Predicting the Occurrence of Falls Among Portuguese Community-Dwelling Adults Aged 50 or Older Using the Timed up and Go Test
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Definition of Fall
2.3. Functional Ability Assessment
2.4. Assessment of Other Variables
2.5. History of Falls After 12 Months
2.6. Statistics
3. Results
3.1. Univariate Analysis
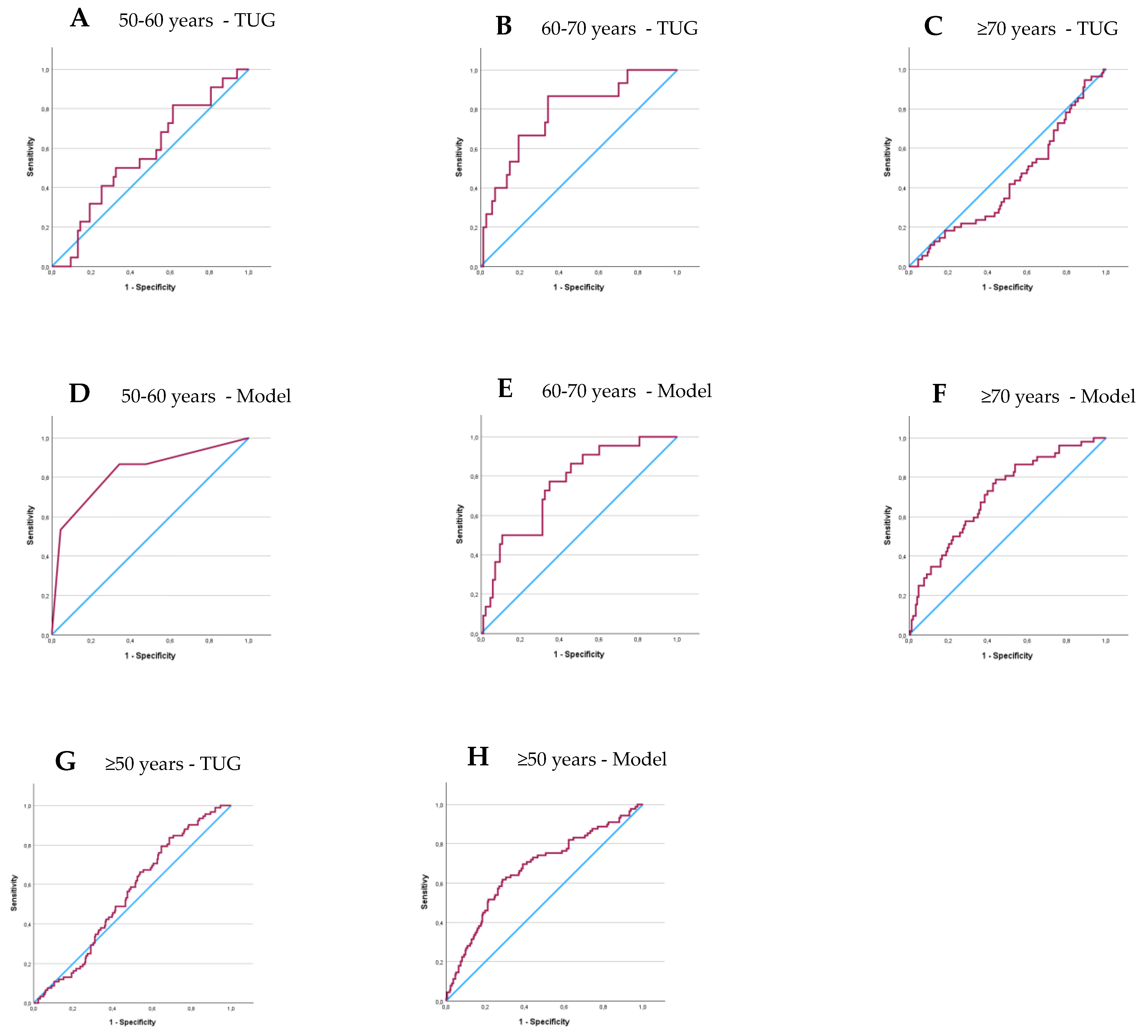
3.2. ROC Curves for TUG
3.3. Logistic Regression
3.4. Logistic Regression Models Validation—ROC Curves
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Avin, K.G.; Hanke, T.A.; Kirk-Sanchez, N.; McDonough, C.M.; Shubert, T.E.; Hardage, J.; Hartley, G. Management of falls in community-dwelling older adults: Clinical guidance statement from the academy of geriatric physical therapy of the american physical therapy association. Phys. Ther. 2015, 95, 815–834. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence (NICE). Assessment and Prevention of Falls in Older People. NICE Clinical Guideline 161. 2013. Available online: https://www.nice.org.uk/guidance/cg161 (accessed on 23 November 2024).
