Quantitative Evaluation of Marginal and Internal Fit of CAD/CAM Ceramic Crown Restorations Obtained by Model Scanner, Intraoral Scanner, and Different CBCT Scans
Abstract
1. Introduction
2. Materials and Methods
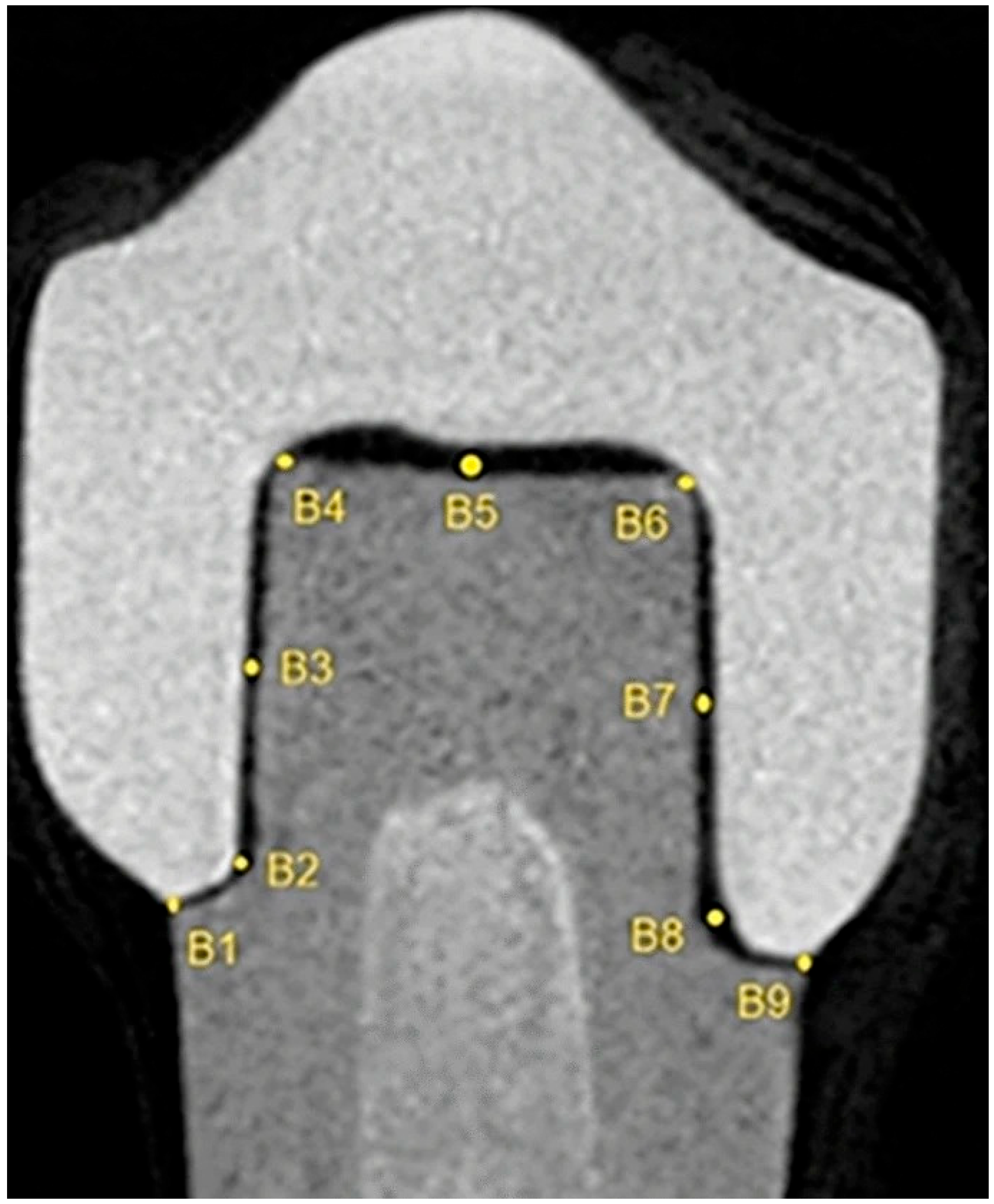
2.1. Linear Measurements
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CAD | Computer-aided design |
| CAM | Computer-aided manufacturing |
| 2D | Two dimensional |
| 3D | Three-dimensional |
| CBCT | Cone beam computed tomography |
| STL | Standard tessellation language |
| MCT | Microcomputed tomography |
| VMD | Vertical marginal discrepancy |
| FOV | Field of view |
References
- Karlsson, S. The fit of Procera titanium crowns. An in vitro and clinical study. Acta Odontol. Scand. 1993, 51, 129–134. [Google Scholar] [CrossRef]
- Contrepois, M.; Soenen, A.; Bartala, M.; Laviole, O. Marginal adap tation of ceramic crowns: A systematic review. J. Prosthet. Dent. 2013, 110, 447–454. [Google Scholar] [CrossRef]
- Hung, S.H.; Hung, K.S.; Eick, J.D.; Chappell, R.P. Marginal fit of por celain-fused-to-metal and two types of ceramic crown. J. Prosthet. Dent. 1990, 63, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Tuntiprawon, M.; Wilson, P.R. The effect of cement thickness on the fracture strength of all-ceramic crowns. Aust. Dent. J. 1995, 40, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Burton, J.F.; Hood, J.A.; Plunkett, D.J.; Johnson, S. The effects of disposable and custom-made impression trays on the accuracy of impressions. J. Dent. 1989, 17, 121–123. [Google Scholar] [CrossRef] [PubMed]
- Thongthammachat, S.; Moore, B.K.; Barco, M.T.; Hovijitra, S.; Brown, D.T.; Andres, C.J. Dimensional accuracy of dental casts: Influence of tray material, impression material, and time. J. Prosthodont. 2002, 11, 98–108. [Google Scholar] [CrossRef]
- Corso, M.; Abanomy, A.; Di Canzio, J.; Zurakowski, D.; Morgano, S.M. The effect of temperature changes on the dimensional stability of polyvinyl siloxane and polyether impression materials. J. Prosthet. Dent. 1998, 79, 626–631. [Google Scholar] [CrossRef]
