In Vitro Accuracy of Two Different Electronic Apex Locators Under Various Conditions
Abstract
1. Introduction
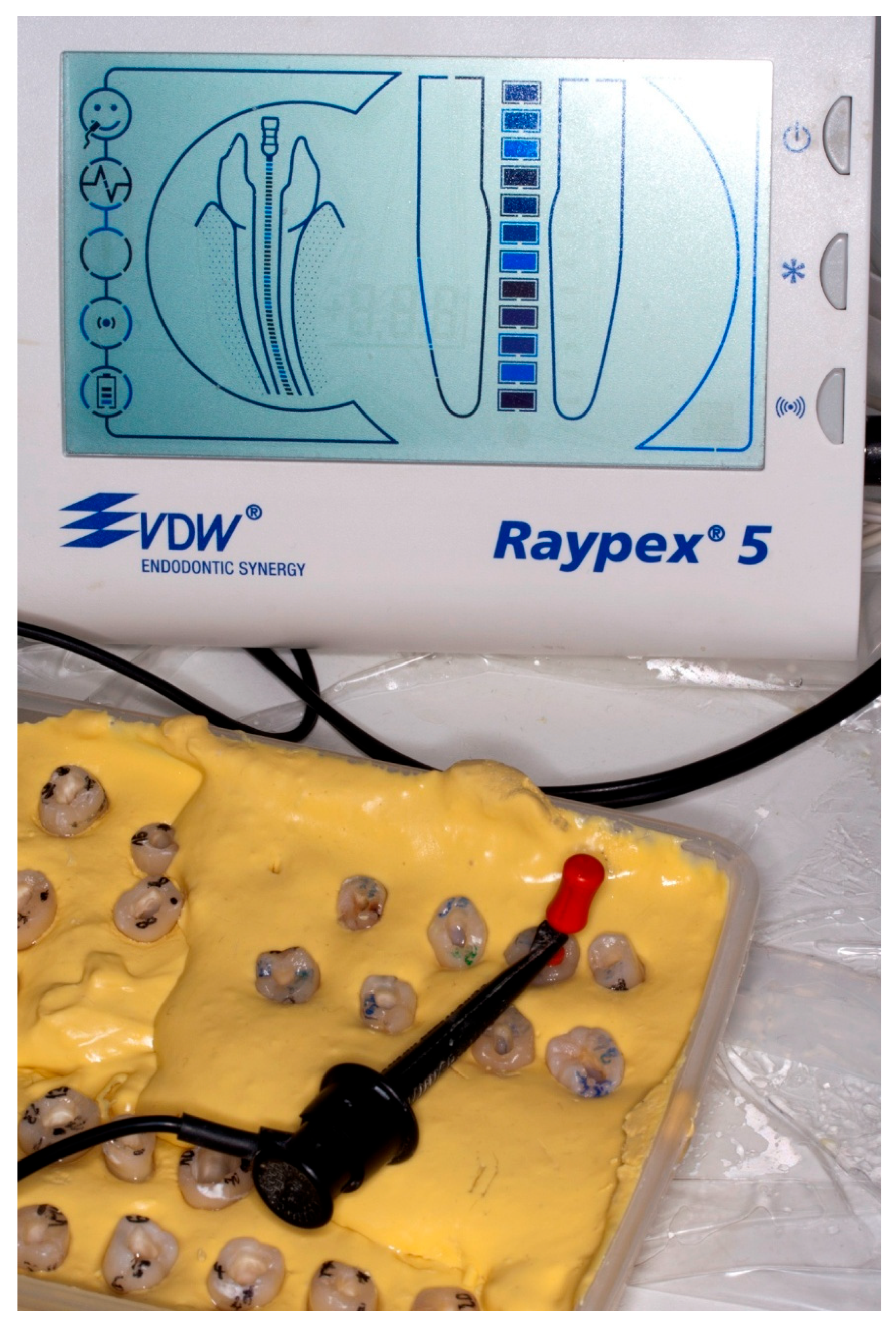
2. Materials and Methods
2.1. Teeth Selection and Preparation
2.2. Length Measurement
2.3. Electronic Length Measurement
- 0.9% saline (Pliva Hrvatska, Zagreb, Croatia),
- FileEZE EDTA 19% (Ultradent Products, South Jordan, UT, USA),
- Glyde EDTA 17% (Dentsply products, York, PA, USA),
- Consepsis V Chlorhexidine 2% CHX (Ultradent Products, South Jordan, UT, USA),
- Chlorcid 3% (Ultradent Products, South Jordan, UT, USA),
- Citric Acid 20% (Ultradent Products, South Jordan, UT, USA),
- EDTA 18% (Ultradent Products, South Jordan, UT, USA).