- Colón-Emeric, C.S.; McDermott, C.L.; Lee, D.S.; Berry, S.D. Risk assessment and prevention of falls in older community-dwelling adults: A review. JAMA 2024, 331, 1397–1406. [Google Scholar] [CrossRef]
- Montero-Odasso, M.; Van Der Velde, N.; Martin, F.C.; Petrovic, M.; Tan, M.P.; Ryg, J.; Aguilar-Navarro, S.; Alexander, N.B.; Becker, C.; Blain, H.; et al. World guidelines for falls prevention and management for older adults: A global initiative. Age Ageing 2022, 51, 1501. [Google Scholar] [CrossRef] [PubMed]
- Sampaio, F.; Nogueira, P.; Ascenção, R.; Henriques, A.; Costa, A. The epidemiology of falls in Portugal: An analysis of hospital admission data. PLoS ONE 2021, 16, e0261456. [Google Scholar] [CrossRef] [PubMed]
- Australian Commission on Safety and Quality in Healthcare. Preventing Falls and Harm from Falls in Older People. Australian Community Care. 2009. Available online: https://www.safetyandquality.gov.au/publications-and-resources/resource-library/preventing-falls-and-harm-falls-older-people-best-practice-guidelines-australian-community-care (accessed on 15 September 2024).
- Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society. Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J. Am. Geriatr. Soc. 2011, 59, 148–157. [Google Scholar] [CrossRef] [PubMed]
- Tinetti, M.E.; Speechley, M.; Ginter, S.F. Risk factors for falls among elderly persons living in the community. N. Engl. J. Med. 1988, 319, 1701–1707. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Speechley, M. Multiple risk factors approach prevention of falls. In Reducing Frailty and Falls in Older Persons; Weindruch, R.W., Hadley, E.C., Ory, M.G., Eds.; Charles C Thomas Publisher: Springfield, IL, USA, 1991; pp. 126–131. [Google Scholar]
- Rubenstein, L.Z.; Josephson, K.R.; Robbins, A.S. Falls in the nursing home. Ann. Intern. Med. 1994, 121, 442–451. [Google Scholar] [CrossRef]
- Lach, H.W.; Reed, A.T.; Arfken, C.L.; Miller, J.P.; Paige, G.D.; Birge, S.J.; Peck, W.A. Falls in the Elderly: Reliability of a Classification System. J. Am. Geriatr. Soc. 1991, 39, 197–202. [Google Scholar] [CrossRef]
- Appeadu, M.K.; Bordoni, B. Falls and Fall Prevention in Older Adults. StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK560761/ (accessed on 15 September 2024).