- Robaian, A.; Maawadh, A.; Alghomlas, Z.I.; Alqahtani, A.M.; Alothman, T.A.; Alhajri, F.F.; Albar, N. Evaluation of the marginal microleakage of CAD CAM compared with conventional interim crowns luted with different types of cement: An in vitro study. Niger. J. Clin. Pract. 2021, 24, 828–832. [Google Scholar] [CrossRef]
- Miyazaki, T.; Hotta, Y. CAD/CAM systems available for the fabrication of crown and bridge restorations. Aust. Dent. J. 2011, 56, 97–106. [Google Scholar] [CrossRef]
- Beuer, F.; Schweiger, J.; Edelhoff, D. Digital dentistry: An overview of recent developments for CAD/CAM generated restorations. Br. Dent. J. 2008, 204, 505–511. [Google Scholar] [CrossRef]
- Güth, J.F.; Keul, C.; Stimmelmayr, M.; Beuer, F.; Edelhoff, D. Accuracy of digital models obtained by direct and indirect data capturing. Clin. Oral. Investig. 2013, 17, 1201–1208. [Google Scholar] [CrossRef]
- Wismeijer, D.; Mans, R.; van Genuchten, M.; Reijers, H.A. Patients’ preferences when comparing analogue implant impressions using a polyether impression material versus digital impressions (Intraoral Scan) of dental implants. Clin. Oral. Implant. Res. 2014, 25, 1113–1118. [Google Scholar] [CrossRef]
- Joda, T.; Brägger, U. Digital vs. conventional implant prosthetic workflows: A cost/time analysis. Clin. Oral. Implant. Res. 2015, 26, 1430–1435. [Google Scholar] [CrossRef] [PubMed]
- Abduo, J.; Lyons, K.; Swain, M. Fit of zirconia fixed partial denture: A systematic review. J. Oral. Rehabil. 2010, 37, 866–876. [Google Scholar] [CrossRef] [PubMed]
- Hunter, A.J.; Hunter, A.R. Gingival margins for crowns: A review and discussion. Part II: Discrepancies and configurations. J. Prosthet. Dent. 1990, 64, 636–642. [Google Scholar] [CrossRef] [PubMed]
- Batson, E.R.; Cooper, L.F.; Duqum, I.; Mendonça, G. Clinical outcomes of three different crown systems with CAD/CAM technology. J. Prosthet. Dent. 2014, 112, 770–777. [Google Scholar] [CrossRef]
