3D Soft-Tissue Prediction Methodologies for Orthognathic Surgery—A Literature Review
Abstract
1. Introduction
2. Materials and Methods
3. Results
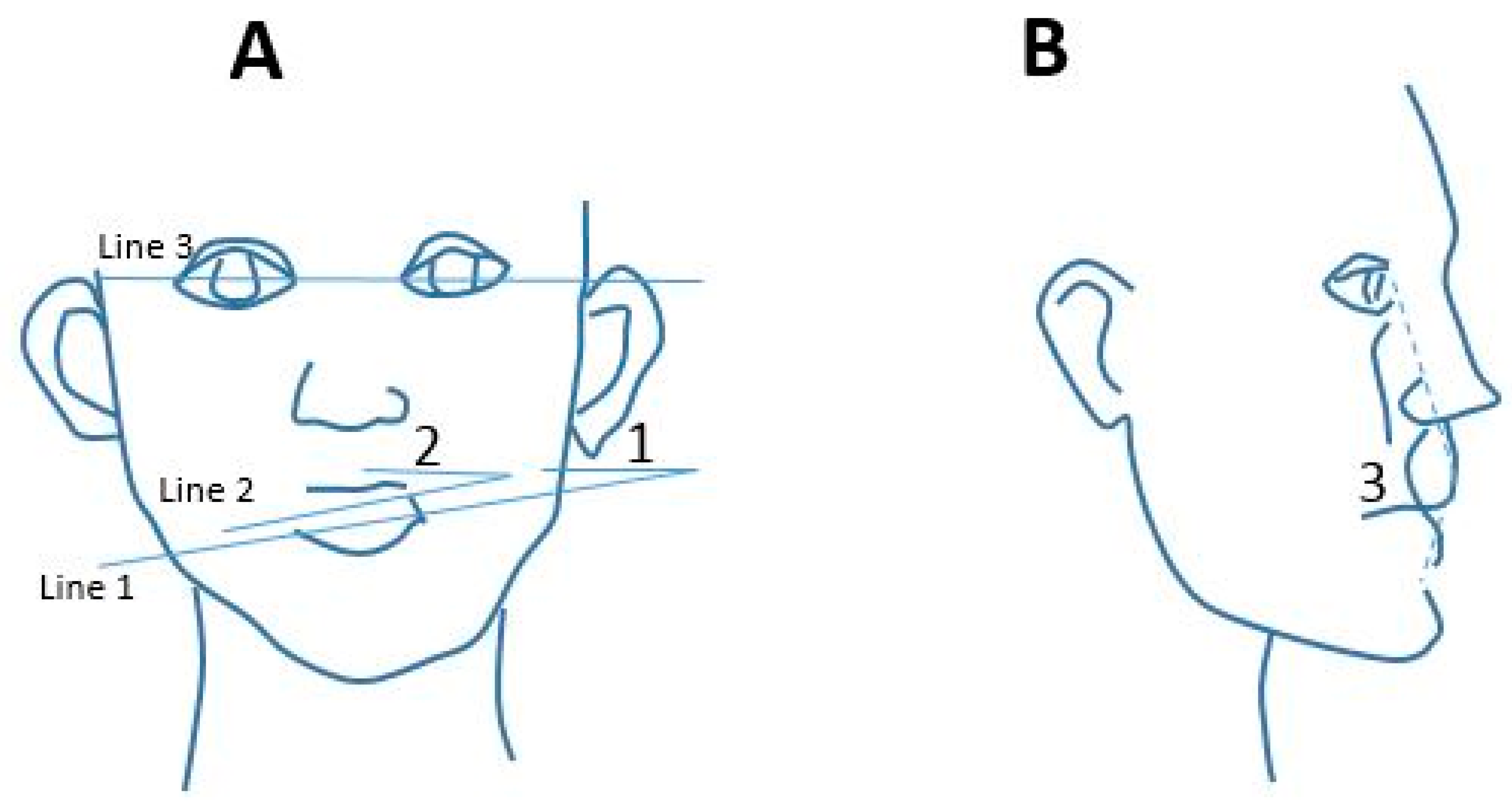
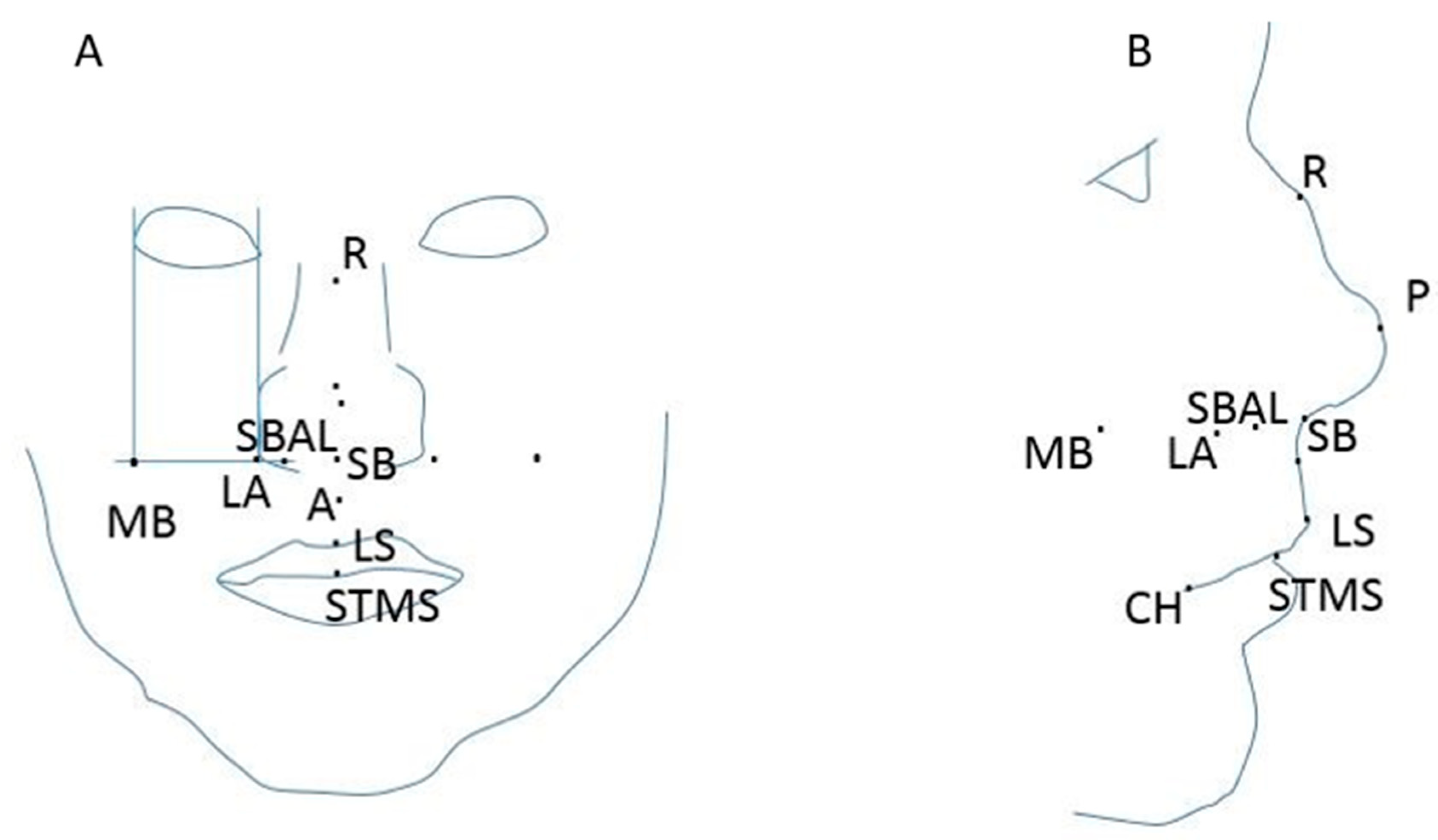
3.1. Clinincal Details
3.2. Prediction Methodologies
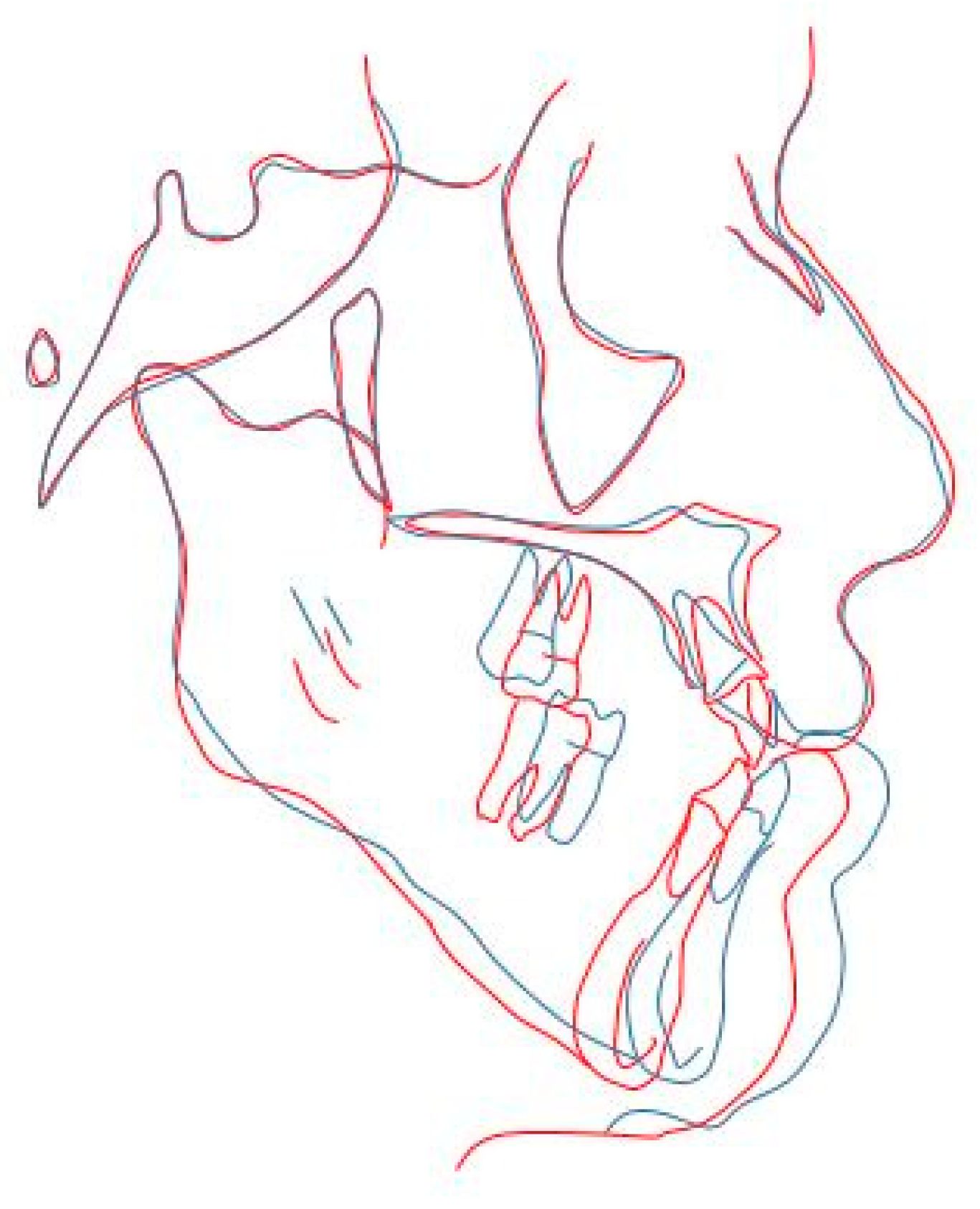
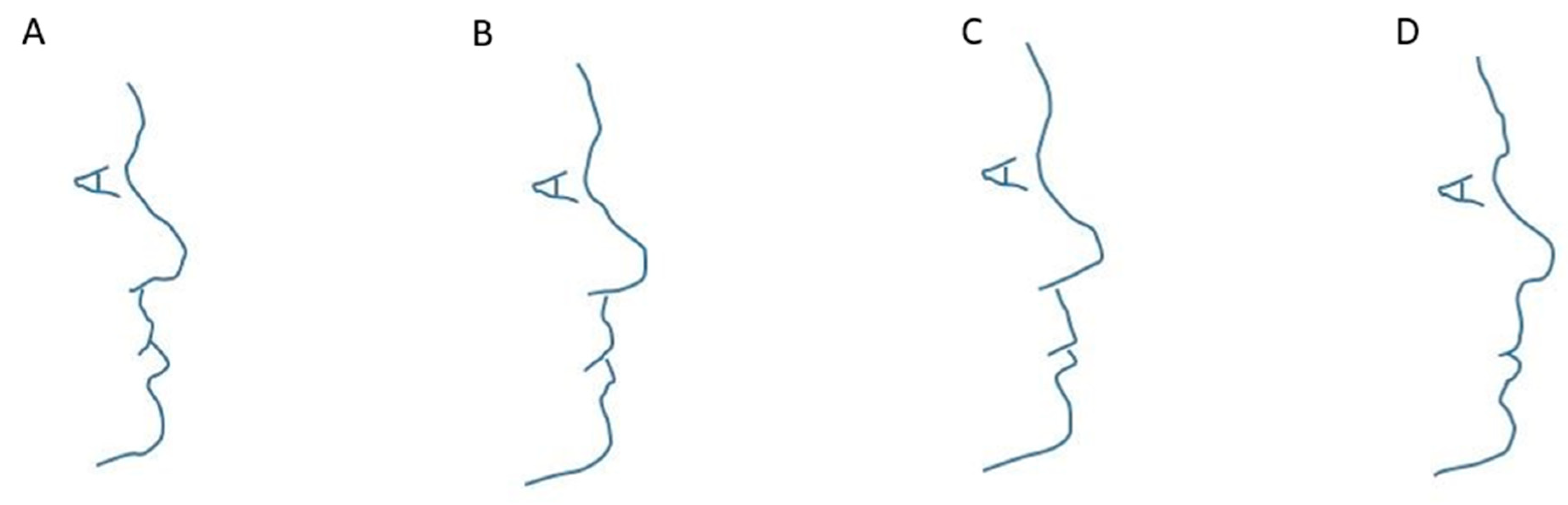
3.2.1. Works Based on Traditional (2D) Methodologies
3.2.2. Works Based on Maxilim Software (3D)
3.2.3. Works Based on Other 3D Software
4. Discussion and Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bruce, V. Applied Research in face Processing. In The Oxford Handbook of Face Perception; Oxford University Press: New York, NY, USA, 2011; pp. 131–146. [Google Scholar]
- Eckardt, C.; Cunningham, S. How predictable is orthognathic surgery? Eur. J. Orthod. 2004, 26, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Jo, L.-J.; Weng, J.-L.; Ho, C.-T.; Lin, H.-H. Three-dimensional region-based study on the relationship between soft and hard tissue changes after orthognatic surgery in patients with prognathism. PLoS ONE 2018, 13, e0200589. [Google Scholar]
- Suh, H.-Y.; Lee, H.-J.; Lee, Y.-S.; Eo, S.-H.; Donatelli, R.; Lee, S.-J. Predicting soft tissue changes after orthognatic surgery: The sparse partial least squares method. Ang. Orthod. 2019, 89, 910–916. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Chun-Yu Ho, D.; Mai, H.; Zhang, X.; Shen, S.G.F.; Shen, S.; Yuan, P.; Liu, S.; Zhang, G.; Zhou, X.; et al. A clinically validated simulation method for facial soft tissue change prediction following double jaw orthognatic surgery. Med. Phys. 2017, 44, 4252–4261. [Google Scholar] [CrossRef]
- Knoops, P.; Borghi, A.; Ruggiero, F.; Badiali, G.; Bianchi, A.; Marchetti, C.; Rodriguez-Flores, N.; Breakey, R.; Jeelani, O.; Dunaway, D.; et al. A novel soft tissue prediction methodology for orthognatic surgery based on probabilistic finite alament modelling. PLoS ONE 2018, 13, e0197209. [Google Scholar] [CrossRef]
- Swennen, G.; Schutyser, F.; Barth, E.; de Groeve, P.; de Mey, A. A new method of 3D cephalometery part I: The anatomic cartesian 3D reference system. J. Craniofac. Surg. 2006, 17, 314–325. [Google Scholar] [CrossRef]
- Van Twisk, P.-H.; Tenhagen, M.; Gul, A.W.E.; Kuonstaal, M. How accurate is the soft tissue prediction of Dolphin Imaging for orthognatic surgery? Int. Orthod. 2019, 17, 488–496. [Google Scholar] [CrossRef]
- Rustemeyer, J.; Groddeck, A.; Zwerger, S.; Bremerich, A. The accuracy of two-dimensional planning for routine orthognatic surgery. Br. J. Oral Maxillofac. Surg. 2010, 48, 271–275. [Google Scholar] [CrossRef]
- Peterman, R.; Jiang, S.; Johe, R.; Mukherjee, P. Accuracy of Dolphin visual treatment objective (VTO) patients treated with maxillary advancement and mandibular set back. Prog. Orthod. 2016, 17, 17–19. [Google Scholar] [CrossRef]
