1. Introduction
Augmented Reality (AR) is an innovative technology that overlays computer-generated 2D and 3D objects onto a real-world camera view, creating an immersive and interactive experience [
1]. In rehabilitation, AR has gained significant attention due to its unique ability to provide immediate, real-time feedback and foster engaging training environments [
2,
3]. This real-time interactive nature of AR facilitates precise movements by enabling users to concurrently adjust their actions while following virtual model demonstrations. Consequently, AR proves highly effective for rehabilitation training by seamlessly integrating motivating and engaging content, which is crucial for patient adherence and progress [
2]. Notably, AR has consistently demonstrated significant utility for patients requiring rehabilitation by effectively incorporating key therapeutic elements such as repetitive practice, immediate feedback, and enhanced motivation [
1].
Individuals who have undergone leg amputation due to accident or illness typically ambulate using a prosthesis. Rehabilitation training is multifaceted, encompassing foundational exercises like strengthening residual limb muscles and improving balance, progressing to complex tasks such as weight shifting, standing up, and navigating stairs and ramps [
4,
5]. A fundamental and critical element in prosthetic training is achieving effective weight-bearing on the prosthetic side. However, post-amputation, patients frequently experience pain, edema, and skin issues in the residual limb [
6], creating significant barriers to early weight-bearing, which is otherwise crucial for symptom alleviation and quicker prosthetic adaptation [
7]. Rehabilitation commonly begins with static standing exercises aimed at even weight distribution, gradually advancing to more dynamic tasks like inducing weight-bearing on the amputated side via healthy leg movements, or standing on the amputated leg while the healthy leg is elevated on a step box [
5]. While physical therapists primarily guide these exercises with verbal instructions, the inherent asymmetry between the two legs often leads to considerable balance challenges for patients. Relying solely on verbal cues can thus limit the achievement of accurate movements and sufficient weight-bearing, particularly during the initial stages of prosthetic use where finer motor control and psychological adjustment are paramount [
7].
Recognizing these limitations, researchers have explored advanced technologies to augment traditional rehabilitation approaches. Previous studies show that diverse forms of feedback, including mirrors, verbal cues, and augmented sensory feedback, effectively aid weight-bearing and balance training for individuals with lower limb amputations [
7,
8,
9]. Authors of one study specifically suggested that visual feedback is particularly beneficial for controlling sway in amputees, advocating for its inclusion in rehabilitation plans [
7]. Furthermore, studies have reported that visual feedback improves gait asymmetry [
8], and biofeedback training incorporating visual feedback assists in retraining equal weight-bearing [
9].
The provision of diverse feedback is essential for optimizing correct movement execution during rehabilitation [
10]. Specifically, visual feedback stimulates proprioception, offering neurological benefits, and the visual confirmation of achieving target movement trajectories has been shown to result in more accurate exercise performance and enhanced motor learning [
3]. Building on these insights, AR technology emerges as a compelling solution, offering real-time visual guidance that could directly address the balance and accuracy challenges faced by lower limb amputees, thereby fostering greater engagement and more effective rehabilitation outcomes.
Existing research shows promising results for AR-based rehabilitation training across various patient populations. Numerous studies on stroke patients indicate AR’s effectiveness in enhancing upper and lower limb functional recovery [
11]. Specifically, regarding lower limb functional recovery, AR training has been shown to improve balance and gait in stroke patients [
11,
12,
13], and even home-based AR exercises have positively impacted balance ability after stroke [
14].
Similarly, in studies involving older adults, AR-based Otago exercises demonstrated improvements in balance, gait ability, and fall self-efficacy [
15]. Training utilizing 3D AR systems has been shown to enhance stability, reduce the risk of falls, and improve balance [
16], while AR-based physical exercises effectively increased walking speed and balance ability [
17].
Research on the therapeutic applications of AR for amputee patients includes case studies demonstrating its effectiveness in reducing phantom limb pain in upper limb amputees [
18]. However, studies concerning lower limb amputees have primarily focused on the interventional effects of Virtual Reality (VR) training, which offers a higher level of immersion compared to AR. These VR studies have reported significant improvements in balance metrics (e.g., Berg Balance Scale, Timed Up and Go test, Dynamic Gait Index) when compared to traditional training methods [
19].
