Comparative Effects of Rubber Dam and Traditional Isolation Techniques on Orthodontic Bracket Positioning: A 3D Digital Model Evaluation
Abstract
1. Introduction
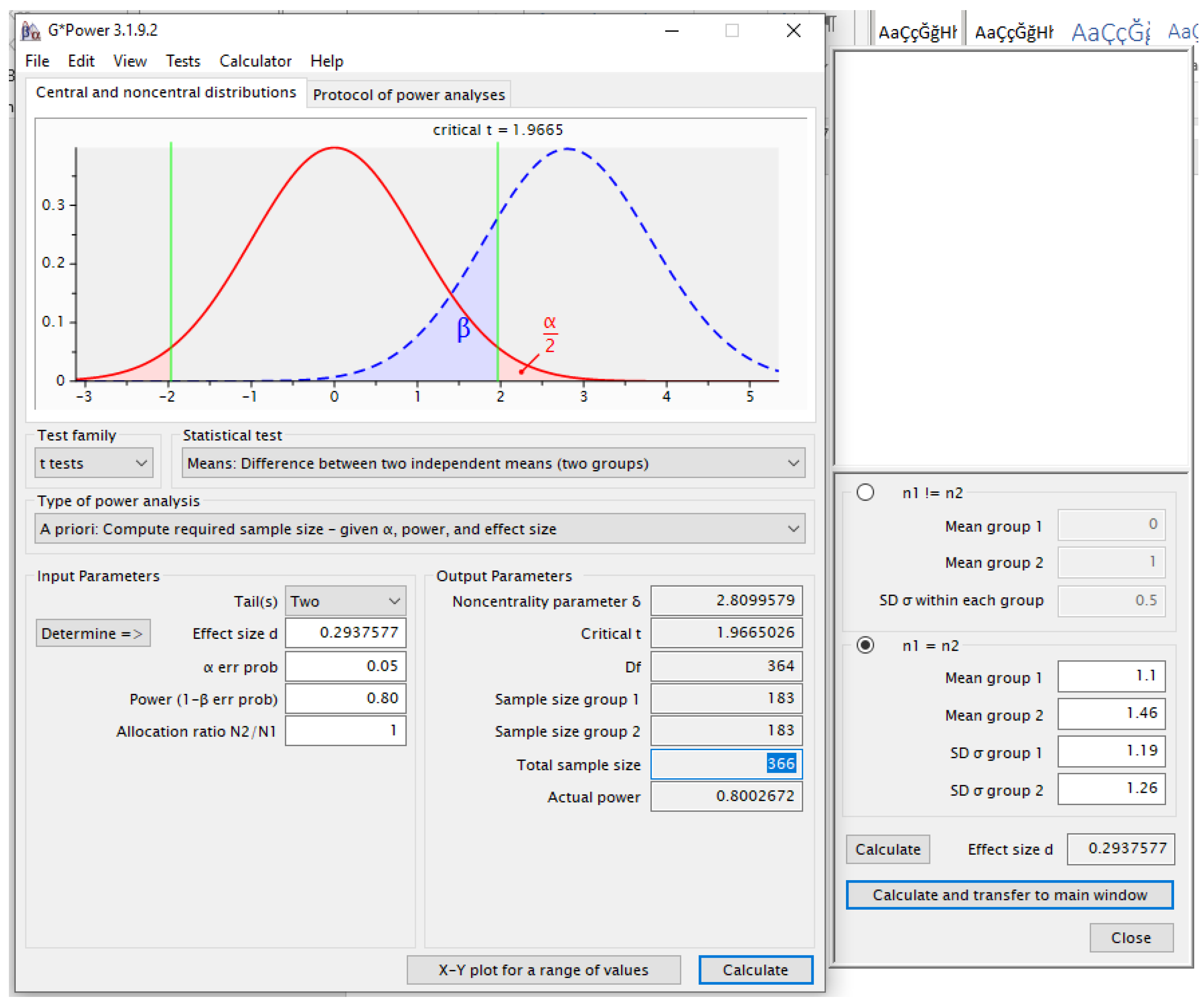
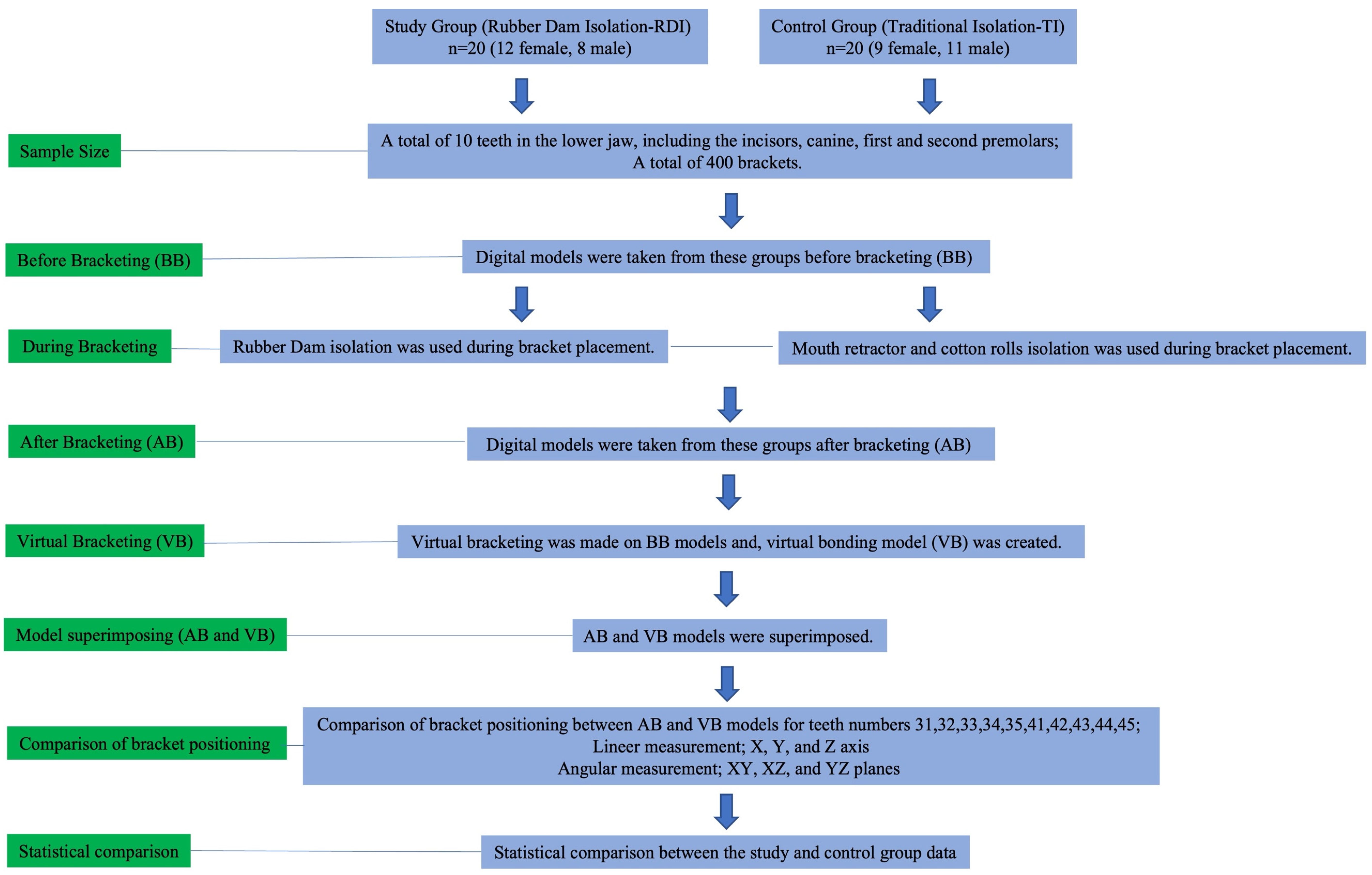
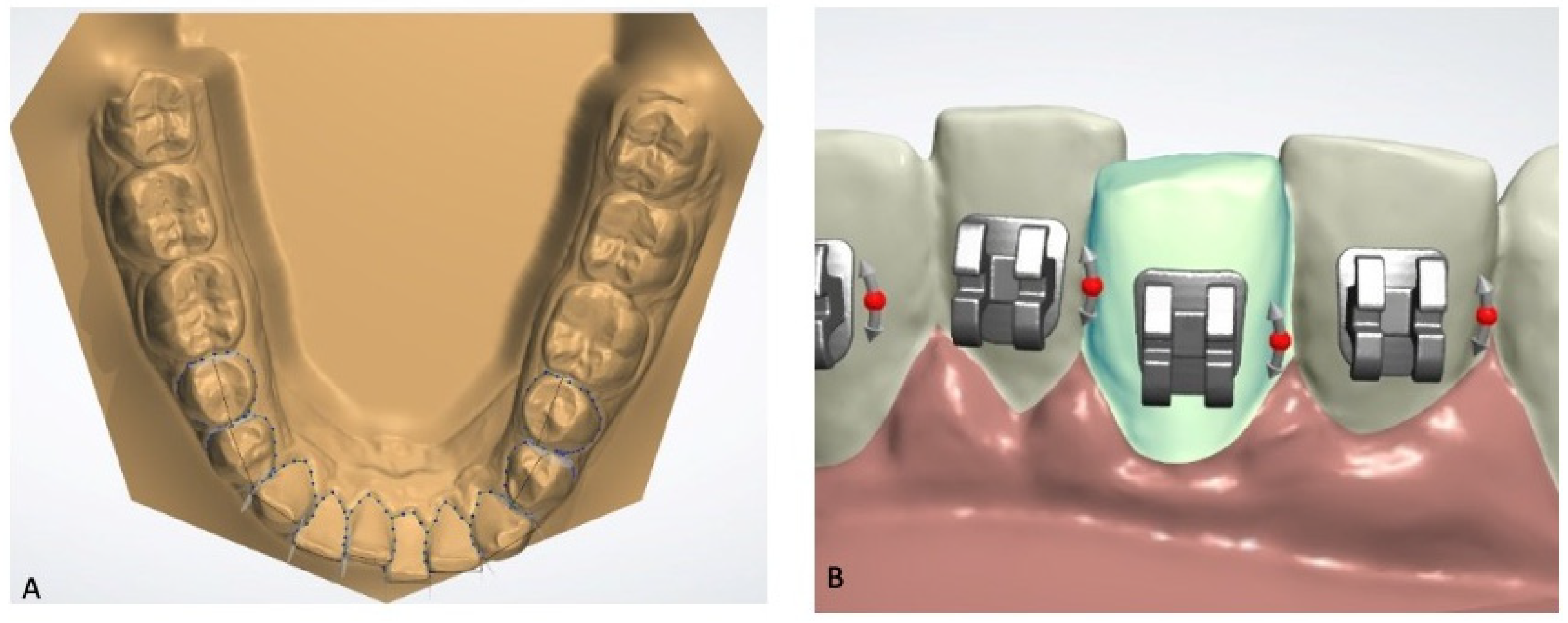
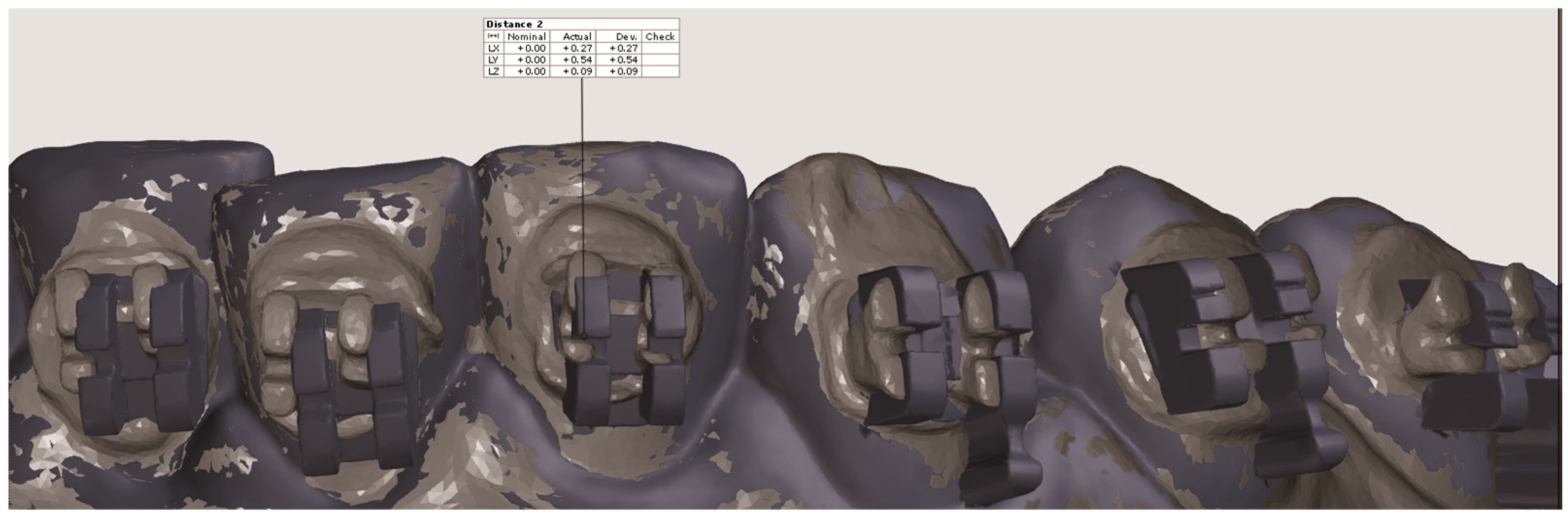
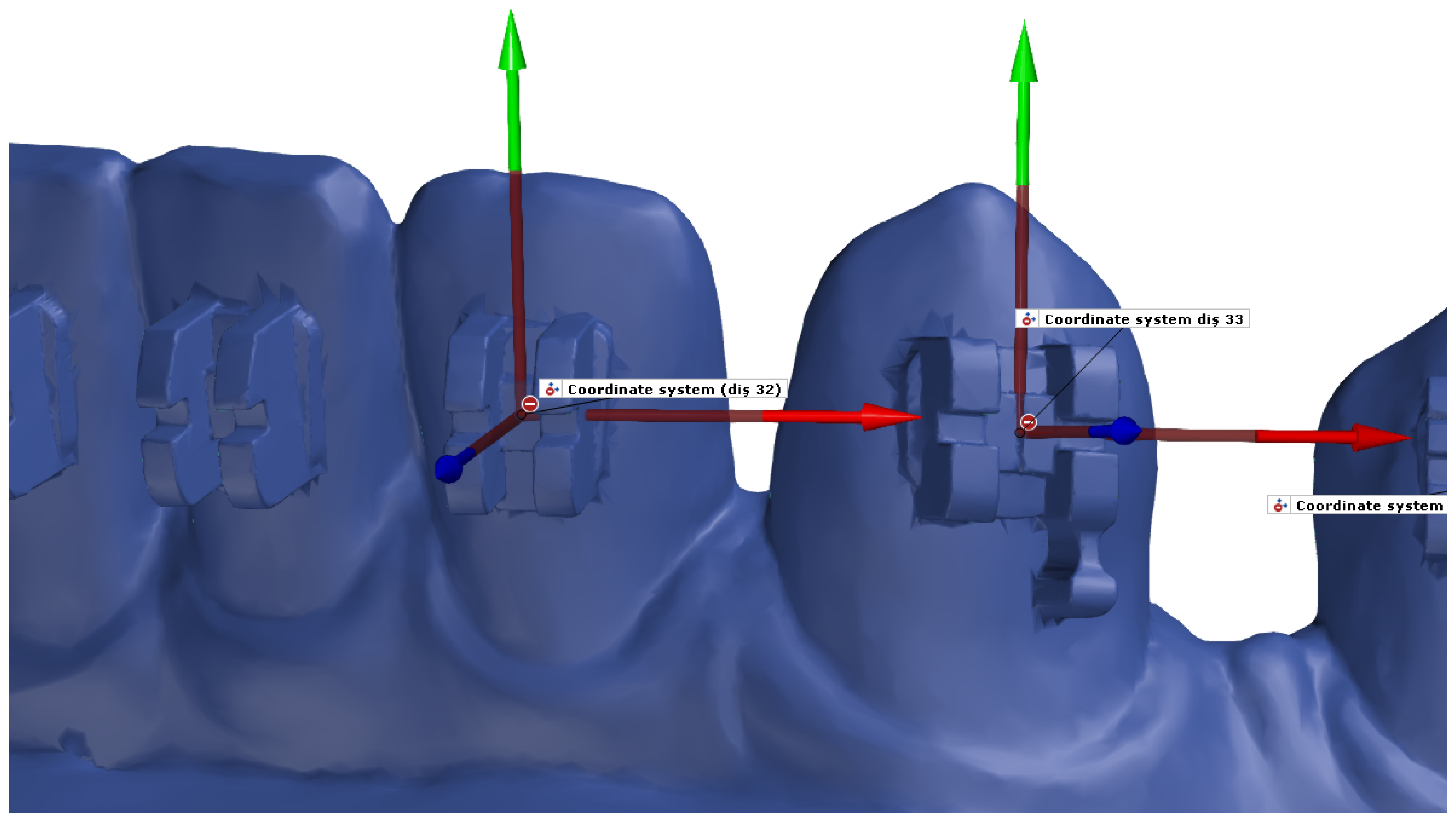
2. Materials and Methods
- -
- No missing teeth in the mandible. To maintain statistical consistency when comparing the teeth only patients with a complete dentition in the arch were included in this study.
- -
- Complete permanent dentition with all teeth fully erupted. Attention was given to ensuring the presence of fully erupted teeth for the correct placement of the brackets.
