The Effect on Bone Stress in Oral Prosthetic Rehabilitation Supported by Different Number of Dental Implants: A Numerical Analysis
Abstract
:1. Introduction
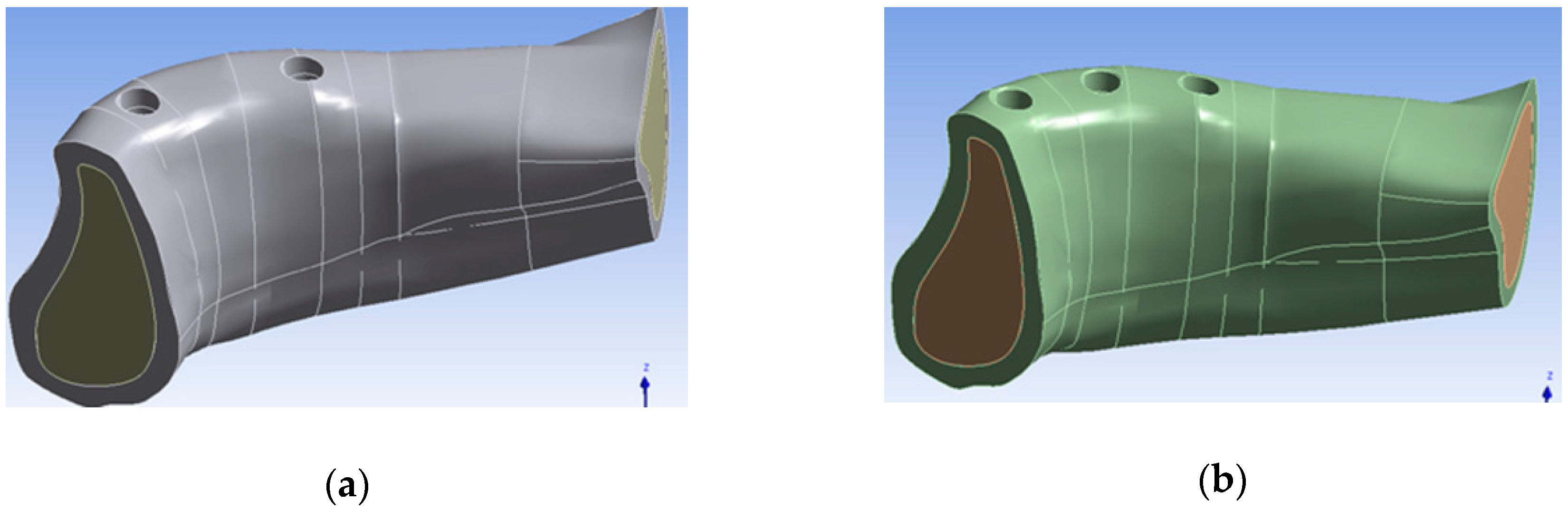
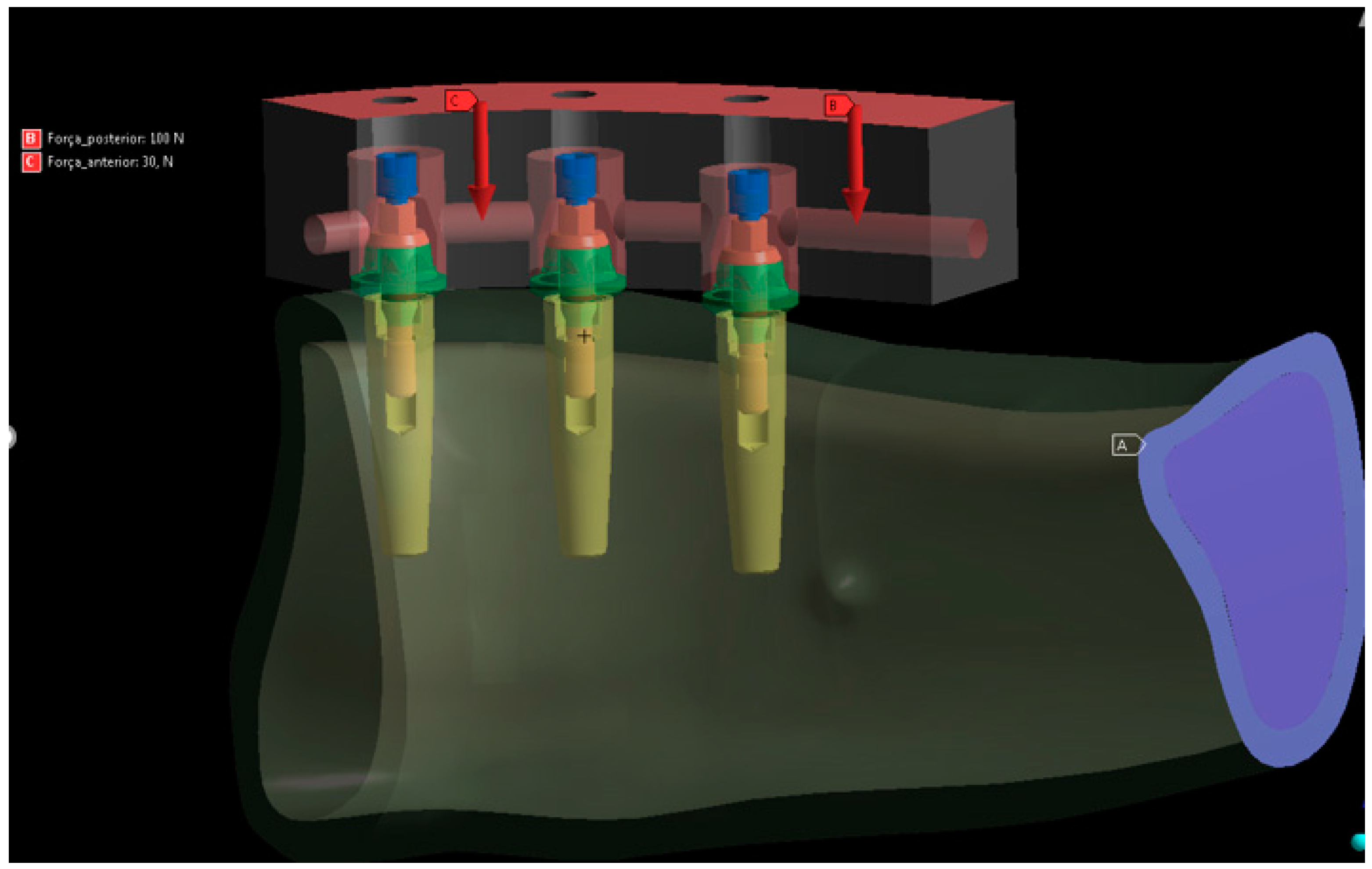
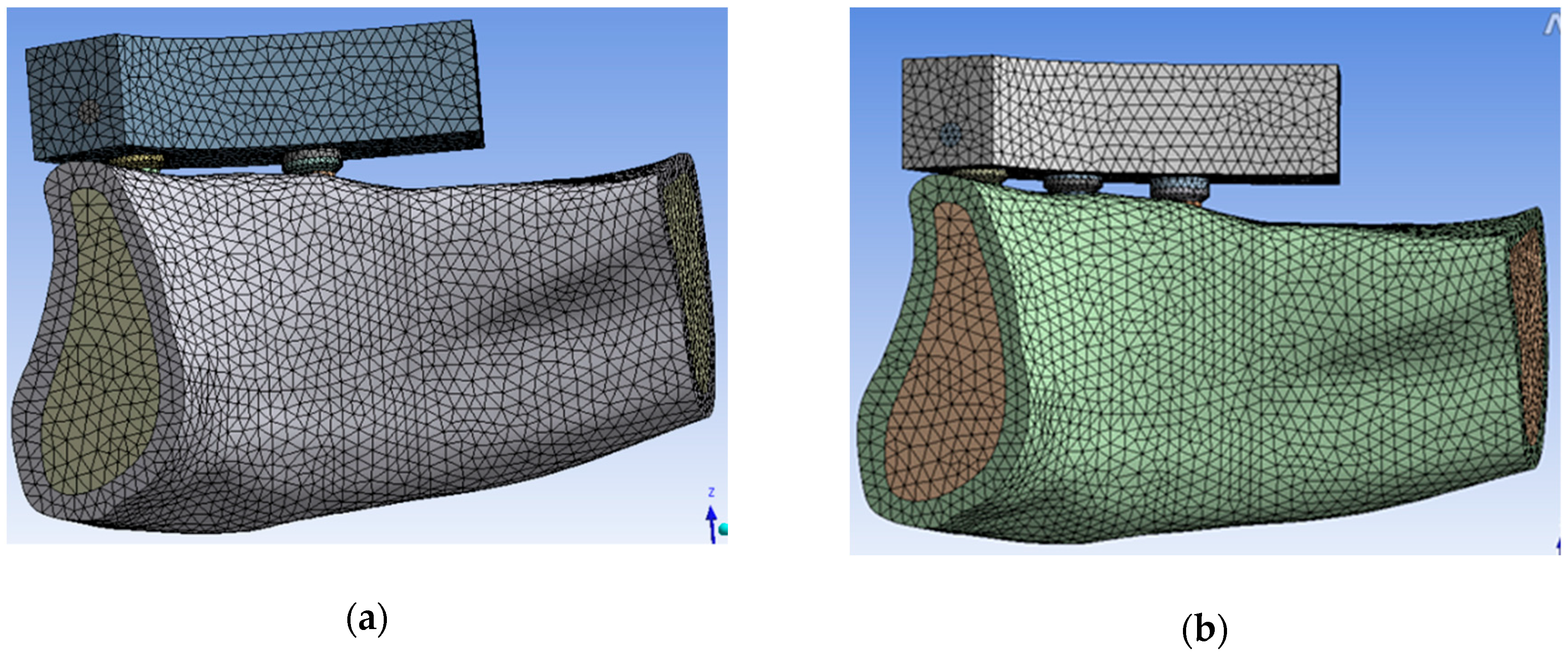
2. Materials and Methods
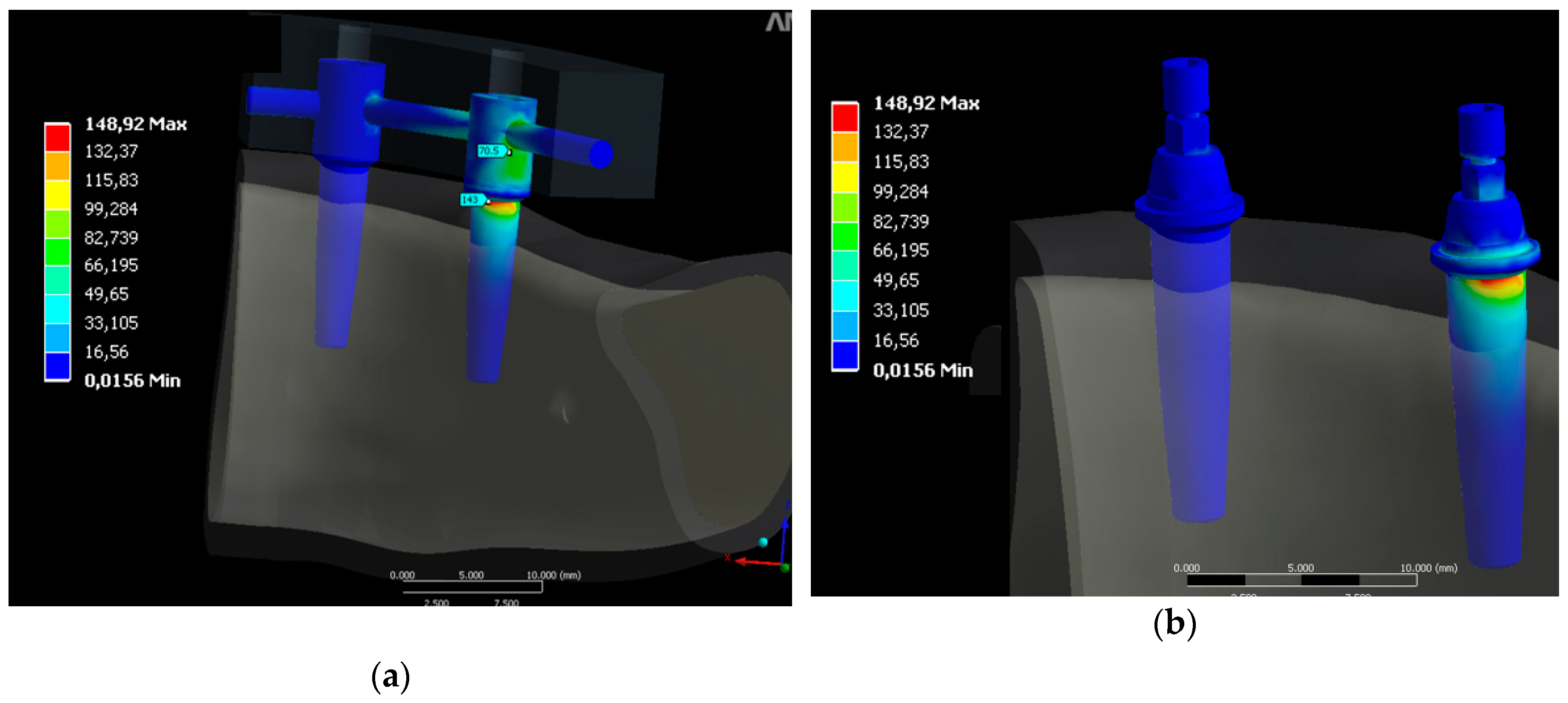
3. Results
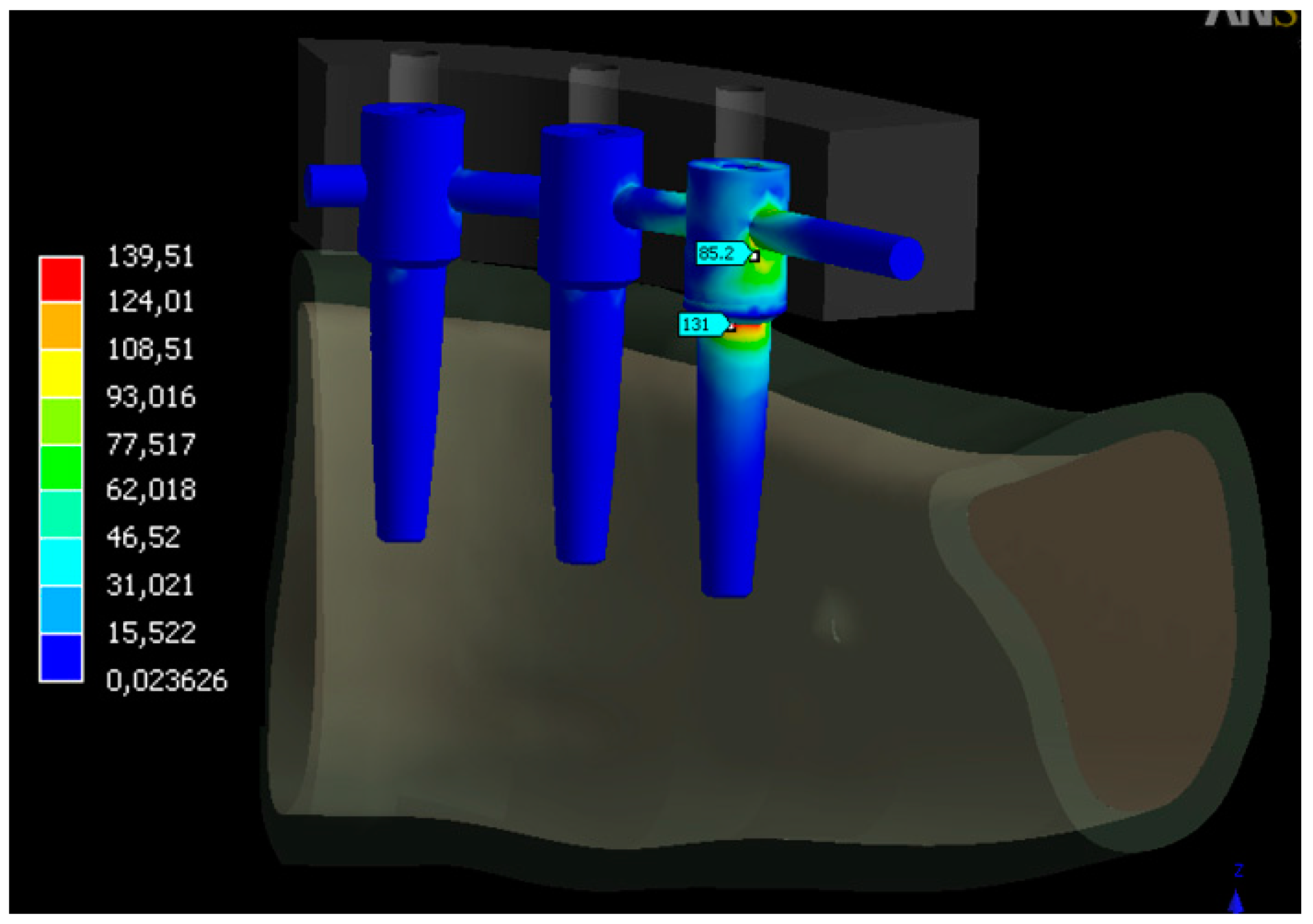
3.1. Distribution Stress in Dental Implants
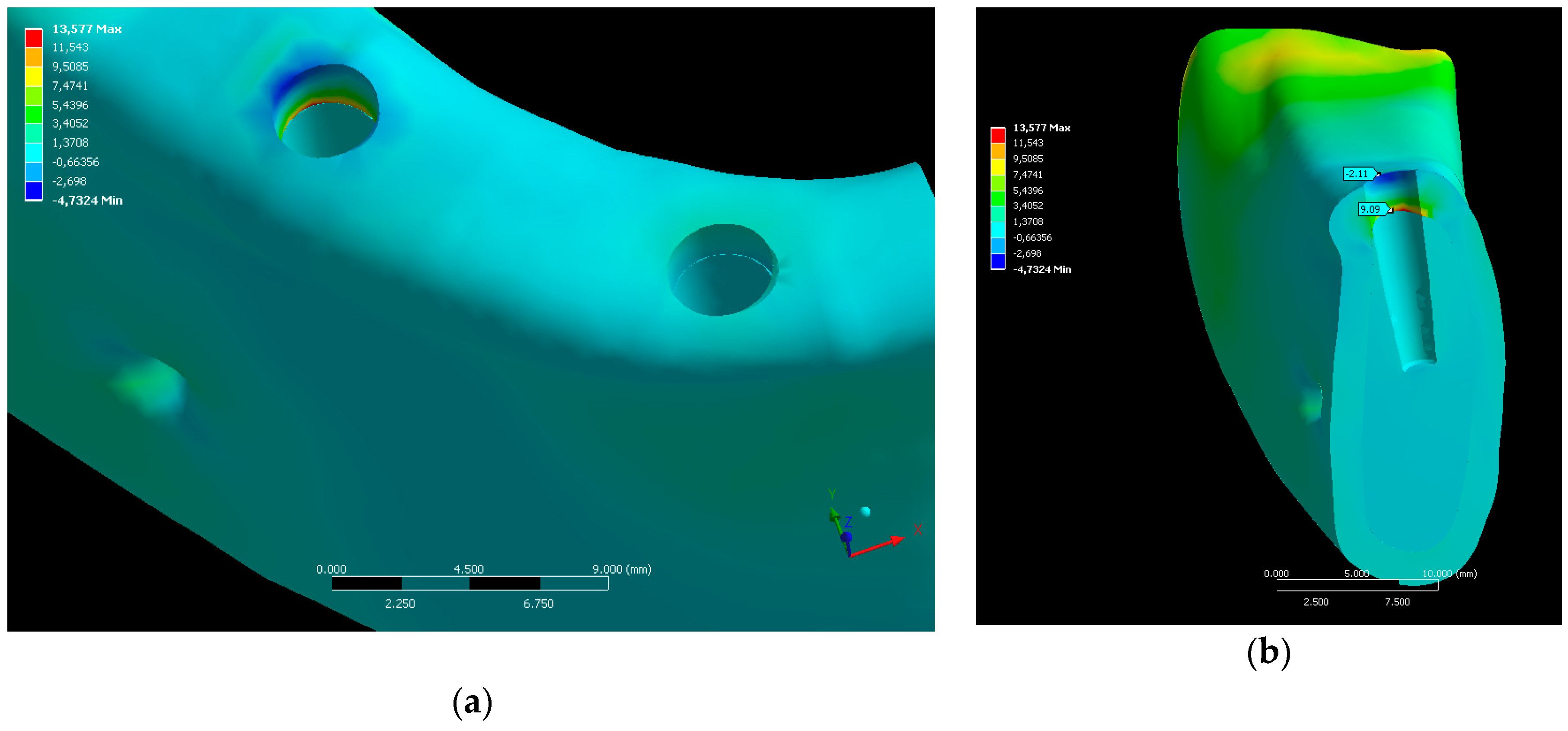
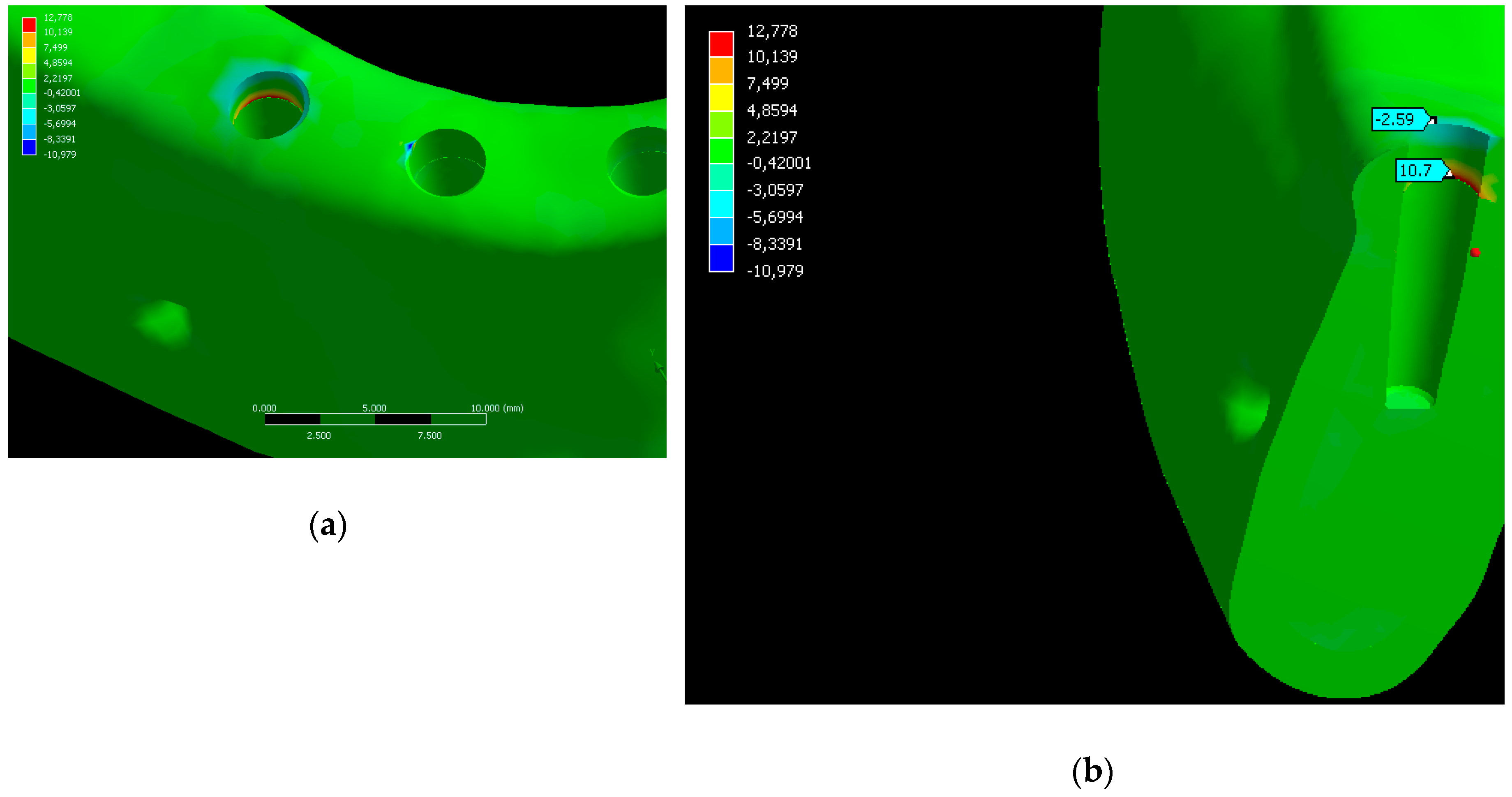
3.2. Distribution Stress in Bone
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Siadat, H.; Rokn, A.; Beyabanaki, E. Full Arch All-on-4 Fixed Implant-Supported Prostheses with 8.5 Years of Follow-Up: A Case Report. J. Dent. (Tehran) 2018, 15, 259–265. [Google Scholar]
- Maló, P.; Araújo Nobre, M.; Lopes, A.; Ferro, A.; Botto, J. The All-on-4 treatment concept for the rehabilitation of the completely edentulous mandible: A longitudinal study with 10 to 18 years of follow-up. Clin. Implant. Dent. Relat. Res. 2019, 21, 565–577. [Google Scholar] [CrossRef] [PubMed]
- Falisi, G. “All on short” prosthetic-implant supported rehabilitations. Oral Implant. (Rome) 2017, 10, 477. [Google Scholar] [CrossRef] [PubMed]
