Fate of the Mandible in Class III Patients Subjected to Bimaxillary Surgery with a New 3D Planning Reference
Abstract
1. Introduction
2. Material and Methods
2.1. Sample Selection
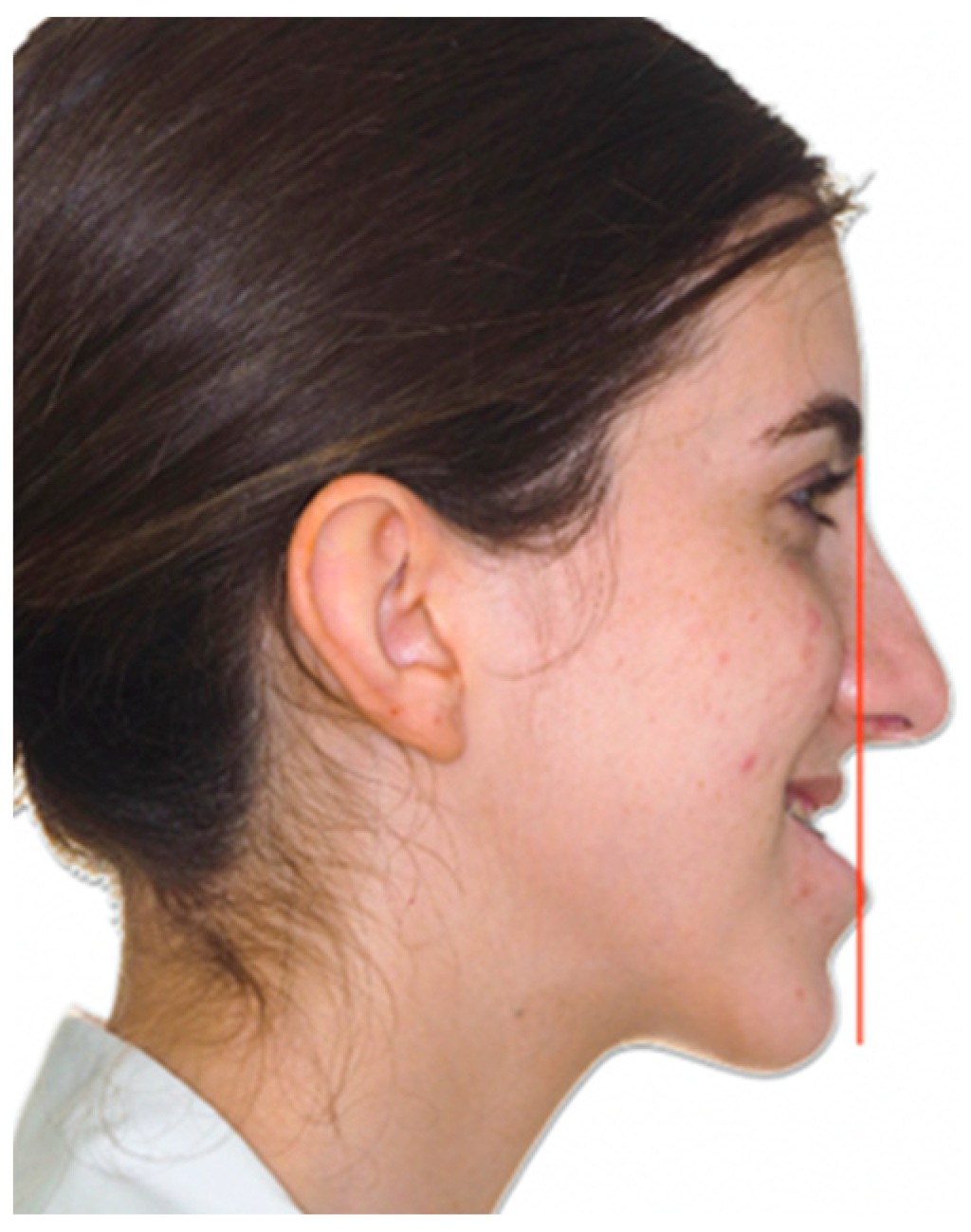
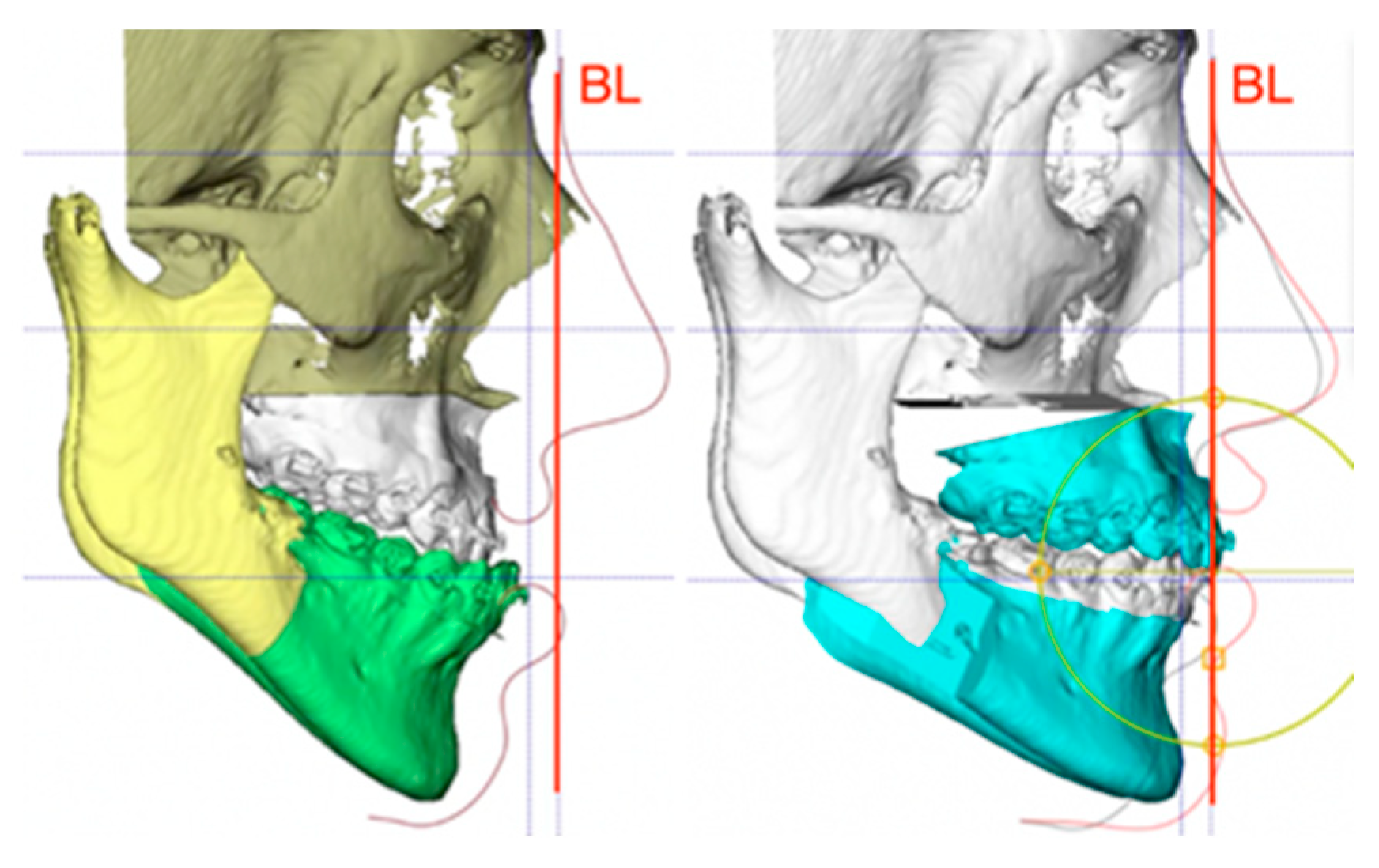
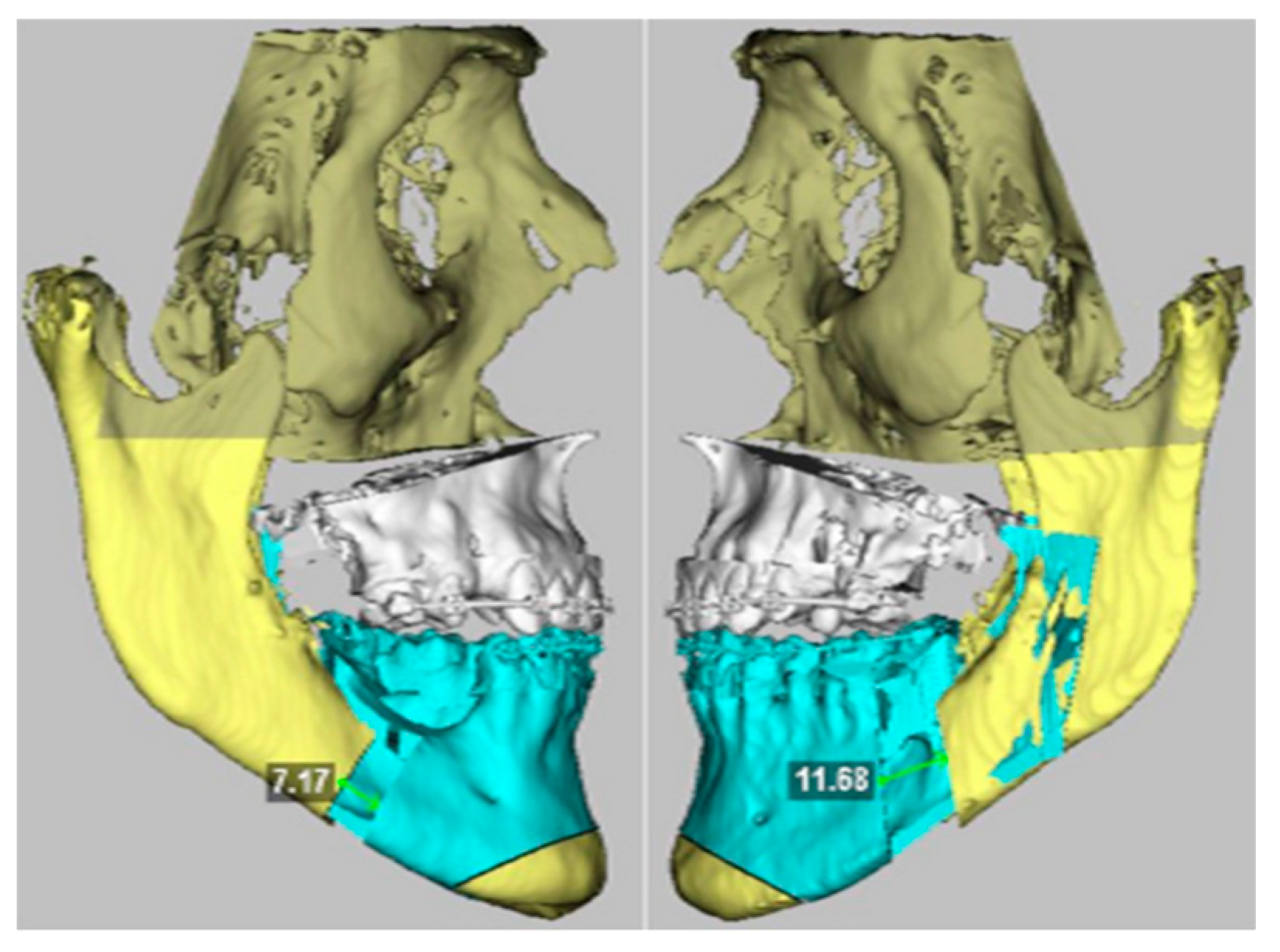
2.2. Virtual Planning
2.3. Surgery
2.4. Evaluation
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zere, E.; Chaudhari, P.K.; Sharan, J.; Dhingra, K.; Tiwari, N. Developing Class III malocclusions: Challenges and solutions. Clin. Cosmet. Investig. Dent. 2018, 10, 99–116. [Google Scholar] [CrossRef] [PubMed]
- Mousoulea, S.; Tsolakis, I.; Ferdianakis, E.; Tsolakis, A.I. The effect of chin-cup therapy in Class III malocclusion: A systematic review. Open Dent. J. 2016, 10, 664–679. [Google Scholar] [CrossRef]
- Ngan, P.; Moon, W. Evolution of Class III treatment in orthodontics. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 22–36. [Google Scholar] [CrossRef]
- Profit, W.; Fields, H., Jr. Contemporary Orthodontics, 3rd ed.; Mosby: St. Louis, MI, USA, 2007. [Google Scholar]
- Alhammadi, M.S.; Almashraqi, A.A.; Khadhi, A.H.; Arishi, K.A.; Alamir, A.A.; Beleges, E.M.; Halboub, E. Orthodontic camouflage versus orthodontic-orthognathic surgical treatment in borderline class III malocclusion: A systematic review. Clin. Oral Investig. 2022, 26, 6443–6455. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Alfaro, F. Upper incisor to Soft Tissue Plane (UI-STP): A new reference for diagnosis and planning in dentofacial deformities. Med. Oral Patol. Oral Cir. Bucal 2010, 15, e779–e781. