A Comparative In Vitro Analysis of Attachment and Enhanced Structural Features for Molar Distalization in Clear Aligner Therapy
Abstract
1. Introduction
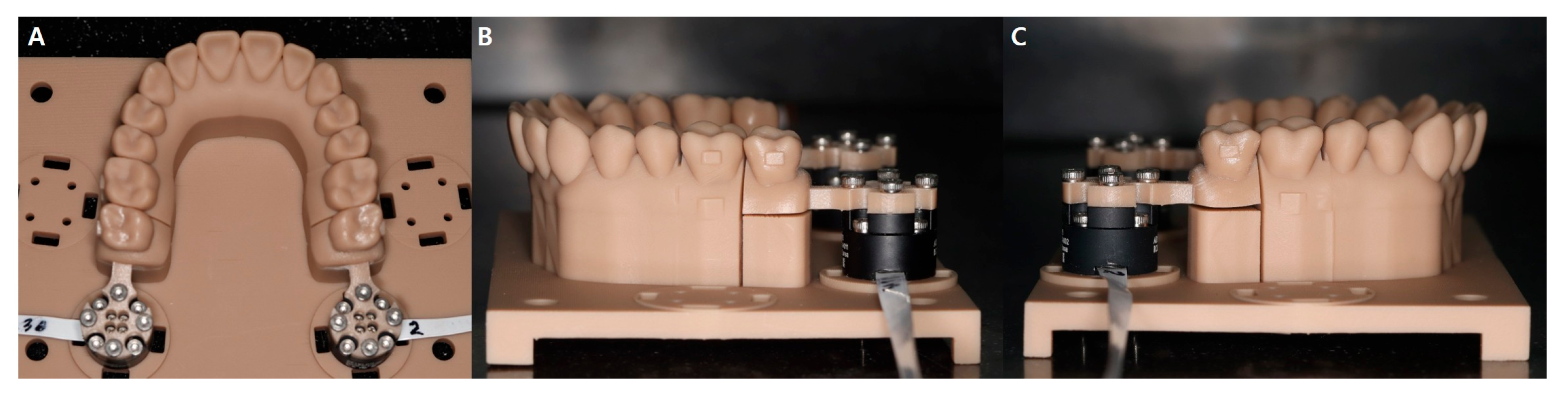
2. Materials and Methods
2.1. Design and Fabrication of a Force/Moment Measurement System
2.2. Design Modification and Fabrication of the Experimental CA for the Distal Bodily Movement of Maxillary Second Molars
- Group 1: #6 attachment and non-enhanced structure
- Group 2: #6 no attachment and non-enhanced structure
- Group 3: #6 attachment and enhanced structure (addition of a direct flowable resin)
- Group 4: #6 no attachment and enhanced structure (addition of a direct flowable resin)
2.3. Statistical Analysis
3. Results
3.1. Forces on Multi-Axes
3.2. Moments on Multi-Axes
3.3. Mx/Fy Ration
4. Discussion
5. Conclusions
- Distal, intrusive forces are generated during the posterior movement of the second molar.
- The incorporation of local enhancing structures increases the molar distal force, moment, and moment-to-force ratio, which increases the tendency of the second molar posterior bodily movement.
- The localized structural strengthening method proposed in this study is a practical approach that can be easily implemented for CA treatment in clinical practice, especially when bonding attachments are not feasible.
- However, the conclusions should be interpreted with caution, as this in vitro study does not fully simulate the dynamic intraoral environment, including adjacent tooth interactions and biological factors such as saliva and occlusal forces.
- Future clinical research is necessary to evaluate the long-term effectiveness, material durability, and patient comfort of this technique under realistic treatment conditions.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CA | Clear aligner |
References
- Weir, T. Clear aligners in orthodontic treatment. Aust. Dent. J. 2017, 62, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Kravitz, N.D.; Kusnoto, B.; BeGole, E.; Obrez, A.; Agran, B. How well does Invisalign work? A prospective clinical study evaluating the efficacy of tooth movement with Invisalign. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 27–35. [Google Scholar] [CrossRef]
- Lombardo, L.; Arreghini, A.; Ramina, F.; Ghislanzoni, L.T.; Siciliani, G. Predictability of orthodontic movement with orthodontic aligners: A retrospective study. Prog. Orthod. 2017, 18, 35. [Google Scholar] [CrossRef] [PubMed]
- Galan-Lopez, L.; Barcia-Gonzalez, J.; Plasencia, E. A systematic review of the accuracy and efficiency of dental movements with Invisalign®. Korean J. Orthod. 2019, 49, 140–149. [Google Scholar] [CrossRef]
- Jedliński, M.; Mazur, M.; Greco, M.; Belfus, J.; Grocholewicz, K.; Janiszewska-Olszowska, J. Attachments for the orthodontic aligner treatment-state of the art-a comprehensive systematic review. Int. J. Environ. Res. Public. Health. 2023, 20, 4481. [Google Scholar] [CrossRef]
- Tepedino, M.; Paoloni, V.; Cozza, P.; Chimenti, C. Movement of anterior teeth using clear aligners: A three-dimensional, retrospective evaluation. Prog. Orthod. 2018, 19, 9. [Google Scholar] [CrossRef]
- Bechtold, T.E.; Park, Y.C.; Kim, K.H.; Jung, H.K.; Kang, J.Y.; Choi, Y.J. Long-term stability of miniscrew anchored maxillary molar distalization in Class II treatment. Angle Orthod. 2020, 90, 362–368. [Google Scholar] [CrossRef]
- D′Antò, V.; Valletta, R.; Ferretti, R.; Bucci, R.; Kirlis, R.; Rongo, R. Predictability of maxillary molar distalization and derotation with clear aligners: A prospective study. Int. J. Environ. Res. Public Health 2023, 20, 2941. [Google Scholar] [CrossRef] [PubMed]
- Ravera, S.; Castroflorio, T.; Garino, F.; Daher, S.; Cugliari, G.; Deregibus, A. Maxillary molar distalization with aligners in adult patients: A multicenter retrospective study. Prog. Orthod. 2016, 17, 12. [Google Scholar] [CrossRef]
- Caruso, S.; Nota, A.; Ehsani, S.; Maddalone, E.; Ojima, K.; Tecco, S. Impact of molar teeth distalization with clear aligners on occlusal vertical dimension: A retrospective study. BMC Oral Health 2019, 19, 182. [Google Scholar] [CrossRef]
