Comparison of the Pullout Strength of Pedicle Screws According to the Thread Design for Various Degrees of Bone Quality
Abstract
:1. Introduction
2. Material and Method
2.1. Types of Pedicle Screw
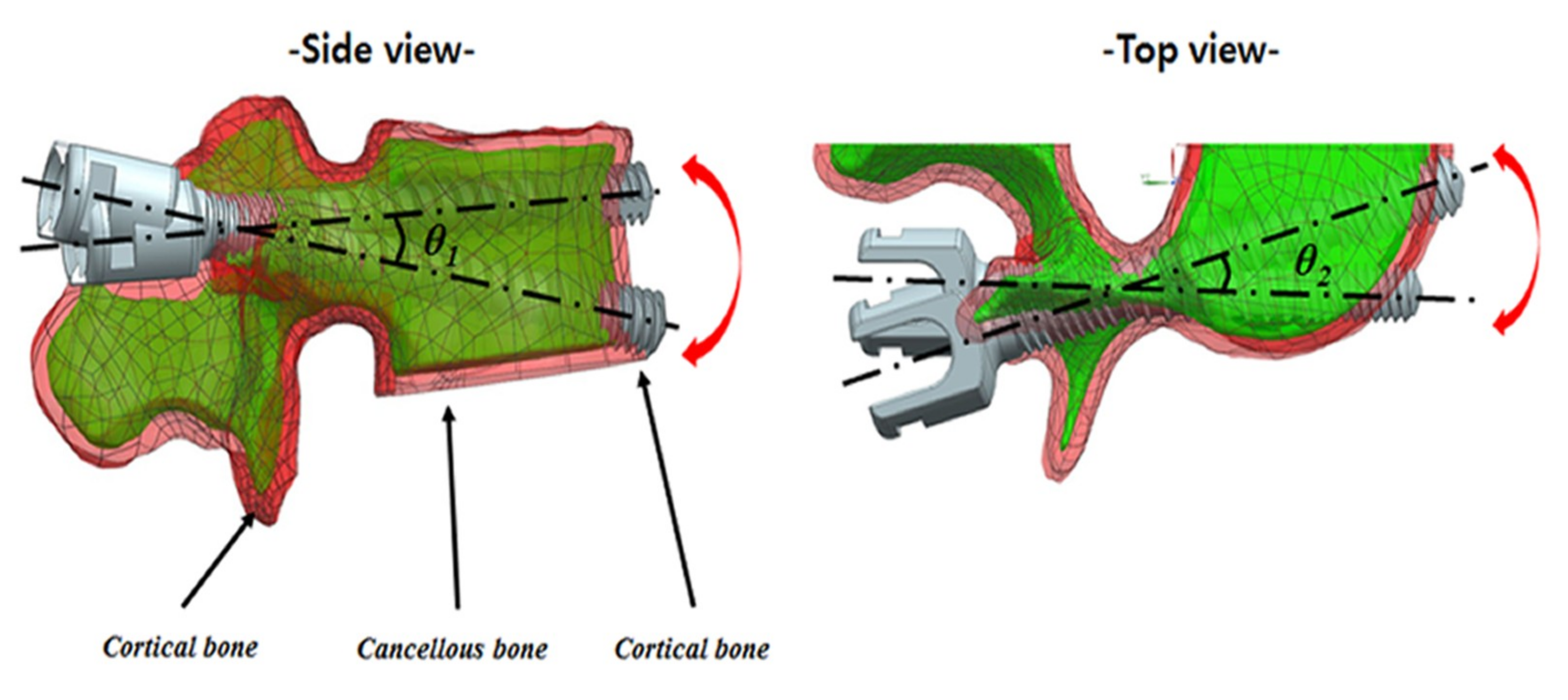
2.2. Preparation of Specimens
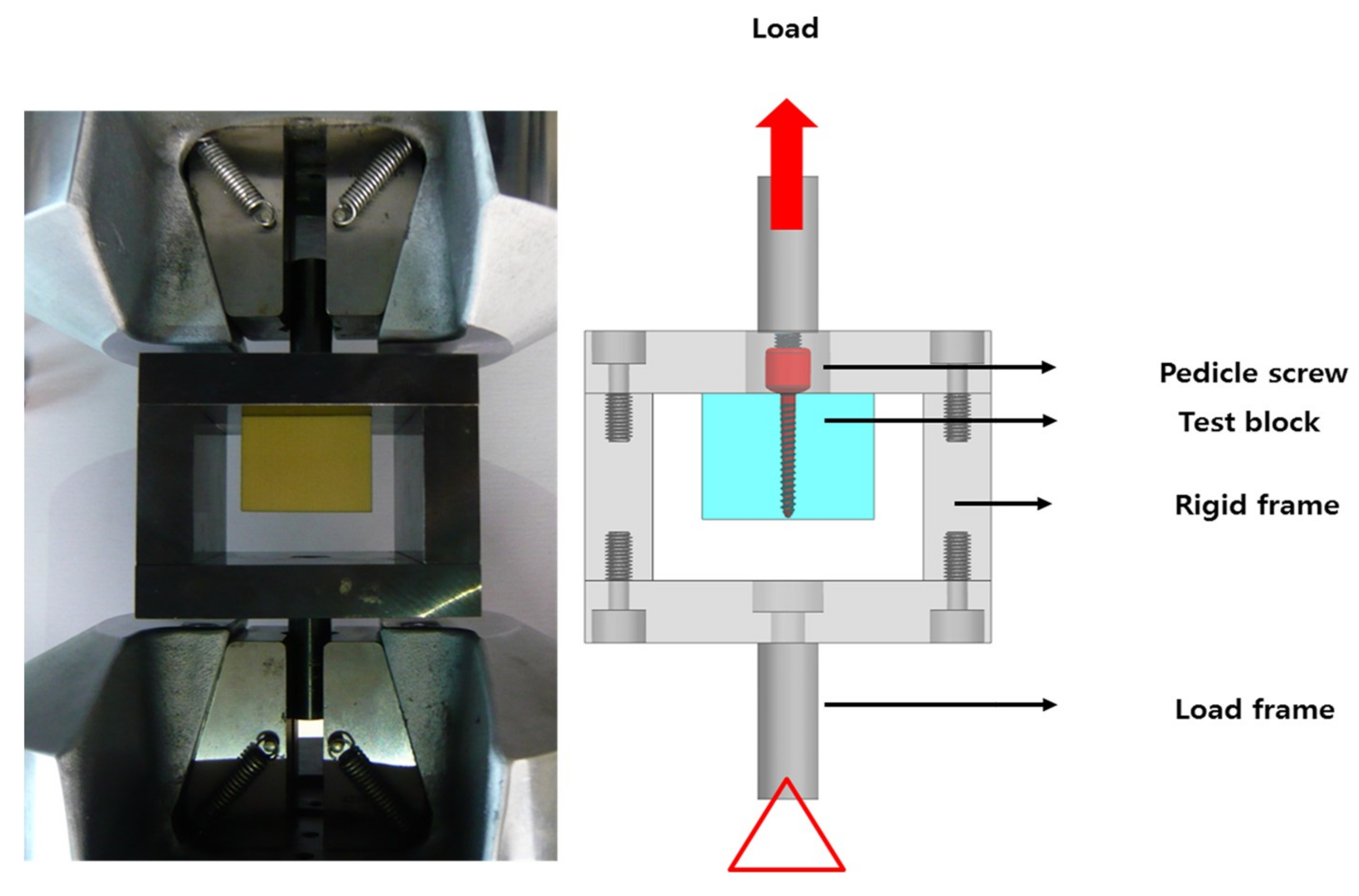
2.3. Test Apparatus
2.4. Biomechanical Testing Procedures
2.5. Statistical Analysis
3. Results
3.1. Comparison among Type I, Type II, and Type III Screws in Type A, B, C, and D Bone Specimens (in Normal and Osteoporotic Bone)
3.2. Comparison among Type I, Type II, and Type IV screws in Type C and E Bone Specimen (in Osteoporotic Bone with and without Bi-cortical Bone)
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Gertzbein, S.D.; Robbins, S.E. Accuracy of pedicular screw placement in vivo. Spine 1990, 15, 11–14. [Google Scholar] [CrossRef]
- Weinstein, J.N.; Rydevik, B.L.; Rauschning, W. Anatomic and technical considerations of pedicle screw fixation. Clin. Orthop. Relat. Res. 1992, 34–46. [Google Scholar] [CrossRef]
- Enker, P.; Steffee, A.D. Interbody fusion and instrumentation. Clin. Orthop. Relat. Res. 1994, 300, 90–101. [Google Scholar] [CrossRef]
- Baliga, S.; Treon, K.; Craig, N.J.A. Low Back Pain: Current Surgical Approaches. Asian Spine J. 2015, 9, 645–657. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.C.; Chao, C.K.; Wang, J.L.; Hou, S.M.; Tsai, Y.T.; Lin, J. Increase of pullout strength of spinal pedicle screws with conical core: Biomechanical tests and finite element analyses. J. Orthop. Res. 2005, 23, 788–794. [Google Scholar] [CrossRef]