- Pektas, Z.; Kircelli, B.; Cilasun, U.; Uckan, S. The accuracy of computer assisted surgical planning in soft tissue prediction following orthognathic surgery. Int. J. Med. Robot. Comput. Assist. Surg. 2007, 3, 64–71. [Google Scholar] [CrossRef]
- De Lira, A.D.L.S.; de Moura, W.L.; Artese, F.; Bittencourt, M.A.V.; Nojima, L.I. Surgical prediction of skeletal and soft tissue changes in treatment of Class II. J. Cranio-Maxillo-Fac. Surg. 2013, 41, 198–203. [Google Scholar] [CrossRef] [PubMed]
- De Lira, A.D.L.S.; de Moura, W.L.; de Barros Vieira, J.M.; Nojima, M.G.; Nojima, L.I. Surgical prediction of skeletal and soft tissue changes in Class III treatment. J. Oral Maxillofac. Surg. 2012, 70, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Magro-Filho, O.; Magro-Hernica, N.; Queiroz, T.P.; Aranega, A.M.; Garcia, I.R., Jr. Comparative study of 2 software programs for predicting profile changes in Class III patients having double-jaw orthognathic surgery. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 452.e1–452.e5. [Google Scholar] [CrossRef] [PubMed]
- Abe, N.; Kuroda, S.; Furutani, M.; Tanaka, E. Data-based prediction of soft tissue changes after orthognathic surgery: Clinical assessment of new simulation software. Int. J. Oral Maxillofac. Surg. 2015, 3, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Donatsky, O.; Hillerup, S.; Bjorn-Jorgensen, J.; Jacobsen, P. Computerized cephalometric orthognathic surgical simulation, prediction and postoperative evaluation of precision. Int. J. Oral Maxillofac. Surg. 1992, 21, 199–203. [Google Scholar] [CrossRef]
- Koh, C.H.; Chew, M.T. Predictability of soft tissue profile changes following bimaxillary surgery in skeletal class III chinese patients. J. Oral Maxillofac. Surg. 2004, 62, 1505–1509. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.; Khambay, B.; McHugh, S.; Ayoub, A. The validity of a computer-assisted simulation system for orthognatic surgery (CASSOS) for planning the surgical correction of class III skeletal deformities: Single jaw vs. bimaxillary surgery. Oral Maxillofac. Surg. 2007, 36, 900–908. [Google Scholar] [CrossRef]
- Mollemans, W.; Schutyser, F.; Nadjmi, N.; Maes, F.; Suetens, P. Predicting soft tissue deformations for a maxillofacial surgery planning system: From computational strategies to a complete clinical validation. Med. Image Anal. 2007, 11, 282–301. [Google Scholar] [CrossRef]
- Cotin, S.; Dekingette, H.; Ayache, N. A hybrid elastic model allowing real-time cutting, deformations and force-feedback for surgery training and simulation. Vis. Comput. 2000, 16, 437–452. [Google Scholar] [CrossRef]
- Shafi, M.; Ayoub, A.; Ju, X.; Khambay, B. The accuracy of three-dimensional prediction planning for the surgical correction of facial deformities using Maxilim. Int. J. Oral Maxillofac. Surg. 2013, 42, 801–806. [Google Scholar] [CrossRef]