- Kim, S.H. Risk factors for severe injury following indoor and outdoor falls in geriatric patients. Arch. Gerontol. Geriatr. 2016, 62, 75–82. [Google Scholar] [CrossRef]
- Rubenstein, L.Z.; Josephson, K.R. The epidemiology of falls and syncope. Clin. Geriatr. Med. 2002, 18, 141–158. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Powell, L. Fear of falling and low self-efficacy: A case of dependence in elderly persons. J. Gerontol. 1993, 48, 35–38. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.; Jeon, G.S.; Cho, S.I. Prospective study on the impact of fear of falling on functional decline among community dwelling elderly women. Int. J. Environ. Res. Public Health 2017, 14, 469. [Google Scholar] [CrossRef]
- Rubenstein, L.Z.; Vivrette, R.; Harker, J.O.; Stevens, J.A.; Kramer, B.J. Validating an evidence-based, self-rated fall risk questionnaire (FRQ) for older adults. J. Saf. Res. 2011, 42, 493–499. [Google Scholar] [CrossRef]
- Fabre, J.M.; Ellis, R.; Kosma, M.; Wood, R.H. Falls risk factors and a compendium of falls risk screening instruments. J. Geriatr. Phys. Ther. 2010, 33, 184–197. [Google Scholar] [CrossRef] [PubMed]
- de Jong, M.R.; Van Der Elst, M.; Hartholt, K.A. Drug-related falls in older patients: Implicated drugs, consequences, and possible prevention strategies. Ther. Adv. Drug Saf. 2010, 4, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Hartikainen, S.; Lönnroos, E.; Louhivuori, K. Medication as a risk factor for falls: Critical systematic review. J. Gerontol. Biol. Sci. Med. Sci. 2007, 62, 1172–1181. [Google Scholar] [CrossRef]
- Ziere, G.; Dieleman, J.P.; Hofman, A.; Pols, H.A.P.; van der Cammen, T.J.M.; Stricker, B.H.C. Polypharmacy and falls in the middle age and elderly population. Br. J. Clin. Pharmacol. 2006, 61, 218–223. [Google Scholar] [CrossRef]
- McMahon, S.K.; Greene, E.J.; Latham, N.; Peduzzi, P.; Gill, T.M.; Bhasin, S.; Reuben, D.B. Engagement of older adults in STRIDE’s multifactorial fall injury prevention intervention. J. Am. Geriatr. Soc. 2022, 72, 3116–3126. [Google Scholar] [CrossRef]
- Gillespie, L.D.; Robertson, M.C.; Gillespie, W.J.; Sherrington, C.; Gates, S.; Clemson, L.M.; Lamb, S.E. Interventions for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2009, 15, CD007146, Update in Cochrane Database Syst. Rev. 2012, 12, CD007146. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, J.V. A review of stairway falls and stair negotiation: Lessons learned and future needs to reduce injury. Gait Posture 2016, 49, 159–167. [Google Scholar] [CrossRef]
- Jones, C.J.; Rikli, R.E.; Beam, W.C. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Res. Q. Exerc. Sport 1999, 70, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Middleton, A.; Fritz, S.L.; Lusardi, M. HHS Public Access. J. Aging Phys. Act. 2015, 23, 314–322. [Google Scholar] [CrossRef]
- Kang, L.; Han, P.; Wang, J.; Ma, Y.; Jia, L.; Fu, L.; Chen, X. Timed Up and Go Test can predict recurrent falls: A longitudinal study of the community-dwelling elderly in China. Clin. Interv. Aging 2017, 12, 2009–2016. [Google Scholar] [CrossRef]
- Rose, D.J.; Jones, C.J.; Lucchese, N. Predicting the probability of falls in community-residing older adults using the 8-foot up-and-go: A new measure of functional mobility. J. Aging Phys. Act. 2002, 10, 466–475. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The timed ‘Up and Go’: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Gates, S.; Smith, L.A.; Fisher, J.D.; Lamb, S.E. Systematic review of accuracy of screening instruments for predicting fall risk among independently living older adults. J. Rehabil. Res. Dev. 2008, 45, 1105–1116. [Google Scholar] [CrossRef]
- Barry, E.; Galvin, R.; Keogh, C.; Horgan, F.; Fahey, T. Is the Timed Up and Go Test a useful predictor of risk of falls in community dwelling older adults: A systematic review and meta-analysis. BMC Geriatr. 2014, 14, 14. [Google Scholar] [CrossRef]
- Talbot, L.A.; Musiol, R.J.; Witham, E.K.; Metter, E.J. Falls in young, middle-aged and older community dwelling adults: Perceived cause, environmental factors and injury. BMC Public Health 2005, 5, 86. [Google Scholar] [CrossRef]
- Beauchet, O.; Fantino, B.; Allali, G.; Muir, S.W.; Montero-Odasso, M.; Annweiler, C. Timed Up and Go test and risk of falls in older adults: A systematic review. J. Nutr. Health Aging 2011, 15, 933–938. [Google Scholar] [CrossRef]
- Martins, A.C.; Moreira, J.; Silva, C.; Silva, J.; Tonelo, C.; Baltazar, D.; Rocha, C.; Pereira, T.; Sousa, I. Multifactorial Screening Tool for Determining Fall Risk in Community-Dwelling Adults Aged 50 Years or Over (FallSensing): Protocol for a Prospective Study. JMIR Res. Protoc. 2018, 7, e10304. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Centers for Disease Control and Prevention. Algorithm for Fall Risk Screening, Assessment, and Intervention. 2017. Available online: https://www.cdc.gov/steadi/pdf/STEADI-Algorithm-508.pdf (accessed on 14 September 2024).