- Chowdhary, R.; Kumararama, S.S. “Simpli5y” a noval concept for fixed rehabilitation of completely edentulous maxillary and mandibular edentulous arches: A 3-year randomized clinical trial, supported by a numerical analysis. Clin. Implant. Dent. Relat. Res. 2018, 20, 749–755. [Google Scholar] [CrossRef] [PubMed]
- Toniollo, M.B.; Vieira, L.J.P.; dos Santos Sá, M.; Macedo, A.P.; de Melo, J.P.; Terada, A.S.S.D. Stress distribution of three-unit fixed partial prostheses (conventional and pontic) supported by three or two implants: 3D finite element analysis of ductile materials. Comput. Methods Biomech. Biomed. Eng. 2019, 22, 706–712. [Google Scholar] [CrossRef] [PubMed]
- Rubo, J.H.; Souza, E.A.C. Finite element analysis of stress in bone adjacent to dental implants. J. Oral Implant. 2008, 34, 248–255. [Google Scholar] [CrossRef]
- Sánchez Lasheras, F.; Gracia Rodríguez, J.; Mauvezín-Quevedo, M.; Martín-Fernández, E.; Bobes-Bascarán, J.; Llanos-Lanchares, H.; Álvarez-Arenal, Á. Does the transversal screw design increase the risk of mechanical complications in dental implants? A finite elements analysis. Int. J. Numer. Method Biomed. Eng. 2019, 35, e3205. [Google Scholar] [CrossRef]
- Kitamura, E.; Stegaroiu, R.; Nomura, S.; Miyakawa, O. Biomechanical aspects of marginal bone resorption around osseointegrated implants: Considerations based on a three-dimensional finite element analysis. Clin. Oral Implant. Res. 2004, 15, 401–412. [Google Scholar] [CrossRef]