- Liebregts, J.; Tong, X.; Timmermans, M.; de Konig, M.; Bergè, S.; Hoppenreijs, T.; Maal, T. Accuracy of three-dimensional soft tissue simulation in bimaxillary osteotomies. J. Cranio-Maxillo-Fac. Surg. 2015, 43, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Liebregts, J.; Timmermans, M.; de koning, M.; Bergè, S.; Maal, T. Three-dimensional facial simulation in bilateral sagittal split osteotomy: A validation study of 100 patients. J. Oral Maxillo Fac. Surg. 2015, 73, 961–970. [Google Scholar] [CrossRef] [PubMed]
- Mundluru, T.; Almukhtar, A.; Ju, X.; Ayoub, A. The accuracy of three-dimensional prediction of soft tissue changes following the surgical correction of facial asymmetry: An innovative concept. Int. J. Oral Maxillofac. Surg. 2017, 46, 1517–1524. [Google Scholar] [CrossRef] [PubMed]
- De Riu, G.; Virdis, P.; Meloni, S.; Lumbau, A.; Vaira, L. Accuracy of computer-assisted orthognathic surgery. J. Cranio-Maxillofac. Surg. 2018, 46, 293–298. [Google Scholar] [CrossRef]
- Van Hemelen, G.; van Genechten, M.; Renier, L.; Desmedt, M.; Verbruggen, E.; Nadjimi, N. Three-dimensional virtual planning in orthognatic surgery enhances the accuracy of soft tissue prediction. J. Cranio-Maxillo-Fac. Surg. 2015, 43, 918–925. [Google Scholar] [CrossRef]
- Nadjmi, N.; Tehranchi, A.; Azami, N.; Saedi, B.; Mollemans, W. Comparison of soft tissue profiles in Le Fort I osteotomy patients with Dolphin and Maxilim softwares. Am. J. Orthod. Dentofac. Orthoprothes. 2013, 144, 654–662. [Google Scholar] [CrossRef]
- Resnick, C.; Dang, R.; Glick, S.; Padwa, B. Accuracy of three-dimensional soft tissue prediction for Le Fort I osteotomy using Dolphin 3D software: A pilot study. Int. J. Oral Maxillofac. Surg. 2017, 46, 289–295. [Google Scholar] [CrossRef]
- Bianchi, A.; Muyldermans, L.; di Martino, M.; Lancellotti, L.; Amadori, S.; Sarti, A.; Marchetti, C. Facial Soft Tissue Esthetic Predictions: Validation in Craniomaxillofacial Surgery with Cone Beam Computed Tomography Data. J. Oral Maxillofac. Surg. 2010, 68, 1471–1479. [Google Scholar] [CrossRef]
- Marchetti, C.; Bianchi, A.; di Martino, M.; Lancellotti, L.; Sarti, A. Validation of new soft tissue software in orthognathic surgery planning. Int. J. Oral Maxillofac. Surg. 2011, 40, 26–32. [Google Scholar] [CrossRef]
- Khambay, B.; Ullah, R. Current methods of assessing the accuracy of three-dimensional soft tissue facial prediction: Technical and clinical considerations. Oral Maxillofac. Surg. 2015, 44, 132–138. [Google Scholar] [CrossRef]
- Terzic, A.; Combescure, C.; Scolozzi, P. Accuracy of computational soft tissue predictions in orthognathic surgery from three-dimensional photographs 6 months after completion of surgery: A preliminary study of 13 patients. Int. Soc. Aesthet. Plast. Surg. 2013, 38, 184–191. [Google Scholar] [CrossRef] [PubMed]
- Ullah, R.; Turner, P.; Khambay, P. Accuracy of three-dimensional soft tissue predictions in orthognathic surgery after Le Fort I advancement osteotomies. Br. J. Oral Maxillofac. Surg. 2014, 53, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Holzinger, D.; Juergens, P.; Shahim, K.; Reyes, M.; Schicho, K.; Millesi, G.; Perisanidis, C.; Zeilhofer, H.; Seemann, R. Accuracy of soft tissue prediction in surgery-first treatment concept in orthognathic surgery: A prospective study. J. Cranio-Maxillofac. Surg. 2018, 46, 1455–1460. [Google Scholar] [CrossRef] [PubMed]