- -
- -
- Crowding of less than 4 mm.
- -
- No active dental caries, fractures, dimensional anomalies, or dental prostheses.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sepkowitz, K.A.; Eisenberg, L. Occupational Deaths among Healthcare Workers. Emerg. Infect. Dis. 2005, 11, 1003–1008. [Google Scholar] [CrossRef]
- Izzetti, R.; Nisi, M.; Gabriele, M.; Graziani, F. COVID-19 Transmission in Dental Practice: Brief Review of Preventive Measures in Italy. J. Dent. Res. 2020, 99, 1030–1038. [Google Scholar] [CrossRef]
- Ahmad, I.A. Rubber Dam Usage for Endodontic Treatment: A Review. Int. Endod. J. 2009, 42, 963–972. [Google Scholar] [CrossRef]
- Ostrovskyi, P.; Smirnova, V.; Boitsaniuk, S.; Kochan, O.; Levkiv, M. COVID-19 transmission in dental practice: Risks and prevention–narrative review. EUREKA 2023, 31, 67–72. [Google Scholar] [CrossRef]
- Singh, R.; Goel, A.; Pani, P.; Negi, B.S.; Rajguru, J.P.; Somayaji, N.S. Coronavirus: An emerging and future challenge for dental clinicians. Nat. J. Maxillofac. Surg. 2022, 13, 20–26. [Google Scholar] [CrossRef]
- Al-Amad, S.H.; Awad, M.A.; Edher, F.M.; Khalil, S.; Omran, T.A. The effect of rubber dam on atmospheric bacterial aerosols during restorative dentistry. J. Infect. Public Health 2017, 10, 195–200. [Google Scholar] [CrossRef]
- Samaranayake, L.P.; Fakhruddin, K.S.; Buranawat, B.; Panduwawala, C. The efficacy of bio-aerosol reducing procedures used in dentistry: A systematic review. Acta Odontol. Scand. 2021, 79, 69–80. [Google Scholar] [CrossRef]
- Reuter, J.E. The isolation of teeth and the protection of the patient during endodontic treatment. Int. Endod. J. 1983, 16, 173–181. [Google Scholar] [CrossRef]
- Filipović, J.; Jukić, S.; Miletić, I.; Pavelić, B.; Malčić, A.; Anić, I. Patient’s attitude to rubber dam use. Acta Stomatolog. Croat. 2004, 38, 313–317. Available online: https://hrcak.srce.hr/file/3699 (accessed on 22 January 2025).