- Hanaoka, M.; Gehrke, S.A.; Mardegan, F.; Gennari, C.R.; Taschieri, S.; Del Fabbro, M.; Corbella, S. Influence of Implant/Abutment Connection on Stress Distribution to Implant-Surrounding Bone: A Finite Element Analysis. J. Prosthodont. 2014, 23, 565–571. [Google Scholar] [CrossRef]
- Pellizzer, E.P.; Lemos, C.A.A.; Almeida, D.A.F.; de Souza Batista, V.E.; Santiago Júnior, J.F.; Verri, F.R. Biomechanical analysis of different implant-abutments interfaces in different bone types: An in silico analysis. Mater. Sci. Eng. C 2018, 90, 645–650. [Google Scholar] [CrossRef]
- Rubo, J.H.; Capello Souza, E.A. Finite-Element Analysis of Stress on Dental Implant Prosthesis. Clin. Implant. Dent. Relat. Res. 2009, 12, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Solberg, K.; Heinemann, F.; Pellikaan, P.; Keilig, L.; Stark, H.; Bourauel, C.; Hasan, I. Finite element analysis of different loading conditions for implant-supported overdentures supported by conventional or mini implants. Comput. Methods Biomech. Biomed. Eng. 2017, 20, 770–782. [Google Scholar] [CrossRef] [PubMed]
