Abstract
Three-dimensional printing has significantly transformed the design and manufacture of robotic prostheses, making these devices more accessible, customized, and functional. This paper examines the historical evolution of prosthetic technology, tracing its development from rudimentary mechanical devices to the integration of advanced technologies, such as 3D printing. This innovation has enabled the production of prostheses at lower costs while enhancing their adaptability and performance. The review highlights how 3D printing has driven a disruptive shift in prosthetic customization, and how emerging technologies—including smart materials and artificial intelligence—have expanded the capabilities of prosthetic devices, offering more adaptive and natural movements. However, challenges persist, particularly regarding the need for standardization and infrastructural expansion to ensure equitable access to these technologies. Future research into novel materials and manufacturing techniques holds the potential to further improve the functionality, affordability, and accessibility of prosthetic devices. In conclusion, while 3D printing has marked a significant milestone in the evolution of robotic prosthetics, overcoming existing challenges is essential to realize its global impact and benefits fully.
1. Introduction
Prostheses have historically served as essential tools for enhancing the quality of life for individuals with amputations or physical disabilities. Technological advancements over the centuries have facilitated the development of increasingly functional and aesthetically refined prosthetic devices. However, high production costs and the limited accessibility of advanced technologies have constrained access to high-quality prostheses for many patients, particularly in developing countries where healthcare and insurance systems often lack the resources to support costly prosthetic options. Traditional manufacturing processes contribute to the high price of robotic prosthetics due to expensive materials and labor-intensive fabrication techniques. In contrast, 3D printing technology, which has emerged as a transformative force over the past two decades, offers more affordable, customizable, and efficient solutions, even though initial prototyping can still be costly. The long-term potential for reducing production costs and facilitating local manufacturing, however, has made 3D printing a promising approach to expanding accessibility and personalizing prostheses to better meet individual needs [1].
Three-dimensional printing has revolutionized numerous fields, including engineering and medicine. Its capability to produce three-dimensional objects from digital designs by sequentially depositing material layers has significantly impacted healthcare, enabling the creation of highly personalized medical devices that can be manufactured closer to the point of care. In the realm of robotic prosthetics, 3D printing allows for the creation of devices precisely matched to the anatomical requirements of each patient, thereby enhancing both functionality and comfort [2]. Compared to traditional prosthetic manufacturing, which often requires significant customization expenses, 3D printing provides an adaptable and cost-effective production method that lowers the financial barrier for patients and healthcare providers alike, especially in resource-limited settings.
Traditional robotic prosthetics have been characterized by costly materials and complex manufacturing processes, limiting their accessibility to a broad segment of the population. In contrast, the integration of 3D printing has notably reduced production costs, enabling the development of affordable, functional, and aesthetically customized prostheses [3]. This technology not only offers increased design flexibility—facilitating the creation of modular prostheses that can be easily adapted and updated as patient needs evolve—but also has the potential to significantly reduce healthcare system expenditures over time by enabling local and scalable prosthetic production.
This paper aims to review recent advancements in the field of robotic prosthetics produced through 3D printing, as well as to address current challenges and future prospects. In this review, a comprehensive overview of the current state of this technology is presented, emphasizing its impact on improving the quality of life for amputees and identifying areas where further research can optimize both functionality and accessibility.
2. The Necessity of 3D Printing in Robotic Prosthesis Development
Three-dimensional printing has revolutionized the field of robotic prostheses by providing a rapid, customizable, and cost-effective alternative to traditional manufacturing. Traditional prosthesis production often involves lengthy processes, from casting molds to assembling each component by hand, which can take weeks or even months. In contrast, 3D printing enables the swift production of tailored designs, significantly reducing wait times for patients and making prostheses more accessible [4].
Another major advantage of 3D printing is the flexibility it offers in the customization of prosthetic components. Every patient has unique anatomical and functional requirements, and 3D printing allows for a high degree of customization to fit these needs. Adjustments, such as adapting the prosthesis shape to the patient’s limb or incorporating specific functional mechanisms, can be rapidly iterated, helping to refine fit and comfort before final production. This capability is essential for the effective integration of robotic elements, such as sensors and actuators, that require exact placements and housings [5].
Furthermore, 3D printing enables resource-limited regions and non-profit initiatives to provide prosthetic solutions at a fraction of the cost of traditional methods. Organizations like e-NABLE leverage 3D printing to create prosthetic limbs that are affordable and can be produced locally, reducing the logistical complexities associated with importing expensive devices. By using locally available materials and simplified assembly processes, 3D printing supports prosthetic distribution in underserved areas where advanced medical equipment may not be readily accessible [6].
In addition to reducing costs, the material versatility offered by 3D printing allows for innovations in the use of lightweight, durable materials suited to withstand daily wear. As 3D printing materials and techniques advance, the potential to integrate sensory and adaptive technologies directly into the printed components themselves is becoming feasible, paving the way for even more sophisticated prosthetic designs [7].
3. A Brief History of Prostheses
Prostheses have a history that extends back thousands of years. Over the centuries, technological advances and material innovations have transformed prosthetics from simple mechanical replacements into highly sophisticated devices, such as modern robotic prosthetics. This progress has significantly improved the quality of life for individuals with physical disabilities, reflecting a gradual evolution from basic functionality to advanced systems that closely mimic natural movement and adaptability. Table 1 is a historical overview of prosthetic evolution, from early rudimentary models to contemporary innovations (the table is not a complete chronology; it is only a representation with some relevant examples).
Early prosthetics, dating back to ancient civilizations, were crafted from basic materials like wood, metal, and leather, primarily aimed at restoring fundamental functionality. Contrary to the view that these devices served purely aesthetic purposes, historical records reveal practical applications. For instance, the iron hand of Roman General Marcus Sergiu represents one of the earliest functional prosthetic devices specifically designed for combat, highlighting both its utility and symbolic importance [8]. Similarly, the discovery of an artificial toe on an Egyptian mummy, dating back to 950–710 B.C., Figure 1, illustrates early efforts to meet both functional and aesthetic needs in limb replacement [9]. These examples underscore that ancient prosthetics served purposes beyond appearance, demonstrating that designers valued usability alongside visual aspects.
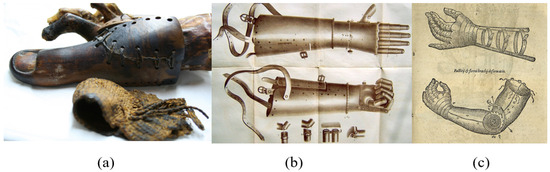
Figure 1.
(a) Egyptian toe prosthesis made of wood and leather, (b) iron leg prosthesis used by soldiers in the Crusades, (c) the “Voltaic Arm”, introduced by Sir James Syme [10].
In the mid-20th century, the first robotic prosthetics emerged, driven by a need to provide functional solutions for war veterans. These devices introduced electrically controlled mechanisms that enabled more complex movements. A significant milestone was reached in 1919 with the development of the first externally powered prosthesis, utilizing pneumatic and electric systems, thus marking a pivotal point in prosthetic innovation. However, these early robotic devices faced limitations, including high production costs, significant weight, and limited customization, which hindered widespread adoption. Despite being a breakthrough, early robotic prosthetics were often constructed from expensive materials and required complex manufacturing processes that did not adapt readily to individual anatomy, making them less practical for broader use [1].
During the 1970s and 1980s, advancements in materials science and electronics significantly improved the functionality, durability, and comfort of prosthetics (Figure 2). The introduction of lightweight materials, such as carbon fiber composites, not only enhanced the resilience of prosthetic devices but also made them more comfortable, thus better replicating the appearance and functionality of natural limbs. Recent advancements in bionic and myoelectric prosthetics have further enabled users to control artificial limbs through residual muscle signals, translating these signals into fluid, precise movements for enhanced daily functionality.
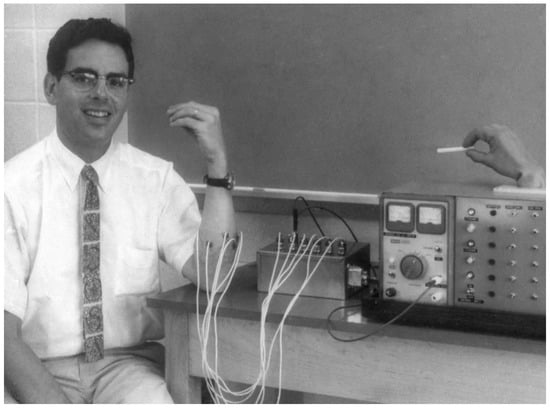
Figure 2.
Design of an externally powered artificial elbow for electromyographic control, developed in 1966 by MIT’s Research Laboratory of Electronics [11].