- Kapitan, M.; Sustova, Z.; Ivancakova, R.; Suchanek, J. A comparison of different rubber dam systems on a dental simulator. Acta Med. 2014, 57, 15–20. [Google Scholar] [CrossRef]
- Mattar, R.; Sulimany, A.M.; Binsaleh, S.S.; Al-Majed, I.M. Comparison of Fissure Sealant Chair Time and Patients’ Preference Using Three Different Isolation Techniques. Children 2021, 8, 444. [Google Scholar] [CrossRef]
- Andrews, L.F. The Straight-Wire Appliance. Br. J. Orthod. 1979, 6, 125–143. [Google Scholar] [CrossRef]
- McLaughlin, R.P.; Bennett, J.C. Finishing and Detailing with a Preadjusted Appliance System. J. Clin. Orthod. 1991, 25, 251–264. [Google Scholar] [PubMed]
- Shin, S.H.; Yu, H.S.; Cha, J.Y.; Kwon, J.S.; Hwang, C.J. Scanning Accuracy of Bracket Features and Slot Base Angle in Different Bracket Materials by Four Intraoral Scanners: An in Vitro Study. Materials 2021, 14, 365. [Google Scholar] [CrossRef]
- Aboujaoude, R.; Kmeid, R.; Gebrael, C.; Amm, E. Comparison of the Accuracy of Bracket Positioning between Direct and Digital Indirect Bonding Techniques in the Maxillary Arch: A Three-Dimensional Study. Prog. Orthod. 2022, 23, 31. [Google Scholar] [CrossRef] [PubMed]
- Hodge, T.M.; Dhopatkar, A.; Rock, P.A. Randomized clinical trial comparing the accuracy of direct versus indirect bracket placement. J. Orthod. 2004, 31, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.; Kee, Y.; Lee, K.C. Effect of the presence of orthodontic brackets on intraoral scans. Angle Orthod. 2021, 1, 98–104. [Google Scholar] [CrossRef]
- Gelgör, I.E.; Karaman, A.I.; Ercan, E. Prevalence of malocclusion among adolescents in central anatolia. Eur. J. Dent. 2007, 1, 125–131. [Google Scholar] [CrossRef] [PubMed]
- Celikoglu, M.; Akpinar, S.; Yavuz, I. The pattern of malocclusion in a sample of orthodontic patients from Turkey. Med. Oral. Patolog. Oral. Cir. Bucal 2010, 15, 791–796. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Youn-Sic, C.; Minji, K. Accuracy of bracket positions with a CAD/CAM indirect bonding system in posterior teeth with different cusp heights. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 298–307. [Google Scholar] [CrossRef]
- World Health Organization. Keep Health Workers Safe to Keep Patients Safe: WHO. 2020. Available online: https://www.who.int/news/item/17-09-2020-keep-health-workers-safe-to-keep-patients-safe-who (accessed on 22 January 2025).