- Baig, M.R.; Tan, K.B.; Nicholls, J.I. Evaluation of the marginal fit of a zirconia ceramic computer-aided machined (CAM) crown system. J. Prosthet. Dent. 2010, 104, 216–227. [Google Scholar] [CrossRef]
- Dauti, R.; Cvikl, B.; Lilaj, B.; Heimel, P.; Moritz, A.; Schedle, A. Micro-CT evaluation of marginal and internal fit of cemented polymer infiltrated ceramic network material crowns manufactured after conventional and digital impressions. J. Prosthodont. Res. 2019, 63, 40–46. [Google Scholar] [CrossRef]
- McLean, J.W.; von Fraunhofer, J.A. The estimation of cement film thickness by an in vivo technique. Br. Dent. J. 1971, 131, 107–111. [Google Scholar] [CrossRef]
- Hamza, T.A.; Ezzat, H.A.; El-Hossary, M.M.; Katamish, H.A.; Shokry, T.E.; Rosenstiel, S.F. Accuracy of ceramic restorations made with two CAD/CAM systems. J. Prosthet. Dent. 2013, 109, 83–87. [Google Scholar] [CrossRef]
- Luthardt, R.; Sandkuhl, O.; Herold, V.; Walter, M. Accuracy of mechanical digitizing with a CAD/CAM system for fixed restorations. Int. J. Prosthodont. 2001, 14, 146–151. [Google Scholar]
- Boening, K.W.; Wolf, B.H.; Schmidt, A.E.; Kastner, K.; Walter, M.H. Clinical fit of Procera AllCeram crowns. J. Prosthet. Dent. 2000, 84, 419–424. [Google Scholar] [CrossRef]
- Renne, W.; McGill, S.T.; Forshee, K.V.; DeeFee, M.R.; Mennito, A.S. Predicting marginalfit of CAD/CAM crowns based on the presence or absence of common preparation errors. J. Prosthet. Dent. 2012, 108, 310–315. [Google Scholar] [CrossRef]
- Pauwels, R.; Jacobs, R.; Singer, S.R.; Mupparapu, M. CBCT-based bone quality assessment: Are Hounsfield units applicable? Dentomaxillofacial Radiol. 2015, 44, 20140238. [Google Scholar] [CrossRef] [PubMed]
- Liang, X.; Jacobs, R.; Hassan, B.; Li, L.; Pauwels, R.; Corpas, L. A comparative evaluation of cone beam computed tomography (CBCT) and multi-slice CT (MSCT): Part II. On 3D model accuracy. Eur. J. Radiol. 2018, 102, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Holden, J.E.; Goldstein, G.R.; Hittelman, E.L.; Clark, E.A. Comparison of the marginal f it of pressable ceramic to metal ceramic restorations. J. Prosthodont. 