Frictional Cohesive Force and Multifunctional Simple Machine for Advanced Engineering and Biomedical Applications
Abstract
Featured Application
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| FCF | Frictional Cohesion Force |
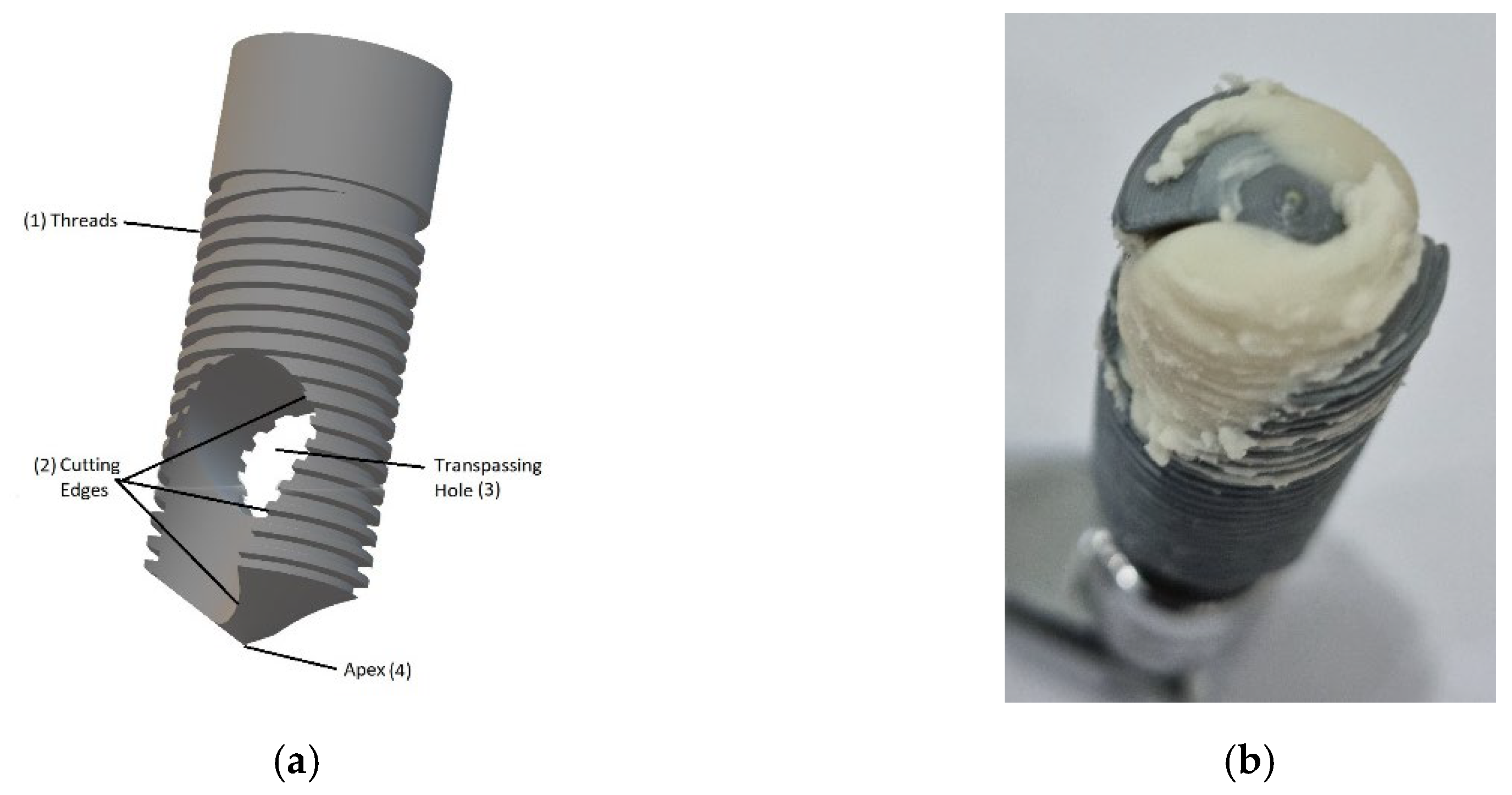
| BKS | Bioactive Kinetic Screw |
| MIT | Maximum Insertion Torque |
| MRT | Maximum Removal Torque |
References
- Andreucci, C.A. Bioactive Kinetic Screw (BKS)—Multifunctional Simple Machine; University of Porto: Porto, Portugal, 2024. [Google Scholar]
- SINOROCK. Self-Drilling Soil Nailing Equipment. 2023. Available online: https://www.sinorockco.com/news/industry-news/self-drilling-soil-nail-equipment.html (accessed on 12 July 2025).