The integration of 3D printing technology has also revolutionized the field, allowing for the rapid, cost-effective customization of prosthetics tailored to individual needs. Not only does 3D printing expedite production, but it also reduces costs, making advanced prosthetics more accessible. Concurrently, neural interface technology is advancing toward connecting prosthetic devices directly with the nervous system to provide sensory feedback. Although still in its developmental stages, this technology holds the potential to revolutionize prosthetics by allowing users to experience sensation through their devices, bringing them closer to full integration between humans and machines. One of the first 3D-printed prostheses to make a big impact was made by Anatomics, an Australian medical device manufacturer, in late 2015, and a medical team led by neurosurgeon Ralph Mobbs successfully implanted two 3D-printed artificial vertebrae in a patient (Figure 3).
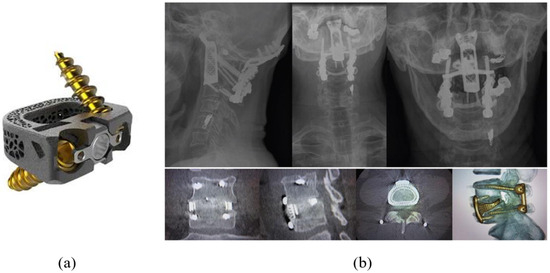
Figure 3.
(a) Three-dimensional-printed artificial vertebrae; (b) prosthesis implanted in a patient; the figure shows the progress over time, demonstrating solid mature fusion, no failure of fixation, and no subsidence [12].
Additionally, artificial intelligence (AI) is playing a critical role in adaptive prosthetics, enabling devices to learn and adjust to users’ movements and preferences. These “smart” prosthetics analyze user movement patterns and adjust in real time to provide smoother, more natural motion. Such advances are transforming the industry, delivering affordable, customized options that enhance both comfort and control, illustrating how the field has evolved to meet both the functional and emotional needs of users [13].


Table 1.
Evolution of prosthetic technology.
Table 1.
Evolution of prosthetic technology.
| Period | Description | Example | Materials Used | Technology/Innovation |
|---|---|---|---|---|
| Antiquity [14] | First prostheses with both functional and aesthetic purposes. | Egyptian toe prosthesis made of wood and leather (950–710 B.C.) and the iron hand of Roman General Marcus Sergius, designed for combat. | Wood, leather, metal, iron | Manual craftsmanship |
| Middle Ages [15] | Limited advancements; prostheses used for knights in battle, serving both functional and symbolic roles. | Iron leg prosthesis used by soldiers in the Crusades, showcasing both utility and status. | Iron, leather, wood | Manual adjustments and basic mechanisms |
| Renaissance [16] | Mechanical innovations for limb prostheses, improving mobility and articulation. | Prosthetic hand created by Ambroise Paré in the 16th century, featuring joint mechanisms for improved grip. | Wood, iron, leather, paper | Basic hinge mechanisms |
| Nineteenth century [2] | Development of functional prostheses with greater mobility; introduction of arm hooks for work tasks. | The “Voltaic Arm”, introduced by Sir James Syme, allowing for greater functionality with mechanical fingers. | Metal, rubber, leather | Movements controlled by belts and pulleys |
| Twentieth century [3] | Advanced prosthetics developed after WWI and WWII, driven by the need for functional solutions for veterans. | The first externally powered prosthesis in 1919, designed by Dr. Edward Taub, using pneumatic and electric systems. | Aluminum, steel, plastic | Myoelectric control, devices operated by muscle signals |
| Late 20th century [4] | Emergence of bionic prostheses that interact with the nervous system, enhancing control and dexterity. | The “Bionic Hand” developed by Dean Kamen in the 1990s, allowing users to control movements through neural signals. | Titanium, carbon fiber, silicone | Electromyography (EMG), neural sensors |
| XXI Century [5] | Integration of advanced technologies such as 3D printing, AI, and smart materials, facilitating greater customization and accessibility. | Prosthetic limbs created using 3D printing technology by organizations like e-NABLE, providing affordable solutions for amputees. | Plastics, smart polymers, light metals | 3D printing, artificial intelligence, brain–machine interfaces (BCIs) |
4. Limitations of Early Robotic Prostheses
The development of robotic prosthetic devices began in earnest in the 1960s, aiming to restore mobility in individuals with upper limb amputations. One notable advancement from this era is the myoelectric prosthesis, which utilizes electrical signals produced by the residual muscles of the user to control the movement of the prosthetic limb. This innovative approach allowed for more natural movements compared to earlier mechanical designs, but it was not without limitations, such as sensitivity to noise and a lack of precise control over movements [6].
Contemporary research highlights the foundational contributions of pioneers like Tomovic and Schmidl, who explored biofeedback and control theory, significantly influencing the evolution of prosthetic technologies [7]. Their work laid the groundwork for modern advancements, addressing critical issues such as weight optimization, feedback control mechanisms, and practical functionality. As a result, today’s prosthetic devices benefit from improved responsiveness and user experience, showcasing the evolution from initial concepts to sophisticated solutions that enhance the quality of life for users.
4.1. Weight and Size
The first robotic prostheses were considerably heavy and bulky due to the technology available at the time. The electric motors and batteries needed to power the device added significant weight, which was uncomfortable for users and limited prolonged use [8]. The size of these components also negatively affected the aesthetics and functionality of the prosthetics, as they could not effectively mimic the natural shape and movement of a human limb.
Efforts to address weight and usability are evidenced in recent studies on lighter, efficient actuators and optimized materials [9]. Such advancements draw on historical limitations but apply modern materials science to enhance both the aesthetic and practical aspects of prosthetic devices.
4.2. Lack of Autonomy
Early myoelectric prostheses had limited autonomy due to the capacity of the available batteries. Users had to frequently recharge the prostheses, which reduced the practicality of their daily use. Battery life was insufficient for prolonged operations, compromising all-day functionality [10]. Schmidl’s recent work on optimizing battery life has provided solutions to improve prosthesis autonomy without significantly increasing weight, addressing a longstanding issue in prosthetic design [1].
4.3. Limited Control and Lack of Feedback
One of the biggest challenges for early robotic prosthetics was the lack of precise control. Although myoelectric prostheses allowed for some degree of control through muscle signals, this was limited to basic movements such as opening and closing the hand. In addition, the absence of sensory feedback meant that users could not feel contact with objects, making tasks that require fine precision difficult [11]. This lack of tactile feedback also affected the user’s learning and adaptation to the prosthesis, as the control of force and position was less intuitive than in a natural limb.
Recent research by Tomovic, building on feedback mechanisms initially conceptualized decades ago, has contributed to haptic feedback advancements that allow users to perceive tactile information, significantly improving the functionality and user experience of modern prostheses [12].
4.4. Cost and Accessibility
Another major challenge of early robotic prosthetics was their high cost. Table 2 shows a group of different robotic prostheses available on the market with their respective prices, aiming to obtain a better idea of the cost differences of modern prostheses. Since the technology involved was complex and limited in production, only a small number of people could afford to access these types of devices. This limited the mass implementation of robotic prostheses and restricted the impact they could have on the physically disabled population [13].
Today’s research in modular design and accessible materials, inspired by early limitations, has led to prostheses that are both more affordable and customizable for broader populations [14]. These modern advancements reflect the influence of early work while making prosthetics more accessible and versatile.


Table 2.
Commercial prosthesis price list.
Table 2.
Commercial prosthesis price list.
| Name of the Prosthesis | Maker | Price, USD | Features |
|---|---|---|---|
| Hero Arm [15] | Open Bionics | 3000–5000 | Lightweight, multi-grip prosthesis, compatible with children and adults, customized, bionic design |
| LUKE Arm [17] | Mobius Bionics | 100,000 | Advanced, multi-articulated prosthesis, electrode control, high precision and functionality |
| i-Limb Quantum [18] | Össur | 80,000–100,000 | Intuitive control, various grip patterns, water resistance, quick grip change |
| MyoPro [19] | Myomo | 25,000–50,000 | Arm support system, electromyographic control, movement assistant |
| Michelangelo Hand [20] | Ottobock | 60,000–75,000 | Natural look, multiple grip modes, intuitive control, rotating wrist |
| bebionic Hand | Ottobock | 40,000–60,000 | High functionality, aesthetic design, multi-grip, durable materials |
| TASKA Hand [21] | TASKA Prosthetics | 50,000–60,000 | Waterproof, multi-grip, robust and durable |
| TrueLimb | Unlimited Tomorrow | 7995 | Custom design, 3D scanning for fit, multiple color and design options |
| Nexobrace [22] | YouBionic | 1200 | Muscle control, 3D printing, customized, simple design |
| Handiii [23] | Exiii | 300–500 | Low cost, smartphone control, 3D printing, light weight |
5. Evolution of Robotic Prostheses with 3D Printing
The evolution of prosthetics has been marked by constant technological and scientific advances, from simple mechanical extensions to highly functional robotic devices. In this context, the introduction of 3D printing has represented a paradigm shift, allowing for greater customization, cost reduction, and wider access to advanced technologies. To understand the magnitude of this advance, it is important to trace the development of robotic prosthetics from their earliest mechanical designs to modern devices that combine sensors, actuators, and 3D-printed bio-compatible materials [24].
