Rancho Bernardo Study. J. Prev. Alzheimers Dis. 2017, 4, 165–173. [Google Scholar] [CrossRef]
- Whitfield, K.E.; Allaire, J.C.; Gamaldo, A.; Aiken-Morgan, A.T.; Sims, R.; Edwards, C. Blood Pressure and Memory in Older African Americans. Ethn. Dis. 2008, 18, 181–186. [Google Scholar]
- Wei, J.; Yin, X.; Liu, Q.; Tan, L.; Jia, C. Association between Hypertension and Cognitive Function: A Cross-Sectional Study in People over 45 Years Old in China. J. Clin. Hypertens. 2018, 20, 1575–1583. [Google Scholar] [CrossRef]
- Dregan, A.; Stewart, R.; Gulliford, M.C. Cardiovascular Risk Factors and Cognitive Decline in Adults Aged 50 and over: A Population-Based Cohort Study. Age Ageing 2013, 42, 338–345. [Google Scholar] [CrossRef]
- Okusaga, O.; Stewart, M.C.W.; Butcher, I.; Deary, I.; Fowkes, F.G.R.; Price, J.F. Smoking, Hypercholesterolaemia and Hypertension as Risk Factors for Cognitive Impairment in Older Adults. Age Ageing 2013, 42, 306–311. [Google Scholar] [CrossRef]
- Hebert, L.E.; Scherr, P.A.; Bennett, D.A.; Bienias, J.L.; Wilson, R.S.; Morris, M.C.; Evans, D.A. Blood Pressure and Late-Life Cognitive Function Change. Neurology 2004, 62, 2021–2024. [Google Scholar] [CrossRef]
- Bucur, B.; Madden, D.J. Effects of Adult Age and Blood Pressure on Executive Function and Speed of Processing. Exp. Aging Res. 2010, 36, 153–168. [Google Scholar] [CrossRef]
- Cherbuin, N.; Mortby, M.E.; Janke, A.L.; Sachdev, P.S.; Abhayaratna, W.P.; Anstey, K.J. Blood Pressure, Brain Structure, and Cognition: Opposite Associations in Men and Women. Am. J. Hypertens. 2015, 28, 225–231. [Google Scholar] [CrossRef]
- Saxby, B.K.; Harrington, F.; McKeith, I.G.; Wesnes, K.; Ford, G.A. Effects of Hypertension on Attention, Memory, and Executive Function in Older Adults. Health Psychol. 2003, 22, 587–591. [Google Scholar] [CrossRef]
- Harrington, F.; Saxby, B.K.; Mckeith, I.G.; Wesnes, K.; Ford, G.A. Cognitive Performance in Hypertensive and Normotensive Older Subjects Methods. Hypertension 2000, 36, 1079–1082. [Google Scholar] [CrossRef]
- Elias, P.K.; Elias, M.F.; Robbins, M.A.; Budge, M.M. Blood Pressure-Related Cognitive Decline. Hypertension 2004, 44, 631–636. [Google Scholar] [CrossRef]
- Waldstein, S.R.; Giggey, P.P.; Thayer, J.F.; Zonderman, A.B. Nonlinear Relations of Blood Pressure to Cognitive Function: The Baltimore Longitudinal Study of Aging. Hypertension 2005, 45, 374–379. [Google Scholar] [CrossRef]
- Yeung, S.E.; Thornton, W.L. Do It-Yourself: Home Blood Pressure as a Predictor of Traditional and Everyday Cognition in Older Adults. PLoS ONE 2017, 12, e0177424. [Google Scholar] [CrossRef]
- Stewart, R.; Prince, M.; Mann, A. Age, Vascular Risk, and Cognitive Decline in an Older, British, African-Caribbean Population. J. Am. Geriatr. Soc. 2003, 51, 1547–1553. [Google Scholar] [CrossRef]