- Motoyoshi, M.; Inaba, M.; Ono, A.; Ueno, S.; Shimizu, N. The Effect of Cortical Bone Thickness on the Stability of Orthodontic Mini-Implants and on the Stress Distribution in Surrounding Bone. Int. J. Oral Maxillofac. Implant. 2009, 38, 13–18. [Google Scholar] [CrossRef]
- Tethys Engineering. Advanced Anchoring and Mooring Study. 2020. Available online: https://tethys.pnnl.gov/sites/default/files/publications/Advanced-Anchor-and-Mooring-Study.pdf (accessed on 12 July 2025).
- Zhang, W.; Chen, Y.; Wang, H. Analysis of Drilling Vibration Characteristics of Anchoring Systems. Sensors 2023, 23, 10542. [Google Scholar]
- Han, C.; Xie, Z.; Yang, K.; Zhang, N. Anchoring Method Utilizing Self-Drilling and Self-Anchoring Extendable Anchor Rod Applicable to Soft and Weak Coal Rocks. U.S. Patent 10,487,654, 26 November 2019. [Google Scholar]
- Liu, Y.; Wang, S.; Zhao, L. Mechanical Characteristics of Anchor Drilling Rig Groups for Rapid Excavating. Sci. Rep. 2023, 13, 4556. [Google Scholar] [CrossRef] [PubMed]
- Sun, S.; Mao, S.; Xue, X.; Wang, C.; Ma, H.; Guo, Y.; Yuan, H.; Su, H. Research on Obstacle-Avoidance Trajectory Planning for Drill and Anchor Materials Handling by a Mechanical Arm on a Coal Mine Drilling and Anchoring Robot. Sensors 2024, 24, 6866. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Zhao, J.; Davis, T. Novel Adhesive Anchoring System through Engineered Adhesive–Concrete Interface. Structures 2021, 33, 947–956. [Google Scholar] [CrossRef]
- Wang, Y.; Huang, J.; Zhao, X. Ground Anchors and Anchored Systems; DOT Research Library: Washington, DC, USA, 2023. [Google Scholar]
- Jiang, X.; Liu, H.; Sun, Y. Experimental Analysis on Applicability Degree and Influence Factors. Sens. Actuators A Phys. 2024, 353, 114072. [Google Scholar]
- Zhang, S.; Wang, Q. Design and key technology research of ZYWL-4000SY remote control drilling rig. Coal Sci. Technol. 2021, 49, 129–134. [Google Scholar]
- TechInsight, Inc. Why Anchor Tool Selection Matters in Drilling Applications. 2024. Available online: https://www.techinsight.com/blog/anchor-tool-selection-drilling (accessed on 12 July 2025).
- Liu, Z.; Li, Z.; Zou, K.; Xie, C. Research and Application of excavation and anchoring machine airborne advanced exploration drilling rig. ResearchSquare. 2023. Available online: https://www.researchsquare.com/article/rs-4200090/v1 (accessed on 12 July 2025).
