Featured Application
Stabilizing device for electromagnetic articulograph sensors.
Abstract
Electromagnetic articulography is a technique developed for recording three-dimensional movements. It is based on magnetic induction, where small currents are induced in miniature receiver coils acting as motion sensors by means of electromagnetic fields generated by transmitter coils. This technology has been applied in dental research to record mandibular movements during mastication, Posselt’s envelope of motion, and micromovements of dental prostheses. The AG501 electromagnetic articulograph (Carstens Medizinelektronik GmbH, Bovenden, Germany) provides a Head Correction (HC) procedure to eliminate head movement, which requires the reference sensors to be firmly attached to the subject’s head. If the sensors shift during the recordings, it becomes necessary to reposition them and repeat the head correction procedure. The aim of this study was to develop a 3D-printed helmet to securely fix the reference sensors to the head of a subject in the context of performing a series of recordings involving the mastication of 36 foods and the execution of Posselt’s envelope of motion. The number of HCs required was recorded for a group using the helmet and for a control group in which the sensors were attached to the subject’s head using tissue adhesive. A total of 29 recordings were conducted with and without the helmet. Without the helmet 44 HCs were required; on the other hand, with the helmet 36 HCs were required. On average, 1.5 HCs were required per session without the helmet and 1.2 HCs with the helmet, showing a non-significant difference (p < 0.05). A reduction in the number of HCs required per session was observed. However, more than one HC was still needed to complete a session. This could be addressed in future research by designing a series of helmets that adapt to different head sizes.
1. Introduction
The analysis of mandibular movement is of great interest in the field of dentistry. It has implications for the development of new full digital workflows for temporomandibular disorders treatment [1,2], the study of the temporomandibular joint (TMJ) condition [3], bruxism [4], relationship between cognitive decline and kinematic parameters of mastication [5] and relationship between dental status and food intake [6] among others. Certain studies require simple recording methods, which capture only aspects such as chewing time, the number of masticatory cycles, and frequency (derived from the previous variables). For this purpose, video recording alone is sufficient [6,7]. More complex studies that involve mandibular position in space require not only the tracking of mandibular movement but also the isolation of this movement from head movement [8,9,10,11,12].
Various technologies have been developed for this purpose. Ferrario et al. designed a system based on external markers and motion capture using six cameras. Three of these markers were placed on the head, while the other three were attached to a frame fixed to the mandible [13]. Other systems are based on the emission of ultrasound, with the transmitter attached to the mandible and the receiver fixed to the head. The system determines the mandibular position by measuring the time it takes for the sound waves to reach the receiver [14]. Kinesiography is based on recording the movement of a magnet attached to the mandible by means of a sensing system fixed to the head [15]. Electromagnetic articulography (EMA) was originally developed for use in the field of speech–language pathology, enabling the recording of tongue movement during speech [16]. It consists of a set of emitter coils that generate electromagnetic fields at different frequencies. These induce a current in small receiver coils, which is acquired by the equipment and used to determine the spatial position of the receiver coils that act as motion sensors [17]. While there are various methods for recording the movement of external structures, such as the lips and mouth, during speech [18], EMA allows for the recording of internal structures, such as the tongue [19,20]. These techniques appear to be safer than alternatives that require radiation, such as cineradiography [21] and fluoroscopy [22]. Ultrasound [23,24] and MRI [25] are alternative techniques that provide movement records without exposing subjects to radiation. While these systems offer a full view of mouth and tongue movements, it is more difficult to determine spatial coordinates from these recordings.
EMA has been employed in various studies conducted at the Oral Physiology Laboratory of the Universidad de La Frontera, focusing on dental research. This technique has been applied to the analysis of tongue and mandibular movements during chewing [26], speech [27], and swallowing [28], as well as in the evaluation of denture micromovements [29]. All these studies utilized the AG501 electromagnetic articulograph (Carstens Medizinelektronik GmbH, Bovenden, Germany). Tests using the AG 501 were conducted on young adults [26,27,28] or involved only chewing movements [29]; consequently, skin movement may have been reduced, as increased age is associated with greater skin laxity [30,31].
This equipment not only allows for recording movement but also isolates it from other movements that may interfere. In the case of mandibular and tongue movements, it is possible to eliminate head movement using the head correction procedure. This consists in the use of reference sensors that are attached to skin on glabella and left and right mastoid processes [28]. With these sensors adhered to the patient’s head, a first record is made and used as reference to eliminate head movement in the next records. This procedure uses the algorithms based on analysis of Procrustes developed by Gower [32] as well as Rohlf and Slice [33].
However, because the sensors are attached to the skin, they can shift as the patient moves their head or chews, displacing the sensors from their original position during the Head Correction. This is known as skin motion artifact [34] and causes the equipment to lose calibration, requiring the Head Correction procedure to be repeated. In their work, Wang et al. [20,35,36] used glasses to attach the reference sensors to avoid skin movement error. Although skin movement is minimal during speech analysis and does not significantly affect the accuracy of reference sensors, in chewing and border movement analyses this may pose a limitation, as the mastoid skin tends to move with the mandible during these tasks.
In this work, we develop a 3D-printed helmet to secure the reference sensors. This study was conducted within the context of research involving older adults and extensive recording sessions. Therefore, efforts were made to reduce the number of head correction procedures required during each session in order to improve participant comfort. The number of head corrections performed during each recording session was used as a method to evaluate the effect of the helmet on the fixation of the reference sensors, as repeating this procedure multiple times during the recordings increases the session duration and may cause discomfort to the subject. This device is designed to provide greater stability and allow for faster preparation of the reference sensors in studies using electromagnetic articulography, which is employed in oral physiology and dental research.