- Robbins, M.A.; Elias, M.F.; Elias, P.K.; Budge, M.M. Blood Pressure and Cognitive Function in an African-American and a Caucasian-American Sample: The Maine-Syracuse Study. Psychosom. Med. 2005, 67, 707–714. [Google Scholar] [CrossRef][Green Version]
- Nguyen, L.A.; Haws, K.A.; Fitzhugh, M.C.; Torre, G.A.; Hishaw, G.A.; Alexander, G.E. Interactive Effects of Subjective Memory Complaints and Hypertension on Learning and Memory Performance in the Elderly. Aging Neuropsychol. Cogn. 2016, 23, 154–170. [Google Scholar] [CrossRef]
- Nation, D.A.; Wierenga, C.E.; Delano-wood, L.; Jak, A.J.; Delis, D.C.; Salmon, D.P.; Bondi, M.W. Elevated Pulse Pressure Is Associated with Age-Related Decline in Language Ability. J. Int. Neuropsychol. Soc. 2010, 16, 933–938. [Google Scholar] [CrossRef]
- Waldstein, S.R.; Ryan, C.M.; Manuck, S.B.; Parkinson, D.K.; Bromet, E.J. Learning and Memory Function in Men With Untreated Blood Pressure Elevation. J. Consult. Clin. Psychol. 1991, 59, 513–517. [Google Scholar] [CrossRef]
- Schmidt, R.; Fazekas, F.; Offenbacher, H.; Lytwyn, H.; Blematl, B.; Niederkorn, K.; Horner, S.; Payer, F.; Freidl, W. Magnetic Resonance Imaging White Matter Lesions and Cognitive Impairment in Hypertensive Individuals. Arch. Neurol. 1991, 48, 417–420. [Google Scholar] [CrossRef]
- Petersen, R.C.; Caracciolo, B.; Brayne, C.; Gauthier, S.; Jelic, V.; Fratiglioni, L. Mild Cognitive Impairment: A Concept in Evolution. J. Intern. Med. 2014, 275, 214–228. [Google Scholar] [CrossRef]
- Squire, L.R.; Bayley, P.J. The Neuroscience of Remote Memory. Curr. Opin. Neurobiol. 2007, 17, 185–196. [Google Scholar] [CrossRef]
- Regenhardt, R.W.; Das, A.S.; Lo, E.H.; Caplan, L.R. Advances in Understanding the Pathophysiology of Lacunar Stroke: A Review. JAMA Neurol. 2018, 75, 1273–1281. [Google Scholar] [CrossRef]
- Stuhec, M.; Keuschler, J.; Serra-Mestres, J.; Isetta, M. Effects of Different Antihypertensive Medication Groups on Cognitive Function in Older Patients: A Systematic Review. Eur. Psychiatry 2017, 46, 1–15. [Google Scholar] [CrossRef]
- Alloubani, A.; Saleh, A.; Abdelhafiz, I. Hypertension and Diabetes Mellitus as a Predictive Risk Factors for Stroke. Diabetes Metab. Syndr. Clin. Res. Rev. 2018, 12, 577–584. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Thrippleton, M.J.; Makin, S.D.; Marshall, I.; Geerlings, M.I.; de Craen, A.J.; van Buchem, M.A.; Wardlaw, J.M. Cerebral Blood Flow in Small Vessel Disease: A Systematic Review and Meta-Analysis. J. Cereb. blood flow Metab. 2016, 36, 1653–1667. [Google Scholar] [CrossRef] [PubMed]
- Kisler, K.; Nelson, A.R.; Montagne, A.; Zlokovic, B.v. Cerebral Blood Flow Regulation and Neurovascular Dysfunction in Alzheimer Disease. Nat. Rev. Neurosci. 2017, 18, 419–434. [Google Scholar] [CrossRef] [PubMed]