- Raaj, G.; Manimaran, P.; Kumar, C.D.; Sadan, D.S.; Abirami, M. Comparative Evaluation of Implant Designs: Influence of Diameter, Length, and Taper on Stress and Strain in the Mandibular Segment-A Three-Dimensional Finite Element Analysis. J. Pharm. Bioallied Sci. 2019, 11, S347–S354. [Google Scholar] [CrossRef] [PubMed]
- Zieliński, R.; Kozakiewicz, M.; Świniarski, J. Comparison of Titanium and Bioresorbable Plates in “A” Shape Plate Properties-Finite Element Analysis. Materials (Basel) 2019, 12, 1110. [Google Scholar] [CrossRef]
- Pjetursson, B.E.; Valente, N.A.; Strasding, M.; Zwahlen, M.; Liu, S.; Sailer, I. A systematic review of the survival and complication rates of zirconia-ceramic and metal-ceramic single crowns. Clin. Oral Implant. Res. 2018, 29, 199–214. [Google Scholar] [CrossRef]
- Meijer, H.J.; Kuiper, J.H.; Starmans, F.J.; Bosman, F. Stress distribution around dental implants: Influence of superstructure, length of implants, and height of mandible. J. Prosthet. Dent. 1992, 68, 96–102. [Google Scholar] [CrossRef]
- Iplikçioğlu, H.; Akça, K. Comparative evaluation of the effect of diameter, length and number of implants supporting three-unit fixed partial prostheses on stress distribution in the bone. J. Dent. 2002, 30, 41–46. [Google Scholar] [CrossRef]
- Cağlar, A.; Aydin, C.; Ozen, J.; Yilmaz, C.; Korkmaz, T. Effects of mesiodistal inclination of implants on stress distribution in implant-supported fixed prostheses. Int. J. Oral Maxillofac. Implant. 2006, 21, 36–44. [Google Scholar]