2009, 18, 645–648. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Rus, F.; Suárez, M.J.; Rivera, B.; Pradíes, G. Evaluation of the absolute marginal discrepancy of zirconia-based ceramic copings. J. Prosthet. Dent. 2011, 105, 108–114. [Google Scholar] [CrossRef]
- Burns, D.R.; Beck, D.A.; Nelson, S.K. A review of selected dental literature on contemporary provisional fixed prosthodontic treatment: Report of the committee on research in fixed prosthodontics of the academy of fixed prosthodontics. J. Prosthet. Dent. 2003, 90, 474–497. [Google Scholar] [CrossRef]
- Kim, D.Y.; Kim, J.H.; Kim, H.Y.; Kim, W.C. Comparison and evaluation of marginal and internal gaps in cobalt-chromium alloy copings fabricated using subtractive and additive manufacturing. J. Prosthodont. Res. 2018, 62, 56–64. [Google Scholar] [CrossRef]
- Boitelle, P.; Mawussi, B.; Tapie, L.; Fromentin, O. A systematic review of CAD/CAM fit restoration evaluations. J. Oral. Rehabil. 2014, 41, 853–874. [Google Scholar] [CrossRef]
- Kale, E.; Cilli, M.; Özçelik, T.B.; Yilmaz, B. Marginal fit of CAD-CAM monolithic zirconia crowns fabricated by using cone beam computed tomography scans. J. Prosthet. Dent. 2020, 123, 731–737. [Google Scholar] [CrossRef] [PubMed]
- Belgin, H.B.; Kale, E.; Özçelik, T.B.; Yilmaz, B. Marginal fit of 3-unit CAD-CAM zirconia frameworks fabricated using cone beam computed tomography scans: An experimental study. Odontology 2022, 110, 339–348. [Google Scholar] [CrossRef] [PubMed]
- Hassan, B.; Couto Souza, P.; Jacobs, R.; de Azambuja Berti, S.; van der Stelt, P. Influence of scanning and reconstruction parameters on quality of three dimensional surface models of the dental arches from cone beam computed tomography. Clin. Oral. Investig. 2010, 14, 303–310. [Google Scholar] [CrossRef]