Specifically, a case study on transtibial amputees indicated that VR-based gait training providing real-time feedback effectively improved hip, pelvis, and trunk movements, reduced oxygen consumption, and enhanced overall gait performance [
20]. Furthermore, rehabilitation interventions combining VR training with traditional methods have been shown to positively impact pain reduction, depression, and mental health status in lower limb amputees [
21]. Immersive VR game training has also been found to contribute to improved proprioception, balance, and agility in transfemoral amputees [
22].
Nevertheless, there is a current lack of research directly investigating the impact of AR systems on lower limb amputees, particularly concerning movement accuracy and subjective satisfaction.
Based on the positive results of AR-based rehabilitation training observed in studies involving stroke patients and older adults, particularly AR’s potential for lower limb functional recovery and balance improvement, we hypothesize that applying AR-based visual feedback to rehabilitation training for lower limb amputees will enhance movement accuracy and consequently improve exercise efficacy compared to training without such feedback.
Therefore, this study aims to differentiate itself from existing VR research by comparing and analyzing differences in movement accuracy and subjective satisfaction based on the application of an AR system in unilateral lower limb amputees. The goal of this study is to empirically verify the immediate effects of using AR systems in lower limb amputee rehabilitation, and to provide essential foundational data for the future development and clinical application of customized AR-based rehabilitation training programs.
This paper begins with an introduction that outlines the potential of AR technology in rehabilitation and the current limitations in lower limb amputee rehabilitation, thereby establishing the necessity and objective of the study. The research methodology section then elaborates on the study participants, system, equipment, and procedures. Following this, the results section presents the analysis of movement accuracy and subjective satisfaction based on the application of the AR system. These findings are thoroughly interpreted in the discussion, and finally, the conclusion summarizes the key discoveries and future prospects.
2. State of the Art
Over the past two decades, research has consistently demonstrated the robust potential of Augmented Reality (AR), Virtual Reality (VR), and Mixed Reality (MR) technologies in medical rehabilitation, particularly within exercise-based interventions. These technologies are rapidly advancing, complementing the limitations of traditional rehabilitation approaches and opening new possibilities by offering real-time feedback, immersive training environments, and enhanced patient motivation. AR/VR rehabilitation is being utilized across diverse clinical scenarios, including phantom limb pain management, post-stroke functional recovery, hand rehabilitation, and geriatric rehabilitation, with a specific focus on improving movement accuracy and increasing patient engagement. Numerous studies analyze the effectiveness of AR/VR/MR systems, exploring approaches to increase autonomy and improve adherence in the absence of a therapist.
AR/MR rehabilitation is actively being researched and tailored to various patient populations and rehabilitation objectives. AR has shown promising effects in alleviating phantom limb pain (PLP) and reversing cortical reorganization by providing visual representations of intact limbs to patients with distorted phantom limbs [
23]. For lower limb amputees, existing research has primarily focused on highly immersive VR training, reporting positive effects on balance, gait, and reduction in phantom limb phenomena (PLT) [
24,
25,
26]. Notably, MR systems, when combined with sEMG analysis, can contribute to monitoring muscle activity and enhancing muscle activation and training effectiveness through real-time synchronization with virtual prostheses [
27].
AR technology has been proven effective in enhancing upper and lower limb functional recovery in stroke patients [
11]. Low-cost solutions, such as phone-based AR systems (CARS), have shown significant effects on improving upper limb exercise and cognitive function, thereby expanding the potential for home-based rehabilitation [
28]. Research actively integrates VR/AR and gamification into robot-assisted therapy to boost patient motivation and improve motor function [
29]. Furthermore, AR and MR therapies have outperformed conventional treatments in terms of upper limb disability and activities of daily living (ADL) functional outcomes in stroke upper limb rehabilitation [
30].
AR/VR interventions have also proven effective in hand rehabilitation, an area frequently affected by work-related hand injuries. Real-time feedback, challenging tasks, and individualized difficulty progression act as motivating factors that enhance patient adherence [
31]. Rotator cuff rehabilitation games utilizing VR and motion tracking technology have also been developed and received positive preliminary evaluations [
32].