- Hammond, T.; Wilson, A. Polypharmacy and falls in the elderly: A literature review. Nurs. Midwifery Stud. 2011, 2, 171–175. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Díaz-Gutiérrez, M.J.; Martínez-Cengotitabengoa, M.; Sáez de Adana, E.; Cano, A.I.; López, P.; Besga, A. Relationship between the use of benzodiazepines and falls in older adults: A systematic review. Maturitas 2017, 101, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Frieson, C.W.; Tan, M.P.; Ory, M.G.; Smith, M.L. Editorial: Evidence-Based Practices to Reduce Falls and Fall-Related Injuries Among Older Adults. Front. Public Health 2018, 21, 222. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jehu, D.A.; Skelton, D.A. The Measurement and Reporting of Falls: Recommendations for Research on Falls Data Collection and Capturing Social Determinants of Health. J. Frailty Sarcopenia Falls 2024, 9, 166–168. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lewis, S.R.; McGarrigle, L.; Pritchard, M.W.; Bosco, A.; Yang, Y.; Gluchowski, A.; Sremanakova, J.; Boulton, E.R.; Gittins, M.; Spinks, A.; et al. Population-based interventions for preventing falls and fall-related injuries in older people. Cochrane Database Syst. Rev. 2024, 1, CD013789. [Google Scholar] [CrossRef]
- Chepisheva, M.K. Spatial orientation, postural control and the vestibular system in healthy elderly and Alzheimer’s dementia. PeerJ 2023, 11, e15040. [Google Scholar] [CrossRef]
| Factors | Total (n = 403) | Fallers (n = 97) | Non-Fallers (n = 306) | p |
|---|---|---|---|---|
| Intrinsic | ||||
| Gender | 0.039 | |||
| Male | 121 (30) | 21 (17) | 100 (83) | |
| Female | 282 (70) | 76 (27) | 206 (73) | |
| History of Fall | <0.001 | |||
| Yes | 127 (32) | 47 (37) | 80 (63) | |
| No | 276 (69) | 50 (18) | 226 (82) | |
| Fear of Fall | 0.113 | |||
| Yes | 192 (48) | 53 (28) | 139 (72) | |
| No | 211 (52) | 44 (21) | 167 (79) | |
| Extrinsic | ||||
| Medication | ||||
| Benzodiazepines | 0.002 | |||
| Yes | 106 (26) | 37 (35) | 69 (65) | |
| No | 297 (74) | 60 (20) | 237 (80) | |
| Antidepressants | 0.010 | |||
| Yes | 94 (23) | 32 (34) | 62 (66) | |
| No | 309 (77) | 65 (21) | 244 (79) | |
| Antihypertensive | 0.048 | |||
| Yes | 257 (64) | 70 (27) | 187 (73) | |
| No | 146 (36) | 27 (19) | 119 (82) | |
| Polypharmacy | 0.009 | |||
| Yes | 232 (58) | 67 (29) | 165 (71) | |
| No | 171 (42) | 30 (18) | 141 (82) | |
| Upper Extremities | 0.026 | |||
| Yes | 132 (33) | 41 (31) | 91 (69) | |
| No | 271 (67) | 56 (21) | 215 (79) | |
| Mobility assistive | 0.800 | |||
| Yes | 51 (13) | 13 (26) | 38 (74) | |
| No | 352 (87) | 84 (24) | 268 (76) | |