- Knoops, P.; Borghi, A.; Breakey, R.; Ong, J.; Jeelani, N.; Bruun, R.; Schievano, S.; Dunaway, D.J.; Padwa, B.L. Three-dimensional soft tissue prediction in orthognatic surgery: A clinical comparison of Dolphin, ProPlan CMF and probabilistic finite element modelling. Int. J. Oral Maxillofac. Surg. 2019, 48, 511–518. [Google Scholar] [CrossRef]
- Nam, K.-U.; Hong, J. Is three-dimensional soft tissue prediction by software accurate? J. Craniofac. Surg. 2015, 26, e729–e733. [Google Scholar] [CrossRef]
- Brice, W.; Indresano, A.; O’Rian, F. Venous tromboembolism in oral maxillofacial surgery: A literature review. J. Oral Maxillo Fac. Surg. 2011, 69, 840–844. [Google Scholar]
- Simurda, T.; Kubisz, P.; Necas, L.; Stasko, J. Perioperative coagulation management in in a patient with congenital afibrinogemia during revision total hip arthroplasty. Semin. Thromb. Emost. 2016, 42, 689–692. [Google Scholar]
- Simurda, T.; Stanciakova, L.; Stasko, J.; Dobrotova, M.; Kubisz, P. Yes or no for secondary prophilaxis in afibrinogenemia? Blood Coagul. Fibrinolysis 2015, 26, 978–980. [Google Scholar]
- Ghadimi, K.; Levy, J.; Welsby, I. Perioperative management of the bleeding patient. Br. J. Anaesth. 2016, 117, iii18–iii30. [Google Scholar] [CrossRef]
- Donatsky, O.; Bjorn-Jorgensen, J.; Hermund, U.; Nielsen, H.; Holmqvist-Larsen, M.; Nerder, P. Accuracy of combined maxillary and mandibular repositioning and of soft tissue prediction in relation to maxillary antero-superior repositioning combined with mandibular set-back. J. Cranio-Maxillofac. Surg. 2009, 37, 279–284. [Google Scholar] [CrossRef]
| Population | Patients with angle class II, III dentoskeletal deformities, indicated for a maxillary osteotomy to correct the malocclusion |
| Intervention | Le Fort I osteotomy, bimaxillary osteotomy, BSSO (bilateral sagittal split osteotomy), IVRO (intraoral ramus vertical osteotomy), SSRO (sagittal split ramus osteotomy), genioplasty |
| Comparison | 3D orthognathic surgery planning and prediction method |
| Outcome | Soft tissue post-operative change, prediction and accuracy of the technique |
| Study design | Clinical trials, retrospective and prospective studies (CT, RS and PS, respectively) with the aim of assessing the methodologies of soft and hard tissue prediction. |
| References | Journal | Study Design | Sample Size | Male Pts. | Female Pts. | Mean Age | Diagnosis | Surgery |
|---|---|---|---|---|---|---|---|---|
| N. Abe et al. 2015 | Int J Oral and maxillofacial surgery | RS | 45 | NA | NA | NA | Asymmetry, Class I, Class II | LFI, SSRO, IVRO |
| C.M. Resnick et al. 2016 | J oral maxillofacial surgery | RS | 7 | 2 | 5 | 18.1 | Maxilla hypoplasia | A single segment LFI osteotomy |