A three-dimensional interactive AR system (3D-ARS) for balance and mobility rehabilitation in the elderly has demonstrated clinical efficacy, showing significant improvements in balance and mobility scales [
16]. AR-based training systems can also be utilized for cognitive rehabilitation in the elderly, improving abilities such as spatial visualization and mental rotation [
33].
Despite the demonstrated positive effects of AR/MR technologies across various rehabilitation domains, several critical research gaps persist. Firstly, there is still a paucity of research directly investigating the effects of AR systems on lower limb amputees, particularly studies focusing on movement accuracy and subjective satisfaction. Existing amputee rehabilitation research primarily concentrates on highly immersive VR interventions, and the specific effects of precise movement guidance and feedback offered by AR’s real-world overlay characteristics have not been sufficiently explored. Secondly, there is an overall lack of high-quality randomized controlled trials (RCTs), and heterogeneity and risk of bias among studies make it challenging to conclusively determine whether AR/VR interventions are definitively superior to traditional rehabilitation [
24,
34]. Lastly, while exercise interventions improve gait speed and distance, consistent evidence regarding balance outcomes remains insufficient, necessitating further investigation [
35].
This research gap, specifically the lack of direct empirical evidence regarding the effects of AR system application on movement accuracy and subjective satisfaction in lower limb amputee rehabilitation, constitutes the core problem statement of this study.
This study aims to address the aforementioned research gaps by specifically focusing on comparing and analyzing the effects of AR system application on lower limb amputee rehabilitation training in terms of movement accuracy and subjective satisfaction. By distinguishing itself from existing VR research, this study seeks to empirically verify how AR-based visual feedback enhances the accuracy of rehabilitation exercises in lower limb amputees and how it influences their perceived satisfaction during the process.
The main contributions of this study are as follows: Firstly, it provides foundational data by clearly verifying the effectiveness of AR-based visual feedback for lower limb amputee rehabilitation, demonstrating that AR systems can significantly improve patients’ movement accuracy. Secondly, it highlights the importance of patient-centered rehabilitation by showing that AR systems can enhance patients’ satisfaction with the training process, thereby contributing to improved treatment adherence and persistence. Ultimately, the results of this study are expected to serve as essential foundational data for the future development and clinical implementation of personalized AR-based rehabilitation training programs for lower limb amputees, thereby contributing to an improved quality of life for patients through more effective and engaging rehabilitation solutions.
3. Methods
3.1. Participants
Ten individuals with unilateral lower limb amputations participated in this study. The group consisted of 9 transfemoral and 1 transtibial amputee. Participants for this study were selected based on the following criteria: they had a unilateral or bilateral lower limb amputation, were at least two years post-initial amputation, possessed the ability to perform daily activities and ambulate with a prosthesis, and exhibited no cognitive impairment that would hinder their understanding of the experimental procedures.
Participants were excluded if they presented with incomplete weight-bearing on the prosthetic side due to phantom limb pain, residual limb pain, or joint contracture, had a limited range of motion in the joints of their intact limb, experienced difficulty bearing full weight on their intact limb, or had physical injuries to upper limb joints (beyond the lower limb amputation) that would impede their ability to perform the exercises. All participants were traumatic amputees resulting from industrial accidents. The participants had a mean age of 61.1 ± 5.8 years, a mean height of 172.0 ± 4.4 cm, a mean weight of 76.5 ± 12.2 kg, and a mean prosthetic use duration of 8.6 ± 3.7 years. This study received approval from the Institutional Review Board of the Rehabilitation Engineering Research Institute (RERI-IRB-240831-1). Prior to participation, all subjects provided voluntary written informed consent after receiving a thorough explanation of the study’s objectives and procedures.