- Chobanian, A.v.; Alderman, M.H.; DeQuattro, V.; Frohlich, E.D.; Gifford, R.W.; Hill, M.N.; Kaplan, N.M.; Langford, H.G.; Moore, M.A.; Nickey, W.A.; et al. The 1988 Report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. Arch. Intern. Med. 1988, 148, 1023–1038. [Google Scholar] [CrossRef]
- Staessen, J.; Bulpitt, C.; Clement, D.; de Leeuw, P.; Fagard, R.; Fletcher, A.; Forette, F.; Leonetti, G.; Nissinen, A.; O’Malley, K. Relation between Mortality and Treated Blood Pressure in Elderly Patients with Hypertension: Report of the European Working Party on High Blood Pressure in the Elderly. Br. Med. J. 1989, 298, 1552–1556. [Google Scholar] [CrossRef]
- Niermeyer, M.A. Cognitive and Gait Decrements among Non-Demented Older Adults with Type 2 Diabetes or Hypertension: A Systematic Review. Clin. Neuropsychol. 2018, 32, 1256–1281. [Google Scholar] [CrossRef]
- Gifford, K.A.; Badaracco, M.; Liu, D.; Tripodis, Y.; Gentile, A.; Lu, Z.; Palmisano, J.; Jefferson, A.L. Blood Pressure and Cognition Among Older Adults: A Meta-Analysis. Arch. Clin. Neuropsychol. 2013, 28, 649–664. [Google Scholar] [CrossRef]
- Hachinski, V.; Iadecola, C.; Petersen, R.C.; Breteler, M.M.; Nyenhuis, D.L.; Black, S.E.; Powers, W.J.; DeCarli, C.; Merino, J.G.; Kalaria, R.N.; et al. National Institute of Neurological Disorders and Stroke-Canadian Stroke Network Vascular Cognitive Impairment Harmonization Standards. Stroke 2006, 37, 2220–2241. [Google Scholar] [CrossRef]
- Stern, Y. Cognitive Reserve. Neuropsychologia 2009, 47, 2015–2028. [Google Scholar] [CrossRef]

| Study | Design (Years) | Goup | N | Age M (SD) | Sex (% Men) | Edu M (SD) | SBP M (SD) | DBP M (SD) | AHT Definition | Links Cognitive Impairment |
|---|---|---|---|---|---|---|---|---|---|---|
| Kritz-Silverstein et al., 2017 [40] | C-s | Man Hipertensive = 62.6% | 693 | 73.8 (9.9) | Some college o more 77% | 135 (20) | 77.5 (9) | A SBP ≥ 160 DBP ≥ 90 | Positive HTA | |
| Woman Hipertensive = 63.4 | 1022 | 73.2 (9.3) | Some college o more 62% | 136 (21) | 75 (9) | |||||
| Fischer et al. 2016 [34] | C-s | Hipertensive = 37.6% | 85 | 71.4 (5.5) | 69.4 | 14.3 (2.3) | 130 (15) | 74 (9) | A | Positive PP |
| Cherbuin et al., 2015 [47] | C (8) | Hipertensive = 51% | 266 | 70.4 (1.4) | 54 | 14.2 (2.6) | 150 (19) | 81 (10) | DM SBP ≥ 160 DBP ≥ 90 | Women Positive SBD/ Men Negative DBP |
| Okusaga et al., 2013 [44] | C (5) | - | 2312 | 61.7 (6.5) | 26.9 | - | 147 (21) | 84 (11) | - | Positive SBP |
| Dregan et al. 2013 [43] | C (8) | Hipertensive = 15% | 5936 | 66.9 (10.1) | 45 | 46% > 8 | 136 (19) | 75 (11) | Normal < 140/90 Border 140–160/90–99 High 160/100 | Positive SBP & DBP |