- Bahadirli, G.; Yilmaz, S.; Jones, T.; Sen, D. Influences of Implant and Framework Materials on Stress Distribution: A Three-Dimensional Finite Element Analysis Study. Int. J. Oral Maxillofac. Implant. 2018, 33, e117–e126. [Google Scholar] [CrossRef]
- Baggi, L.; Cappelloni, I.; Di Girolamo, M.; Maceri, F.; Vairo, G. The influence of implant diameter and length on stress distribution of osseointegrated implants related to crestal bone geometry: A three-dimensional finite element analysis. J. Prosthet. Dent. 2008, 100, 422–431. [Google Scholar] [CrossRef]
- Silva, G.C.; Mendonça, J.A.; Lopes, L.R.; Landre, J. Stress patterns on implants in prostheses supported by four or six implants: A three-dimensional finite element analysis. Int. J. Oral Maxillofac. Implant. 2010, 25, 239–246. [Google Scholar]
- Semper, W.; Heberer, S.; Nelson, K. Retrospective analysis of bar-retained dentures with cantilever extension: Marginal bone level changes around dental implants over time. Int. J. Oral Maxillofac. Implant. 2010, 25, 385–393. [Google Scholar]
- Hingsammer, L.; Pommer, B.; Hunger, S.; Stehrer, R.; Watzek, G.; Insua, A. Influence of Implant Length and Associated Parameters Upon Biomechanical Forces in Finite Element Analyses. Implant. Dent. 2019, 28, 296–305. [Google Scholar] [CrossRef] [PubMed]