3.2. Instruments
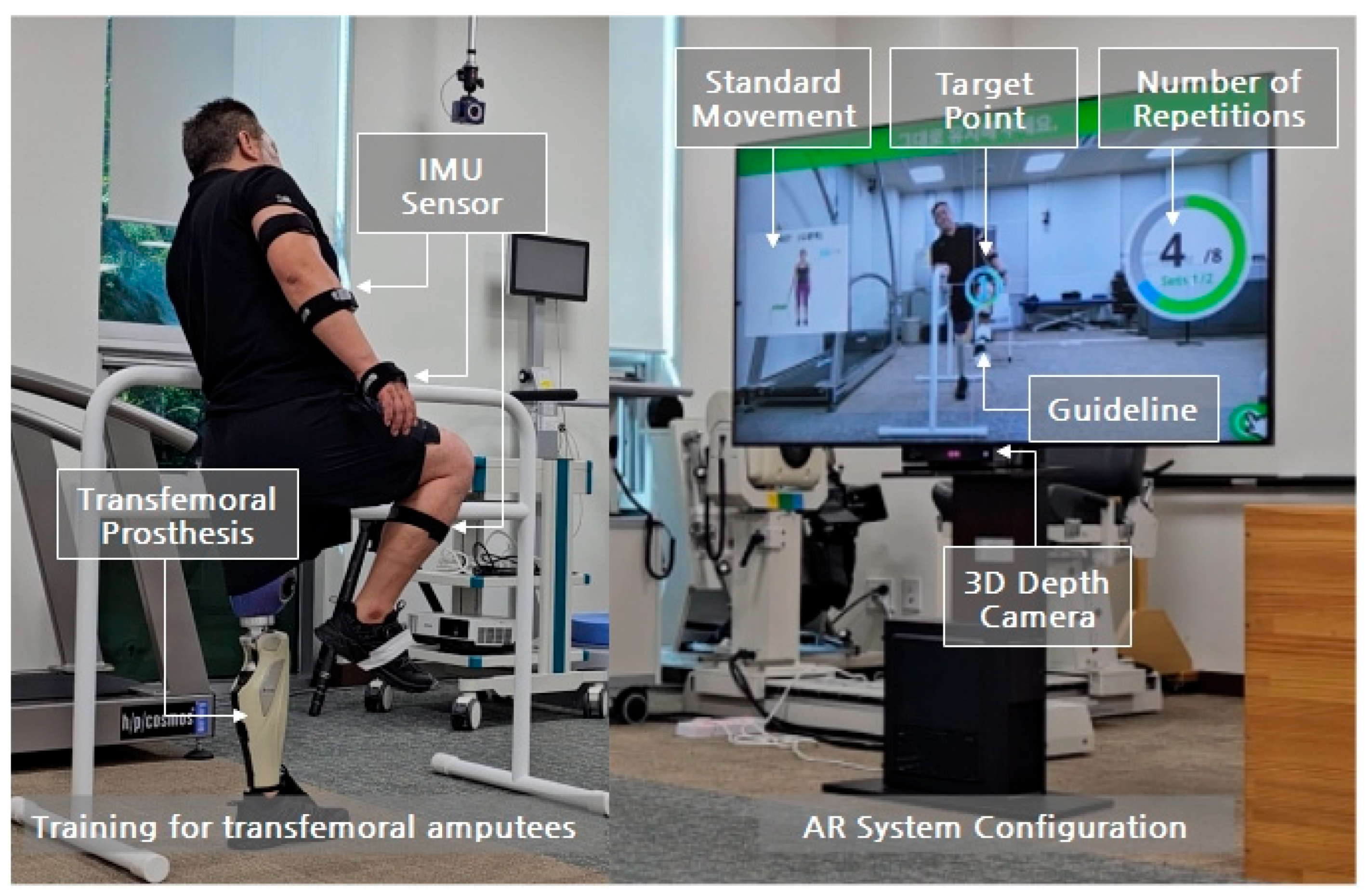
For the Augmented Reality application in this study, a commercially available AR system (UINCARE, Uincare Co., Ltd., Seoul, Republic of Korea) was utilized. This system comprises a 3D depth camera, a 64-inch monitor, operating software, and approximately 300 types of body exercise content [
9].
Upon system initiation, the participant stands motionless at a distance of 1.5 m in front of the 3D depth camera. The camera identifies the participant’s joints and generates overlaid joint segments on the participant’s image displayed on the screen. When pre-set exercise content is activated, a model demonstration for the participant to emulate appears on the left side of the monitor, while the target and completed repetition counts are shown on the right (
Figure 1). The user performs the exercise by following the on-screen model. The target range of motion and guiding lines to achieve it are displayed.