- Petersen, D.; Lin, Z.; Zhao, J. Design of anchor reinforcement for seismic tension loads. Eng. Struct. 2018, 164, 109–118. [Google Scholar] [CrossRef]
- Li, M.; Zhang, Z.; Xu, Q. Novel Construction Method for Efficiently Drilling Slope Protection Anchor Rods. Chinese Patent CN114370228A, 22 April 2023. [Google Scholar]
- Li, H.; Wang, Y.; Chen, D. Asteroid Anchoring Method Based on Cross-Drilling Geometric Force Closure. Acta Astronaut. 2020, 173, 1–8. [Google Scholar] [CrossRef]
- Liu, K.; Cheng, J.; Sun, X.; Li, Z.; Wan, Z.; Xing, Z.; Xing, K.; Liu, J. Automated Stratum Interface Detection Using the Optimized Drilling Specific Energy through Self-Adaptive Logistic Function. Sensors 2023, 23, 8594. [Google Scholar] [CrossRef]
- Cehreli, M.C.; Comert, M.; Karasoy, D.; Sahin, S. Mechanical Properties of Self-Drilling and Self-Tapping Orthodontic Mini-Implants. Angle Orthod. 2010, 80, 821–827. [Google Scholar] [CrossRef]
- Chen, J.; Lv, X.; Kang, J.; Liu, G.; Zhou, Y. Experimental Study on the Anchoring Mechanism and Performance of BFRP Bolt-Anchorage System in Supporting Clay Slopes. Polymer Testing 2025, 147, 108822. [Google Scholar] [CrossRef]
- Zhang, J.; Song, B.; Wei, Q.; Bourell, D.; Shi, Y. A Review of Selective Laser Melting of Aluminum Alloys: Processing, Microstructure, Property and Developing Trends. J. Mater. Sci. Technol. 2019, 35, 270–284. [Google Scholar] [CrossRef]
- Braga, D.F.O.; Eslami, S.; Moreira, P.M.G.P. Friction Stir Welding. In Advanced Joining Processes; da Silva, L., El-Zein, M., Martins, P., Eds.; Elsevier: Amsterdam, The Netherlands, 2021; pp. 173–206. [Google Scholar] [CrossRef]
- Timon, C.; Keady, C. Thermal Osteonecrosis Caused by Bone Drilling in Orthopedic Surgery: A Literature Review. Cureus 2019, 11, e5226. [Google Scholar] [CrossRef]
- Bachiri, A.; Djebbar, N.; Boutabout, B.; Serier, B. Effect of Different Impactor Designs on Biomechanical Behavior in the Interface Bone-Implant: A Comparative Biomechanics Study. Comput. Methods Programs Biomed. 2020, 197, 105723. [Google Scholar] [CrossRef]
- Andreucci, C.A.; Fonseca, E.M.M.; Jorge, R.N. A New Simplified Autogenous Sinus Lift Technique. Bioengineering 2023, 10, 505. [Google Scholar] [CrossRef]
- Andreucci, C.A.; Fonseca, E.M.M.; Natal, R.M.J. Structural analysis of the new Bioactive Kinetic Screw in titanium alloy vs. commercially pure titanium. J. Comp. Art. Int. Mec. Biomec. 2022, 2, 35–43. [Google Scholar]
- Andreucci, C.A.; Alshaya, A.; Fonseca, E.M.M.; Jorge, R.N. Proposal for a New Bioactive Kinetic Screw in an Implant, Using a Numerical Model. Appl. Sci. 2022, 12, 779. [Google Scholar] [CrossRef]
- Andreucci, C.A.; Fonseca, E.M.M.; Jorge, R.N. 3D Printing as an Efficient Way to Prototype and Develop Dental Implants. BioMedInformatics 2022, 2, 44. [Google Scholar] [CrossRef]
- Andreucci, C.A.; Fonseca, E.M.M.; Jorge, R.N. Increased Material Density within a New Biomechanism. Math. Comput. Appl. 2022, 27, 90. [Google Scholar] [CrossRef]
- Andreucci, C.A.; Fonseca, E.M.M.; Jorge, R.N. Bio-lubricant Properties Analysis of Drilling an Innovative Design of Bioactive Kinetic Screw into Bone. Designs 2023, 7, 21. [Google Scholar] [CrossRef]
- Andreucci, C.A.; Fonseca, E.M.M.; Jorge, R.N. Immediate Autogenous Bone Transplantation Using a Novel Kinetic Bioactive Screw 3D Design as a Dental Implant. BioMedInformatics 2023, 3, 299–305. [Google Scholar] [CrossRef]