2. Materials and Methods
2.1. Helmet Design
The helmet was designed and printed by the Department of Computer Science and Informatics of the Universidad de la Frontera. The design was based on a public design from Printables.com made by the user OpenTechLab (Neural Interface—Printed Parts by OpenTechLab|Download Free STL Model, s. f.) which is licensed under a Creative Commons license (4.0 International License).
The original model was simplified by removing all components and leaving only the head support structures (Figure 1). This was done using Fusion 360 (Version 2.0.19440, Autodesk Inc., San Francisco, CA, USA). Three arms were created that conformed to the shape of the head and allowed the placement of three reference sensors in a distribution similar to that achieved when they are placed on the skin (glabella and left and right mastoid processes) (Figure 2). The lateral arms consist of a single piece (Figure 2a), while the upper arm was printed separately (Figure 2b) due to the printer’s size limitations. Additionally, a guide channel was created to allow each sensor cable to adapt smoothly to the shape of the helmet (Figure 2c). These modifications were made using Tinkercad (Autodesk, Inc. San Francisco, CA, USA). The final STL file was created with Fusion 360.
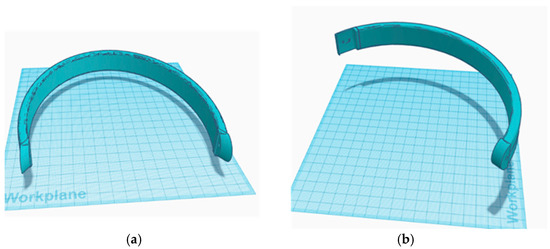
Figure 1.
Pieces of helmet designed. (a) Lateral arms. (b) Superior arm.
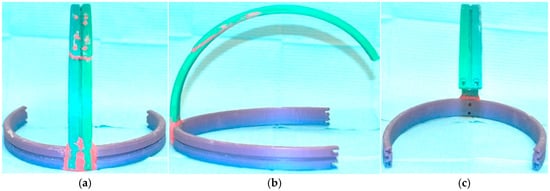
The helmet was printed with a fused filament fabrication 3D printer model 3DWOX 1 (Sindoh Co., Seongsui-ro 24-gil, Seongdong-gu, Seoul, Korea) using 3DWOX Desktop (Windows) software (Version 1.6.3220, Sindoh Co., Seongsui-ro 24-gil, Seongdong-gu, Seoul, Korea). Both parts were printed resting on their edges. The printing parameters were set as follows: layer height of 0.2 mm, infill density of 15% using a mesh pattern, printing temperature of 200 °C, and bed temperature of 60 °C. Support structures were required, configured with a zigzag pattern, a support angle of 40°, and a density of 50%. Bed adhesion was ensured using a skirt type. Finally, both parts were welded using a 3D pen (3D PEN-2, Qiya Technology Co., Ltd., Huizhou, China). All prints were performed using 1.75 mm PLA filament (Shenzhen Creality 3D Technology Co., Ltd., Shenzhen, China).
The helmet was designed with the intention of allowing the combined use of electromagnetic articulography and surface electromyography (sEMG) of the masseter and anterior temporal muscles. For this reason, the helmet does not fully enclose the head and leaves the temporal regions uncovered to permit electrode placement on the temples. No fit tests were conducted prior to the execution of the study.
2.2. Electromagnetic Articulography
Electromagnetic articulography is a motion recording technique based on magnetic induction. The electromagnetic articulograph AG 501 (Carstens Medizinelektronik GmbH, Bovenden, Germany) operates by means of three pairs of coils that emit electromagnetic fields at different frequencies. These fields induce small currents in receiver coils of 2 × 2 mm. These currents are detected by the system and used to determine the spatial position of each coil. When the coil is attached to a structure of interest, its movement can be recorded.
The AG 501 allows the connection of up to 16 sensors. These sensors must be pre-calibrated, following the procedure established by manufacturer, in an automatic process that takes approximately 20 min. Once calibration is complete, the sensors can be used in multiple recording sessions without the need for recalibration. Each set of sensors has its own calibration file, which is loaded when the system interface is opened.
During the recording sessions, although the sensors are physically identical, they can be classified into two types according to their function: motion sensors, which are used to record the movement of the structure of interest, and reference sensors, which the system uses during the head correction procedure to eliminate unwanted movement from the motion sensor recordings.
In this work, the reference sensors were placed either on the head of subjects or on the helmet, depending on the condition, and were used to remove head motion from the recordings of the motion sensor. The motion sensor was placed below the midline between the lower central incisors and was used to record mandibular movement.
2.3. Reference Sensors
2.3.1. Sensor Placement on Helmet
References sensors used for head correction were placed over the helmet following the channels present in each arm (Figure 3a). These are sensors of 2 × 2 mm, model HS150-L120-B (Carstens Medizinelektronik GmbH, Bovenden, Germany). They were attached to the helmet using microporous adhesive paper tape of 5 cm width (Reutter, Santiago de Chile, Chile). A double fixation was used. First each sensor was fixed in the most frontal point of each arm. After that, the wire of each sensor was secured to keep the wire from pulling directly from the coils when the subject moves (Figure 3b).