- Duyck, J.; Van Oosterwyck, H.; Vander Sloten, J.; De Cooman, M.; Puers, R.; Naert, I. Magnitude and distribution of occlusal forces on oral implants supporting fixed prostheses: An in vivo study. Clin. Oral Implant. Res. 2000, 11, 465–475. [Google Scholar] [CrossRef] [PubMed]
- Davis, D.M.; Zarb, G.A.; Chao, Y.L. Studies on frameworks for osseointegrated prostheses: Part 1. The effect of varying the number of supporting abutments. Int. J. Oral Maxillofac. Implant. 1988, 3, 197–201. [Google Scholar]
- Greco, G.D.; Jansen, W.C.; Landre Junior, J.; Seraidarian, P.I. Stress analysis on the free-end distal extension of an implant-supported mandibular complete denture. Braz. Oral Res. 2009, 23, 182–189. [Google Scholar] [CrossRef]
- Ogawa, T.; Dhaliwal, S.; Naert, I.; Mine, A.; Kronstrom, M.; Sasaki, K.; Duyck, J. Impact of implant number, distribution and prosthesis material on loading on implants supporting fixed prostheses. J. Oral Rehabil. 2010, 37, 525–531. [Google Scholar] [CrossRef]
- Jemt, T. Failures and complications in 391 consecutively inserted fixed prostheses supported by Brånemark implants in edentulous jaws: A study of treatment from the time of prosthesis placement to the first annual checkup. Int. J. Oral Maxillofac. Implant. 1991, 6, 270–276. [Google Scholar]