The development of 3D printing at the end of the twentieth century radically changed the landscape of the manufacture of robotic prostheses. This technology, which allows for the creation of three-dimensional objects by superimposing layers of materials, transformed the design and production processes. The ability to create custom parts accurately and quickly made it easier to adapt robotic prosthetics to the individual needs of users [25].
The e-NABLE project, launched in 2011, was one of the pioneers in the use of 3D printing to manufacture low-cost prosthetics for children (Figure 4). This project demonstrated that it was possible to produce functional devices at a fraction of the cost of traditional prosthetics, and it ushered in a trend towards democratizing access to customized robotic prosthetics [26].

Figure 4.
Low-cost prosthetics for children designed by e-NABLE project [27].
The evolution of robotic prostheses with 3D printing has allowed for the creation of devices that not only fulfill the basic functions of a prosthesis (such as replacing a lost limb), but can also incorporate advanced features such as pressure sensors, myoelectric control, and actuators that replicate complex movements. This has been made possible by the use of computer-aided design (CAD) software, which allows engineers to create highly accurate three-dimensional models that can then be printed with various materials, from plastics to light metals (Figure 5).

Figure 5.
Advanced robotic prosthesis with the ability to make a wide range of movements [16].
Three-dimensional-printed robotic prostheses have evolved at a fairly rapid pace, so Table 3 provides a summary of some of the most important events in this area. Table 3 is not a complete summary; it only shows specific events that were part of the development process of prostheses with the intervention of 3D printing.

Table 3.
Advances in 3D printing for prosthetics.
6. Advantages of Including 3D Printing in the Manufacture of Prostheses
The inclusion of 3D printing in prosthetic manufacturing has revolutionized the field of medicine and engineering, providing more accessible, personalized, and cost-effective solutions for amputees. This technology allows for the creation of customized devices adapted to the individual needs of each patient, significantly reducing production times and costs compared to traditional methods. In addition, the ability to experiment with new materials and innovative designs expands the possibilities of improving the functionality, comfort, and aesthetics of prostheses, offering a better quality of life to users.
The integration of 3D printing into robotic prosthetic manufacturing has been a disruptive breakthrough that has radically transformed the prosthetic field in terms of accessibility, customization, production time, and cost reduction. Traditionally, prosthetic manufacturing involves long, expensive, and inflexible processes, making it difficult for many people to access high-quality devices. However, the advent of 3D printing has enabled a revolutionary approach to the design and production of robotic prosthetics, democratizing access and enabling significant advances in terms of customization and functionality.
6.1. Revolution in Customization
One of the most significant changes that 3D printing brought to the realm of robotic prosthetics is the ability to customize at an unprecedented level. Through three-dimensional scans of the patient’s body, designers can create devices that perfectly adapt to each person’s anatomy, improving not only the functionality of the prosthesis but also comfort and aesthetics. This is especially relevant for children who require prostheses that can be adjusted or replaced as they grow [32]. Unlike traditional prostheses, which were often mass-produced and then adapted in a limited way to the individual needs of patients, 3D printing makes it possible to create tailor-made devices. Digital prosthetic models can be tailored exactly to the patient’s dimensions and physical characteristics, resulting in a prosthesis that is not only more comfortable but also more functional [33]. This is particularly relevant for children, whose needs change rapidly as they grow, and 3D printing makes it possible to create prostheses that can be easily adjusted or replaced (Figure 6).

Figure 6.
Three-dimensional-printed prostheses can be customized to fit the user’s size, different needs, and even personal preferences. The examples shown in the figure demonstrate the possibility of customizing the prostheses as if they were accessories [34].
Three-dimensional printing also offers the possibility of biomimetic designs, i.e., prostheses that mimic not only the shape but also the function of natural limbs. This has allowed for greater dexterity in robotic prosthetics, facilitating more precise and natural movements, something that previous technologies could not easily achieve.
6.2. Reduced Costs and Production Time
Another disruptive change brought by 3D printing was the drastic reduction in production costs. Traditionally, the manufacture of robotic prosthetics involved complex and expensive techniques, such as precision molding or machining, which meant that many people could not access advanced robotic devices. Three-dimensional printing, on the other hand, makes it possible to manufacture high-quality prostheses at a fraction of the cost, using more affordable materials such as PLA, ABS, and nylon, which have good mechanical properties for prosthetic applications [35]. Traditional robotic prosthetics can cost between $5000 and $50,000, making them inaccessible to many people, especially in developing countries [36]. In contrast, 3D printing has enabled the production of functional prostheses at a cost of between $50 and $500, depending on the complexity of the design and the materials used [37]. (This estimate is based on some commercial prosthetics and the costs that 3D-printed prosthetics can have).
This advancement has enabled more people around the world to access robotic prosthetics while significantly reducing production times. Traditional prostheses could take weeks or even months to manufacture, whereas 3D printing can produce one within days [38]. It is essential to note that 3D printing is only part of the process. Creating a complete prosthesis also involves molding the residual limb and assembling the prosthetic device, which can extend production to around a week. This shorter timeline not only benefits patients needing urgent solutions but also supports rapid, cost-effective design iterations for custom adjustments.
Below is a Table 4 showing average production times for prostheses using various technologies. These times are averages, as each prosthesis design varies significantly [39,40].

Table 4.
Comparison of production methods for prosthetics.
6.3. Innovation in Materials and Functionality
With the integration of 3D printing, designers have had access to a wider variety of materials that can better adapt to the different parts of a robotic prosthesis (Table 5). Three-dimensional printing allows for the combination of different types of materials in a single construction, such as rigid plastics for external structures and flexible materials for moving parts or contact surfaces. This ability to use multiple materials in the same printing process has made it possible to develop more functional and resistant prostheses [46].
In addition, technology has allowed for prostheses to be lighter without sacrificing durability. This has been crucial in improving comfort and usability, especially in upper-limb prosthetics, where weight is a determining factor in the user’s ability to use the device for long periods [47].


Table 5.
Comparison of materials for 3D-printed prostheses. This table highlights various materials used in 3D-printing prosthetic devices, along with their specific advantages and applications in prosthetics.
Table 5.
Comparison of materials for 3D-printed prostheses. This table highlights various materials used in 3D-printing prosthetic devices, along with their specific advantages and applications in prosthetics.
| Material Type | Characteristics | Applications in Prosthetics |
|---|---|---|
| Polylactic Acid (PLA) [48] | Biodegradable, easy to print, low strength | Suitable for basic prosthetic models and non-load-bearing components |
| Acrylonitrile Butadiene Styrene (ABS) | Durable, higher strength than PLA, resistant to impact | Used for structural components and housing for electronics |
| Nylon [48] | High flexibility, excellent strength-to-weight ratio, resistant to wear | Ideal for joints, gears, and load-bearing parts in functional prosthetics |
| Thermoplastic Polyurethane (TPU) [49] | Elastic, high resilience, and wear resistance | Used in flexible joints and sockets that require cushioning |
| Polyether Ether Ketone (PEEK) [50] | High mechanical strength, chemical, and thermal resistance | Suitable for high-performance prosthetic parts in demanding applications |
| Resin (SLA/DLP Printing) | Smooth finish, suitable for detailed parts, variable flexibility | Best for cosmetic covers and intricate parts; limited strength for structural use |
| Carbon Fiber Reinforced Polymers [2] | Lightweight with high stiffness and strength | Used in prosthetic frames and load-bearing components for high durability |
6.4. Ease of Distribution and Global Collaboration
Three-dimensional printing has revolutionized global collaboration in the development of robotic prosthetics, allowing for digital designs to be freely shared on platforms such as Thingiverse and Cults3D (Figure 7). This accessibility has fostered a collaborative environment where communities of developers, researchers, and clinicians can collectively enhance prosthetic designs, adapting them to meet specific patient needs. Additionally, nonprofits have leveraged 3D printing to distribute prosthetics to resource-limited communities—overcoming barriers previously posed by high costs and logistical challenges.
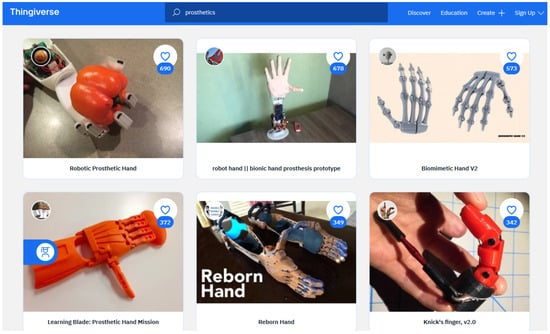
Figure 7.