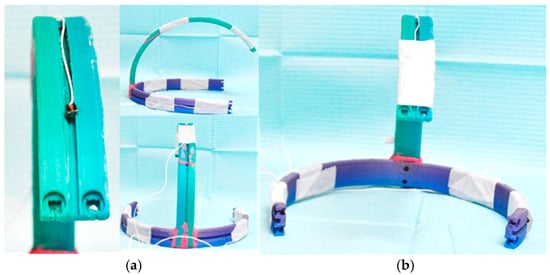
Figure 3.
Printed helmet with sensors attached with paper tape. (a) Sensor placed in the guide channel. (b) Sensors secured with paper tape.
2.3.2. Sensor Placement on Head
Reference sensors were placed on left and right mastoid processes (Figure 4a) and glabella (Figure 4b) with tissue adhesive (Epiglu; Meyer-Haake GmbH, Ober-Mörlen, Germany).

Figure 4.
Reference sensors attached to the skin of patient. (a) Mastoid process. (b) Glabella.
2.4. Subjects
The tests were conducted on subjects with functional dentition (21 or more teeth) or complete denture wearers between 60 and 80 years old, without signs or symptoms of temporomandibular disorders. This study is part of the project entitled “Novel dietary guidelines for elderly denture wearers to ensure adequate nutritional intake, good quality of life, and enhanced performance on cognitive tasks”, in which participants are required to chew a series of food items and perform Posselt’s envelope of motion recordings as part of the protocol. The subjects were recruited through convenience sampling.
Two groups were tested. The first group (control) was assessed without the helmet (12 women, 5 men, aged 62 ± 1.2), all participants with functional dentition, and the second group was assessed using the helmet (15 women, 3 men, aged 61 ± 1.5), 15 subjects with functional dentition and 3 complete denture wearers. The participants were invited to be part of the study after signing an informed consent form. The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Scientific Ethical Committee of the Universidad de La Frontera, Temuco, Chile (folio N°068_23).
2.5. Testing Condition
Participants were asked to perform Posselt’s polygons and chew a series of foods (Appendix A Table A1). Posselt’s polygons represent the extreme, non-functional mandibular movements that the jaw is capable of performing. An envelope can be defined for each spatial plane, outlining the maximum range of mandibular motion. A full description of these foods and its selection is described by Marinelli et al. [37]. Based on the results of this study, a set of foods was selected from each group, including items with different levels of hardness, in order to assess mandibular movement as a function of food hardness. Due to the extensive number of food items included in the protocol, data collection was conducted across two separate recording sessions. Each session was planned to last approximately one hour in order to minimize participant discomfort and fatigue.
The first session involved the execution of Posselt’s envelope of motion and the mastication of selected dairy products, fruits, and vegetables. The second session included only the mastication assessment of food items belonging to the vegetal protein, animal protein, cereals and grains, and high lipid foods and others groups, as well as peanuts (Appendix A Table A1).
The subject was placed under the AG501 (Figure 5). The three Posselt’s polygons were recorded first. The subject was initially instructed to hold their head in a straight position, and a brief practice period was allowed before each recording. The polygons were recorded in the following order: frontal, sagittal, and horizontal.
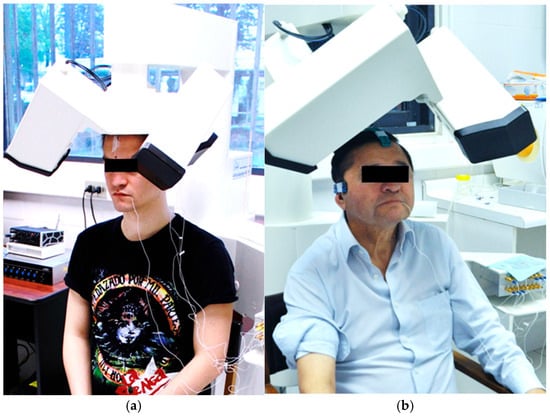
Figure 5.
Subject placement under EMA’s transmitter coils. (a) Sensors on skin. (b) Sensors in helmet.
The frontal polygon consisted of four movements. The first movement was recorded by asking the subject to move the jaw from maximum intercuspation (MIC) to the extreme right lateral position. Then, the subject was instructed to perform a right border opening movement until reaching maximum mouth opening (MMO). The same procedure was repeated on the left side.
The sagittal polygon consisted of two movements. The first movement was recorded by asking the subject to move the jaw from MIC to the extreme protrusive position, passing through the edge-to-edge position. From there, the subject performed a protrusive opening movement until reaching MMO. The second movement started in MIC and the subject performed an extreme retrusive movement. From that position, the subject performed an extreme retrusive opening movement until MMO was reached.
The horizontal polygon consisted of two symmetrical movements. Starting from MIC, the subject performed a lateral mandibular movement with tooth contact to the extreme right lateral position. From that point, the movement continued with a lateral border protrusive movement until the midsagittal plane was reached.
For chewing tasks, the food portion was placed in the participant’s mouth, and they were instructed to hold it between the tongue and palate until given the signal to begin chewing. The participant was asked to chew until they felt the urge to swallow and to raise their hand upon reaching this point. At that moment, the recording was stopped. Posselt’s polygons and chewing were recorded once.
The protocols used to record chewing and Posselt’s polygons have been previously described by Lezcano et al. [38].
2.6. Recording Sessions and Participant Distribution
In the group without the helmet, 10 out of 17 participants completed both recording sessions, while 6 participants completed only the first session. One participant completed three sessions due to a data-saving error in the second session, which required it to be repeated. However, this did not affect the count of Head Corrections (HCs) performed, and all three sessions were included in the analysis.