- Andreucci, C.A.; Fonseca, E.M.M.; Natal Jorge, R.M. BKS Drill-and-Seal Technique: Innovative Design and Aseptic Bone Implant. In Lecture Notes in Bioengineering, Proceedings of the 10th Congress of the Portuguese Society of Biomechanics, Figueira da Foz, Portugal, 5–6 May 2023; Martins Amaro, A., Ed.; Springer: Cham, Switzerland, 2023. [Google Scholar] [CrossRef]
- Andreucci, C.A.; Fonseca, E.M.M.; Jorge, R.N. Static in bone implants: Standard steady-state torque and primary stability in a bioactive kinetic screw. J. Braz. Soc. Mech. Sci. Eng. 2023, 45, 651. [Google Scholar] [CrossRef]
- Andreucci, C.A.; Fonseca, E.M.M.; Jorge, R.N. A New Simple Machine That Converts Torque into Steady-State Pressure in Solids. In Proceedings of the 2023 IEEE 7th Portuguese Meeting on Bioengineering (ENBENG), Porto, Portugal, 22–23 June 2023; pp. 148–150. [Google Scholar] [CrossRef]
- Rosenholm, J.B.; Peiponen, K.-E.; Gornov, E. Materials Cohesion and Interaction Forces. Adv. Colloid Interface Sci. 2008, 141, 48–65. [Google Scholar] [CrossRef]
- Röderer, G.; Scola, A.; Schmölz, W.; Gebhard, F.; Windolf, M.; Hofmann-Fliri, L. Biomechanical in vitro assessment of screw augmentation in locked plating of proximal humerus fractures. Injury 2013, 44, 1327–1332. [Google Scholar] [CrossRef]
- Lenich, A.; Mayr, E.; Rüter, A.; Möckl, C.; Füchtmeier, B. First results with the trochanter fixation nail (TFN): A report on 120 cases. Arch. Orthop. Trauma Surg. 2006, 126, 706–712. [Google Scholar] [CrossRef]
- Erhart, S.; Schmoelz, W.; Blauth, M.; Lenich, A. Biomechanical Effect of Bone Cement Augmentation on Rotational Stability and Pull-Out Strength of the Proximal Femur Nail Antirotation™. Injury 2011, 42, 1322–1327. [Google Scholar] [CrossRef]
- Simmermacher, R.K.J.; Ljungqvist, J.; Bail, H.; Hockertz, T.; Vochteloo, A.J.H.; Ochs, U.; vd Werken, C. The new proximal femoral nail antirotation (PFNA®) in daily practice: Results of a multicentre clinical study. Injury 2008, 39, 932–939. [Google Scholar] [CrossRef]
- Baumgaertner, M.R.; Curtin, S.L.; Lindskog, D.M.; Keggi, J.M. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. JBJS 1995, 77, 1058–1064. [Google Scholar] [CrossRef]
- Unger, S.; Erhart, S.; Kralinger, F.; Blauth, M.; Schmoelz, W. The Effect of In Situ Augmentation on Implant Anchorage in Proximal Humeral Head Fractures. Injury 2012, 43, 1759–1763. [Google Scholar] [CrossRef]
- Lindtner, R.A.; Schmid, R.; Nydegger, T.; Konschake, M.; Schmoelz, W. Pedicle screw anchorage of carbon fiber-reinforced PEEK screws under cyclic loading. Eur. Spine J. 2018, 27, 1775–1784. [Google Scholar] [CrossRef]
- Bullmann, V.; Schmoelz, W.; Richter, M.; Grathwohl, C.; Schulte, T.L. Revision of Cannulated and Perforated Cement-Augmented Pedicle Screws: A Biomechanical Study in Human Cadavers. Spine 2010, 35, E932–E939. [Google Scholar] [CrossRef] [PubMed]
- Brunner, A.; Büttler, M.; Lehmann, U.; Frei, H.C.; Kratter, R.; Di Lazzaro, M.; Scola, A.; Sermon, A.; Attal, R. What is the optimal salvage procedure for cut-out after surgical fixation of trochanteric fractures with the PFNA or TFN?: A multicentre study. Injury 2016, 47, 432–438. [Google Scholar] [CrossRef] [PubMed]