| Nation et al., 2010 [56] | C-s | Hipertensive = 52% | 109 | 74.2 (10) | 44 | 16.2 (2.3) | 126 (13) | 73 (9) | DM | Positive PP |
| Whitfield et al., 2008 [41] | C-s | - | 361 | 61.5 (9.4) | - | 12 (3.9) | 141 (22) | 82 (12) | - | Positive SBP |
| Singh-Manoux, et al., 2005 [35] | C (12) | Man | 4158 | 43.9 (6.0) | 70% > 8 | Low = 45% Medium = 40% Hihg = 15% | Low < 120/80 Medium 120–139/80–89 Hihg > 139/90 | Positive SBP & DBP | ||
| Woman | 1680 | 44.4 (6.0) | 48% > 8 | Low = 50% Medium = 34% High = 16% | ||||||
| Robbins et al., 2005 [54] | C (23) | African HTA = 42% | 147 | 54.7 (15.1) | 61.2 | 12.6 (2.5) | 139 (30) | 84 (20) | DM | Positive SBP |
| Caucasico Hipertensive = 36% | 1416 | 56.6 (17.1) | 56.2 | 14.4 (2.6) | 138 (27) | 81 (17.8) | ||||
| Waldstein, Giggey et al., 2005 [51] | C (11) | Hipertensive = 33.4% | 847 | 70.6 (8.5) | 59 | 16.6 (2.7) | 139 (20) | 82 (10.9) | A | Positive SBP U curve DBP |
| Hebert et al., 2004 [45] | C (6) | - | 4284 | 74 (6.4) | 38 | 12 (3.7) | 140 (20) | 77 (11.5) | - | U curve DBP |
| Ellias et al. 2004 [50] | C (20) | <47 years Hipertensive = 55.8% | 285 | 34.9 (7.6) | 48.4 | 14.3 (2.3) | 130 (18) | 80 (11.4) | SBP ≥ 160 DBP ≥ 90 | Positive SBP |
| ≥47 years Hipertensive = 73.8% | 244 | 58.1 (8.4) | 48.8 | 14.2 (2.7) | 146 (22) | 83 (12.2) | ||||
| Steward et al., 2003 [53] | C (1.5) | Hipertensive = 58% | 216 | 64 (5.3) | 44 | 66% > 8 | 138 (28) | 81 (18.1) | A | No association |
| Izquierdo-Porrera & Waldstein, 2002 [33] | C-s | Hipertensive = 53% | 43 | 59 (11.2) | 7 | 14 (2.5) | 136 (21) | 78 (11) | DM | Positive DBP |
| Morris et al., 2002 [32] | C-s | Hipertensive = 55% | 5816 | 65 a 74 (59%) 75–84 (30%) >85(11%) | 39 | 81% > 8 | 65–74 = 139 75–84 = 140 >85=138 | 65–74 = 79 75–84 = 75 >85=73 | SBP ≥ 160 DBP ≥ 90 | Positive SBP U curve DBP |
| Wei et al., 2018 [42] | C-c | Controlled hipertensive | 695 | 61(19) | 32.3 | 32% > 6 | 126 (10) | 74 (8) | DMS BP ≥ 140 DBP ≥ 90 | Positive AHT |
| Treated high BP hipertensive | 970 | 63 (9) | 31.1 | 26.4% > 6 | 156 (19) | 88 (14) | ||||
| Untreated hipertensive | 343 | 61 (9) | 41.7 | 30% > 6 años | 155 (19) | 89 (13) | ||||
| Normotensive | 4724 | 58 (9) | 34.3 | 32% > 6 | 118 (12) | 71 (9) | ||||
| Yeung et al.,2017 [52] | C-c | Hipertensive | 71 | 70.3 (6.5) | 51 | 14.2 (2.5) | 126 (10) | 73 (8) | DM | No association |
| Normotensive | 62 | 70.2 (6.4) | 49 | 15 (2.7) | 119 (13) | 71 (8) | ||||
| Nguyen et al., 2017 [55] | C-c | Hipertensive | 44 | 79 (5) | 46 | 17 (3.1) | 149 (16) | 83 (11) | DM | Positive AHT |
| Normotensive | 61 | 78.1 (5) | 53 | 15.9 (2.7) | 143 (17) | 78 (8) | ||||
| Hudak et al., 2013 [37] | C-c | Hipertensive | 390 | 73.3 (5.9) | - | 13.9 (2.7) | - | - | DM | Positive AHT |
| Normotensive | 380 | 73.3 (5.9) | - | 13.9 (2.7) | - | - | ||||