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Alfaro, F.; Vivas-Castillo, J.; Belle de Oliveira, R.; Hass-Junior, O.; Giralt-Hernando, M.; Valls-Ontañón, A. Barcelona line. A multicentre validation study of a facial projection reference in orthognathic surgery. Br. J. Oral Maxillofac. Surg. 2023, 61, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Moscarino, S.; Kötter, F.; Brandt, M.; Modabber, A.; Kniha, K.; Hölzle, F.; Wolf, M.; Möhlhenrich, S.C. Influence of different surgical concepts for moderate skeletal class II and III treatment on the nasopharyngeal airway space. J. Craniomaxillofac. Surg. 2019, 47, 1489–1497. [Google Scholar] [CrossRef]
- Chen, M.W.J.; Lum, J.L.; Yong, C.W.; Lai, W.M.C.; Wong, R.C.W. Placing the maxilla in the most aesthetic sagittal position: Validation of several reference lines in relation to the forehead shape. Int. J. Oral Maxillofac. Surg. 2024, 53, 405–412. [Google Scholar] [CrossRef]
- Hunsuck, E.E. A modified intraoral sagittal splitting technique for correction of mandibular prognathism. J. Oral Surg. 1968, 26, 250–253. [Google Scholar]
- Hernández Alfaro, F.; Guijarro-Martínez, R. “Twist Technique” for pterygomaxillary dysjunction in minimally invasive Le Fort I Osteotomy. J. Oral Maxillofac. Surg. 2013, 71, 389–392. [Google Scholar] [CrossRef] [PubMed]
- Wylie, G.A.; Fish, L.C.; Epker, B.N. Cephalometrics: A comparison of five analyses currently used in the diagnosis of dentofacial deformities. Int. J. Adult Orthodon Orthognath. Surg. 1987, 2, 15–36. [Google Scholar]
- Steiner, C.C. Cephalometrics for you and me. Am. J. Orthod. 1953, 39, 729–755. [Google Scholar] [CrossRef]