In the group using the helmet, 11 participants completed both sessions, while 7 participants completed only the first session.
2.7. Head Correction
2.7.1. Description
To eliminate head movement from the movement of the incisal sensor, the AG501 uses a procedure called Head Correction (HC). This process involves applying a rotation–translation matrix (RTM) to the sensors. The matrix is generated from a static recording of the reference sensors.
To apply HC, it is first necessary to generate a 3D reference object. For this, a static recording of the reference sensors (three sensors placed on the skin or on the helmet) is made while asking the subject to hold their head straight and still. This recording lasts 5 s. From it, the software generates the spatial reference object. Based on this object, for each frame of subsequent recordings, the system calculates the RTM to achieve the best alignment of the reference sensors—which move with the subject’s head—with the initial reference using a least-squares criterion. The same RTM is then applied to the movement sensor, thereby eliminating head movement.
During this correction, the system calculates the distance between the corrected position of the reference sensors and the initial recording. This is known as the taxonomic distance and is the square root of the average of the squared distances between all reference sensors and their corresponding positions in the reference object. If this value exceeds a certain threshold, the system displays an error message, indicating that one of the reference sensors has loosened or shifted from its original relative position (Figure 6). Figure 6 illustrates an example in which the mean taxonomic distances exceed the established threshold of 1.5 mm. This suggests the need to review either the head correction sweep or the placement of the reference sensors. The EMA system allows the selection of the sweep used for head correction, which may represent a potential source of error. Alternatively, one of the sensors may have shifted from its original position during the reference sweep, requiring repositioning and recalibration.
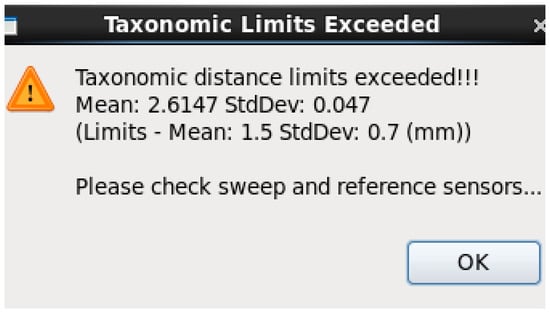
Figure 6.
Warning signal that the taxonomic distance limits have been exceeded.
2.7.2. Number of Head Correction per Session
Once the recording session began, the subject was asked to perform Posselt’s polygons and then chew the foods listed in Appendix A. During these sessions, if the established taxonomic distance limit was exceeded (Mean: 1.5 mm, StdDev: 0.7 mm), the sensors were adjusted by reattaching them with adhesive. A new HC was then performed, and recordings continued until the session was completed. During the sessions, the number of HCs performed until the end of the session was recorded.
2.8. Statistical Analysis
The Shapiro–Wilk test was used to assess data normality due to the small sample size (n = 29 per group). The number of HCs per session was analyzed as the dependent variable. Since the data did not follow a normal distribution, the non-parametric Mann–Whitney U test was employed to compare differences between groups (helmet vs. no helmet). The Wilcoxon signed-rank test was used to compare paired samples. A one-sample Wilcoxon signed-rank test was conducted to assess whether the median differed from the theoretical value of 1. The level of statistical significance was set at p < 0.05.
3. Results
A total of 29 recordings were conducted with and without the helmet. Table 1 provides a summary of the results obtained.

Table 1.
Number of head corrections for group with reference sensors on skin and on helmet.
Figure 7 shows the frequency diagram of number of HC procedures performed in each recording session with the sensors placed on the subject’s skin (S) and those placed on the helmet (H). Twenty (69%) sessions with the reference sensor on skin required only one HC, four (14%) required two and three HC, and one (3%) required four HC. When sensors were placed on the helmet, 23 (79%) required 1 HC, 5 (17%) sessions required 2 HC and 1 (3%) required 3 HC. The descriptive measures for each group were as follows: in the group without the helmet, the median was 1.5 (range: 1–4), while in the group with the helmet, it was 1.2 (range: 1–3). No statistically significant differences were found between the groups (p > 0.05). Figure 8 shows a violin graph summarizing these data.
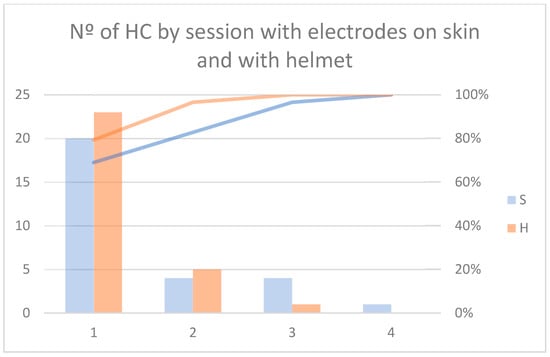
Figure 7.
Frequency diagram with number of head correction procedures performed in sessions with sensors on skin (S) and attached to helmet (H).
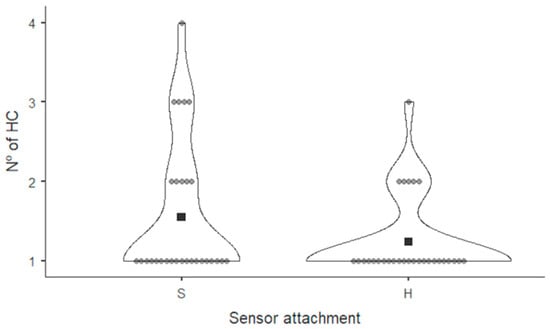
Figure 8.