Free websites allow for downloading files so anyone can build their own prosthesis [3].
However, the implementation of 3D-printed prosthetics varies significantly across countries due to differing national certification standards that ensure device safety and effectiveness. While these regulatory pathways are essential, they can also impact access and innovation, as certification processes can be lengthy and costly. For example, in the United States, the FDA requires rigorous testing and approvals for prosthetic devices, particularly those intended for children. In the European Union, the Medical Device Regulation (MDR) establishes strict certification protocols, including design transparency and quality control. Consequently, while projects like “e-NABLE” successfully distribute 3D-printed prosthetic hands to underserved regions, further adaptation is often necessary to comply with local standards and achieve formal medical certification, ensuring user safety [4,5].
The global volunteer network “e-NABLE” exemplifies this approach, using 3D printing to produce personalized prosthetic hands for children and adults and demonstrating the power of open collaboration. Volunteers design and deliver custom prosthetics to individuals who might otherwise lack access. Despite these efforts, regulatory challenges remain in securing certification for such devices across countries, where regulations vary widely and may limit their clinical use. This underscores the transformative yet complex role of 3D printing in prosthetics, balancing accessibility with regulatory compliance [6].
6.5. Rapid and Accessible Prototype Development
Three-dimensional printing has allowed researchers and designers to experiment with new concepts more quickly and cheaply, which has accelerated the development cycle of robotic prosthetics. Researchers no longer need to wait weeks to receive test prototypes. They can produce them in their own labs or workshops in a matter of hours, allowing for a rapid iteration of designs. This has not only improved the quality of the prostheses but has also allowed for further innovation in terms of functionality and design [7].
The ease with which prototypes can be modified and tweaked has significantly reduced the time between conceiving an idea and creating a viable final product. This immediate access to 3D-printed prototypes has been a crucial factor in the evolution of robotic prosthetics, where the needs of users vary greatly from person to person.
7. 3D Printing Technologies Applied to Prostheses
Three-dimensional printing has revolutionized the development of robotic prosthetics due to its versatility, accuracy, and ability to manufacture customized devices at a low cost. Several 3D printing technologies have been applied to the creation of prostheses, each with particular advantages depending on the specific needs of the patient, the type of prosthesis, and the materials used. Among the main technologies used for prosthetic manufacturing are stereolithography (SLA), selective laser sintering (SLS), and fused deposition modeling (FDM). These technologies have enabled advances in terms of functionality, durability, and accessibility, transforming the field of robotic prosthetics.
7.1. Fused Deposition Modeling (FDM)
Fused deposition modeling (FDM) is one of the most widely used 3D printing technologies for prosthetic manufacturing due to its simplicity, low cost, and ease of access (Figure 8). In this process, a filament of thermoplastic material, such as ABS or PLA, is heated and extruded through a nozzle, depositing layer-by-layer to form the prosthesis. FDM has become the preferred technology for many prosthetic manufacturers due to its low cost of materials and the availability of printers in the market, which allows both professionals and amateurs to create custom prostheses.
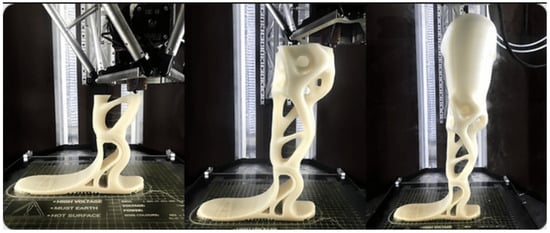
Figure 8.
UniLeg Spotlight: the world’s first complete 3D-printed below-knee prosthesis solution [8].
In addition, FDM makes it possible to manufacture lightweight but durable prosthetics, which is crucial for users who need functional devices that do not cause discomfort during prolonged use. The technology has proven particularly useful for creating upper limb prostheses, such as hands and fingers, that require a balance between structural rigidity and flexibility in moving parts [9]. However, one of the main limitations of FDM is the relatively low surface quality and limited accuracy compared to other printing technologies, which may require post-processing processes to improve the aesthetics and functionality of the device [10].
7.2. Stereolithography (SLA)
Stereolithography (SLA) is another widely used technology in the manufacture of robotic prosthetics. Unlike FDM, which uses thermoplastic filaments, SLA employs a photosensitive liquid resin that solidifies layer-by-layer when exposed to an ultraviolet laser. This allows for extremely precise details and smooth surface finishes, which are essential for prostheses that require a high degree of precision in shape and fit [1].
The SLA process is particularly suitable for creating prostheses that fit more ergonomically to the patient’s body. Due to the high resolution of the technology, it is possible to design devices with very fine details, such as joints or complex structures that better mimic the body’s natural functions (Figure 9). In addition, prostheses created with SLA often have superior aesthetics than those made with FDM, which improves the patient’s perception of the device and their willingness to use it.

Figure 9.
Three-dimensional-printed models and surgical guides are indispensable in modern dental practices, setting new standards for precision in dental surgeries [11].
However, one of the main challenges of SLA is the relatively high cost of both the equipment and the resins used, which limits its adoption in countries or regions with more limited resources [12]. However, its ability to create prostheses with high precision and its potential for design customization make this technology a preferred choice in applications where quality and fit are paramount.
7.3. Selective Laser Sintering (SLS)
Selective laser sintering (SLS) is a 3D printing technology that uses a laser to fuse dust particles from materials such as nylon or polyamide into a solid structure. This process has the advantage of being able to create prostheses without the need for support structures, which allows for more complex and robust shapes to be manufactured than with FDM or SLA [13]. In addition, prostheses made using SLS are often stronger and more durable, making them an ideal choice for users who require devices that can withstand intensive use under demanding conditions [14].
One of the biggest advantages of SLS technology is its ability to create prostheses that combine rigidity and flexibility in different areas of the same device. For example, in a prosthetic hand, the parts that make up the fingers may be made of more flexible materials to facilitate movement, while the rest of the structure may be more rigid to provide stability [15]. This versatility has allowed for the development of more advanced and functional robotic prostheses, which provide greater freedom of movement and better adaptation to the user’s daily activities (Figure 10).

Figure 10.
A Titan model finger is inserted into a 3D-printed socket that is attached to the patient’s body [16].
Although SLS is an expensive technology compared to FDM, its ability to produce highly functional and customized prosthetics has been instrumental in the evolution of robotic prosthetics. In addition, the use of more durable materials such as nylon has expanded the range of applications of these prostheses, allowing users to perform physical activities that they could not previously carry out.
7.4. Metal Powders in 3D Printing
Metal powder 3D printing is an emerging technology that has begun to be applied in the manufacture of robotic prostheses, particularly for those that require a greater structural strength, such as lower-limb prostheses. In this process, a laser is used to melt layers of metal powder, such as titanium or stainless steel, creating extremely strong and lightweight structures. This technology has been used mainly in specialized clinical settings due to its high cost, but it promises to considerably improve the durability and functionality of prostheses [2].
The use of metal materials has allowed for prostheses to be much more resistant to fatigue and wear, which is essential for users who rely on devices that support heavy loads. Although metallic 3D printing technology is still in its early stages of adoption in the prosthetic space, its long-term benefits in terms of durability and customization are undeniable [3].
Three-dimensional printing technology continues to change constantly. Table 6 shows a review of the main 3D printing technologies with some of their most important features focused on the creation of prosthetics.

Table 6.
Comparison of 3D printing technologies for prosthetics.
8. Current Challenges in the Development of 3D-Printed Prostheses
Despite the significant advances that 3D printing has brought to the field of prosthetics, there are still technical and economic challenges that limit its widespread adoption. The upfront costs of high-quality 3D printers and specialized materials remain major barriers, especially in developing countries. In addition, although technologies such as FDM and SLA allow for the rapid production of prosthetics, the time and post-processing costs to improve finishes and functionality still represent a challenge [11].
The future of 3D printing in prosthetics looks promising, with advances in hybrid technologies that combine plastic and metal materials, as well as the use of bio-compatible materials that allow for a more natural integration with the human body. More advanced 3D printers that can print on multiple materials simultaneously are also being developed, which could further expand the design and functionality possibilities of robotic prosthetics [12].
Despite significant advances in 3D printing and its application in the development of robotic prosthetics, several technical, economic, and integration challenges persist that limit its large-scale adoption. Key challenges include material optimization, prosthetic durability and functionality, advanced customization, integration with biological systems, and affordability. In addition, aspects such as regulation and standardization in the use of these technologies also play a key role in their expansion.