- Ricketts, R. Cephalometric analysis and synthesis. Angle Orthod. 2009, 31, 141–156. [Google Scholar]
- Arnett, G.W.; Bergman, R.T. Facial keys to orthodontic diagnosis and treatment planning-Part II. Am. J. Orthod. Dentofac. Orthop. 1993, 103, 395–411. [Google Scholar] [CrossRef] [PubMed]
- Maspero, C.; Cenzato, N.; Inchingolo, F.; Cagetti, M.G.; Isola, G.; Sozzi, D.; Del Fabbro, M.; Tartaglia, G.M. The Maxilla-Mandibular Discrepancies through Soft-Tissue References: Reliability and Validation of the Anteroposterior Measurement. Children 2023, 10, 459. [Google Scholar] [CrossRef]
- Bailey, L.J.; White, R.P.; Proffit, W.R.; Turvey, T.A. Segmental Le Fort I osteotomy for management of transverse maxillary de deficiency. J. Oral Maxillofac. Surg. 1997, 55, 728. [Google Scholar] [CrossRef]
- Ertty, E.; Méndez-Manjón, I.; Haas, O.L., Jr.; Hernández-Alfaro, F.; Meloti, F. Definition of New Three-Dimensional Cephalometric Analysis of Maxillomandibular Sagittal Relationship for Orthodontics and Orthognathic Surgery: Normative Data Based on 700 CBCT Scans. J. Craniofac Surg. 2023, 34, 1291–1295. [Google Scholar] [CrossRef] [PubMed]
- Proffit, W.R.; Phillips, C.; Turvey, T.A. Stability after mandibular setback: Mandible-only versus 2-jaw surgery. J. Oral Maxillofac. Surg. 2012, 70, e408–e414. [Google Scholar] [CrossRef]
- Jakobsone, G.; Stenvik, A.; Sandvik, L.; Espeland, L. Three-year follow-up of bimaxillary surgery to correct skeletal Class III malocclusion: Stability and risk factors for relapse. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 80–89. [Google Scholar] [CrossRef]