- Eliasson, A.; Palmqvist, S.; Svenson, B.; Sondell, K. Five-year results with fixed complete-arch mandibular prostheses supported by 4 implants. Int. J. Oral Maxillofac. Implant. 2010, 15, 505–510. [Google Scholar]
- Box, V.H.; Sukotjo, C.; Knoernschild, K.L.; Campbell, S.D.; Afshari, F.S. Patient-Reported and Clinical Outcomes of Implant-Supported Fixed Complete Dental Prostheses: A Comparison of Metal-Acrylic, Milled Zirconia, and Retrievable Crown Prostheses. J. Oral Implant. 2018, 44, 51–61. [Google Scholar] [CrossRef]
- Scribante, A.; Vallittu, P.K.; Özcan, M. Fiber-Reinforced Composites for Dental Applications. Biomed. Res. Int. 2018, 2018, 1–2. [Google Scholar] [CrossRef] [PubMed]

| Component | Poisson’s Ratio | Young’s Module [GPa] |
|---|---|---|
| Cortical bone | 0.3 | 14.7 |
| Trabecular bone | 0.3 | 0.49 |
| Implants and abutments (titanium alloy) | 0.33 | 117 |
| Acrylic | 0.3 | 3.8 |
| Bar | 0.33 | 205 |
| Distal Section of the Distal Implant (MPa) | Screw (MPa) | Abutment (MPa) | Implant/Abutment Contact (MPa) | |
|---|---|---|---|---|
| M1 group | 148.92 | 22.0 | 22.2 | 51.1 |
| M2 group | 139.51 | 19.9 | 23.9 | 46 |