- Peng, X.; Xu, X.; Li, Y.; Cheng, L.; Zhou, X.; Ren, B. Transmission Routes of 2019-NCoV and Controls in Dental Practice. Int. J. Oral. Sci. 2020, 12, 9. [Google Scholar] [CrossRef] [PubMed]
- Volgenant, C.M.C.; de Soet, J.J. Cross-transmission in the Dental Office: Does This Make You Ill? Cur. Oral. Health Rep. 2018, 5, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Marui, V.C.; Souto, M.L.S.; Rovai, E.S.; Romito, G.A.; Chambrone, L.; Pannuti, C.M. Efficacy of preprocedural mouthrinses in the reduction of microorganisms in aerosol: A systematic review. J. Am. Dent. Assoc. 2019, 150, 1015–1026. [Google Scholar] [CrossRef] [PubMed]
- Dutil, S.; Meriaux, A.; de Latremoille, M.-C.; Lazure, L.; Barbeau, J.; Duchaine, C. Measurement of airborne bacteria and endotoxin generated during dental cleaning. J. Occup. Environ. Hyg. 2009, 6, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Nikitin, N.; Petrova, E.; Trifonova, E.; Karpova, O. Influenza virus aerosols in the air and their infectiousness. Adv. Virol. 2014, 2014, 859090. [Google Scholar] [CrossRef]
- Browning, W.D.; McCarthy, J.P. A case series: Herpes simplex virus as an occupational hazard. J. Esthet. Restor. Dent. 2012, 24, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Phillips, H.W. Dr. Homer W. Phillips on Bonding (Part 2). Interview by EL Gottlieb. J. Clin. Orthod. 1980, 14, 462–480. [Google Scholar] [PubMed]
- Panayi, N.C.; Tsolakis, A.I.; Athanasiou, A.E. Digital Assessment of Direct and Virtual Indirect Bonding of Orthodontic Brackets: A Clinical Prospective Cross-Sectional Comparative Investigation. Int. Orthod. 2020, 18, 714–721. [Google Scholar] [CrossRef]
- McMullan, R.E.; Richardson, A. Spontaneous Changes in the Rotation of Premolar Teeth from Eruption until the Established Dentition. Eur. J. Orthod. 1991, 13, 392–396. [Google Scholar] [CrossRef] [PubMed]
- Bennett, J.C.; McLaughlin, R.P. Orthodontic Management of the Dentition with the Preadjusted Appliance; ISIS Medical Media: Mosby, MD, USA, 1997. [Google Scholar]
- Ludwig, F.J. The Mandibular Second Premolars: Morphologic Variation and Inheritance. J. Dent. Res. 1957, 36, 263–273. [Google Scholar] [CrossRef]
- Carlsen, O.; Alexandersen, V. Mandibular Premolar Differentiation. Scand. J. Dent. Res. 1994, 102, 81–87. [Google Scholar] [CrossRef]
- McLaughlin, R.P. Bracket Placement with the Preadjusted Appliance. J. Clin. Orthod. 1995, 29, 302–311. [Google Scholar] [PubMed]
- Stasinopoulos, D.; Papageorgiou, S.N.; Kirsch, F.; Daratsianos, N.; Jäger, A.; Bourauel, C. Failure Patterns of Different Bracket Systems and Their Influence on Treatment Duration: A Retrospective Cohort Study. Angle Orthod. 2018, 88, 338–347. [Google Scholar] [CrossRef] [PubMed]