- Krishnan, V.; Varghese, V.; Kumar, G.S. Comparative Analysis of Effect of Density, Insertion Angle and Reinsertion on Pull-Out Strength of Single and Two Pedicle Screw Constructs Using Synthetic Bone Model. Asian Spine J. 2016, 10, 414–421. [Google Scholar] [CrossRef]
- Serhan, H.; Slivka, M.; Albert, T.; Kwak, S.D.; Ibrahim, H.; Jahadakbar, A.; Dehghan, A.; Moghaddam, N.S.; Amerinatanzi, A.; Elahinia, M. Is galvanic corrosion between titanium alloy and stainless steel spinal implants a clinical concern? Spine J. 2004, 4, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, H.; Jahadakbar, A.; Dehghan, A.; Moghaddam, N.S.; Amerinatanzi, A.; Elahinia, M. In vitro corrosion assessment of additively manufactured porous NiTi structures for bone fixation applications. Metals 2018, 8, 164. [Google Scholar] [CrossRef]
- Ševčíková, J.; Bártková, D.; Goldbergová, M.; Kuběnová, M.; Čermák, J.; Frenzel, J.; Weiser, A.; Dlouhý, A. On the Ni-ion release rate from surfaces of binary NiTi shape memory alloys. Appl. Surf. Sci. 2018, 427, 434–443. [Google Scholar] [CrossRef]
- Tillmann, W.; Stangier, D.; Denkena, B.; Grove, T.; Lucas, H. Influence of PVD-coating technology and pretreatments on residual stresses for sheet-bulk metal forming tools. Prod. Eng. Res. Dev. 2016, 10, 17–24. [Google Scholar] [CrossRef]
- Ohe, M.; Moridaira, H.; Inami, S.; Takeuchi, D.; Nohara, Y.; Taneichi, H. Pedicle screws with a thin hydroxyapatite coating for improving fixation at the bone-implant interface in the osteoporotic spine: Experimental study in a porcine model. J. Neurosurg. Spine 2018, 28, 679–687. [Google Scholar] [CrossRef] [PubMed]
- Dehghanghadikolaei, A.; Ibrahim, H.; Amerinatanzi, A.; Hashemi, M.; Moghaddam, N.S.; Elahinia, M. Improving corrosion resistance of additively manufactured nickel–titanium biomedical devices by micro-arc oxidation process. J. Mater. Sci. 2019, 54, 7333–7355. [Google Scholar] [CrossRef]