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACL | Actual Canal Length |
| EALs | Electronic Apex Locators |
| AF | Apical Foramen |
| ECL | Electronic Canal Length |
| WL | Working Length |
| GS | Gold standard |
References
- Sjogren, U.; Hagglund, B.; Sundqvist, G.; Wing, K. Factors affecting the long-term results of endodontic treatment. J. Endod. 1990, 16, 498–504. [Google Scholar] [CrossRef] [PubMed]
- Dummer, P.M.; McGinn, J.H.; Rees, D.G. The position and topography of the apical canal constriction and apical foramen. Int. Endod. J. 1984, 17, 192–198. [Google Scholar] [CrossRef] [PubMed]
- Farzaneh, M.; Abitbol, S.; Lawrence, H.P.; Friedman, S. Treatment outcome in endodontics—The Toronto Study. Phase II: Initial. treatment. J. Endod. 2004, 30, 302–309. [Google Scholar] [CrossRef] [PubMed]
- Martos, J.; Ferrer-Luque, C.M.; González-Rodríguez, M.P.; Castro, L.A. Topographical evaluation of the major apical foramen in permanent human teeth. Int. Endod. J. 2009, 42, 329–334. [Google Scholar] [CrossRef]
- West, J.D.; Roane, J.B.; Goerig, A.C. Cleaning and shaping the root canal length system. In Pathways of the Pulp, 6th ed.; Cohen, S., Burns, R.C., Eds.; Mosby: St. Louis, MO, USA, 1994; pp. 179–218. [Google Scholar]
- Suzuki, K. Study on iontophoresis. J. Jap Stomato 1942, 16, 411–417. [Google Scholar]
- Ebrahim, A.K.; Wadachi, R.; Suda, H. An in vitro evaluation of the accuracy of Dentaport ZX apex locator in enlarged root canals. Aust. Dent. J. 2007, 52, 193–197. [Google Scholar] [CrossRef]
- Huang, L. An experimental study of the principle of electronic root canal measurement. J. Endod. 1987, 13, 60–64. [Google Scholar] [CrossRef]
- Nasiri, K.; Wrbas, K.T. Accuracy of different generations of apex locators in determining working length; a systematic review and meta-analysis. Saudi Dent. J. 2022, 34, 11–20. [Google Scholar] [CrossRef]
- Meredith, N.; Gulabivala, K. Electrical impedance measurements of root canal length. Endod. Dent. Traumatol. 1997, 13, 126–131. [Google Scholar] [CrossRef]
- Jenkins, J.A.; Walker, W.A., 3rd; Schindler, W.G.; Flores, C.M. An in vitro evaluation of the accuracy of the root ZX in the presence of various irrigants. J. Endod. 2001, 27, 209–211. [Google Scholar] [CrossRef]
- Krizaj, D.; Jan, J.; Valencic, V. Modeling AC current conduction through a human tooth. Bioelectromagnetics 2004, 25, 185–195. [Google Scholar] [CrossRef] [PubMed]
- Venturi, M.; Breschi, L. A comparison between two electronic apex locators: An ex vivo investigation. Int. Endod. J. 2007, 40, 362–373. [Google Scholar] [CrossRef]
- Ozsezer, E.; Inan, U.; Aydin, U. In vivo evaluation of ProPex electronic apex locator. J. Endod. 2007, 33, 974–977. [Google Scholar] [CrossRef] [PubMed]