The participant moves their body along the guidelines towards the target. Accurate target achievement triggers a success sound, and the repetition count increases. This process is repeated continuously [
9].
In this study, a sensor-based 3D motion capture system (Ultium Motion Sensor, Noraxon, Scottsdale, AZ, USA) was employed to measure the accuracy of exercise movements both with and without the AR system. This system utilizes an array of multiple inertial measurement units (IMUs) to measure and analyze anatomical joint angles, orientation, and linear acceleration during specific tasks performed in daily activities or natural environments. The system comprises 9 inertial sensors, a data receiver, an experimental laptop, and analysis software.
The placement of the nine sensors was as follows: upper thoracic spine (midline below C7), lower thoracic spine (midline between L1 and T12), pelvis (sacral region), intact upper arm (midpoint between shoulder and elbow joints, lateral to the bone axis), forearm (posterior and distal), hand (dorsum), intact thigh (anterior and distal half), calf (anterior and slightly medial, along the tibia), and foot (dorsum, slightly below the ankle). The sensors for the upper thoracic, lower thoracic, and pelvis regions were placed directly on the bare skin beneath the participants’ clothes.
To analyze the users’ subjective satisfaction based on the presence or absence of the AR system, a five-item questionnaire was administered, assessing interest, motivation, exercise effectiveness, accuracy of movement, and overall satisfaction. Each item was rated on a 5-point Likert scale, yielding a total possible satisfaction score of 25 points.
3.3. Selection of Exercise Tasks
In this study, six training protocols tailored for individuals with lower limb amputations were developed from approximately 300 body movements available within the UINCARE system. These protocols encompassed pre-prosthetic training, post-prosthetic training, basic left–right stepping training, center of mass transfer training, balance training, and flexibility training.
For the purpose of this experiment, eight specific test movements were selected from the post-prosthetic training protocol. These movements were categorized by their balance demand into three difficulty levels: high (4 movements), medium (2 movements), and low (2 movements). The details of the selected exercise movements and their difficulty criteria are presented in
Table 1.
For each exercise movement, the range of motion of the primary involved joint was measured. Specifically, the shoulder abduction angle was measured for the standing arm raise to the side, the shoulder flexion angle for the standing arm raise overhead, the trunk lateral flexion angle for the standing trunk lateral flexion, the trunk rotation angle for the standing diagonal medicine ball lift, the knee flexion angle for the standing dumbbell forward lunge, the hip abduction angle for the standing leg raise to the side, the hip flexion angle for the standing knee flexion to maximum height, and the knee flexion angle for the standing step out to the side with arm extension.
3.4. Experimental Procedure
Prior to the experiment, participants were fitted with comfortable attire (short-sleeved shirts, shorts, and athletic shoes). A physical therapist provided thorough instruction on the eight exercise movements to ensure accurate comprehension. Following familiarization with the exercises, participants rested for 10 min. After sensor attachment, a calibration procedure was performed to ensure accurate data acquisition, and the experiment commenced upon verification of normal sensor operation.