- Shea, T.M.; Laun, J.; Gonzalez-Blohm, S.A.; Doulgeris, J.J.; Lee, W.E.; Aghayev, K.; Vrionis, F.D. Designs and techniques that improve the pullout strength of pedicle screws in osteoporotic vertebrae: Current status. Biomed Res Int. 2014, 2014, 748393. [Google Scholar] [CrossRef]
- Bianco, R.J.; Arnoux, P.J.; Wagnac, E.; Mac-Thiong, J.M.; Aubin, C.É. Minimizing pedicle screw pullout risks: A detailed biomechanical analysis of screw design and placement. Clin Spine Surg. 2017, 30, E226–E232. [Google Scholar] [CrossRef] [PubMed]
- Brasiliense, L.B.; Lazaro, B.C.; Reyes, P.M.; Newcomb, A.G.; Turner, J.L.; Crandall, D.G.; Crawford, N.R. Characteristics of immediate and fatigue strength of a dual-threaded pedicle screw in cadaveric spines. Spine J. 2013, 13, 947–956. [Google Scholar] [CrossRef]
- ASTM International. Standard Specification for Rigid Polyurethane Foam for Use as a Standard Material for Testing Orthopedic Devices and Instrument; ASTM F1839-01; ASTM International: West Conshohocken, PA, USA, 2001. [Google Scholar]
- Kim, Y.-Y.; Choi, W.-S.; Rhyu, K.-W. Assessment of pedicle screw pullout strength based on various screw designs and bone densities-an ex vivo biomechanical study. Spine J. 2012, 12, 164–168. [Google Scholar] [CrossRef]
- ASTM International. Standard Specification and Test Methods for Metallic Medical Bone Screws; ASTM F543-13; ASTM International: West Conshohocken, PA, USA, 2013. [Google Scholar]
- Abshire, B.B.; McLain, R.F.; Valdevit, A.; Kambic, H.E. Characteristics of pullout failure in conical and cylindrical pedicle screws after full insertion and back-out. Spine J. 2001, 1, 408–414. [Google Scholar] [CrossRef]