| Stairs | 0.978 | |||
| Yes | 312 (77) | 75 (24) | 237 (76) | |
| No | 91 (23) | 22 (24) | 69 (76) |
|
50–60 Years (n = 83) |
60–70 Years (n = 106) |
≥70 Years (n = 214) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Factors | Fallers (n = 16) | Non-Fallers (n = 67) | p | Fallers (n = 22) | Non-Fallers (n = 84) | p | Fallers (n = 59) | Non-Fallers (n = 155) | p |
| Intrinsic | |||||||||
| Gender | 0.064 | 0.776 | 0.054 | ||||||
| Male | 0 (0) | 13 (100) | 4 (17) | 20 (83) | 17 (20) | 67 (80) | |||
| Female | 16 (23) | 54 (77) | 18 (22) | 64 (78) | 42 (32) | 88 (68) | |||
| History of Fall | 0.003 | 0.346 | 0.004 | ||||||
| Yes | 9 (43) | 12 (57) | 8 (27) | 22 (73) | 30 (40) | 46 (60) | |||
| No | 7 (11) | 55 (89) | 14 (18) | 62 (82) | 29 (21) | 109 (79) | |||
| Fear of Fall | 0.016 | 0.842 | 0.754 | ||||||
| Yes | 9 (36) | 16 (64) | 11 (22) | 40 (78) | 33 (28) | 83 (72) | |||
| No | 7 (12) | 51 (88) | 11 (20) | 44 (80) | 26 (27) | 72 (73) | |||
| Extrinsic | |||||||||
| Medication | |||||||||
| Benzodiazepines | 0.012 | 0.038 | 0.330 | ||||||
| Yes | 7 (44) | 9 (56) | 8 (38) | 13 (62) | 22 (32) | 47 (68) | |||
| No | 9 (13) | 58 (87) | 14 (17) | 71 (83) | 37 (25) | 108 (75) | |||
| Antidepressants | 0.037 | 0.562 | 0.120 | ||||||
| Yes | 7 (39) | 11 (61) | 6 (26) | 17 (74) | 19 (36) | 34 (64) | |||
| No | 9 (14) | 56 (86) | 16 (19) | 67 (81) | 40 (25) | 121 (75) | |||
| Antihypertensive | 0.553 | 0.084 | 0.651 | ||||||
| Yes | 6 (23) | 20 (77) | 17 (26) | 47 (74) | 47 (28) | 119 (72) | |||
| No | 10 (18) | 47 (82) | 5 (12) | 36 (88) | 12 (25) | 36 (75) | |||
| Polypharmacy | 0.003 | 0.045 | 0.876 | ||||||
| Yes | 9 (43) | 12 (57) | 16 (28) | 41 (72) | 42 (27) | 112 (73) | |||
| No | 7 (11) | 55 (89) | 6 (12) | 43 (88) | 17 (28) | 43 (72) | |||
| Upper Extremities | 0.017 | 0.021 | 0.910 | ||||||
| Yes | 7 (41) | 10 (59) | 9 (39) | 14(61) | 25 (27) | 67 (73) | |||
| No | 9 (14) | 57(86) | 13 (16) | 70 (84) | 34 (28) | 88 (72) | |||
| Mobility assistive | 0.035 | 1.00 | 0.531 | ||||||
| Yes | 2 (100) | 0 (0) | 0 (0) | 3 (100) | 11 (24) | 35 (76) | |||
| No | 14 (17) | 67 (83) | 22 (21) | 81 (79) | 48 (29) | 120 (71) | |||
| Stairs | 1.000 | 0.730 | 0.692 | ||||||
| Yes | 14 (20) | 57 (80) | 19 (20) | 74 (80) | 42 (28) | 106 (72) | |||
| No | 2 (17) | 10 (83) | 3 (23) | 10 (77) | 17 (26) | 49 (74) | |||
| Models | β | SE | Wald | p | OR | 95% CI |
|---|---|---|---|---|---|---|
| ≥50 years | ||||||
| (a) TUG | −0.185 | 0.022 | 67.424 | <0.001 | 0.83 | 0.80–0.87 |
| (b) HoF (1) | 0.848 | 0.263 | 10.382 | 0.001 | 2.34 | 1.39–3.91 |
| (c) UpExt (1) | 0.585 | 0.285 | 4.212 | 0.040 | 1.79 | 1.11–21.4 |