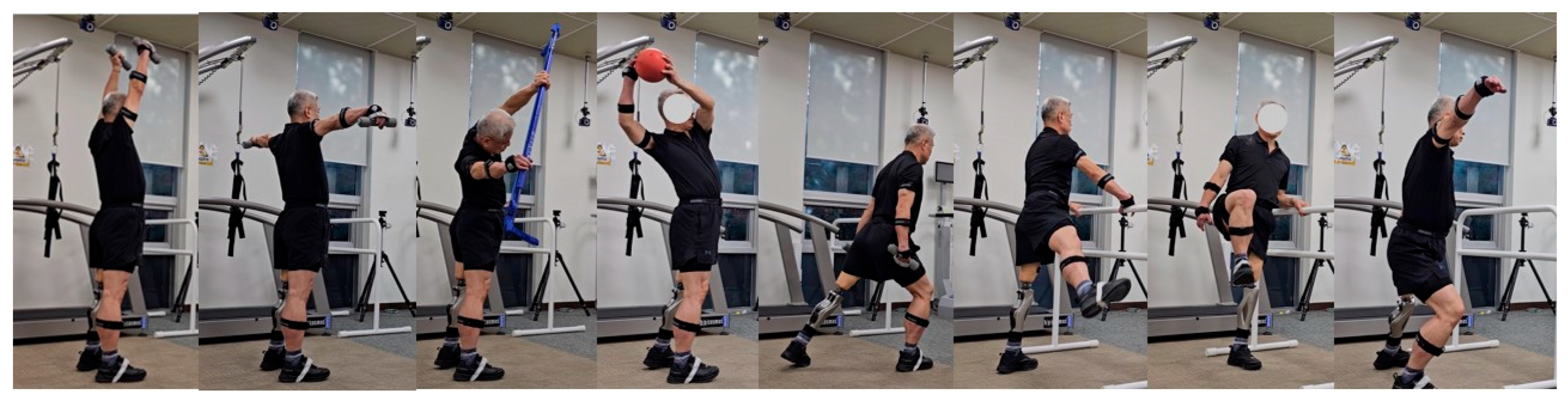
The experiment involved two conditions: with the AR system and without the AR system. In both conditions, participants performed the same sequence of eight exercise movements, presented in ascending order of difficulty (
Figure 2): (1) standing arm raise to the side, (2) standing arm raise overhead, (3) standing trunk lateral flexion, (4) standing diagonal medicine ball lift, (5) standing dumbbell forward lunge, (6) standing leg raise to the side, (7) standing knee flexion to maximum height, and (8) standing step out to the side with arm extension.
Each exercise movement followed a consistent timing protocol: 3 s of performance, a 3 s hold, and a 3 s rest, with each movement repeated eight times. Each experimental condition lasted approximately 20 min, with a 20 min rest interval between the two conditions. To mitigate potential order effects, the sequence of the AR and non-AR conditions was randomized across participants.
In the condition without the AR system, the performance, hold, and rest phases of each exercise were guided by verbal commands from the physical therapist. Upon completion of both experimental conditions, participants completed the subjective satisfaction questionnaire.
3.5. Statistical Analysis
For each exercise movement, the primary joint angle, as specified in
Table 1, was analyzed. The mean and standard deviation of these joint angles were calculated. To evaluate movement accuracy, the standard deviation of the mean joint angle across the eight repetitions of each movement was specifically examined. For each movement, the average joint angle across the eight repetitions was used in the analysis. Similarly, for the subjective satisfaction questionnaire, the mean and standard deviation were calculated for each of the five items (interest, motivation, exercise effectiveness, movement accuracy, and overall satisfaction), as well as for the total satisfaction score.
To determine the statistical differences between the AR and non-AR conditions, the normality of the data was first assessed using the Kolmogorov–Smirnov test. Following this, paired t-tests were employed to compare the conditions. The level of statistical significance was set at p < 0.05. To compensate for potential limitations in statistical power due to the small sample size, % difference confidence intervals (%difference CIs) and Cohen’s d values were also analyzed alongside the primary inferential statistics. The % difference CI provides an estimated range for the relative difference between the two conditions, indicating both the magnitude and direction of the effect as a percentage. Cohen’s d, a measure of effect size, quantifies the standardized mean difference between the two conditions. It expresses the difference in means in terms of standard deviation units, allowing for a more objective comparison of effect magnitudes independent of sample size. Common interpretations included ≈ 0.2 for a small effect, d ≈ 0.5 for a medium effect, and d ≈ 0.8 for a large effect. A substantial Cohen’s d value, even with a non-significant p-value, can indicate a meaningful effect that warrants further investigation.
5. Discussion
This study explored the potential of AR technology for rehabilitation training in individuals with lower limb amputations by comparing the accuracy and subjective satisfaction of exercise movements with and without AR system application. Our findings indicate that while AR feedback did not substantially increase the range of motion in all tested movements, it proved effective in significantly reducing the variability (standard deviation) across repetitions for most exercises. This enhanced consistency in performance implies that AR-based visual feedback can guide individuals to execute target movements with greater precision and stability, which is particularly relevant for the challenges with balance often encountered by lower limb amputees, especially in the early stages of prosthetic use. Therefore, the improved movement consistency facilitated by AR feedback holds promise for positively influencing the overall effectiveness of rehabilitation exercises.