- Giralt-Hernando, M.; Valls-Ontañón, A.; Junior, O.L.H.; Masià-Gridilla, J.; Hernández-Alfaro, F. What are the Surgical Movements in Orthognathic Surgery That Most Affect the Upper Airways? A Three-Dimensional Analysis. J. Oral Maxillofac. Surg. 2021, 79, 450–462. [Google Scholar] [CrossRef]
- Hochban, W.; Schurmann, R.; Brandenburg, U. Mandibular setback for surgical correction of mandibular hyperplasia— Does it provoke sleep-related breathing disorders? Int. J. Oral Maxillofac. Surg. 1996, 25, 333. [Google Scholar] [CrossRef] [PubMed]
- Liukkonen, M.; Vähätalo, K.; Peltomäki, T.; Tiekso, J.; Happonen, R.-P. Effect of mandibular setback surgery on the posterior airway size. Int. J. Adult Orthod. Orthognath. Surg. 2002, 17, 41–46. [Google Scholar]
- Riley, R.W.; Powell, N.B.; Guilleminault, C.; Ware, W. Obstructive sleep apnea syndrome following surgery for mandibular prognathism. J. Oral Maxillofac. Surg. 1987, 45, 450. [Google Scholar] [CrossRef] [PubMed]
- Demetriades, N.; Chang, D.J.; Laskarides, C.; Papageorge, M. Effects of mandibular retropositioning, with or without maxillary advancement, on the oro-naso-pharyngeal airway and development of sleep-related breathing disorders. J. Oral Maxillofac. Surg. 2010, 68, 2431–2436. [Google Scholar] [CrossRef] [PubMed]
- Foltán, R.; Hoffmannová, J.; Pavlíková, G.; Hanzelka, T.; Klíma, K.; Horká, E.; Adámek, S.; Šedý, J. The influence of orthognathic surgery on ventilation during sleep. Int. J. Oral Maxillofac. Surg. 2011, 40, 146–149. [Google Scholar] [CrossRef]

| N | % | ||
|---|---|---|---|
| Mandibular sagittal movement | Total | 124 | 100 |
| Setback | 9 | 7.3 | |
| Advancement | 112 | 90.3 | |
| No sagittal movement | 3 | 2.4 | |