| A. Bianchi et al. 2010 | J oral maxillofacial surgery | NA | 10 | 6 | 4 | 24 | NA | LFI, BSSO, genioplasty |
| B. Khambay et al. 2015 | Int J Oral and maxillofacial surgery | NA | 10 | NA | NA | NA | NA | LFI |
| M.I. Shafi et al. 2013 | Int J Oral and maxillofacial surgery | NA | 13 | 8 | 5 | NA | NA | LFI |
| J. Liebregts et al. 2014 | J of cranio-maxillo-facial surgery | NA | 60 | 15 | 45 | 26 | NA | LFI, BSSO |
| A. Marchetti et al. 2011 | Int J Oral and maxillofacial surgery | NA | 10 | 5 | 5 | NA | NA | LFI, BSSO, genioplasty |
| T. Mundluru et al. 2017 | Int J Oral and maxillofacial surgery | RS | 13 | NA | NA | NA | Asymmetry | Bimaxillary, BSSO |
| Ana de Lourdes sa de lira et al. 2012 | J Oral Maxillofacial Surgery | CS, RS | 80 | 19(group1) 20(group2) | 21(group1) 20(group2) | 22.8(group1) 22.4(group2) | Class II | group1: BSSO group2: bimaxillary |
| Ana de Lourdes sa de lira et al. 2012 | J Oral Maxillofacial Surgery | CS, RS | 76 | 10(group1) 26(group2) | 26(group1) 14(group2) | 25.4(group1) 25.6(group2) | Class III | LFI, bimaxillary |
| A. Terzic et al. 2013 | Aesthetic Plastic Surgery | RS | 13 | 5 | 8 | 25.2 | NA | Bimaxillary (10 pts.) BSSO (3 pts.) |
| R.J. Peterman et al. 2016 | Progress in Orthodontic | RS | 14 | 3 | 11 | 22.5 | Class III | LFI, BSSO |
| R. Ullah et al. 2014 | British J of Oral and Maxillofacial Surgery | RS | 13 | 5 | 8 | 23 | Class III | LFI |
| Osvaldo Magro Filho et al. 2010 | Am J Orthod Dentofacial Orthop | NA | 10 | NA | NA | NA | Class III | LFI, BSSO |
| D. Holzinger et al. 2018 | J of cranio-maxillo-facial surgery | PS | 16 | 8 | 8 | 26 | Class III,II,I | NA |
| Chay Hui Koh et al. 2004 | J Oral Maxillofacial Surgery | NA | 35 | 14 | 21 | 22.8 | Class III | Bimaxillary |
| O. Donatsky et al. 2009 | J of cranio-maxillo-facial surgery | PS | 52 | 21 | 31 | 20 | Class III | LFI, SSRO |
| Z.Ö. Pektas et al. 2007 | Int J Med and Robotics Comput Assist Surg | RS | 11 | 4 | 7 | 23.5 | NA | LFI, BSSO |
| De Riu et al. 2018 | J of cranio-maxillo-facial surgery | RS | 49 | 19 | 30 | 26.4 | NA | Bimaxillary |
| Van Hemelen et al. 2015 | J of cranio-maxillo-facial surgery | PS | 66 | 29 | 37 | NA | Angle class II/class III malocclusion | Bimaxillary, BSSO, LFI, genioplasty |
| Knoops et al. 2019 | Int J Oral and maxillofacial surgery | RS | 7 | 2 | 5 | 18 | Maxillary sagittal hypoplasia | LFI maxillary advancement |
| Liebregts et al. 2015 | J Oral Maxillofacial Surgery | PS | 100 | 35 | 65 | 32 | Nonsyndromic mandibular hypoplasia | BSSO |
| Nam et al. 2015 | J of craniofacial surgery | PS | 29 | 16 | 13 | NA | NA | LFI, BSSRO, genioplasry |
| Nadjmi et al. 2013 | Am J Orthod Dent Orthop | RS | 13 | 2 | 11 | NA | NA | LFI, BSSO |
| Reference | Imaging Technology | Software Adopted for Prediction | Adoption of Land-Marks | Soft Tissue Land-Marks | Hard Tissue Land-Marks | Time Interval from Surgery to Post-Surgery CT | Results | Conclusions |