| Yasar et al., 2011 [38] | C-c (9) | Hipertensive SBP ≥ 160 | 190 | 74.1 (2.7) | - | 93.6% ≥ 12 | 178 (12) | 88 (17) | SBP > 140 | Positive AHT |
| Hipertensive SBP 140–159 | 113 | 73.7 (2.8) | - | 91% ≥ 12 | 149 (5) | 73 (12) | ||||
| Normotensive | 103 | 72.2 (2.9) | - | 92.2% ≥ 12 | 129 (9) | 67 (10) | ||||
| Bucur & Madden., 2010 [46] | C-c | Hipertensive | 21 | 68 (4.7) | 57 | 16.6 (4.7) | 139 (7) | 79 (9) | SBP ≥ 130 DBP ≥ 85 | Positive AHT |
| Normotensive | 22 | 67.8 (5.1) | 38 | 16.8 (2.3) | 118 (8) | 72 (5) | ||||
| Brady et al., 2005 [39] | C-c(2) | Controlled hipertensive | 34 | 68.6 (6) | - | 14.7 (2.4) | 127 (9) | 78 (8) | SBP ≥ 140 DBP ≥ 90 | Positive AHT |
| Treatable high BP hipertensives | 45 | 69.5 (6.1) | - | 14.5 (3.1) | 153 (14) | 89 (9) | ||||
| Untreatable hipertensive | 75 | 68.4 (7.5) | - | 13.8 (2.6) | 157 (16) | 89 (11) | ||||
| Normotensive | 203 | 66 (7) | - | 14.4 (2.6) | 124 (9) | 78 (6) | ||||
| Waldstein, Brown et al., 2005 [31] | C-c | Controlled hypertensive | 12 | 68.4 (9.8) | 69 | 16.8 (3.8) | 133 (5) | 76 (8) | DM | Positive AHT |
| High BP Hypertensive | 17 | 67.6 (5) | 62 | 15.5 (3.2) | 159 (9) | 85 (6) | ||||
| Normotensive | 57 | 65.8 (6.5) | 61 | 16.9 (2.7) | 120 (11) | 70 (7) | ||||
| High BP No hypertensive | 15 | 67 (6) | 65 | 15.3 (2.7) | 145 (8) | 81 (5) | ||||
| Waldstein & Katzel, 2004 [36] | C-c | Hypertensive Man | 31 | 68.9 (6.6) | 16.5 (3.4) | 147 (14) | 80.4 (7.5) | SBP ≥ 140 DBP ≥ 90 | Positive AHT | |
| Hypertensive Woman | 11 | 66.1 (5.6) | 14.6 (2) | 146 (13) | 81 (7) | |||||
| Normotensive Man | 30 | 66.8 (6.7) | 16.9 (2.6) | 123 (10) | 72 (7) | |||||
| Normotensive Woman | 26 | 65.1 (6.6) | 17 (2.8) | 117 (11) | 67 (7) | |||||
| Saxby et al., 2003 [48] | C-c | Hypertensive | 250 | 74 (4) | 47 | 10 (2) | 165 (8) | 89 (7) | SBP ≥ 160–79 DBP ≥ 90–99 | Positive AHT |
| Normotensive | 256 | 74 (4) | 56 | 10 (2) | 131 (11) | 74 (7) | ||||
| Harrington et al., 2000 [49] | C-c | Hypertensive | 107 | 76 (4) | 49 | 10 (2) | 164 (9) | 89 (7) | SBP ≥ 160 DBP ≥ 90 | Positive AHT |
| Normotensive | 116 | 76 (4) | 49 | 10 (2) | 131 (10) | 74 (7) |
| Study | Executive Functions | Work Memory | Processing Speed | Cognitive Inhibition | Short-Term Memory and Learning | Differed Memory | Reasoning |
|---|---|---|---|---|---|---|---|
| Kritz-Silverstein et al., 2017 [40] | PVF SVF | TMTB * | WL (10) MV | MV (30 min) | |||
| Fischer et al. 2016 [34] | DSB+ LNS + DEFS * | WL (16) | DWL (20 min) | ||||
| Cherbuin et al., 2015 [47] | PVF | DSB | SDMT TMTA TMTB | WL (16) P | DLW (20 min) P | ||
| Okusaga et al., 2013 [44] | VF | DSS TMTA | WL (15) + WL (20 min) * | RM | |||
| Dregan et al. 2013 [43] | SVF + LCT | WL (10) + DWL * | |||||
| Nation et al., 2010 [56] | WCST + TMTB + VF D + VF * | TMTA | HM + DHM + WL + DWL | BD | |||