8.1. Material Optimization
One of the main challenges in the manufacture of robotic prostheses with 3D printing is the selection and development of materials that meet the requirements of durability, flexibility, bio-compatibility, and resistance. Although the most commonly used materials, such as PLA and ABS, are accessible and easy to print, they have limitations in terms of mechanical strength and long-term bio-compatibility. According to [13], 3D-printed materials do not always withstand prolonged use, which can lead to deformation or structural failure in prostheses.
The search for new, more robust, and flexible materials is an area of active research. Advanced polymers and hybrid composites, such as those that combine plastics with carbon fibers or metal materials, offer higher levels of durability and strength. However, these materials are often more expensive and complex to process, making them difficult to use in affordable prosthetics [14].
8.2. Durability and Functionality of Prostheses
Durability is a key concern in the design of robotic prostheses, especially those used in intensive physical activities or extreme conditions. Prostheses must be able to withstand daily wear and tear and continue to function optimally for long periods of time without the need for constant maintenance. This problem is amplified in robotic prosthetics, where the integration of electronic components and motors increases the risk of failure due to continuous use.
In addition, functionality is also a challenge. Although modern robotic prosthetics have advanced in terms of control and movement, there are still limitations in terms of the accuracy, speed, and force they can exert. Current control systems, based on myoelectric signals or sensors, do not yet allow for completely natural and precise control, making it difficult to perform complex tasks such as manipulating small objects or performing fine movements [15]. The development of more advanced control algorithms, such as those based on artificial intelligence, is helping to mitigate this problem, but implementing these systems in accessible prostheses remains a challenge.
8.3. Customization and Adjustment of Prostheses
While 3D printing has made it easier to customize prosthetics, there are still barriers in terms of perfect fit and dynamic fit. Individual differences in the anatomical and physiological characteristics of each person make the design of personalized prostheses a complex process. In many cases, even if an adequate initial adjustment is achieved, the prosthesis may not fit well over time due to changes in the user’s body, such as growth or weight changes [16].
Research into adaptive prosthetics, which can be adjusted automatically or by manual calibration, is ongoing, but the available solutions are expensive and difficult to implement in 3D-printed models. In addition, the lack of standardization in the methods of measuring and manufacturing custom prostheses adds complexity to the process.
8.4. Integration with Biological Systems
A crucial challenge in the development of advanced robotic prosthetics is efficient integration with the user’s biological systems. Myoelectric prostheses, which detect electrical signals from muscles to control the movement of the prosthesis, have made significant advances, but they still have limitations in terms of accuracy and sensitivity. The interpretation of these signals is often imperfect, leading to imprecise movements or delays in the response of the prosthesis [2].
Research on brain–computer interfaces (BCIs) has also shown a potential to improve the connection between robotic prosthetics and the human body. However, these technologies are in the early stages of development, and their implementation in affordable prostheses is not yet viable. In addition, the possibility of BCI systems being invaded by infections or biological rejections remains a major obstacle [3].
8.5. Economic Accessibility
Despite the fact that 3D printing has significantly reduced the costs of manufacturing prosthetics, access to these technologies remains limited, especially in low-income regions. While the costs of 3D-printed dentures are much lower than those of traditional dentures, they still represent a considerable investment for many individuals and families. In addition, the costs associated with the maintenance, customization, and integration of electronic components increase the total price of the device [4].
Global initiatives seeking to improve access to 3D-printed prosthetics have helped bridge this gap, but a lack of adequate infrastructure, such as access to high-quality 3D printers and materials, remains a challenge. Advances in low-cost 3D printing, as well as the availability of printing technologies in rural and developing areas, are critical to making these prostheses more accessible [5].
8.6. Regulation and Standardization
The lack of clear regulations and standardization in the use of 3D printing for prosthetics is another major challenge. Three-dimensional-printed prostheses must meet strict quality and safety standards before being used by patients, but current regulations vary widely between countries. In addition, the personalized nature of these prostheses complicates the regulation process, as each device must be adapted to the specific needs of the user.
Setting international standards for the manufacture and use of 3D-printed robotic prosthetics is crucial to ensure their quality and safety. Regulatory organizations should collaborate with engineers, manufacturers, and healthcare professionals to develop guidelines that balance technological innovation with patient protection [6].
9. Design and Manufacture of Robotic Prostheses with 3D Printing
The design and manufacture of robotic prostheses with 3D printing represent a paradigm shift in the field of biomedical engineering. These technologies make it possible to develop customized, lightweight, functional, and low-cost prostheses that are better adapted to the individual needs of users. The process of creating a robotic prosthesis includes several phases: digital design, selection of suitable materials, manufacturing using 3D printing, and integration of electronic components and actuators that enable movement. This approach has made robotic prostheses more accessible and efficient, improving the quality of life for people with disabilities.
9.1. Digital Design Phase
Robotic prosthetic design begins with the creation of a three-dimensional digital model using computer-aided design (CAD) software. This model is customized according to the anatomical characteristics of the user, allowing for a precise and comfortable fit. One of the main advantages of 3D printing is that designs can be easily modified to suit each person’s specific needs, from the length of a limb to the level of flexibility of joints [7].
CAD software allows engineers to design functional prosthetics that integrate complex structures, such as gear and joint systems, that would not be possible to manufacture using traditional methods. For example, it is possible to simulate the movement of fingers on a robotic prosthetic hand before printing, making it easier to optimize the design to improve functionality. In addition, the use of force and motion simulations in the digital design phase helps ensure that prostheses can withstand the stresses and loads of daily use without compromising their structural integrity [8].
9.2. Selection of Printing Materials
The choice of materials is crucial in the robotic prosthetic manufacturing process, as it impacts both the durability and comfort of the device. The most common materials used in prosthetic 3D printing include plastics such as PLA (polylactic acid) and ABS (acrylonitrile butadiene styrene), both of which are known for their strength, lightness, and ease of printing. In addition, for components that require flexibility, such as joints, softer materials such as TPU (thermoplastic polyurethane) or silicone can be used [9].
The flexibility of 3D printing allows for the combination of different materials in the same prosthesis. For example, in a robotic prosthetic hand, rigid parts can be made from ABS to provide structure and support, while areas that require movement or skin contact can be printed with TPU for comfort and flexibility. The ability to integrate rigid and flexible materials in the same device has been one of the most significant advances in the design of 3D-printed prostheses [10].
In addition, some researchers are exploring the use of bio-compatible materials and even recyclable materials for prosthetic printing, which not only reduces costs, but also makes prostheses more sustainable and globally accessible [1].
9.3. Printing and Post-Processing Phase
Once the digital model has been designed and the materials selected, the next step is the printing of the prosthesis. At this point, 3D printing technologies such as fused deposition modeling (FDM), stereolithography (SLA), and selective laser sintering (SLS) are applied to manufacture the prosthesis layer-by-layer. Each technology has its own advantages and challenges: while FDM is more accessible and economical, SLA and SLS offer greater accuracy and better surface finishes, which is critical in prostheses that require an ergonomic and aesthetic fit [11].
Post-processing is an important stage that is often overlooked. This includes cleaning the part, sanding to improve surface smoothness, and, in some cases, assembling multiple parts if the prosthesis has multiple components. In robotic devices, this stage also includes the integration of sensors, motors, and electronic systems that allow for movement control. For example, in a robotic hand, servo motors can be integrated to provide precise finger movements, while pressure sensors allow the user to regulate the force with which an object is gripped [12].
9.4. Electronics and Control Integration with 3D Printing
One of the most distinctive features of robotic prostheses is the ability to interact with the environment through integrated actuators and sensors. At the final manufacturing stage, electronic components are assembled to enable precise prosthesis control. This includes installing microcontrollers, such as Arduino or Raspberry Pi, servo motors for limb movement, and environmental sensors, such as pressure or temperature sensors. While 3D printing primarily focuses on creating the structural components, it offers the advantage of customizable designs that simplify the housing and placement of electronics within the prosthetic device, making it easier to incorporate more sophisticated control systems at a lower cost.
A major advancement in this field is the use of myoelectric signals, where sensors placed on the skin detect muscle electrical signals, which are then interpreted by a microcontroller to translate the user’s intentions into movement. This type of control, enabled by precise electronic integration, is particularly beneficial for upper-limb prostheses that require nuanced grip and motion control for everyday tasks. With 3D-printed prosthetics, customized sensor placements and module housings can be incorporated into the design, allowing for quick iterations that enhance the prosthesis’s comfort and functionality [13].
In addition, the integration of artificial intelligence and machine learning has opened new possibilities for adaptive prostheses, where devices adjust to user needs by analyzing movement patterns. These technologies improve control accuracy and energy efficiency, which, in turn, extends battery life and device longevity. For instance, adaptive grip mechanisms can now be 3D-printed directly into the design to allow for responsive feedback adjustments in real-time—a feature that significantly improves the user experience in both comfort and functionality [14,15]. This combination of 3D printing and intelligent control systems demonstrates how rapid prototyping can support continuous development and adaptability in prosthetic technology. Figure 11 shows a flow chart explaining the overall process required to create a 3D-printed prosthesis.