- Fowler, P.V. Variations in the Perception of Ideal Bracket Location and Its Implications for the Pre-Adjusted Edgewise Appliance. Br. J. Orthod. 1990, 17, 305–310. [Google Scholar] [CrossRef] [PubMed]
- Taylor, N.G.; Cook, P.A. The Reliability of Positioning Pre-Adjusted Brackets: An in Vitro Study. Br. J. Orthod. 1992, 19, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Xue, C.; Xu, H.; Guo, Y.; Xu, L.; Dhami, Y.; Wang, H.; Liu, Z.; Ma, J.; Bai, D. Accurate Bracket Placement Using a Computer-Aided Design and Computer-Aided Manufacturing–Guided Bonding Device: An in Vivo Study. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 269–277. [Google Scholar] [CrossRef]
- Armstrong, D.; Shen, G.; Petocz, P.; Darendeliler, M.A. A Comparison of Accuracy in Bracket Positioning between Two Techniques—Localizing the Centre of the Clinical Crown and Measuring the Distance from the Incisal Edge. Eur. J. Orthod. 2007, 29, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Deahl, S.T.; Salome, N.; Hatch, J.P.; Rugh, J.D. Practice-Based Comparison of Direct and Indirect Bonding. Am. J. Orthod. Dentofac. Orthop. Off. Publ. Am. Assoc. Orthod. Its Const. Soc. Am. Board. Orthod. 2007, 132, 738–742. [Google Scholar] [CrossRef] [PubMed]
- Dindaroğlu, F.; Doğan, E.; Doğan, S. The Evaluation Of Clinical Chair Time And Bracket Failure Amount Between Direct And Indirect Bonding Methods. J. EGE Univ. Sch. Dent. 2016, 37, 120–125. [Google Scholar] [CrossRef]
- Aguirre, M.J.; King, G.J.; Waldron, J.M. Assessment of Bracket Placement and Bond Strength When Comparing Direct Bonding to Indirect Bonding Techniques. Am. J. Orthod. 1982, 82, 269–276. [Google Scholar] [CrossRef] [PubMed]

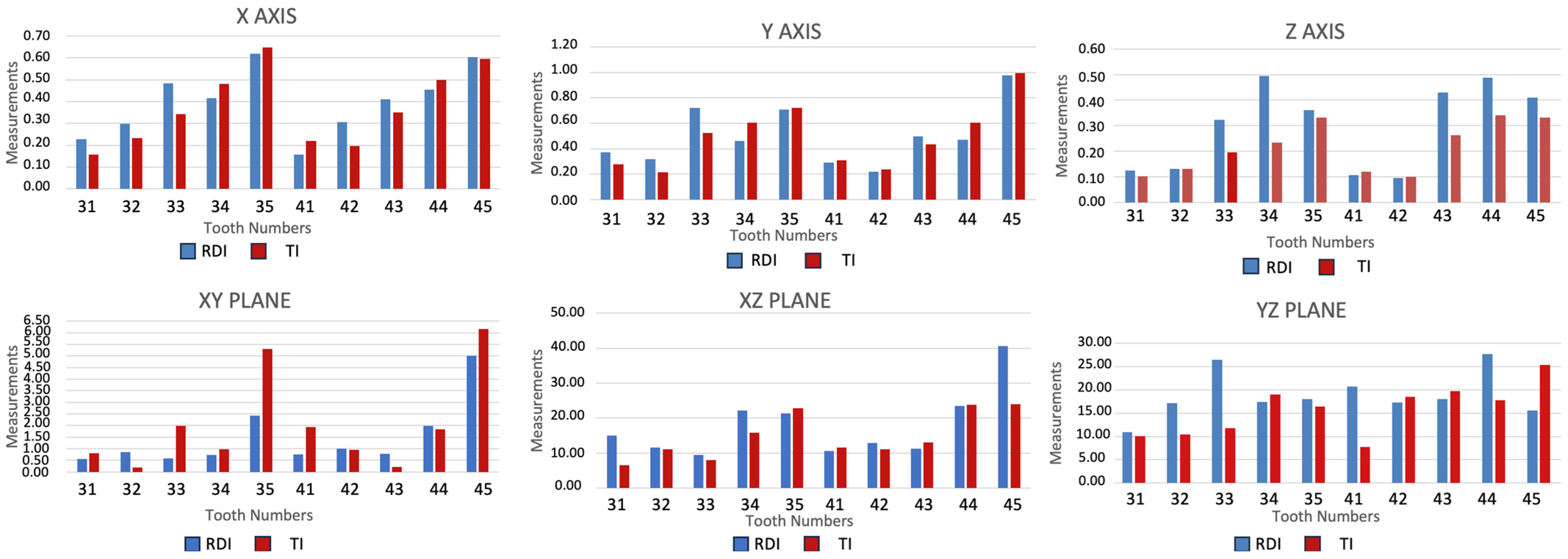
| X | Y | Z | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | RDI | TI | RDI | TI | RDI | TI | |||
| Mean ± SD | Mean ± SD | p | Mean ± SD | Mean ± SD | p | Mean ± SD | Mean ± SD | p | |
| 31 | 0.23 ± 0.15 | 0.16 ± 0.11 | 0.180 | 0.37 ± 0.23 | 0.28 ± 0.20 | 0.192 | 0.12 ± 0.11 | 0.10 ± 0.06 | 0.862 |
| 32 | 0.30 ± 0.23 | 0.23 ± 0.19 | 0.196 | 0.32 ± 0.17 | 0.21 ± 0.16 | 0.043 | 0.13 ± 0.11 | 0.13 ± 0.09 | 0.799 |
| 33 | 0.49 ± 0.36 | 0.34 ± 0.22 | 0.173 | 0.72 ± 0.31 | 0.52 ± 0.31 | 0.04 | 0.32 ± 0.22 | 0.20 ± 0.16 | 0.056 |
| 34 | 0.42 ± 0.36 | 0.48 ± 0.28 | 0.926 | 0.46 ± 0.35 | 0.60 ± 0.40 | 0.201 | 0.49 ± 0.26 | 0.23 ± 0.18 | 0.002 |
| 35 | 0.62 ± 0.38 | 0.65 ± 0.38 | 0.497 | 0.71 ± 0.58 | 0.72 ± 0.47 | 0.718 | 0.36 ± 0.19 | 0.33 ± 0.33 | 0.327 |
| 41 | 0.16 ± 0.12 | 0.22 ± 0.17 | 0.891 | 0.29 ± 0.20 | 0.31 ± 0.23 | 0.841 | 0.11 ± 0.10 | 0.12 ± 0.08 | 0.429 |
| 42 | 0.31 ± 0.21 | 0.20 ± 0.12 | 0.643 | 0.22 ± 0.21 | 0.24 ± 0.21 | 0.82 | 0.10 ± 0.05 | 0.10 ± 0.05 | 0.355 |
| 43 | 0.41 ± 0.25 | 0.35 ± 0.23 | 0.254 | 0.50 ± 0.25 | 0.44 ± 0.26 | 0.398 | 0.43 ± 0.29 | 0.26 ± 0.21 | 0.091 |