- Gomes, S.; Oliver, R.; Macouzet, C.; Mercadé, M.; Roig, M.; Duran-Sindreu, F. In vivo evaluation of the Raypex 5 by using different irrigants. J. Endod. 2012, 38, 1075–1077. [Google Scholar] [CrossRef]
- Altenburger, M.J.; Tchorz, J.P.; Somma, F. In vivo accuracy of three electronic root canal length measurement devices: Dentaport ZX, Raypex 5 and ProPex II. Int. Endod. J. 2012, 45, 1053–1054. [Google Scholar] [CrossRef] [PubMed]
- Duran-Sindreu, F.; Gomes, S.; Stöber, E.; Mercadé, M.; Jané, L.; Roig, M. In vivo evaluation of the iPex and Root ZX electronic apex locators using various irrigants. Int. Endod. J. 2013, 46, 769–774. [Google Scholar] [CrossRef]
- Kaufman, A.Y.; Keila, S.; Yoshpe, M. Accuracy of a new apex locator: An in vitro study. Int. Endod. J. 2002, 35, 186–192. [Google Scholar] [CrossRef]
- Meares, W.A.; Steiman, H.R. The influence of sodium hypochlorite irrigation on the accuracy of the Root ZX electronic apex locator. J. Endod. 2002, 28, 595–598. [Google Scholar] [CrossRef]
- Kang, J.A.; Kim, S.K. Accuracies of seven different apex locators under various conditions. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008, 106, e57–e62. [Google Scholar] [CrossRef]
- Jain, S.; Kapur, R. Comparative evaluation of accuracy of two electronic apex locators in the presence of various irrigants: An in vitro study. Contemp. Clin. Dent. 2012, 3 (Suppl. 2), S140–S145. [Google Scholar] [CrossRef]
- Baruah, Q.; Sinha, N.; Singh, B.; Reddy, P.N.; Baruah, K.; Augustine, V. Comparative Evaluation of Accuracy of Two Electronic Apex Locators in the Presence of Contemporary Irrigants: An In vitro Study. J. Int. Soc. Prev. Community Dent. 2018, 8, 349–353. [Google Scholar] [PubMed]
- Altunbaş, D.; Kuştarcı, A.; Toyoğlu, M. The Influence of Various Irrigants on the Accuracy of 2 Electronic Apex Locators in Locating Simulated Root Perforations. J. Endod. 2017, 43, 439–442. [Google Scholar] [CrossRef]
- Yahya, E.M.; Alchalabi, A.S.; Alkhalidi, E.F. Effect of Different Electroconductive Root Canal Irrigations on the Accuracy of Different Apex Locators: An In Vitro Comparative Study. J. Int. Soc. Prev. Community Dent. 2024, 14, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Karunakar, P.; Reddy, M.S.R.; Faizuddin, U.; Priya, P.S.; Karteek, B.S.; Saideep, C.V. Comparative evaluation of working length determined using integrated apex locator and root ZX mini under various irrigating solutions: An in vivo study. J. Conserv. Dent. Endod. 2023, 26, 590–594. [Google Scholar] [PubMed]
- Cîmpean, S.I.; Chisnoiu, R.M.; Colceriu Burtea, A.L.; Rotaru, R.; Bud, M.G.; Delean, A.G.; Pop-Ciutrilă, I.S. In Vitro Evaluation of the Accuracy of Three Electronic Apex Locators Using Different Sodium Hypochlorite Concentrations. Medicina 2023, 59, 918. [Google Scholar] [CrossRef]