| Difference between models | 6.74% | 10.55% | 7.65% | 11.08% |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prados-Privado, M.; Gehrke, S.A.; Tozaki, L.K.; Zanatta, L.C.S.; Cruz, P.; Mazon, P.; De Aza, P.N.; Prados-Frutos, J.C. The Effect on Bone Stress in Oral Prosthetic Rehabilitation Supported by Different Number of Dental Implants: A Numerical Analysis. Appl. Sci. 2019, 9, 4920. https://doi.org/10.3390/app9224920
Prados-Privado M, Gehrke SA, Tozaki LK, Zanatta LCS, Cruz P, Mazon P, De Aza PN, Prados-Frutos JC. The Effect on Bone Stress in Oral Prosthetic Rehabilitation Supported by Different Number of Dental Implants: A Numerical Analysis. Applied Sciences. 2019; 9(22):4920. https://doi.org/10.3390/app9224920
Chicago/Turabian StylePrados-Privado, María, Sergio A. Gehrke, Lúcia Kurokawa Tozaki, Luiz Carlos Silveira Zanatta, Paulo Cruz, Patricia Mazon, Piedad N. De Aza, and Juan Carlos Prados-Frutos. 2019. "The Effect on Bone Stress in Oral Prosthetic Rehabilitation Supported by Different Number of Dental Implants: A Numerical Analysis" Applied Sciences 9, no. 22: 4920. https://doi.org/10.3390/app9224920
APA StylePrados-Privado, M., Gehrke, S. A., Tozaki, L. K., Zanatta, L. C. S., Cruz, P., Mazon, P., De Aza, P. N., & Prados-Frutos, J. C. (2019). The Effect on Bone Stress in Oral Prosthetic Rehabilitation Supported by Different Number of Dental Implants: A Numerical Analysis. Applied Sciences, 9(22), 4920. https://doi.org/10.3390/app9224920