| 44 | 0.46 ± 0.41 | 0.50 ± 0.45 | 0.862 | 0.47 ± 0.38 | 0.61 ± 0.47 | 0.429 | 0.49 ± 0.22 | 0.34 ± 0.23 | 0.035 |
| 45 | 0.60 ± 0.48 | 0.60 ± 0.35 | 0.958 | 0.97 ± 0.74 | 0.99 ± 0.63 | 0.718 | 0.41 ± 0.23 | 0.33 ± 0.19 | 0.231 |
| XY | XZ | YZ | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | RDI | TI | RDI | TI | RDI | TI | |||
| Mean ± SD | Mean ± SD | p | Mean ± SD | Mean ± SD | p | Mean ± SD | Mean ± SD | p | |
| 31 | 0.55 ± 1.2 | 0.81 ± 2.6 | 0.445 | 15.1 ± 18.6 | 6.6 ± 5.6 | 0.06 | 10.9 ± 6.8 | 10.1 ± 8.8 | 0.398 |
| 32 | 0.85 ± 2.1 | 0.18 ± 0.5 | 0.495 | 11.5 ± 9.5 | 11.1 ± 17.2 | 0.478 | 17.2 ± 14.1 | 10.4 ± 12.2 | 0.096 |
| 33 | 0.58 ± 1.8 | 1.99 ± 5.2 | 0.265 | 9.49 ± 5.12 | 8 ± 6.4 | 0.201 | 26.5 ± 25.1 | 11.8 ± 8.5 | 0.021 |
| 34 | 0.73 ± 2.1 | 0.98 ± 2.7 | 0.862 | 22.2 ± 21.2 | 15.8 ± 9.6 | 0.989 | 17.5 ± 20.4 | 19 ± 17.5 | 0.64 |
| 35 | 2.4 ± 8.4 | 5.31 ± 10 | 0.028 | 21.4 ± 19.3 | 22.9 ± 21.7 | 0.82 | 18.1 ± 15.9 | 16.5 ± 11.1 | 0.883 |
| 41 | 0.76 ± 2.9 | 1.94 ± 3.6 | 0.414 | 10.6 ± 11.2 | 11.5 ± 15.4 | 0.659 | 20.8 ± 34.5 | 7.8 ± 7.2 | 0.021 |
| 42 | 0.99 ± 2.9 | 0.94 ± 3.7 | 0.779 | 12.9 ± 13.2 | 11.1 ± 16.4 | 0.565 | 17.3 ± 14.8 | 18.5 ± 26.5 | 0.265 |
| 43 | 0.78 ± 2.7 | 0.23 ± 0.8 | 0.102 | 11.2 ± 14.1 | 13.1 ± 18.7 | 0.779 | 18 ± 20.1 | 19.8 ± 30.1 | 0.327 |
| 44 | 1.98 ± 4.7 | 1.85 ± 4.7 | 0.134 | 23.5 ± 16 | 23.7 ± 15.8 | 0.82 | 27.7 ± 24.9 | 17.8 ± 16.4 | 0.114 |
| 45 | 5.01 ± 9.3 | 6.17 ± 13.5 | 0.678 | 40.6 ± 29.4 | 23.9 ± 18.3 | 0.043 | 15.6 ± 9.8 | 25.4 ± 33 | 0.925 |
| RDI | TI | |||||||
|---|---|---|---|---|---|---|---|---|
| Chair Time | Mean | Median | SD | Mean | Median | SD | t Value | p |
| Time (min) | 20.38 | 20.38 | 0.22 | 16.47 | 16.59 | 0.63 | 25.344 | <0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sezen Erhamza, T.; Küçük, K.C.; Malikov, İ. Comparative Effects of Rubber Dam and Traditional Isolation Techniques on Orthodontic Bracket Positioning: A 3D Digital Model Evaluation. Appl. Sci. 2025, 15, 2552. https://doi.org/10.3390/app15052552
Sezen Erhamza T, Küçük KC, Malikov İ. Comparative Effects of Rubber Dam and Traditional Isolation Techniques on Orthodontic Bracket Positioning: A 3D Digital Model Evaluation. Applied Sciences. 2025; 15(5):2552. https://doi.org/10.3390/app15052552
Chicago/Turabian StyleSezen Erhamza, Türkan, Kadir Can Küçük, and İsmayil Malikov. 2025. "Comparative Effects of Rubber Dam and Traditional Isolation Techniques on Orthodontic Bracket Positioning: A 3D Digital Model Evaluation" Applied Sciences 15, no. 5: 2552. https://doi.org/10.3390/app15052552
APA StyleSezen Erhamza, T., Küçük, K. C., & Malikov, İ. (2025). Comparative Effects of Rubber Dam and Traditional Isolation Techniques on Orthodontic Bracket Positioning: A 3D Digital Model Evaluation. Applied Sciences, 15(5), 2552. https://doi.org/10.3390/app15052552