Violin graph with number of head correction procedure realized in sessions with sensors on skin (S) and attached to helmet (H). Squares point mean value.
No significant differences were found when comparing Session 1 and Session 2 between the group that used the helmet and the group with sensors adhered to the skin (Table 2).

Table 2.
Number of head corrections performed in each session.
The number of head corrections performed in Sessions 1 and 2 was compared across all participants, regardless of group assignment. This analysis aimed to evaluate potential variability between sessions. Significant differences were found between the recording sessions (Table 3).

Table 3.
Number of head corrections performed in Sessions 1 and 2.
When the variation between sessions was analyzed in both groups, no significant differences were found. For this analysis, data from participants who completed both sessions were used (Table 4).

Table 4.
Number of head corrections for the subjects that performed both sessions.
Finally, a comparison was made against the ideal value of one head correction per session (Table 5). For both groups—sensors attached to the skin or to the helmet—Session 1 showed a value significantly different from 1. In contrast, in Session 2, neither group showed a significant difference from 1.

Table 5.
Mean number of HCs per session in comparison to the ideal value of 1.
4. Discussion
Electromagnetic articulography is a technique that allows the recording of mandibular movement while compensating for head motion. It differs from other technologies, such as video-based marker tracking [13], ultrasound systems [14], or kinesiography [15], by enabling the attachment of the motion sensor inside the oral cavity and by not requiring a facebow to eliminate head movement. However, since reference sensors must remain in a fixed position throughout the entire recording to perform head correction, multiple calibrations may be necessary during a single session. This can be a limitation for long recordings or for protocols requiring border movements. In addition, participants must be instructed to avoid excessive head movements to prevent the cables from pulling on the sensors. This may cause discomfort to the subject and restrict the types of studies that can be conducted using this technology. In the present study, a sensor fixation device was developed to address these limitations and expand the applicability of electromagnetic articulography in dental research.
A reduction in the need to perform repeated head corrections during the session when using the helmet was observed; however, this difference was not statistically significant (Table 1). In addition, the total number of head correction procedures required per session tended to decrease. This is illustrated in Figure 7 and Figure 8, where, in the case of participants with reference sensors attached to the skin, one subject required four head corrections to complete the recording session (Session 1), and four others required three head corrections (three in Session 1 and one in Session 2). In contrast, when using the helmet, only one subject required three head corrections to complete the recording session (Session 1). Table 2 shows an improvement when using the helmet in both sessions 1 and 2; however, no statistically significant differences were found.
The need for multiple head corrections during a session may be influenced by the type of exercises performed in each session. As shown in Table 3, there was a significant reduction in the number of head corrections required between Session 1 and Session 2, regardless of helmet use. This difference may be explained by the fact that, in Session 1, the Posselt’s envelope exercises were performed, which involve instructing the participant to make extensive border mandibular movements. These movements can displace the skin where the reference sensors are attached, leading to potential misalignment of the reference system. Moreover, it was observed during the study that some participants tended to rotate their heads while performing lateral border movements, as well as during the frontal and horizontal envelope exercises, potentially pulling the cables and misaligning the reference system. This may explain why more head corrections were required in Session 1 compared to Session 2. In Table 4, participants who completed both sessions were compared. Again, Session 1 required more head corrections in both groups; however, no statistically significant differences were detected.
Ideally, only one Head Correction would be required per recording session, but because of skin motion, the reference sensors can move and a new Head Correction is required to continue with the recordings. Table 5 presents a comparison of the number of head corrections performed in Sessions 1 and 2, with and without the helmet, against the ideal value of one head correction per session. In Session 2, neither the helmet nor the non-helmet group showed significant differences compared to the ideal value. The helmet group completed all Session 2 recordings with a single head correction.
Due to the positioning of the reference sensors on the mastoid processes and the glabella, misalignment of the reference sensors may occur. The sensors located on the mastoid processes are affected by mandibular movements, as these movements displace the skin in these areas. The sensor on the glabella may be influenced by head movements and involuntary actions, such as eyebrow raising, which also shift the skin. In the case of the helmet, it is primarily affected by head movements that may pull on the cables and cause displacement; however, it isolates the skin movements. This may explain why the need to perform multiple head corrections during recording sessions persists, albeit with a reduced frequency
Skin motion artifacts have been described in literature [39]. This is a result of skin elasticity and depends on factors, such as age, body mass index and movement extent. In other motion capture studies, this problem is addressed by using simple fixation methods, such as tape [40] or elastic warps [34]. Due to the nature of the head correction procedure, these methods are insufficient, since the limit is on the order of 1.5 mm for the three sensors. If the three sensors are loose, even small displacements contribute to an increase in the taxonomic distance, and head correction cannot be performed. If sensors are placed on an elastic surface, such as elastic wraps, any change in the tension of the wrap modifies the relative positions of the reference sensors and increases the taxonomic distance.
In previous studies analyzing mastication or Posselt’s envelope of motion, the samples consisted of subjects aged between 20 and 30 years; therefore, skin laxity was not an issue and skin fixation was sufficient. In our study, tests were conducted on subjects aged between 60 and 80 years, and Posselt’s envelope of motion was analyzed, which requires the subject to move the mandible to extreme positions. Consequently, skin movement may have increased due to the age-related laxity. Moreover, participants were asked to chew a variety of foods, whereas in previous studies only peanuts and carrots were used [26,27,28].