- Şeker, E.; Ozcelik, T.B.; Rathi, N.; Yilmaz, B. Evaluation of marginal fit of CAD/CAM restorations fabricated through cone beam computerized tomography and laboratory scanner data. J. Prosthet. Dent. 2016, 115, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Shenoy, A.; Maiti, S.; Nallaswamy, D.; Keskar, V. An in vitro comparison of the marginal fit of provisional crowns using the virtual tooth preparation workflow against the traditional technique. J. Indian. Prosthodont. Soc. 2023, 23, 391–397. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Neves, F.D.; Prado, C.J.; Prudente, M.S.; Carneıro, T.A.; Zancopé, K.; Davı, L.R. Microcomputed tomography evaluation of marginal fit of lithium disilicate crowns fabricated by using chairside CAD/CAM systems or the heat-pressing technique. J. Prosthet. Dent. 2014, 112, 1134–1140. [Google Scholar] [CrossRef] [PubMed]
- Bayrak, A.; Akat, B.; Ocak, M.; Kılıçarslan, M.; Özcan, M. Micro-computed tomography analysis of fit of ceramic inlays produced with different CAD software programs. Eur. J. Prosthodont. Restor. Dent. 2020, 28, 1–6. [Google Scholar]
- Revilla-León, M.; Özcan, M. Additive manufacturing technologies used for processing polymers: Current status and potential application in prosthetic dentistry. J. Prosthodont. 2017, 28, 146–158. [Google Scholar] [CrossRef]
- Dawood, A.; Marti Marti, B.; Sauret-Jackson, V.; Darwood, A. 3D printing in dentistry. Br. Dent. J. 2015, 219, 521–529. [Google Scholar] [CrossRef]

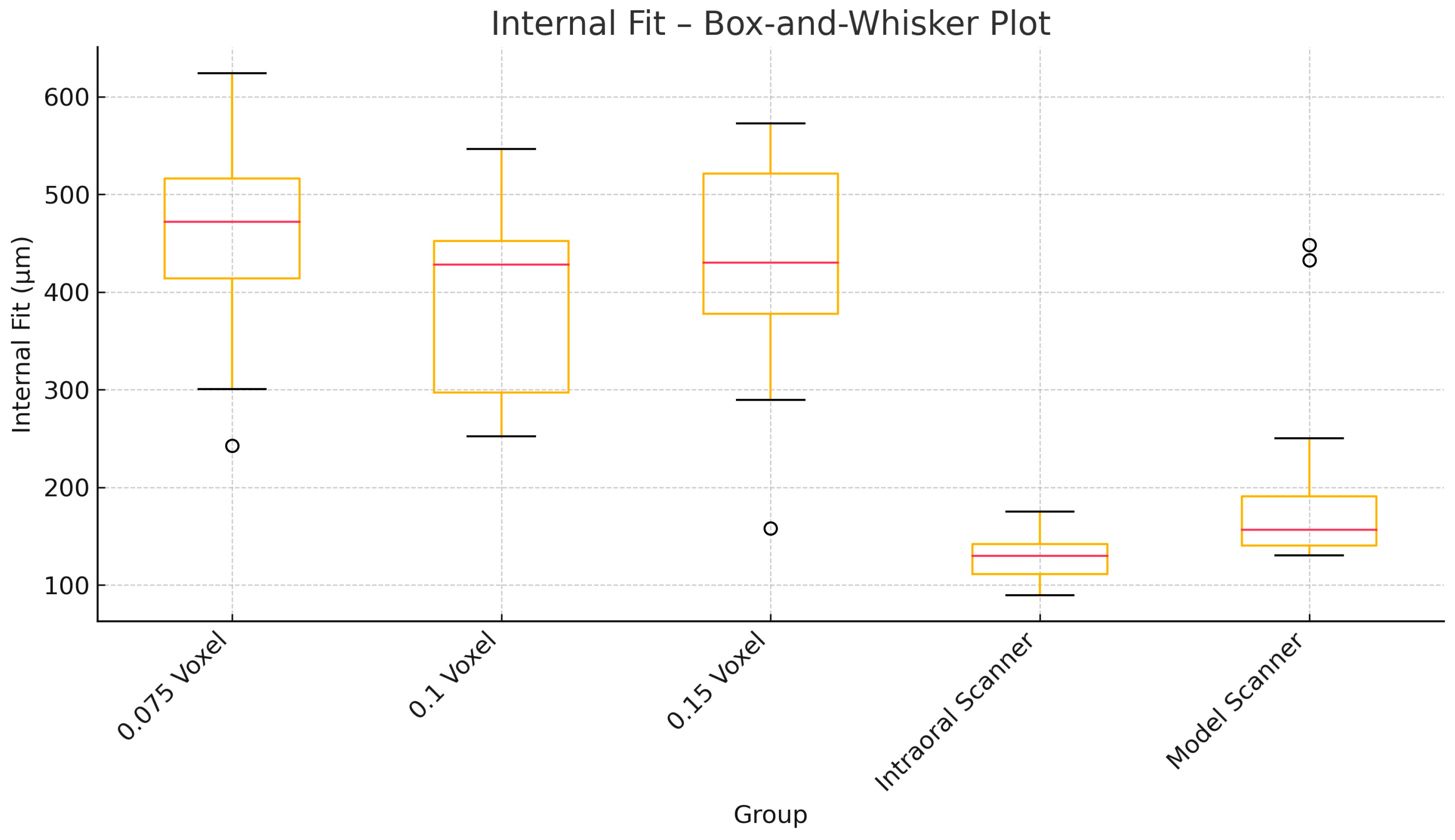
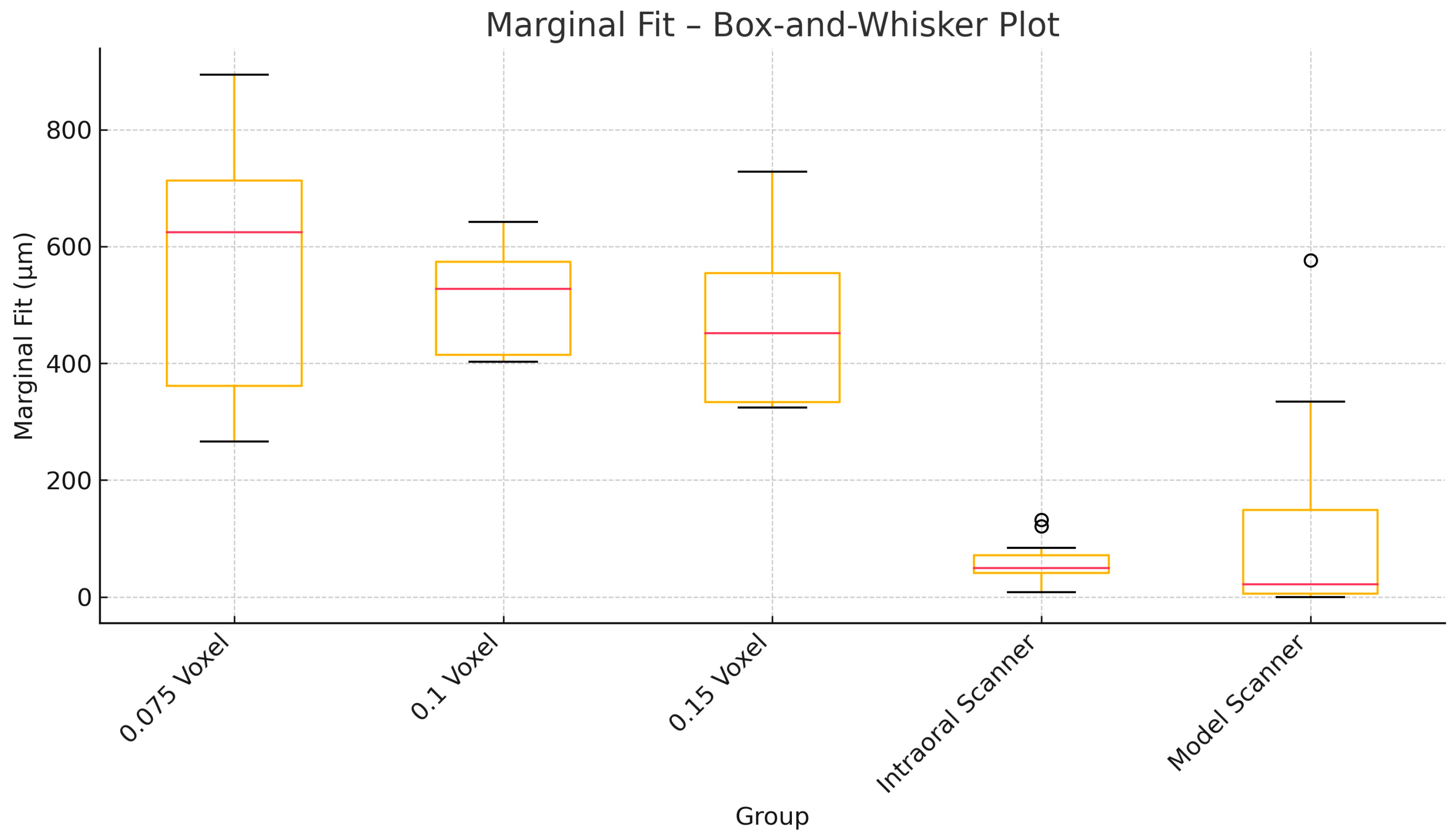
| Group | Marginal Fit (Mean ± SD, µm) | Internal Fit (Mean ± SD, µm) |
|---|---|---|
| 0.075 voxel | 464 ± 139 | 424 ± 122 |
| 0.1 voxel | 513 ± 86 | 396 ± 94 |
| 0.15 voxel | 580 ± 204 | 502 ± 106 |
| Intraoral scanner | 176 ± 61 | 178 ± 71 |
| Model scanner | 77 ± 36 | 117 ± 58 |
| Group | Variable | N | Mean (µm) | Standard Deviation | 95% CI Lower | 95% CI Upper | Shapiro p |
|---|---|---|---|---|---|---|---|
| 0.075 voxel | Marginal fit | 12 | 464.06 | 138.54 | 376.04 | 552.09 | 0.1053 [Normal] |
| 0.075 voxel | Internal fit | 12 | 424.18 | 121.72 | 346.84 | 501.51 | 0.3547 [Normal] |