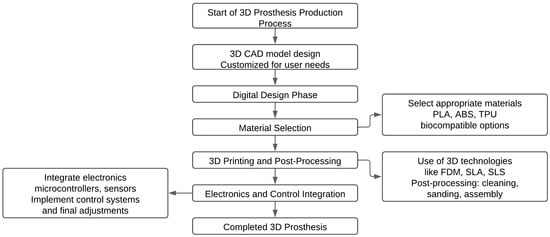
Figure 11.
Workflow for the production of robotic prostheses using 3D printing.
10. Social Impact and Clinical Applications of Robotic Prostheses with 3D Printing
The integration of 3D printing into the development of robotic prostheses has had a transformative impact on both societal and clinical levels. This technology has revolutionized how prosthetics are designed and manufactured, improving accessibility and enhancing rehabilitation options, which collectively contribute to a better quality of life for patients. Below, we analyze the primary social and clinical impacts of 3D-printed prostheses.
10.1. Democratization of Access to Customized Prosthetics
Historically, traditional prosthetics have been costly and difficult to obtain, especially in resource-limited settings. However, 3D printing allows for the production of low-cost robotic prosthetics, expanding access to a wider population. Nonprofit organizations, such as e-NABLE, have adopted 3D printing to create and distribute affordable prosthetic hands and arms, making functional devices accessible to individuals who might otherwise be unable to afford them [16].
Example and Impact: In e-NABLE projects, volunteers collaborate globally to design custom prosthetics that can be tailored to the needs of each user, including options for color and style. This initiative exemplifies how 3D printing democratizes medical device access, significantly improving the lives of economically disadvantaged patients and demonstrating the impact of open-source prosthetic design.
3D Printing Advantage: The speed and low cost of 3D printing allow for rapid and affordable customization, providing a viable solution for populations in need of frequently adjusted prostheses, such as children who outgrow devices quickly.
10.2. Empowerment and Quality of Life Enhancement
The functionality and aesthetic flexibility of 3D-printed robotic prosthetics have redefined societal perceptions of disability by enabling users to perform everyday tasks independently and participate more fully in recreational and work-related activities. This empowerment not only boosts quality of life but also grants individuals greater autonomy. By allowing users to customize prosthetics not only for fit but also for appearance, 3D printing enables a unique personalization that enhances self-esteem and confidence.
Example and Impact: Individuals with access to 3D-printed prosthetics, capable of integrating myoelectric or brain–computer interface control, report improvements in daily task performance, such as handling small objects or engaging in activities requiring dexterity. This functional customization is critical in restoring user independence and confidence (Figure 12).

Figure 12.
Three-dimensional-printed enhanced prosthetics allow patients to access activities that would have been previously impossible, such as riding a bicycle [2].
3D Printing Advantage: The versatility of 3D printing enables prosthetic designs that reflect personal identity, contributing to users’ self-confidence and providing tangible improvements in lifestyle. Additionally, 3D-printed prosthetics are designed with easy replacement parts, which lower maintenance barriers for users.
10.3. Reduction in Clinical Treatment Costs
In the clinical context, 3D printing significantly reduces the costs associated with prosthetic design and production. While traditional prosthetics can be prohibitively expensive, a 3D-printed robotic prosthesis can be produced for a fraction of the price, enabling hospitals and clinics to serve more patients within the same budget constraints [3]. This cost reduction is particularly beneficial in public health systems with limited resources and high demand.
Example and Impact: Hospitals in regions with constrained healthcare budgets have implemented 3D printing labs to produce prosthetics in-house, allowing them to deliver personalized devices at a fraction of traditional costs and often within shorter lead times.
3D Printing Advantage: By simplifying the supply chain and reducing material costs, 3D printing minimizes both initial expenses and long-term maintenance, facilitating widespread clinical adoption and enabling more equitable healthcare access.
10.4. Clinical Applications and Customization of Prosthetics
The adaptability of 3D printing technology has facilitated the production of prosthetics tailored to specific patient needs in ways not previously possible. Three-dimensional scanners capture precise anatomical data, enabling engineers to design prosthetics that fit each individual’s body with precision. This high level of customization enhances comfort and minimizes the risk of complications like skin irritations or sores often associated with poorly fitted traditional prostheses [4].
Example and Impact: The ability to create patient-specific devices quickly has made 3D printing invaluable in rehabilitation settings. For example, transitional prosthetics printed in-house can help patients gradually adapt to more advanced devices, improving outcomes and reducing complication rates.
3D Printing Advantage: The customization afforded by 3D printing not only improves the fit and comfort of prostheses but also enables rapid adjustments and improvements, offering patients devices that evolve with their rehabilitation needs.
10.5. Social Impact on Labor and Social Inclusion
Three-dimensional-printed robotic prostheses have proven to have a significant impact on labor inclusion and social participation for individuals with disabilities. By providing prosthetics that combine functionality with aesthetic appeal, 3D printing enables individuals with physical disabilities to re-enter competitive job markets, reducing stigma associated with limb loss. This improvement is especially relevant in fields requiring manual skills where precise movement is essential [5].
Example and Impact: In addition to enhancing employability, the availability of affordable prosthetics has encouraged social engagement by allowing users to participate in recreational, sports, and cultural activities previously limited by their disability.
3D Printing Advantage: Through reduced production costs and high customization capabilities, 3D printing not only improves functional capabilities for work and social activities but also promotes social inclusion by breaking down physical and psychological barriers associated with traditional prostheses.
11. Future Perspectives in the Design and Manufacture of Robotic Prostheses with 3D Printing
The future of robotic prostheses made with 3D printing promises even more profound transformations in the medical and social spheres. With the continuous advancement in technology, materials, and impression techniques, robotic prosthetics are on the threshold of a new era of customization and functionality. Future prospects range from the integration of emerging technologies to the expansion in global access, which could redefine the impact and effectiveness of these solutions on the lives of people with disabilities.
11.1. Advances in Printing Materials and Techniques
One of the most promising developments in 3D printing for robotic prosthetics is innovation in materials. Researchers are exploring new types of polymers and compounds that offer improved properties, such as increased strength, flexibility, and biocompatibility. Smart materials, which respond to external stimuli such as temperature and humidity, could allow for the creation of prostheses that automatically adjust to changing environmental or user conditions [6].
In addition, 3D printing techniques are evolving towards faster and more accurate methods. Multi-material 3D printing and 4D printing, where materials change shape in response to stimuli, are beginning to influence the design of robotic prosthetics. These advances could allow for the manufacture of prostheses that dynamically adapt to the needs of the user and environmental conditions, thus improving functionality and durability [7].
11.2. Integration of Emerging Technologies
The convergence of 3D printing with other emerging technologies, such as artificial intelligence (AI) and advanced robotics, is opening up new possibilities for prosthetic design. AI algorithms can improve the control of robotic prosthetics by interpreting signals from myoelectric or other sensors more accurately. The integration of machine learning systems will allow prostheses to adapt and optimize their operation based on the user’s activity, offering a more natural and efficient experience [8].
Augmented reality (AR) and virtual reality (VR) are also beginning to play a role in prosthetic design and rehabilitation. These technologies can be used to simulate the use of a prosthesis in a virtual environment, allowing users to train and adapt to their device before physically receiving it. This approach could improve rehabilitation outcomes and facilitate faster and more effective adaptation [9].
11.3. Advanced Customization and Customization
Customization will continue to be one of the main areas of development for 3D-printed robotic prosthetics. Advances in 3D scanning and digital modeling will allow for more precise adaptation to patients’ individual anatomical characteristics. Future prosthetics could incorporate automatic adjustment systems that adapt to changes in the user’s body shape over time, providing a more comfortable and functional fit [10].
Customization will also extend to the integration of brain–computer interfaces (BCIs), which could allow for more intuitive and natural control of prosthetics. Research into advanced neural interfaces is progressing, and in the future, we could see prosthetics that connect directly with the wearer’s nervous system, offering seamless integration and a more precise response to neuromuscular signals [1].
11.4. Global Access and Cost Reduction
One of the main promises of the future of 3D-printed robotic prosthetics is the expansion of their global access. With the continued reduction in 3D printing costs and the increased availability of printing technologies in disadvantaged regions, these prostheses are likely to become a viable option for a greater number of people around the world. Non-profit initiatives and grant programs could play a crucial role in expanding this access, ensuring that innovations in robotic prosthetics benefit communities in need [11].
Collaboration between governments, international organizations, and technology companies will be essential to develop strategies to reduce the cost of prostheses and improve the infrastructure needed for their manufacture and distribution. Public policies and international cooperation efforts will be critical to ensure that the benefits of 3D-printed robotic prosthetics are equitably distributed globally [12].