- Chukka, R.R.; Bellam, M.D.; Marukala, N.R.; Dinapadu, S.; Konda, N.K.; Nagilla, J. Efficiency of an Integrated Apex Locator in Determining Working Length in Various Irrigating Solutions: An In Vivo Study. J. Pharm. Bioallied Sci. 2020, 12 (Suppl. 1), S410–S414. [Google Scholar] [CrossRef] [PubMed]
- Prasad, A.B.; Harshit, S.; Aastha, S.A.; Deepak, R. An In vitro Evaluation of the Accuracy of Two Electronic Apex Locators to Determine Working Length in the Presence of Various Irrigants. Ethiop. J. Health Sci. 2016, 26, 457–462. [Google Scholar] [CrossRef]
- Tinaz, A.C.; Maden, M.; Aydin, C.; Türköz, E. The accuracy of three different electronic root canal measuring devices: An in vitro evaluation. J. Oral. Sci. 2002, 44, 91–95. [Google Scholar] [CrossRef]
- Bernardes, R.A.; Duarte, M.A.; Vasconcelos, B.C.; Moraes, I.G.; Bernardineli, N.; Garcia, R.B.; Baldi, J.V.; Victorino, F.R.; Bramante, C.M. Evaluation of precision of length determination with 3 electronic apex locators: Root ZX, Elements Diagnostic Unit and Apex Locator, and RomiAPEX D-30. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 104, e91-4. [Google Scholar] [CrossRef]
- D’Assunção, F.L.; de Albuquerque, D.S.; de Queiroz Ferreira, L.C. The ability of two apex locators to locate the apical foramen: An in vitro study. J. Endod. 2006, 32, 560–562. [Google Scholar] [CrossRef]
- de Camargo, E.J.; Zapata, R.O.; Medeiros, P.L.; Bramante, C.M.; Bernardineli, N.; Garcia, R.B.; de Moraes, I.G.; Duarte, M.A. Influence of preflaring on the accuracy of length determination with four electronic apex locators. J. Endod. 2009, 35, 1300–1302. [Google Scholar] [CrossRef]
- Kim, E.; Lee, S.J. Electronic apex locator. Dent. Clin. N. Am. 2004, 48, 35–54. [Google Scholar] [CrossRef] [PubMed]
- Briseño-Marroquín, B.; Frajlich, S.; Goldberg, F.; Willershausen, B. Influence of instrument size on the accuracy of different apex locators: An in vitro study. J. Endod. 2008, 34, 698–702. [Google Scholar] [CrossRef] [PubMed]
- Marek, E.; Łagocka, R.; Kot, K.; Woźniak, K.; Lipski, M. The influence of two forms of chlorhexidine on the accuracy of contemporary electronic apex locators. BMC Oral Health 2019, 20, 3. [Google Scholar] [CrossRef]
- Herrera, M.; Ábalos, C.; Lucena, C.; Jiménez-Planas, A.; Llamas, R. Critical diameter of apical foramen and of file size using the Root ZX apex locator: An in vitro study. J. Endod. 2011, 37, 1306–1309. [Google Scholar] [CrossRef]
- Çelebi Keskin, İ.S.; Yalçın, T.Y. Evaluation of heated sodium hypochlorite’s effect on the accuracy of contemporary electronic apex locators: An in vitro study. BMC Oral Health 2025, 25, 634. [Google Scholar] [CrossRef] [PubMed]