Further examination based on movement difficulty revealed interesting patterns. In the low-difficulty movements, we observed a statistically significant increase in the average shoulder abduction angle during ‘standing arm abduction’ when AR feedback was provided (p = 0.04). Conversely, ‘standing arm raise overhead’, another low-difficulty movement, did not show a significant difference with AR feedback. We interpret this by suggesting that the ‘standing arm raise overhead’ movement might inherently push individuals towards their maximum range of motion, thereby limiting the additional benefit of visual feedback. In contrast, for ‘standing arm abduction’, the AR feedback likely provided salient visual cues regarding the target angle, effectively guiding participants to achieve a wider range of motion.
Extending our analysis to the medium-difficulty movements, we observed a similar pattern. The ‘standing trunk lateral flexion’ exercise showed a statistically significant increase in the average trunk lateral flexion angle with the application of AR feedback (p = 0.02). This aligns with the findings from the low-difficulty ‘standing arm abduction’, suggesting that the visual cues provided by AR feedback effectively facilitated a greater range of motion in lateral trunk bending. Conversely, the ‘standing diagonal raise with a medicine ball’ did not exhibit a significant difference, likely due to the inherent limitations in the range and radius of trunk rotation involved in this movement, thus limiting the potential impact of AR feedback on this specific aspect of motion.
The high-difficulty movements presented a unique set of demands, requiring both stable weight-bearing on the prosthetic limb and precise control of the sound limb. Notably, within this category, the ‘standing knee flexion to maximum height’ movement demonstrated a significant increase in hip flexion angle with AR feedback (p = 0.03). This finding echoes the results from the low- and medium-difficulty movements where AR feedback enhanced the range of motion, indicating its potential effectiveness in guiding a larger hip flexion range in this challenging exercise as well. In contrast, the ‘standing forward lunge with dumbbells’ and ‘stepping sideways and extending arms laterally’ did not show discernible differences in the range of motion with or without AR feedback. For the ‘standing single-leg lateral raise’, while a slight increase in the average value was noted, the inherent difficulty of lifting the sound leg laterally while weight-bearing on the prosthesis might explain why a more substantial change was not observed, possibly because participants were already operating near their maximal achievable range.
In summary, while AR feedback did not consistently increase the joint range of motion across all exercises, statistically significant increases were noted specifically in standing arm abduction, standing trunk lateral flexion, and standing knee flexion to maximum height. This suggests that the effect of AR feedback on range of motion is likely contingent upon the nature of the exercise and the demands of the movement. For example, AR feedback may be particularly beneficial in guiding a greater range of motion in exercises with simpler, more defined paths. Conversely, its impact might be less pronounced in more complex movements or those where individuals already exhibit a full range of motion. Consequently, the implementation of AR feedback in rehabilitation training may necessitate the development of tailored feedback approaches that take into account the specific exercise and the intended joint movements.
Beyond the effects on movement accuracy and range of motion, a particularly compelling finding of this study is the statistically significant higher subjective satisfaction reported by lower limb amputees who utilized AR feedback. This encompassed aspects such as the enjoyment of training, motivation levels, perceived exercise effectiveness, and perceived accuracy of movement. This suggests that AR technology’s benefits extend beyond mere kinematic improvements, potentially fostering a more positive training experience that could encourage greater patient engagement and adherence to rehabilitation protocols. The immersive qualities and real-time feedback inherent in AR may clarify a patient’s understanding of their performance during what can often be repetitive rehabilitation exercises, thereby promoting more active participation and potentially maximizing the therapeutic benefits [
2,
3]. This observed enhancement in subjective satisfaction aligns with findings from a study on a low-cost, mobile-phone-based AR system (CARS) for stroke patients, which showed significant effects on improving upper limb motor and cognitive functions, thus expanding the potential for home-based rehabilitation. It also resonates with research integrating VR/AR and gamification into robot-assisted therapy, contributing to increased patient motivation [
28,
29].