| Mandibular centering movement | Total | 124 | 100 |
| Yes | 84 | 67.7 | |
| No | 40 | 32.3 | |
| Mandibular counter-clockwise rotation | Total | 124 | 100 |
| Yes | 65 | 52.4 | |
| No | 59 | 47.6 | |
| Mandibular centering and counter-clockwise rotation | Total | 124 | 100 |
| Yes | 85 | 68.5 | |
| No | 39 | 31.5 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hernández-Alfaro, F.; de la Fuente-Vázquez, C.; Valls-Ontañón, A.; Haas-Junior, O.-L.; Giralt-Hernando, M.; Masià-Gridilla, J. Fate of the Mandible in Class III Patients Subjected to Bimaxillary Surgery with a New 3D Planning Reference. Appl. Sci. 2025, 15, 1069. https://doi.org/10.3390/app15031069
Hernández-Alfaro F, de la Fuente-Vázquez C, Valls-Ontañón A, Haas-Junior O-L, Giralt-Hernando M, Masià-Gridilla J. Fate of the Mandible in Class III Patients Subjected to Bimaxillary Surgery with a New 3D Planning Reference. Applied Sciences. 2025; 15(3):1069. https://doi.org/10.3390/app15031069
Chicago/Turabian StyleHernández-Alfaro, Federico, Carlos de la Fuente-Vázquez, Adaia Valls-Ontañón, Orion-Luiz Haas-Junior, Maria Giralt-Hernando, and Jorge Masià-Gridilla. 2025. "Fate of the Mandible in Class III Patients Subjected to Bimaxillary Surgery with a New 3D Planning Reference" Applied Sciences 15, no. 3: 1069. https://doi.org/10.3390/app15031069
APA StyleHernández-Alfaro, F., de la Fuente-Vázquez, C., Valls-Ontañón, A., Haas-Junior, O.-L., Giralt-Hernando, M., & Masià-Gridilla, J. (2025). Fate of the Mandible in Class III Patients Subjected to Bimaxillary Surgery with a New 3D Planning Reference. Applied Sciences, 15(3), 1069. https://doi.org/10.3390/app15031069