- Grechenig, S.; Gänsslen, A.; Gueorguiev, B.; Berner, A.; Müller, M.; Nerlich, M.; Schmitz, P. PMMA-augmented SI screw: A biomechanical analysis of stiffness and pull-out force in a matched paired human cadaveric model. Injury 2015, 46, S125–S128. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, P.; Baumann, F.; Grechenig, S.; Gaensslen, A.; Nerlich, M.; Müller, M.B. The cement-augmented transiliacal internal fixator (caTIFI): An innovative surgical technique for stabilization of fragility fractures of the pelvis. Injury 2015, 46, S114–S120. [Google Scholar] [CrossRef]
- Vittore, D.; Vicenti, G.; Caizzi, G.; Abate, A.; Moretti, B. Balloon-assisted reduction, pin fixation and tricalcium phosphate augmentation for calcanear fracture. Injury 2014, 45, S72–S79. [Google Scholar] [CrossRef]
- Schliemann, B.; Wähnert, D.; Theisen, C.; Herbort, M.; Kösters, C.; Raschke, M.J.; Weimann, A. How to enhance the stability of locking plate fixation of proximal humerus fractures? An overview of current biomechanical and clinical data. Injury 2015, 46, 1207–1214. [Google Scholar] [CrossRef]
- Buckley, R.E.; Moran, C.G.; Apivatthakakul, T. AO Principles of Fracture Management, 3rd ed.; Thieme: New York, NY, USA, 2018; ISBN 9783132423091. [Google Scholar]
- Prendergast, P.J.; Huiskes, R. The Biomechanics of Wolff’s law: Recent advances. IJMS 1995, 164, 152–154. [Google Scholar] [CrossRef]
- Wong, K.C. 3D-printed Patient-specific Applications in Orthopedics. ORR 2016, 8, 57–66. [Google Scholar] [CrossRef]
- Wegst, U.G.; Bai, H.; Saiz, E.; Tomsia, A.P.; Ritchie, R.O. Bioinspired structural materials. Nat. Mater. 2015, 14, 23–36. [Google Scholar] [CrossRef]
- Callens, S.; Betts, D.; Müller, R.; Zadpoor, A. The local and global geometry of trabecular bone. Acta Biomater. 2021, 130, 13–23. [Google Scholar] [CrossRef]


| PCF 10 Sample | Density (g/cm3) | MIT (N/cm) | MRT (N/cm) | μsf |
|---|---|---|---|---|
| 1 | 0.16 | 20 | 21 | 1.05 |
| 2 | 0.16 | 21 | 22 | 1.05 |
| 3 | 0.16 | 20 | 21 | 1.05 |
| 4 | 0.16 | 20 | 21 | 1.05 |
| 5 | 0.16 | 20 | 21 | 1.05 |
| Feature | BKS | Expanding Screws | Cemented Systems | Traditional Implants |
|---|---|---|---|---|
| Lateral Compression | No | Yes | Yes | Yes |
| Compacts/Collects Bone | Yes | No | No | No |
| Requires Cement | No | No | Yes | No |
| Risk of Thermal Necrosis | Minimal | Moderate | High | Moderate |
| Revision Friendly | Yes | Variable | No | Yes |
| Dependence on Bone Density | Low | Moderate | Low | High |
| Autograft Potential | Yes | No | No | No |
| Clinical Maturity | Emerging | Moderate | Established | Established |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andreucci, C.A.; Yaseen, A.; Fonseca, E.M.M. Frictional Cohesive Force and Multifunctional Simple Machine for Advanced Engineering and Biomedical Applications. Appl. Sci. 2025, 15, 8215. https://doi.org/10.3390/app15158215
Andreucci CA, Yaseen A, Fonseca EMM. Frictional Cohesive Force and Multifunctional Simple Machine for Advanced Engineering and Biomedical Applications. Applied Sciences. 2025; 15(15):8215. https://doi.org/10.3390/app15158215
Chicago/Turabian StyleAndreucci, Carlos Aurelio, Ahmed Yaseen, and Elza M. M. Fonseca. 2025. "Frictional Cohesive Force and Multifunctional Simple Machine for Advanced Engineering and Biomedical Applications" Applied Sciences 15, no. 15: 8215. https://doi.org/10.3390/app15158215
APA StyleAndreucci, C. A., Yaseen, A., & Fonseca, E. M. M. (2025). Frictional Cohesive Force and Multifunctional Simple Machine for Advanced Engineering and Biomedical Applications. Applied Sciences, 15(15), 8215. https://doi.org/10.3390/app15158215