Another consideration in the design of the present helmet in the context of dental research was the use of sEMG to record anterior temporal muscle activity, along with electromagnetic articulography [38]. To allow this function, the anterior temporal area must be free for electrode placement. This could be an inconvenience if goggles, lens or elastic wraps are used as in the studies by Katz et al. [20] and Wang et al. [35,36].
Although the reduction in the average number of HCs seems to suggest a benefit of the helmet, statistical analysis indicates that this difference could be attributed to chance, possibly due to variability in the helmet’s fit. A possible solution to this problem is the design of a set of helmets that adapt to different head sizes or to design an adjustable fixation system. On the other hand, the use of the helmet allows preparation prior to the subject’s arrival, which saves recording time. A limitation of this study is the small sample size. For this reason, statistical analyses comparing male and female participants, as well as those with functional dentition and complete denture wearers, were not performed. In addition, no method was established to verify the level of sensor fixation.
The only similar device found in the literature was the use of plastic glasses by Katz et al. [20] and Wang et al. [35,36], but no comparison between the use of glasses and sensors on skin was made by these authors.
5. Conclusions
A 3D-printed helmet was designed to securely hold the reference sensors of the AG 501 electromagnetic articulograph, enabling its use in the analysis of mastication and Posselt’s envelope of motion in a sample of older adults. It was observed that a relevant factor influencing the number of head corrections required during a recording may be the performance of border movements, as both groups required a higher number of recalibrations. The helmet presented here could be useful in studies involving border movements. In studies limited to food mastication, its use might be unnecessary. The use of a helmet to secure the reference sensors instead of attaching them to the patient’s skin has shown a reduction in the number of HCs required during chewing recordings. However, situations still occur where more than one HC is needed to complete a session. This could be addressed in future research by designing a series of helmets that adapt to different head sizes.
Author Contributions
Conceptualization, F.M. and F.A.E.J.; methodology, F.M.; software, F.A.E.J.; validation, C.V.-O., G.C.-S., J.A. and G.Á.; formal analysis, F.M.; investigation, C.V.-O., G.C.-S., J.A. and G.Á.; resources, G.M. and R.F.F.; data curation, P.N.; writing—original draft preparation, J.A.; writing—review and editing, M.J.-P. and R.F.F.; visualization, F.M.; supervision, R.F.F.; project administration, R.F.F.; funding acquisition, R.F.F. All authors have read and agreed to the published version of the manuscript.
Funding
Project Fondecyt Regular Nº 1230616.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Comité Ético Científico De La Universidad De La Frontera, protocol code 068_23, 3 May 2023.
Informed Consent Statement
The participants have given consent for publication.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available since no public database is available.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A

Table A1.
List of Foods.
Table A1.
List of Foods.
| Session 1 | Session 2 | ||||||
|---|---|---|---|---|---|---|---|
| Fruits | Dairy | Vegetables | Vegetal Protein | Animal Protein | Cereals and Grains | High Lipid Food and Others | |
| Kiwi | Soft unsalted cheese | Tomato | Lentil 4 mm | Eggs | Oatmeal and milk | Yogurt and flax | Peanut |
| Orange | Chanco Cheese | Lettuce | Lentil 5 mm | Jack Mackerel | Whole-wheat sliced bread | Yogurt and chia | |
| Banana | Buttery cheese | Cucumber | Beans | Chicken thigh | Whole-wheat bread with seeds | Peach jam | |
| Sweet cucumber | Yogurt | Raw carrot | Chickpeas | Turkey breast | Whole-grain rice | PACAM cream | |
| Red apple | Ricotta | Raw beets | Split peas | Beef | Couscous | Avocado | |
References
- Chou, T.-H.; Liao, S.-W.; Huang, J.-X.; Huang, H.-Y.; Vu-Dinh, H.; Yau, H.-T. Virtual Dental Articulation Using Computed Tomography Data and Motion Tracking. Bioengineering 2023, 10, 1248. [Google Scholar] [CrossRef] [PubMed]
- Tecco, S.; Nota, A.; Pittari, L.; Clerici, C.; Mangano, F.; Gherlone, E.F. Full-Digital Workflow for TMDs Management: A Case Series. Healthcare 2023, 11, 790. [Google Scholar] [CrossRef] [PubMed]