11.5. Global Regulation and Standards
Finally, the creation of global standards and clear regulations will be crucial for the future development of robotic prosthetics with 3D printing. Standardizing manufacturing processes, quality testing, and safety requirements will ensure that prosthetics are safe and effective for users worldwide. Collaboration between standards bodies, manufacturers, and healthcare professionals will be essential to develop and implement these standards [13].
Creating a unified regulatory framework will help ensure that innovations in 3D-printed robotic prosthetics are not only technologically advanced, but also safe and accessible to all. Implementing these standards will contribute to trust in the technology and promote its widespread adoption.
12. Discussion
The integration of 3D printing into the design and manufacture of robotic prostheses represents a significant advance in medical technology, offering a number of benefits that transform both the clinical and social spheres. This discussion explores the implications of these advances, analyzing the impact on the accessibility, customization, and functionality of prostheses, and addressing the challenges that still persist in this field.
One of the greatest achievements of 3D printing in the field of robotic prosthetics has been the reduction of costs and the democratization of access to personalized devices. Traditional, often prohibitively expensive, prosthetics have been replaced by 3D-printed alternatives that offer an economical solution without compromising quality. This has been particularly beneficial for populations in developing countries and for families with limited resources. The ability to manufacture prostheses at a low cost has allowed organizations such as e-NABLE to provide functional devices to a greater number of people, contributing to a significant improvement in quality of life [14].
However, cost reduction is not the only factor at play. The ability to customize prostheses to fit the user’s individual needs is another crucial aspect. This customization not only improves the comfort and functionality of the prostheses, but also allows for a more precise fit and better performance in the wearer’s daily life [10]. Three-dimensional printing facilitates this level of customization through the use of 3D scans and digital modeling, resulting in devices that more precisely match the patient’s anatomical features [15].
Continuous development in materials and impression techniques has expanded the capabilities of robotic prosthetics. Advanced materials and multidimensional printing techniques make it possible to create prostheses with improved properties, such as greater strength, flexibility, and adaptability. Four-dimensional printing, where materials respond to external stimuli, opens up new possibilities for the design of prostheses that adapt to changing environmental conditions.
The integration of emerging technologies, such as artificial intelligence and brain–computer interfaces, promises to take the functionality of robotic prosthetics to an even higher level. AI algorithms can improve the control of prostheses by interpreting myoelectric signals more accurately, while advanced neural interfaces could allow for more intuitive and natural control. These innovations have the potential to deliver a more natural and efficient user experience, moving ever closer to full integration with the user’s neuromuscular system.
Despite significant advances, there are still challenges that need to be addressed to maximize the impact of 3D-printed robotic prosthetics. One of the main challenges is global standardization and regulation. The lack of a unified regulatory framework can lead to inconsistencies in the quality and safety of prostheses. The creation of global standards and the implementation of clear regulations are essential to ensure that prostheses are safe and effective.
In addition, although 3D printing has reduced costs, the infrastructure for the manufacture and distribution of prosthetics remains limited in many regions. The global expansion of technology and access to resources are crucial to ensure that the benefits of robotic prosthetics reach the communities most in need. Collaboration between governments, international organizations, and businesses will be critical to overcoming these barriers and improving accessibility.
Finally, the adaptation of prostheses to the changing needs of the user and to environmental conditions remains an active area of research. The development of prostheses that can be dynamically adjusted and adapted to different situations will represent an important advance in the functionality and usefulness of these devices.
13. Conclusions
Three-dimensional printing has revolutionized the design and manufacture of robotic prosthetics, offering a number of significant advantages that transform the field of prosthetics. Through this technology, a notable reduction in production costs has been achieved, allowing prostheses to be more accessible to people with disabilities around the world. The ability to customize these devices to fit individual anatomical features and specific user needs has significantly improved their functionality and comfort.
Advances in printing materials and techniques, such as 4D printing and the use of smart materials, have expanded the capabilities of robotic prosthetics, allowing for greater adaptability and strength. The integration of emerging technologies, such as artificial intelligence and brain–computer interfaces, promises to further improve the accuracy and naturalness of prosthetic control, approaching full integration with the user’s neuromuscular system.
However, despite these advances, challenges remain that need to be addressed to maximize the positive impact of 3D-printed robotic prosthetics. A lack of standardization and global regulation can lead to inconsistencies in device quality and safety. Expanding infrastructure for manufacturing and distribution, as well as developing strategies to improve access in disadvantaged regions, are crucial to ensure that the benefits of these technologies are equitably distributed.
In conclusion, as the field of 3D-printed robotic prosthetics continues to advance, it is essential to continue addressing these challenges to fully realize the potential of this technology. The combination of technological advances with a strategy focused on accessibility and standardization will allow 3D-printed robotic prostheses to have an even greater impact on the lives of people with disabilities, promoting greater equality of opportunities and an improvement in the quality of life globally.
Author Contributions
Conceptualization, M.S. and P.P.; Methodology, M.S.; Formal Analysis, M.S. and P.P.; Investigation, M.S. and P.P.; Data Curation, M.S. and P.P.; Writing—Original Draft Preparation, M.S.; Writing—Review and Editing, M.Z. and R.R.; Supervision, P.P.; Validation, M.Z. and R.R. All authors have read and agreed to the published version of the manuscript.
Funding
The authors declare having received the following financial support for the research, authorship, and/or publication of this article: this work was supported by the Instituto Tecnológico Superior Rumiñahui as part of the research department.
Acknowledgments
The activities that gave rise to the results presented were carried out in the context of the project to develop a fruit-harvesting robot. This project is in its initial stage, and the research gave rise to the results presented, with the support of the Rumiñahui University Institute. We deeply appreciate the collaboration of all the researchers, students, and professionals involved in this project, whose dedication and effort have been fundamental to achieving our objectives.
Conflicts of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Gretsch, K.F.; Lather, H.D.; Peddada, K.V.; Deeken, C.R.; Wall, L.B.; Goldfarb, C.A. Development of novel 3D-printed robotic prosthetic for transradial amputees. Prosthet. Orthot. Int. 2016, 40, 400–403. [Google Scholar] [CrossRef] [PubMed]
- Pozo, P.M. PRÓTESIS ROBÓTICAS: Una Revisión Sistemática de la Literatura. ResearchGate. 2021. Available online: https://www.researchgate.net/publication/350734513_PROTESIS_ROBOTICAS_una_Revision_Sistematica_de_la_Literatura_ROBOTIC_PROSTHESES_a_Systematic_Review_of_the_Literature (accessed on 20 November 2024).
- OOrtiz-Catalan, M.; Zbinden, J.; Millenaar, J.; D’Accolti, D.; Controzzi, M.; Clemente, F.; Cappello, L.; Earley, E.J.; Mastinu, E.; Kolankowska, J.; et al. A highly integrated bionic hand with neural control and feedback for dexterous manipulation. Sci. Robot. 2023, 8, eabf7360. [Google Scholar] [CrossRef] [PubMed]
- Giraldi, S.; Chiarella, M.; García Alvarado, R.; Gatica, B. Prótesis Robóticas y Pieles Dinámicas: Programación Visual y Código Abierto como Integración Contextual de Sistemas Industriales Cerrados. In Proceedings of the ACSA International Proceedings, Santiago, Chile, 29 June–1 July 2016; Available online: https://www.acsa-arch.org/chapter/protesis-roboticas-y-pieles-dinamicasprogramacion-visual-y-codigo-abiertocomo-integracion-contextual-desistemas-industriales-cerrados/ (accessed on 3 October 2024).
- Espinosa, F. Desarrollo de un Prototipo de Mano robóTica Utilizando Mecanismos Metamórficos. Master’s Thesis, Universidad Tecnológica de la Mixteca, Huajuapan de León, Mexico, 2019. Available online: https://revistas.iudigital.edu.co/index.php/ids/article/view/139 (accessed on 20 November 2024).
- Rodríguez-García, M.E.; Dorantes-Méndez, G.; Mendoza Gutiérrez, M.O. Desarrollo de una Prótesis para Desarticulado de Muñeca. Rev. Mex. Ing. Biomédica 2017, 38, 602–614. [Google Scholar] [CrossRef]
- Fundación DPT. Prótesis Robótica de Pierna; Fundación DPT: Buenos Aires, Argentina, 2024; Available online: https://fundaciondpt.com.ar/actualidad-y-publicaciones/newsletter-2-2/newsletter-n-81-febrero/n-81-protesis-robotica-de-pierna/ (accessed on 1 October 2024).
- Cadena SER. Funciona la Primera “Mano Robótica” Por Control MagnéTico: Los Afectados ya Pueden Reproducir Movimientos Solo Con el Pensamiento. 2024. Available online: https://cadenaser.com/nacional/2024/09/11/funciona-la-primera-mano-robotica-por-control-magnetico-cadena-ser/ (accessed on 5 October 2024).