- Ono, A.; Brown, M.D.; Latta, L.L.; Milne, E.L.; Holmes, D.C. Triangulated pedicle screw construct technique and pull-out strength of conical and cylindrical screws. J. Spinal. Disord. 2001, 14, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Chapman, J.R.; Harrington, R.M.; Lee, K.M.; Anderson, P.A.; Tencer, A.F.; Kowalski, D. Factors affecting the pullout strength of cancellous bone screws. J. Biomech. Eng. 1996, 118, 391–398. [Google Scholar] [CrossRef]
- Inceoglu, S.; Ferrara, L.; McLain, R.F. Pedicle screw fixation strength: Pullout versus insertional torque. Spine J. 2004, 4, 513–518. [Google Scholar] [CrossRef]
- Krenn, M.H.; Piotrowski, W.P.; Penzkofer, R.; Augat, P. Influence of thread design on pedicle screw fixation. Laboratory investigation. J. Neurosurg. Spine 2008, 9, 90–95. [Google Scholar] [CrossRef]
- Santoni, B.G.; Hynes, R.A.; McGilvray, K.C.; Rodriguez-Canessa, G.; Lyons, A.S.; Henson, M.A.; et al. Cortical bone trajectory for lumbar pedicle screws. Spine J. 2009, 9, 366–373. [Google Scholar] [CrossRef]
- Dehghanghadikolaei, A.; Ansary, J.; Ghoreishi, R. Sol-gel process applications: A mini-review. Proc. Natl. Res. Soc. 2018, 2, 02008. [Google Scholar] [CrossRef]
- Spicher, A.; Lindtner, R.A.; Zimmermann, S.; Stofferin, H.; Schmoelz, W. Ultrasound melted polymer sleeve for improved primary pedicle screw anchorage: A novel augmentation technique. Clin. Biomech. 2019, 63, 16–20. [Google Scholar] [CrossRef]
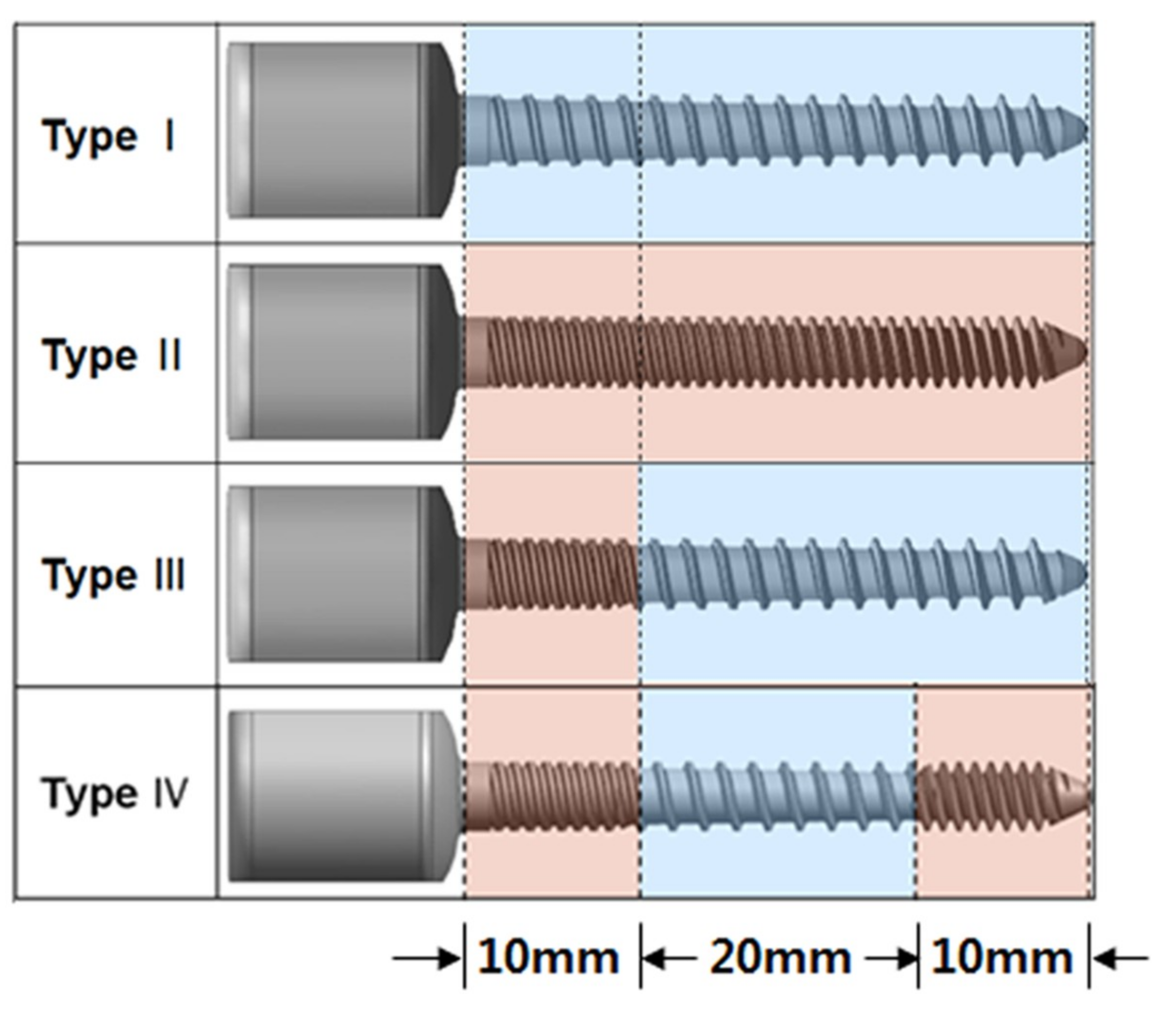



| Screw Type | Length (mm) | Outer Diameter (mm) | Proximal Core Diameter (mm) | Distal Core Diameter (mm) | Proximal Thread Width (mm) | Distal Thread Width (mm) | Pitch (mm) | ||
|---|---|---|---|---|---|---|---|---|---|