- Golvankar, K.; Kader, M.A.; Latheef, A.A.; Ali, A.B.M.; Abullais, S.S.; Sibagathullah, M. Comparison of Accuracy in Determining the Root Canal Working Length by Using Two Generations of Apex Locators—An In Vitro Study. Open Access Maced. J. Med. Sci. 2019, 7, 3276–3280. [Google Scholar] [CrossRef]
- Rifaat, S.; Aljami, A.; Alshehri, T.; TAlameer, S.; Aldossary, A.; Almutairi, W.; NAlmaliki, M.; AFarooqi, F.; Taymour, N. The Effect of Coronal Pre-flaring and Type of Root Canal Irrigation on Working Length Accuracy Using Electronic Apex Locators. F1000Research 2023, 12, 533. [Google Scholar] [CrossRef]
- Gurel, M.A.; Helvacioglu Kivanc, B.; Ekici, A. A comparative assessment of the accuracies of Raypex 5, Raypex 6, iPex and iPex II electronic apex locators: An in vitro study. J. Istanb. Univ. Fac. Dent. 2017, 51, 28–33. [Google Scholar] [CrossRef]
- Nasiri, K.; Wrbas, K.T. Comparing the accuracy of two electronic apex locators in the determination of working length and the detection of root perforations: An in vitro study. Dent. Oral Craniofac. Res. 2019, 5, 1–5. [Google Scholar] [CrossRef]
- Tufenkci, P.; Kalaycı, A. Evaluation of the accuracy of different apex locators in determining the working length during root canal retreatment. J. Dent. Res. Dent. Clin. Dent. Prospects. 2020, 14, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Bilaiya, S.; Patni, P.M.; Jain, P.; Pandey, S.H.; Raghuwanshi, S.; Bagulkar, B. Comparative Evaluation of Accuracy of Ipex, Root Zx Mini, and Epex Pro Apex Locators in Teeth with Artificially Created Root Perforations in Presence of Various Intracanal Irrigants. Eur. Endod. J. 2020, 5, 6–9. [Google Scholar] [CrossRef] [PubMed]
- Shekarbaghani, S.A.; Bolhari, B.; Khalilak, Z. The effect of different root canal irrigations on the accuracy of apex locators: A systematic review. J. Clin. Exp. Dent. 2024, 16, e1538–e1546. [Google Scholar] [CrossRef] [PubMed]
- Mull, J.P.; Manjunath, V.; Manjunath, M. Comparison of accuracy of two electronic apex loca-tors in the presence of various irrigants: An in vitro study. J. Conserv. Dent. 2012, 15, 178–182. [Google Scholar] [CrossRef]
- Fan, W.; Fan, B.; Gutmann, J.L.; Bian, Z.; Fan, M.W. Evaluation of the accuracy of three electronic apex locators using glass tubules. Int. Endod. J. 2006, 39, 127–135. [Google Scholar] [CrossRef]

| Groups (mm) | Raypex 5 | ||||||
|---|---|---|---|---|---|---|---|
| 0.9% Saline | FileEZE EDTA 19% | Glyde EDTA 17% | Consepsis V 2% CHX | ChlorCid 3% | Citric Acid 20% | EDTA 18% | |
| <−1 (A) | 0 (0%) | 1 (2.5%) | 9 (22.5%) | 1 (2.5%) | 0 (0%) | 4 (10%) | 1 (2.5%) |
| −1.00 to −0.5 (B) | 2 (5%) | 10 (25%) | 1 (2.5%) | 4 (10%) | 0 (0%) | 9 (22.5%) | 10 (25%) |