- Balaguer-Castro, M.; Torner, P.; Jornet-Gibert, M.; Martínez-Pastor, J.C. Situación actual de la robótica en cirugía protésica de rodilla, ¿una moda o una realidad? Rev. Esp. Cir. Ortopédica Traumatol. 2023, 67, 334–341. [Google Scholar] [CrossRef] [PubMed]
- UCSE. Prototipo de Prótesis Robótica de Mano Con Impresión 3D. Ediciones UCSE. 2021. Available online: http://ediciones.ucse.edu.ar/ojsucse/index.php/difusiones/article/view/642/747 (accessed on 1 October 2024).
- Resnik, L.; Klinger, S.L.; Etter, K. The DEKA Arm: Its features, functionality, and evolution during the Veterans Affairs Study to optimize the DEKA Arm. Prosthet. Orthot. Int. 2018, 38, 492–504. [Google Scholar] [CrossRef]
- Zhang, L.; Li, J.; Cui, Y.; Dong, M.; Fang, B.; Zhang, P. Design and performance analysis of a parallel wrist rehabilitation robot (PWRR). Robot. Auton. Syst. 2021, 125, 103390. [Google Scholar] [CrossRef]
- Belter, J.T.; Segil, J.L.; Dollar, A.M.; Weir, R.F. Mechanical design and performance specifications of anthropomorphic prosthetic hands: A review. J. Rehabil. Res. Dev. 2013, 50, 599–618. [Google Scholar] [CrossRef]
- Farina, D.; Aszmann, O.C. Bionic limbs: Clinical reality and academic promises. Sci. Transl. Med. 2014, 6, 257ps12. [Google Scholar] [CrossRef]
- Ortiz-Catalan, M.; Mastinu, E.; Sassu, P.; Aszmann, O.; Brånemark, R. Self-contained neuromusculoskeletal arm prostheses. N. Engl. J. Med. 2020, 382, 1732–1738. [Google Scholar] [CrossRef]
- Aszmann, O.C.; Roche, A.D.; Salminger, S.; Paternostro-Sluga, T.; Herceg, M.; Sturma, A.; Hofer, C.; Farina, D. Bionic reconstruction to restore hand function after brachial plexus injury: A case series of three patients. Lancet 2015, 385, 2183–2189. [Google Scholar] [CrossRef]
- Open Bionics. Hero Arm. Available online: https://openbionics.com/hero-arm/ (accessed on 10 September 2024).
- Mobius Bionics. LUKE Arm. Available online: https://www.mobiusbionics.com/luke-arm/ (accessed on 11 September 2024).
- Össur. i-Limb Quantum. Available online: https://www.ossur.com/en-us/prosthetics/arms/i-limb-quantum (accessed on 10 September 2024).
- Myomo. MyoPro. Available online: https://myomo.com/myopro/ (accessed on 10 September 2024).
- Ottobock. Michelangelo Hand. Available online: https://www.ottobock.com/en-us/product/8E500 (accessed on 11 September 2024).
- TASKA Prosthetics. TASKA Hand. Available online: https://www.taskaprosthetics.com/ (accessed on 11 September 2024).
- Unlimited Tomorrow. TrueLimb. Available online: https://www.unlimitedtomorrow.com/ (accessed on 11 September 2024).
- YouBionic. Nexobrace. Available online: https://www.youbionic.com/ (accessed on 9 September 2024).
- Exiii. Handiii. Available online: https://www.exiii-hackberry.com/ (accessed on 9 September 2024).
- Chua, C.K.; Leong, K.F. 3D Printing and Additive Manufacturing: Principles and Applications; World Scientific Publishing: Singapore, 2014. [Google Scholar]
- Chua, C.K.; Yeong, W.Y. Bioprinting: Principles and Applications; World Scientific Publishing: Singapore, 2015. [Google Scholar]
- Hussain, I.; Kashif, M.; Jamil, M.; Khan, N. Development and application of low-cost 3D-printed prosthetics for upper-limb amputees. J. Prosthet. Orthot. 2021, 33, 87–95. [Google Scholar] [CrossRef]
- Gibson, I.; Rosen, D.W.; Stucker, B. Additive Manufacturing Technologies: 3D Printing, Rapid Prototyping, and Direct Digital Manufacturing; Springer: New York, NY, USA, 2015. [Google Scholar]
- Wilson, K.A.; Moore, J.; Rosenzweig, D. 3D Printing in Prosthetics: The Evolution and Future Prospects. J. Biomech. Eng. 2021, 143, 121004. [Google Scholar]
- Premier Prosthetic. The Evolution of Prosthetic Limbs: Current Technological Advancements; Premier Surgical Prosthetic Center: Knoxville, TN, USA, 2023. [Google Scholar]
- Gentile, C.; Cordella, F.; Zollo, L. Hierarchical Human-Inspired Control Strategies for Prosthetic Hands. Sensors 2022, 22, 2521. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gentile, A.; Cordella, F.; Zollo, L. Advancements in Prosthetic Design: Historical Perspective and Future Directions. J. Prosthet. Technol. 2022, 14, 124–137. [Google Scholar]
- Taglietti, L.; Giallanza, A.; Carbonari, G. Robotic Upper Limb Prostheses: Recent Advances in Materials and Manufacturing Processes. Adv. Mater. Res. 2019, 1145, 159–167. [Google Scholar]
- Despopoulos, A. The Renaissance of Prosthetic Limbs; Oxford University Press: Oxford, UK, 2009. [Google Scholar]
- McDonald, J. The advancement of prosthetic limbs in the 20th century. J. Rehabil. Res. Dev. 2010, 47, 389–405. [Google Scholar]
- Popescu, D.; Zapciu, A.; Tarniță, D.; Marsavina, L. 3D Printing for Medical Applications: Innovations in the Production of Custom Prosthetics. J. Mech. Sci. 2021, 44, 120–134. [Google Scholar]
- Schmidl, H.; Zhao, Q.; Lee, M. Enhancing Prosthetic Autonomy through Energy Optimization. IEEE Trans. Med. Robot. Bionics 2022, 14, 985–997. [Google Scholar]
- Llorens, R.; Noé, E.; Colomer, C.; Alcañiz, M.; Gil-Gómez, J.A. Integrating 3D-Printed Prosthetics with Augmented Reality for Functional Rehabilitation. J. NeuroEng. Rehabil. 2021, 18, 98. [Google Scholar]
- Antfolk, C.; D’Alonzo, M.; Rosén, B.; Lundborg, G.; Sebelius, F.; Cipriani, C. Sensory feedback in upper limb prosthetics. Expert Rev. Med. Devices 2013, 10, 45–54. [Google Scholar] [CrossRef]
- Karger, H.; Rosen, E.; Levi, G. Prosthetics in ancient Egypt: The story of the toe. J. Med. Hist. 2012, 12, 117–126. [Google Scholar]
- Kembhavi, A.; Kulkarni, S.; Bhandari, R. 3D Printed Prosthetics: Emerging Trends in Digital Fabrication for Healthcare. J. Med. Devices 2018, 10, 219–230. [Google Scholar]
- O’Connor, J.; Eisenstein, E. 3D Printing in Prosthetic Design: Time and Cost Efficiency. J. Med. Technol. 2019, 5, 55–60. [Google Scholar]
- Wood, L.J.; Adams, R.D.; Taylor, P. Advances in low-cost, 3D-printed prosthetic hands. J. Biomech. 2022, 140, 111246. [Google Scholar]
- Zuniga, J.M.; Katsavelis, D.; Peck, J.L.; Stollberg, J. 3D Printing for Assistive Devices and Prosthetics: A Review. Technol. Innov. 2020, 22, 65–72. [Google Scholar]
- Kamper, D.G.; Kulk, D. Development and testing of a low-cost, 3D-printed bionic hand. J. Rehabil. Res. Dev. 2016, 53, 387–398. [Google Scholar]
- Tomovic, R.; Schmidl, H.; Zollo, L. Biofeedback and Control Theory in Prosthetics: Modern Applications and Historical Development. J. Biomed. Eng. 2021, 47, 211–229. [Google Scholar]
- Smith, J.; Chen, L.; Kumar, A. Advances in Lightweight Actuators for Prosthetic Applications. Int. J. Robot. Res. 2023, 62, 1132–1150. [Google Scholar]
- Tomovic, R.; Schmidl, H. Advances in Haptic Feedback for Prosthetic Limb Control. Sens. Actuators Phys. 2023, 101, 125–138. [Google Scholar]
- Jones, B.; Martinez, R. Modular Prosthetic Design for Accessibility. J. Prosthet. Orthot. 2022, 33, 189–197. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).