| Proximal 1/4 | Middle | Distal 1/4 | |||||||
| Type I | 40 | 4.5 | 4.0 | 2.7 | 0.4 | 0 | 2 | 2 | 2 |
| Type II | 40 | 4.5 | 4.0 | 2.7 | 0.4 | 0 | 1 | 1 | 1 |
| Type III | 40 | 4.5 | 4.0 | 2.7 | 0.4 | 0 | 1 | 2 | 2 |
| Type IV | 40 | 4.5 | 4.0 | 2.7 | 0.4 | 0 | 1 | 2 | 1 |
| Bone Specimens | Screw Types | |||
|---|---|---|---|---|
| Type I (KN) | Type II (KN) | Type III (KN) | Type IV (KN) | |
| Type A | 2.23 ± 0.07 | 2.38 ± 0.18 | 2.28 ± 0.13 | |
| Type B | 2.65 ± 0.16 | 2.87 ± 0.13 | 2.80 ± 0.08 | |
| Type C | 1.56 ± 0.23 | 1.26 ± 0.06 | 1.32 ± 0.13 | 0.98 ± 0.15 |
| Type D | 1.99 ± 0.11 | 1.80 ± 0.14 | 1.82 ± 0.09 | |
| Type E | 2.54 ± 0.15 | 2.68 ± 0.14 | 2.67 ± 0.07 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shen, F.; Kim, H.-J.; Kang, K.-T.; Yeom, J.S. Comparison of the Pullout Strength of Pedicle Screws According to the Thread Design for Various Degrees of Bone Quality. Appl. Sci. 2019, 9, 1525. https://doi.org/10.3390/app9081525
Shen F, Kim H-J, Kang K-T, Yeom JS. Comparison of the Pullout Strength of Pedicle Screws According to the Thread Design for Various Degrees of Bone Quality. Applied Sciences. 2019; 9(8):1525. https://doi.org/10.3390/app9081525
Chicago/Turabian StyleShen, Feng, Ho-Joong Kim, Kyoung-Tak Kang, and Jin S. Yeom. 2019. "Comparison of the Pullout Strength of Pedicle Screws According to the Thread Design for Various Degrees of Bone Quality" Applied Sciences 9, no. 8: 1525. https://doi.org/10.3390/app9081525
APA StyleShen, F., Kim, H.-J., Kang, K.-T., & Yeom, J. S. (2019). Comparison of the Pullout Strength of Pedicle Screws According to the Thread Design for Various Degrees of Bone Quality. Applied Sciences, 9(8), 1525. https://doi.org/10.3390/app9081525