These findings resonate with the positive outcomes observed in prior AR rehabilitation studies targeting stroke patients and the elderly, which have reported improvements in lower limb function and balance [
11,
12,
13,
14,
15,
16,
17]. Specifically, in the context of prosthetic training for lower limb amputees, where weight-bearing exercises are critical, AR-based real-time visual feedback has the potential to facilitate a patient’s intuitive understanding and control of their weight distribution and balance [
7,
9]. Furthermore, our results, when considered alongside the enhanced balance and gait performance reported in VR-based rehabilitation studies for this population [
19,
20], indicate that AR technology represents another promising tool for the rehabilitation of lower limb amputees. Notably, the enhanced real-world interaction offered by AR, in contrast to VR, may provide a more natural and safer training environment for patients. Furthermore, AR holds great potential in alleviating phantom limb pain (PLP) and reversing cortical reorganization by providing patients with distorted phantom limbs a visual representation of an intact limb [
23]. The expandability of AR/MR technology is also demonstrated by the fact that MR systems, when combined with sEMG analysis, can contribute to increased muscle activation and training efficacy through real-time synchronization with virtual prosthetics [
27].
The significance of this study lies in its empirical validation of the positive potential of AR system application in the rehabilitation training of individuals with lower limb amputations. The observed improvements in movement consistency coupled with high levels of subjective satisfaction provide valuable foundational data for the future development of tailored AR-based rehabilitation programs for this population. For instance, an AR environment could offer varied difficulty levels of training content customized to an individual’s abilities and goals, coupled with real-time visual feedback on movement accuracy and balance, thereby potentially maximizing training effectiveness and fostering greater patient engagement.
Limitations
This study, while contributing to the understanding of AR-based rehabilitation for lower limb amputees, has several limitations that warrant consideration for future research.
A significant limitation is the relatively small sample size, which restricts the generalizability of our findings. Within this small cohort, there was also a disproportionate representation of amputation levels, primarily consisting of transfemoral amputees (n = 9) with only one transtibial amputee. While we aimed to explore AR training applicability across lower limb amputations, this asymmetry makes it challenging to definitively conclude if observed AR training effects are equally efficacious across different amputation levels. Future research should aim for a larger, more diverse, and balanced cohort of lower limb amputees, with sufficient representation for each amputation level, to allow for robust comparisons and enhance the generalizability of findings. Additionally, developing and testing amputation-specific AR training protocols would be beneficial to address unique anatomical and biomechanical considerations.
This study primarily investigated the short-term effects of AR training, as long-term follow-up was not conducted. Consequently, we cannot definitively determine the impact of AR training on long-term functional recovery, sustained adherence to training, or changes in quality of life. Future research should incorporate extended follow-up periods to assess the sustained benefits and long-term efficacy of AR-based interventions. Furthermore, a notable limitation is the lack of blinding, as both participants and assessors were aware of the experimental conditions. This open-label design introduces the potential for expectancy effects or subjective bias to influence the reported outcomes. Future research would benefit from implementing blinding strategies, such as using a sham control or a blinded assessor, to minimize these potential confounds and enhance the objectivity of the findings.
This study exclusively focused on specific movements, and therefore, it did not address the full spectrum of movements necessary for the comprehensive rehabilitation of lower limb amputees. Future research should consider incorporating a broader range of functional movements and activities to provide a more holistic understanding of AR training’s impact on overall rehabilitation. Additionally, this study relied on a 5-point Likert scale to assess subjective satisfaction. While useful for a general overview, this approach is somewhat simplistic and does not allow for an in-depth exploration of patients’ experiences with various training modules. Future research could benefit from employing more comprehensive qualitative methods, such as semi-structured interviews or open-ended questionnaires, to gain richer insights into participants’ perceptions, challenges, and preferences regarding AR-based rehabilitation.
Given the current lack of definitive conclusions regarding the superiority of AR/VR interventions over traditional rehabilitation [
24,
34], there is a continuous need for high-quality randomized controlled trials (RCTs) like this study to further clarify the clinical utility of AR systems. Considering the limitations of existing research, which shows improvements in walking speed and distance but still lacks consistent evidence for balance outcomes [
35], future studies should focus more on verifying the long-term and consistent effects of AR on enhancing balance ability in lower limb amputees. Future work should also explore the development of diverse AR-based training content and interaction modalities, and evaluate their comprehensive impact on patients’ functional recovery and psychological well-being within real clinical settings.