| Whitfield et al., 2008 [41] | AF | DSS * | HM ** | HM (10 min) | |||
| Singh-Manoux, et al., 2005 [35] | PVF * SVF * | WL (20) | MR | ||||
| Robbins et al., 2005 [54] | DSB | DSS * | BD * ST * | ||||
| Waldstein, Giggey et al., 2005 [51] | PVF SVF * | DSB TMTBu | TMTAu | WL (16) + DWL * VM + DVM * | |||
| Hebert et al., 2004 [45] | SDMT + MMSE + EBMTu | - | |||||
| Ellias et al. 2004 [50] | DSS | Ar + DSB + DSF | PC + PA + BD + OA * | ||||
| Steward et al., 2003 [53] | TMT A | WL (10) | DWL (2 min) | ||||
| Izquierdo-Porrera & Waldstein, 2002 [33] | DSB | WL (10) | DWL (7 min) | CLOX | |||
| Morris et al., 2002 [32] | SDMTu | EBMTu | EBMTu | ||||
| Wei et al., 2018 [42] | TO + R7 + IC * | WL (10) + DWL (4 min) * | |||||
| Yeung et al.,2017 [52] | PVF SVF * | TMTB | DSS | SCW | WL (16) | DWL (20 min) | EPS * |
| Nguyen et al., 2017 [55] | WL (12) * | DWL (30 min) RCFd | RCFi * | ||||
| Hudak et al., 2013 [37] | TMTB * | TMTA * DSS * UFOV * LC * MC * | WL (12) | DWL (30 min) | |||
| Yasar et al., 2011 [38] | PVF + SVF+ | TMTB * | TMTA * | WL (12) * | DWL (20 min) | ||
| Bucur & Madden., 2010 [46] | TMTA-TMTB + SCW | DSS | |||||
| Brady et al., 2005 [39] | SVF | DSB | SC | WL (10) | DWL (5 min) | ||
| Waldstein, Brown et al., 2005 [31] | DSB TMTB * | TMTA * MSM * | SCW | HM VM * | DHM (30 min) DVM * (30 min) | ||
| Waldstein & Katzel, 2004 [36] | DSB VMSB * | MSM * | HM VM | DHM (30 min) DVM (30 min) | |||
| Saxby et al., 2003 [48] | TMTA + TMTB + SVF + PVF * | NWM * | RT * | WL (12) + DWL + RWL + DRWL * | |||
| Harrington et al., 2000 [49] | CDR | CDR |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sánchez-Nieto, J.M.; Rivera-Sánchez, U.D.; Mendoza-Núñez, V.M. Relationship between Arterial Hypertension with Cognitive Performance in Elderly. Systematic Review and Meta-Analysis. Brain Sci. 2021, 11, 1445. https://doi.org/10.3390/brainsci11111445
Sánchez-Nieto JM, Rivera-Sánchez UD, Mendoza-Núñez VM. Relationship between Arterial Hypertension with Cognitive Performance in Elderly. Systematic Review and Meta-Analysis. Brain Sciences. 2021; 11(11):1445. https://doi.org/10.3390/brainsci11111445
Chicago/Turabian StyleSánchez-Nieto, José Miguel, Uriel Dagoberto Rivera-Sánchez, and Víctor Manuel Mendoza-Núñez. 2021. "Relationship between Arterial Hypertension with Cognitive Performance in Elderly. Systematic Review and Meta-Analysis" Brain Sciences 11, no. 11: 1445. https://doi.org/10.3390/brainsci11111445
APA StyleSánchez-Nieto, J. M., Rivera-Sánchez, U. D., & Mendoza-Núñez, V. M. (2021). Relationship between Arterial Hypertension with Cognitive Performance in Elderly. Systematic Review and Meta-Analysis. Brain Sciences, 11(11), 1445. https://doi.org/10.3390/brainsci11111445