| (d) Benzodiazepines (1) | 0.834 | 0.280 | 8.856 | 0.003 | 2.30 | 1.33–3.99 |
| 50–60 years | ||||||
| (e) TUG cut-off (1) | −2.528 | 0.832 | 9.234 | 0.002 | 0.08 | 0.02–0.41 |
| (b) HoF (1) | 1.666 | 0.689 | 5.856 | 0.016 | 5.29 | 1.37–20.41 |
| Constant | −1.136 | 0.448 | 6.443 | 0.011 | 0.32 | - |
| 60–70 years | ||||||
| (a) TUG | −0.173 | 0.072 | 5.806 | 0.016 | 0.84 | 0.73–0.97 |
| (c) UpExt (0) | −1.345 | 0.468 | 8.245 | 0.004 | 0.26 | 0.10–0.65 |
| (f) Medications/day | 0.215 | 0.086 | 6.214 | 0.013 | 1.24 | 1.05–1.47 |
| ≥70 years | ||||||
| (a) TUG | −0.056 | 0.027 | 4.444 | 0.035 | 0.95 | 0.90–0.99 |
| (b) HoF (1) | 1.125 | 0.347 | 10.497 | 0.001 | 3.08 | 1.56–6.09 |
| (d) Benzodiazepines (1) | 0.797 | 0.362 | 4.836 | 0.028 | 2.22 | 1.09–4.51 |
| Constant | −1.093 | 0.356 | 9.422 | 0.002 | 0.34 | - |
| Cut-Off Scores | Sensitivity (%Fallers) | Specificity (%Non-Fallers) | AUC | 95% CI | p | |
|---|---|---|---|---|---|---|
| TUG | ||||||
| ≥50 years | - | - | - | 54.7 | 48.5–60.9 | 0.136 |
| 50–60 years | 6.9 | 86.7 | 66.7 | 77.7 | 0.66–0.91 | 0.001 |
| 60–70 years | - | - | - | 56.8 | 43.9–69.8 | 0.300 |
| ≥70 years | - | - | - | 43.4 | 34.6–52.1 | 0.137 |
| Models | ||||||
| ≥50 years | 26.5 | 69.7 | 61.0 | 67.1 | 60.5–73.7 | <0.001 |
| 50–60 years | 18.1 | 86.7 | 65.7 | 82.5 | 69.3–95.7 | <0.001 |
| 60–70 years | 17.8 | 77.3 | 65.1 | 75.4 | 64.7–86.1 | <0.001 |
| ≥70 years | 24.8 | 71.2 | 61.5 | 70.8 | 62.8–78.8 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martins, A.C.; Moreira, J.; Silva, C.; Tonelo, C.; Rocha, C. Predicting the Occurrence of Falls Among Portuguese Community-Dwelling Adults Aged 50 or Older Using the Timed up and Go Test. Appl. Sci. 2025, 15, 4370. https://doi.org/10.3390/app15084370
Martins AC, Moreira J, Silva C, Tonelo C, Rocha C. Predicting the Occurrence of Falls Among Portuguese Community-Dwelling Adults Aged 50 or Older Using the Timed up and Go Test. Applied Sciences. 2025; 15(8):4370. https://doi.org/10.3390/app15084370
Chicago/Turabian StyleMartins, Anabela Correia, Juliana Moreira, Catarina Silva, Cláudia Tonelo, and Clara Rocha. 2025. "Predicting the Occurrence of Falls Among Portuguese Community-Dwelling Adults Aged 50 or Older Using the Timed up and Go Test" Applied Sciences 15, no. 8: 4370. https://doi.org/10.3390/app15084370
APA StyleMartins, A. C., Moreira, J., Silva, C., Tonelo, C., & Rocha, C. (2025). Predicting the Occurrence of Falls Among Portuguese Community-Dwelling Adults Aged 50 or Older Using the Timed up and Go Test. Applied Sciences, 15(8), 4370. https://doi.org/10.3390/app15084370