|---|---|---|---|---|---|---|---|---|
| N. Abe et al. 2015 | CBCT | OrthoForecast | yes | 11 on frontal image, 13 on lateral image, 3 lines | None | 12 months | Mean difference in the location of points on predicted and actual postoperative <3.4 mm and <10° in considered angles | Useful, accurate, reliable software to predict soft tissue changes after surgery |
| C.M. Resnick et al. 2016 | CBCT, 3D photographs | Dolphin 3D | yes | 37 | 42 | 14 months | Mean linear prediction error of 2.91 ± 2.16 mm; mean error at nasolabial angle of 8.1° ± 5.6°. Poorest agreement at subnasale. Most accurate lateral point: maxillary buttress (mean error 3.31 ± 1.81 mm). Least accurate lateral point: lateral ala (mean error 4.54 ± 1.97 mm) | Prediction accuracy acceptable for linear changes in the midline, not for lateral points. In the midline changes at nasal base most prone to prediction error (mean error 2.84 ± 2.55 mm) |
| B. Khambay et al. 2015 | CBCT | 3dMDvul-tus | yes | 10 | None | 6 months | 85.2%–94.4% points with error <2 mm; RMS error 0.94–2.49 mm | The use of specific anatomic regions is more meaningful than full face |
| M.I. Shafi et al. 2013 | CBCT | Maxilim | yes | NA | NA | 6–12 months | Accuracy <3 mm except for upper lip region | Clinically satisfactory for assessed regions but associated with marked errors in upper lip region |
| J. Liebregts et al. 2014 | CBCT | Maxilim | yes | 11 | None | 12 months | Mean absolute error for whole face: 0.81 ± 0.22 mm. Accuracy for whole face, upper lip, lower lip, chin subregion: 100%, 93%, 90%, 95% respectively. | The prediction accuracy is influenced by the magnitude of maxillary/mandibular advancement, age of patient, usage of V-Y closure. Low predictability on upper/lower lip regions. |
| A. Marchetti et al. 2011 | MSCT, cephalo-metric radio-graphs | SurgiCase_CMF | yes | NA | NA | 6 months | Mean abs error: 0.50–1.15 mm; percentage of simulation with error ≤ 2 mm: 76–99% | Reliability of soft tissue preview > 91% Realistic, accurate forecast of pt’s face after surgery |
| D. Holzinger et al. 2018 | CT, cephalo-metric radio-graphs | Sotirios planning software | yes | NA | 15 | 6 months | Mean error of 1.46 mm ± 1.53 mm | Quite accurate software; clinically satisfactory 3D soft tissue prediction |
| A. Bianchi et al. 2010 | CBCT | SurgiCase_CMF | yes | NA | NA | 6 months | Average abs error: 0.94 mm. St.dev: 0.90 mm Percentage of error <2 mm for 86.8% | Reliability results shows that the software makes a realistic preview with low X-ray exposure |
| T. Mundluru et al. 2017 | CBCT | Maxilim | yes | NA | NA | 6–12 months | Mean abs distance < 2 mm for all regions. | Prediction of soft tissue clinically acceptable; prediction error < 2 mm; under-prediction around the cheek and chin medio-laterally with opposite effect at inferior border of mandible bilaterally |