| 0.1 voxel | Marginal fit | 12 | 513.44 | 86.24 | 458.64 | 568.23 | 0.1402 [Normal] |
| 0.1 voxel | Internal fit | 12 | 395.83 | 94.06 | 336.07 | 455.58 | 0.2779 [Normal] |
| 0.15 voxel | Marginal fit | 12 | 579.78 | 204.40 | 449.91 | 709.65 | 0.4305 [Normal] |
| 0.15 voxel | Internal fit | 12 | 456.62 | 114.83 | 383.66 | 529.58 | 0.5639 [Normal] |
| Intraoral | Marginal fit | 12 | 58.76 | 38.64 | 34.21 | 83.31 | 0.3198 [Normal] |
| Intraoral | Internal fit | 12 | 127.49 | 24.90 | 111.67 | 143.31 | 0.8254 [Normal] |
| Model | Marginal fit | 12 | 121.28 | 186.87 | 2.55 | 240.01 | 0.0009 [Not] |
| Model | Internal fit | 12 | 205.91 | 114.01 | 133.47 | 278.34 | 0.0004 [Not] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akat, B.; Şentürk, A.; Ocak, M.; Kılıçarslan, M.A.; Orhan, K.; Önder, M.; Gönüldaş, F. Quantitative Evaluation of Marginal and Internal Fit of CAD/CAM Ceramic Crown Restorations Obtained by Model Scanner, Intraoral Scanner, and Different CBCT Scans. Appl. Sci. 2025, 15, 8017. https://doi.org/10.3390/app15148017
Akat B, Şentürk A, Ocak M, Kılıçarslan MA, Orhan K, Önder M, Gönüldaş F. Quantitative Evaluation of Marginal and Internal Fit of CAD/CAM Ceramic Crown Restorations Obtained by Model Scanner, Intraoral Scanner, and Different CBCT Scans. Applied Sciences. 2025; 15(14):8017. https://doi.org/10.3390/app15148017
Chicago/Turabian StyleAkat, Bora, Ayben Şentürk, Mert Ocak, Mehmet Ali Kılıçarslan, Kaan Orhan, Merve Önder, and Fehmi Gönüldaş. 2025. "Quantitative Evaluation of Marginal and Internal Fit of CAD/CAM Ceramic Crown Restorations Obtained by Model Scanner, Intraoral Scanner, and Different CBCT Scans" Applied Sciences 15, no. 14: 8017. https://doi.org/10.3390/app15148017
APA StyleAkat, B., Şentürk, A., Ocak, M., Kılıçarslan, M. A., Orhan, K., Önder, M., & Gönüldaş, F. (2025). Quantitative Evaluation of Marginal and Internal Fit of CAD/CAM Ceramic Crown Restorations Obtained by Model Scanner, Intraoral Scanner, and Different CBCT Scans. Applied Sciences, 15(14), 8017. https://doi.org/10.3390/app15148017