- Silva, J.; Azevedo, A.; Martins, E.; Canabez, A.; Martin, D.; Martin, C. Mandibular Kinematics on an Orthodontic Population Assessed with an Optical Jaw Tracking System: A Comparative Study. Dent. J. 2025, 13, 184. [Google Scholar] [CrossRef] [PubMed]
- Tăut, M.; Chanteux, S.; Kui, A.; Buduru, R.; Negucioiu, M.; Manziuc, M.; Gheorghiu, I.; Hedeșiu, M.; Buduru, S.; Ilea, A. Condylar Parameters and Mandibular Movement Patterns in Bruxers Using an Optical Jaw Tracking System. J. Clin. Med. 2024, 13, 7761. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, E.; Tohara, H.; Kimura, M.; Koide, I.; Abe, K.; Yonenaga, K. Effect of Cognitive Decline on Mandibular Movement during Mastication in Nursing Home Residents. J. Clin. Med. 2024, 13, 6040. [Google Scholar] [CrossRef] [PubMed]
- Wee, M.S.M.; Goh, A.T.; Stieger, M.; Forde, C.G. Correlation of Instrumental Texture Properties from Textural Profile Analysis (TPA) with Eating Behaviours and Macronutrient Composition for a Wide Range of Solid Foods. Food Funct. 2018, 9, 5301–5312. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Doulah, A.; Farooq, M.; Parton, J.; McCrory, M.A.; Higgins, J.A.; Sazonov, E. Statistical Models for Meal-Level Estimation of Mass and Energy Intake Using Features Derived from Video Observation and a Chewing Sensor. Sci. Rep. 2019, 9, 45. [Google Scholar] [CrossRef] [PubMed]
- Radke, J.C.; Kamyszek, G.J.; Kull, R.S.; Velasco, G.R. TMJ Symptoms Reduce Chewing Amplitude and Velocity, and Increase Variability. CRANIO® 2019, 37, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Piancino, M.G.; Tortarolo, A.; Di Benedetto, L.; Crincoli, V.; Falla, D. Chewing Patterns and Muscular Activation in Deep Bite Malocclusion. J. Clin. Med. 2022, 11, 1702. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, M.; Shiga, H.; Ogura, S.; Sano, M.; Komino, M.; Takamori, H.; Uesugi, H.; Haga, K.; Murakami, Y. Functional Differences between Chewing Sides of Implant-Supported Denture Wearers. Prosthesis 2023, 5, 346–357. [Google Scholar] [CrossRef]
- D’Attilio, M.; Di Carlo, B.; Caroccia, F.; Moscagiuri, F.; d’Angelo, D.M.; Chiarelli, F.; Festa, F.; Breda, L. Clinical and Instrumental TMJ Evaluation in Children and Adolescents with Juvenile Idiopathic Arthritis: A Case—Control Study. Appl. Sci. 2021, 11, 5380. [Google Scholar] [CrossRef]
- Sato, R.; Kodama, S.; Okawa, J.; Murakami, K.; Ono, T.; Hori, K. Tongue and Jaw Movement Assessed by 3D Motion Capture during Gum Chewing. Front. Physiol. 2024, 15, 1409005. [Google Scholar] [CrossRef] [PubMed]
- Ferrario, V.F.; Sforza, C.; Lovecchio, N.; Mian, F. Quantification of Translational and Gliding Components in Human Temporomandibular Joint during Mouth Opening. Arch. Oral Biol. 2005, 50, 507–515. [Google Scholar] [CrossRef] [PubMed]
- Sójka, A.; Huber, J.; Kaczmarek, E.; Hędzelek, W. Evaluation of Mandibular Movement Functions Using Instrumental Ultrasound System: Mandibular Movement Analysis. J. Prosthodont. 2017, 26, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Clayton A, C.; Brian, E.H. Physiological State of Occlusal Orthotics and the Diagnosis of Myogenous Orofacial Pain in Reducing TMD Headaches and Other Symptoms. J. Dent. Probl. Solut. 2020, 7, 034–048. [Google Scholar] [CrossRef]
- Haworth, B.; Kearney, E.; Faloutsos, P.; Baljko, M.; Yunusova, Y. Electromagnetic Articulography (EMA) for Real-Time Feedback Application: Computational Techniques. Comput. Methods Biomech. Biomed. Eng. Imaging Vis. 2019, 7, 406–413. [Google Scholar] [CrossRef]
- Rebernik, T.; Jacobi, J.; Jonkers, R.; Noiray, A.; Wieling, M. A Review of Data Collection Practices Using Electromagnetic Articulography. Lab. Phonol. J. Assoc. Lab. Phonol. 2021, 12, 6. [Google Scholar] [CrossRef]
- Feng, Y.; Max, L. Accuracy and Precision of a Custom Camera-Based System for 2-D and 3-D Motion Tracking During Speech and Nonspeech Motor Tasks. J. Speech Lang. Hear. Res. 2014, 57, 426–438. [Google Scholar] [CrossRef] [PubMed]
- Teplansky, K.J.; Wisler, A.; Green, J.R.; Campbell, T.; Heitzman, D.; Austin, S.G.; Wang, J. Tongue and Lip Acceleration as a Measure of Speech Decline in Amyotrophic Lateral Sclerosis. Folia Phoniatr. Logop. 2023, 75, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Katz, W.F.; Mehta, S.; Wood, M.; Wang, J. Using Electromagnetic Articulography with a Tongue Lateral Sensor to Discriminate Manner of Articulation. J. Acoust. Soc. Am. 2017, 141, EL57–EL63. [Google Scholar] [CrossRef] [PubMed]
- McMicken, B.; Vento-Wilson, M.; Von Berg, S.; Rogers, K. Cineradiographic Examination of Articulatory Movement of Pseudo-Tongue, Hyoid, and Mandible in Congenital Aglossia. Commun. Disord. Q. 2014, 36, 3–11. [Google Scholar] [CrossRef]