| O. Donatsky et al. 2009 | Cephalometric radiographs | TIOPS | yes | 8 | 8 | 5–6 weeks | Mean accuracy: 0.0–0.5 mm. Inaccuracies: 0.2–1.1 mm | Useful in surgical simulation, planning and prediction. High variability of predicted individual outcome for hard and soft tissue |
| Z.Ö. Pektas et al. 2007 | Cephalometric radiographs | Dolphin imaging version 10.0 | yes | 7 | 5 | 12 months | Least accurate site: lower lip. Most accurate sites: tip of nose, subnasale. Mean difference < 1 mm (4 pts on 7) | Satisfactory in predicting soft tissue outcome |
| R.J. Peterman et al. 2016 | Lateral cephalometric radiographs | Dolphin imaging version 11.0.03.37 | yes | 9 | 14 | 6 months | Error range: ±2 mm (X axis). | Not useful for precise treatment planning |
| Ana de Lourdes sa de Lira et al. 2012 | Lateral cephalogram | Dolphin imaging | no | NA | NA | 12 months | Surgeries more extensive than planned. Similar values between predicted and actual results for facial convexity and distance from lips to cranial base | Statistical differences do not invalidate surgical predictability because predicted modifications close to surgical results |
| Ana de Lourdes sa de Lira et al. 2012 | Lateral cephalogram | Dolphin imaging version 11.0 | no | NA | NA | 12 months | Predicted surgical reduction in mandibular length and angle significantly greater than actual post- operative | Statistical differences do not invalidate surgical predictability because predicted modifications close to surgical results |
| R. Ullah et al. 2014 | CBCT | 3dMDvultus | yes | NA | NA | 6–12 months | Mean abs distance between actual and predicted soft tissue < 3 mm and ranged from 0.65 mm (chin) to 1.17 (upper lip) | 3D soft tissue prediction is acceptable for LFI advancement osteotomy |
| Osvaldo Magro Filho et al. 2010 | Lateral cephalometric radiographs | Dentofacial planner plus (DFP), Dolphin imaging (DI) | no | NA | NA | 6 months | No statistical differences between the two software (p = 0.7945) | DFP better in predicting nasolabial angle, upper/lower lips. DI better in predicting nasal tip, chin, sub mandibular area |
| A. Terzic et al. 2013 | CT, CBCT | 3dMDvultus version 2.2.0.8 | yes | NA | NA | 6 months | Mean difference between surfaces: −0.64 mm (surgically treated lower half). Errors >3 mm: 4% for upper half and 29.8% for lower half | Accuracy in soft tissue prediction is insufficient |
| Chay Hui Koh et al. 2004 | Lateral cephalograms | CASSOS | yes | 16 | NA | 6 months | Significant differences between 16 of 32 soft tissue measurements (p < 0.05) Under estimation of vertical position for upper/lower lips, over estimation of horizontal position of lower lip | Clinically useful prediction of soft tissue profile change in Chinese patients |
| De Riu et al. 2018 | Frontal/lateral cephalometric radiograph, CBCT | Maxilim, Dolphin | yes | NA | NA | 3–5 days | Differences among 12 of the 15 parameters were considered not significant. Significant differences reported for SNA (p = 0.008), SNB (p = 0.006), anterior facial height (p = 0.033). Average error: 1.98 mm (linear measures), 1.19° (angle measures) | Good degree of accuracy for most of parameters assessed. Tendency towards under-projection of jaws. 3D simulation of soft tissue currently does not allow an accurate management of facial height and chin position |