| −0.5 to 0.0 (C) | 15 (37.5%) | 14 (35%) | 10 (25%) | 12 (30%) | 17 (42.5%) | 11 (27.5%) | 18 (45%) |
| >0.0 to 0.5 (D) | 20 (50%) | 11 (27.5%) | 12 (30%) | 18 (45%) | 16 (40%) | 11 (27.5%) | 7 (17.5%) |
| 0.5 to 1 (E) | 3 (7.5%) | 4 (10%) | 5 (12.5%) | 4 (10%) | 7 (17.5%) | 4 (10%) | 4 (10%) |
| >1 (F) | 0 (0%) | 0 (0%) | 3 (7.5%) | 1 (2.5%) | 0 (0%) | 1 (2.5%) | 0 (0%) |
| Total | 40 | 40 | 40 | 40 | 40 | 40 | 40 |
| Groups (mm) | Ipex | ||||||
|---|---|---|---|---|---|---|---|
| 0.9% Saline | FileEZE EDTA 19% | Glyde EDTA 17% | Consepsis V 2% CHX | ChlorCid 3% | Citric Acid 20% | EDTA 18% | |
| <−1 (A) | 0 (0%) | 0 (0%) | 0 (0%) | 2 (5%) | 0 (0%) | 3 (7.5%) | 2 (5%) |
| −1.00 to −0.5 (B) | 3 (7.5%) | 4 (10%) | 2 (5%) | 3 (7.5%) | 4 (10%) | 5 (12.5%) | 10 (25%) |
| −0.5 to 0.0 (C) | 18 (45%) | 5 (12.5%) | 10 (25%) | 11 (27.5%) | 19 (47.5%) | 17 (42.5%) | 15 (37.5%) |
| >0.0 to 0.5 (D) | 15 (37.5%) | 17 (42.5%) | 13 (32.5%) | 17 (42.5%) | 13 (32.5%) | 10 (25%) | 11 (27.5%) |
| 0.5 to 1 (E) | 4 (10%) | 12 (30%) | 12 (30%) | 6 (15%) | 4 (10%) | 5 (12.5%) | 1 (2.5%) |
| >1 (F) | 0 (0%) | 2 (5%) | 3 (7.5%) | 1 (2.5%) | 0 (0%) | 0 (0%) | 1 (2.5%) |
| Total | 40 | 40 | 40 | 40 | 40 | 40 | 40 |
| Mean Value | SD | N | |
|---|---|---|---|
| Raypex 0.9% saline 1 | 0.038 | 0.362 | 40 |
| Raypex File EZE EDTA 19% 2 | −0.165 | 0.503 | 40 |
| Raypex Glyde EDTA 17% | −0.083 | 0.837 | 40 |
| Raypex Consepsis V 2% CHX | 0.047 | 0.484 | 40 |
| Raypex ChlorCid 3% 2,3 | 0.087 | 0.381 | 40 |
| Raypex Citric Acid 20% | −0.183 | 0.649 | 40 |
| Raypex EDTA 18% 1,3 | −0.239 | 0.488 | 40 |
| Ipex 0.9% saline 4 | 0.017 | 0.351 | 40 |
| Ipex File EZE EDTA 19% 5,6 | 0.266 | 0.513 | 40 |
| Ipex Glyde EDTA 17% 7,8,9,10 | 0.299 | 0.549 | 40 |
| Ipex Consepsis V 2% CHX 4 | 0.048 | 0.519 | 40 |
| Ipex ChlorCid 3% 8 | −0.017 | 0.433 | 40 |
| Ipex Citric Acid 20% 5,9 | −0.141 | 0.533 | 40 |
| Ipex EDTA 18% 4,6,10 | −0.253 | 0.520 | 40 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Čabraja, L.K.; Dukić, W. In Vitro Accuracy of Two Different Electronic Apex Locators Under Various Conditions. Appl. Sci. 2025, 15, 6892. https://doi.org/10.3390/app15126892
Čabraja LK, Dukić W. In Vitro Accuracy of Two Different Electronic Apex Locators Under Various Conditions. Applied Sciences. 2025; 15(12):6892. https://doi.org/10.3390/app15126892
Chicago/Turabian StyleČabraja, Lucija Koturić, and Walter Dukić. 2025. "In Vitro Accuracy of Two Different Electronic Apex Locators Under Various Conditions" Applied Sciences 15, no. 12: 6892. https://doi.org/10.3390/app15126892
APA StyleČabraja, L. K., & Dukić, W. (2025). In Vitro Accuracy of Two Different Electronic Apex Locators Under Various Conditions. Applied Sciences, 15(12), 6892. https://doi.org/10.3390/app15126892