- Taniguchi, H.; Matsuo, K.; Okazaki, H.; Yoda, M.; Inokuchi, H.; Gonzalez-Fernandez, M.; Inoue, M.; Palmer, J.B. Fluoroscopic Evaluation of Tongue and Jaw Movements During Mastication in Healthy Humans. Dysphagia 2013, 28, 419–427. [Google Scholar] [CrossRef] [PubMed]
- Mozaffari, M.H.; Guan, S.; Wen, S.; Wang, N.; Lee, W.-S. Guided Learning of Pronunciation by Visualizing Tongue Articulation in Ultrasound Image Sequences. In Proceedings of the 2018 IEEE International Conference on Computational Intelligence and Virtual Environments for Measurement Systems and Applications (CIVEMSA), Ottawa, ON, Canada, 12–13 June 2018; IEEE: Ottawa, ON, Canada, 2018; pp. 1–5. [Google Scholar]
- McAllister, T.; Preston, J.L.; Hitchcock, E.R.; Hill, J. Protocol for Correcting Residual Errors with Spectral, ULtrasound, Traditional Speech Therapy Randomized Controlled Trial (C-RESULTS RCT). BMC Pediatr. 2020, 20, 66. [Google Scholar] [CrossRef] [PubMed]
- Molnár, V.; Lakner, Z.; Molnár, A.; Tárnoki, D.L.; Tárnoki, Á.D.; Kunos, L.; Jokkel, Z.; Tamás, L. Ultrasound and Magnetic Resonance Imaging of the Tongue in Obstructive Sleep Apnoea. Appl. Sci. 2022, 12, 9583. [Google Scholar] [CrossRef]
- Vargas-Agurto, S.; Lezcano, M.F.; Álvarez, G.; Navarro, P.; Arias, A.; Fuentes, R. Análisis Cinemático de La Masticación de Alimentos Duros y Blandos En Participantes Dentados Utilizando Articulografía Electromagnética 3D. Int. J. Morphol. 2021, 39, 935–940. [Google Scholar] [CrossRef]
- Álvarez, G.; Ruiz, M.; Arias, A.; Lezcano, M.F.; Fuentes, R. Description of Acoustic and Articulatory Parameters of Vowels in Mapudungun Speakers. Pilot Study. Int. J. Odontostomatol. 2020, 14, 205–212. [Google Scholar] [CrossRef]
- Álvarez, G.; Dias, F.J.; Lezcano, F.; Arias, A.; Navarro, P.; Fuentes, R. Description of Tongue Movements on Swallowing Patterns. Arch. Oral Biol. 2020, 113, 104706. [Google Scholar] [CrossRef] [PubMed]
- Marinelli, F.; Venegas, C.; Ruiz, J.V.; Farfán-Beltrán, N.; Staub, E.; Navarro, P.; Alarcón-Apablaza, J.; Fuentes, R. Determination of Micromovements in Removable Prosthesis during Mastication: A Pilot Study with 3D Electromagnetic Articulography. Bioengineering 2024, 11, 229. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.; Yin, S.; Lu, X.; Fu, H.; Gao, H.; Zhang, S. Research on the Correlation Between Skin Elasticity Evaluation Parameters and Age. Cosmetics 2024, 11, 205. [Google Scholar] [CrossRef]
- Rostkowska, E.; Poleszak, E.; Wojciechowska, K.; Dos Santos Szewczyk, K. Dermatological Management of Aged Skin. Cosmetics 2023, 10, 55. [Google Scholar] [CrossRef]
- Gower, J.C. Generalized Procrustes Analysis. Psychometrika 1975, 40, 33–51. [Google Scholar] [CrossRef]
- Rohlf, F.J.; Slice, D. Extensions of the Procrustes Method for the Optimal Superimposition of Landmarks. Syst. Zool. 1990, 39, 40. [Google Scholar] [CrossRef]
- Ekdahl, M.; Ulman, S.; Butler, L. Relationship of Knee Abduction Moment to Trunk and Lower Extremity Segment Acceleration during Sport-Specific Movements. Sensors 2024, 24, 1454. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Green, J.R.; Samal, A.; Carrell, T.D. Vowel Recognition from Continuous Articulatory Movements for Speaker-Dependent Applications. In Proceedings of the 2010 4th International Conference on Signal Processing and Communication Systems, Gold Coast, Australia, 13–15 December 2010; IEEE: Gold Coast, Australia, 2010; pp. 1–7. [Google Scholar]
- Wang, J.; Green, J.R.; Samal, A.; Marx, D.B. Quantifying Articulatory Distinctiveness of Vowels. In Proceedings of the Interspeech, Florence, Italy, 27–31 August 2011; ISCA: Grenoble France, 2011; pp. 277–280. [Google Scholar]
- Marinelli, F.; Venegas, C.; Pirce, F.; Del Carmen Silva Celedón, J.; Navarro, P.; Jarpa-Parra, M.; Fuentes, R. Hardness Analysis of Foods in a Diet Based on the Mediterranean Diet and Adapted to Chilean Gastronomy. Foods 2024, 13, 3061. [Google Scholar] [CrossRef] [PubMed]
- Lezcano, M.F.; Dias, F.; Farfán-Beltrán, N.; Manzanares-Céspedes, M.C.; Cerda, C.; Fuentes, R. Synchronization of Surface Electromyography and 3D Electromagnetic Articulography Applied to Study the Biomechanics of the Mandible: Proof of Concept. Appl. Sci. 2023, 13, 5851. [Google Scholar] [CrossRef]
- Green, J.R.; Wilson, E.M.; Wang, Y.-T.; Moore, C.A. Estimating Mandibular Motion Based on Chin Surface Targets During Speech. J. Speech Lang. Hear. Res. 2007, 50, 928–939. [Google Scholar] [CrossRef] [PubMed]
- Valevicius, A.; Bushey, K.; Jenkyn, T. Validation of a Multi-Segment Kinematic Foot Model and Optical Motion Capture Using Bi-Planar X-Ray Fluoroscopy and a Markerless RSA Approach. Appl. Sci. 2024, 14, 11285. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).