| Van Hemelen et al. 2015 | Frontal/lateral cephalometric radiograph, CBCT | Onyx Ceph, Maxilim | yes | 17 (3D) 16 (2D) | 17 (3D) 16 (2D) | 4 months | horizontal direction: 2.29 mm (2D) vs. 1.48 mm (3D) vertical direction: 2.07 mm (2D) vs. 1.46 mm (3D) | 3D method more predictive, but more time consuming and more difficult to use. |
| Knoops et al. 2019 | CBCT | Dolphin 3D, ProPlan CMF, PFEM | Yes (Dolphin 3D) | NA | NA | 1 year | Dolphin 3D: RMS = 1.8 ± 0.8 mm ProPlan: RMS = 1.2 ± 0.4 mm PFEM: RMS = 1.3 ± 0.4 mm | Dolphin 3D: limited accuracy ProPlan/PFEM: better 3D prediction, mismatch in maxillary position (predicted/real) |
| Liebregts et al. 2015 | CBCT | Maxilim | yes | 5 | 5 | 6 months | Mean abs. err: whole face: 0.9 ± 0.3 mm upper lip: 1.2 ± 0.5 mm chin area: 0.8 ± 0.5 mm | Accurate soft tissue simulation for single surgery |
| Nam et al. 2015 | CT | Simplant Pro | yes | NA | 30 | 6 months | Mean differences: 0.73 mm (x axis), 1.39 mm (y axis), 0.85 mm (z axis). Accuracy: 52.8% | It is needed to improve soft tissue prediction accuracy |
| Nadjmi et al. 2013 | CBCT, lateral cephalograms, profile photographs | Maxilim, Dolphin | yes | 25 | 15 | 4 months | Error range (horizontal plane): −1.41 to 1.20 mm (Dolphin) −1.60 to 1.50 mm (Maxilim) Error range (vertical plane): −1.85 to 1.55 mm (Dolphin) −4.25 to 2.42 mm (Maxilim) | Errors with Dolphin are higher than with Maxilim, but not statistically significant (p > 0.05). Both showed inaccuracies (chin, lips) for complicate surgeries |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Olivetti, E.C.; Nicotera, S.; Marcolin, F.; Vezzetti, E.; Sotong, J.P.A.; Zavattero, E.; Ramieri, G. 3D Soft-Tissue Prediction Methodologies for Orthognathic Surgery—A Literature Review. Appl. Sci. 2019, 9, 4550. https://doi.org/10.3390/app9214550
Olivetti EC, Nicotera S, Marcolin F, Vezzetti E, Sotong JPA, Zavattero E, Ramieri G. 3D Soft-Tissue Prediction Methodologies for Orthognathic Surgery—A Literature Review. Applied Sciences. 2019; 9(21):4550. https://doi.org/10.3390/app9214550
Chicago/Turabian StyleOlivetti, Elena Carlotta, Sara Nicotera, Federica Marcolin, Enrico Vezzetti, Jacqueline P. A. Sotong, Emanuele Zavattero, and Guglielmo Ramieri. 2019. "3D Soft-Tissue Prediction Methodologies for Orthognathic Surgery—A Literature Review" Applied Sciences 9, no. 21: 4550. https://doi.org/10.3390/app9214550
APA StyleOlivetti, E. C., Nicotera, S., Marcolin, F., Vezzetti, E., Sotong, J. P. A., Zavattero, E., & Ramieri, G. (2019). 3D Soft-Tissue Prediction Methodologies for Orthognathic Surgery—A Literature Review. Applied Sciences, 9(21), 4550. https://doi.org/10.3390/app9214550