- Miao, Z.; Zhang, H.; Yang, Y.; Han, Y.; Leng, J.; Wang, S. Influence of maxillary molar distalization with clear aligners on three-dimensional direction: Molar distal movement, intrusion, distal tip and crown buccal torque. Prog. Orthod. 2023, 24, 48. [Google Scholar] [CrossRef] [PubMed]
- Baldwin, D.K.; King, G.; Ramsay, D.S.; Huang, G.; Bollen, A.M. Activation time and material stiffness of sequential removable orthodontic appliances. Part 3: Premolar extraction patients. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 837–845. [Google Scholar] [CrossRef]
- Bichu, Y.M.; Alwaf, A.; Liu, X.; Andrews, J.; Ludwig, B.; Bichu, A.Y.; Zou, B. Advances in orthodontic clear aligner materials. Bioact. Mater. 2022, 22, 384–403. [Google Scholar] [CrossRef]
- Cui, J.Y.; Ting, L.; Cao, Y.X.; Sun, D.X.; Bing, L.; Wu, X.P. Morphology changes of maxillary molar distalization by clear aligner therapy. Int. J. Morphol. 2022, 40, 920–926. [Google Scholar] [CrossRef]
- Fang, D.; Li, F.; Zhang, Y.; Bai, Y.; Wu, B.M. Changes in mechanical properties, surface morphology, structure, and composition of Invisalign material in the oral environment. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 745–753. [Google Scholar] [CrossRef]
- Jin, X.; Tian, X.; Hui, V.L.Z.; Zheng, Y.; Song, J.; Han, X. The effect of enhanced structure in the posterior segment of clear aligners during anterior retraction: A three-dimensional finite element and experimental model analysis. Prog. Orthod. 2024, 25, 3. [Google Scholar] [CrossRef]
- Zhu, Y.; Hu, W.; Li, S. Force changes associated with differential activation of en-masse retraction and/or intrusion with clear aligners. Korean J. Orthod. 2021, 51, 32–42. [Google Scholar] [CrossRef] [PubMed]
- Grant, J.; Foley, P.; Bankhead, B.; Miranda, G.; Adel, S.M.; Kim, K.B. Forces and moments generated by 3D direct printed clear aligners of varying labial and lingual thicknesses during lingual movement of maxillary central incisor: An in vitro study. Prog. Orthod. 2023, 24, 23. [Google Scholar] [CrossRef] [PubMed]
- Simon, M.; Keilig, L.; Schwarze, J.; Jung, B.A.; Bourauel, C. Treatment outcome and efficacy of an aligner technique—regarding incisor torque, premolar derotation and molar distalization. BMC Oral Health 2014, 14, 68. [Google Scholar] [CrossRef]
- Li, L.; Guo, R.; Zhang, L.; Huang, Y.; Jia, Y.; Li, W. Maxillary molar distalization with a 2-week clear aligner protocol in patients with Class II malocclusion: A retrospective study. Am. J. Orthod. Dentofac. Orthop. 2023, 164, 123–130. [Google Scholar] [CrossRef]
- Upadhyay, M.; Arqub, S.A. Biomechanics of clear aligners: Hidden truths & first principles. J. World Fed. Orthod. 2022, 11, 12–21. [Google Scholar] [PubMed]
- Gao, J.; Guo, D.; Zhang, X.; Cheng, Y.; Zhang, H.; Xu, Y.; Jin, Z.; Ma, Y. Biomechanical effects of different staging and attachment designs in maxillary molar distalization with clear aligner: A finite element study. Prog. Orthod. 2023, 24, 43. [Google Scholar] [CrossRef]
- Kohda, N.; Iijima, M.; Muguruma, T.; Brantley, W.A.; Ahluwalia, K.S.; Mizoguchi, I. Effects of mechanical properties of thermoplastic materials on the initial force of thermoplastic appliances. Angle Orthod. 2013, 83, 476–483. [Google Scholar] [CrossRef]
- Palone, M.; Longo, M.; Arveda, N.; Nacucchi, M.; Pascalis, F.; Spedicato, G.A.; Siciliani, G.; Lombardo, L. Micro-computed tomography evaluation of general trends in aligner thickness and gap width after thermoforming procedures involving six commercial clear aligners: An in vitro study. Korean J. Orthod. 2021, 51, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Mao, B.; Tian, Y.; Xiao, Y.; Li, J.; Zhou, Y. The effect of maxillary molar distalization with clear aligner: A 4D finite-element study with staging simulation. Prog. Orthod. 2023, 24, 16. [Google Scholar] [CrossRef]
- Li, N.; Wang, C.; Yang, M.; Chen, D.; Yang, M.; Li, D.; Qui, S.; Chen, Q.; Feng, Y. Effects of different tooth movement patterns and aligner thicknesses on maxillary arch expansion with clear aligners: A three-dimensional finite element study. Front. Bioeng. Biotechnol. 2024, 12, 1424319. [Google Scholar] [CrossRef] [PubMed]
- Guo, R.; Lam, X.Y.; Zhang, L.; Li, W.; Lin, Y. Biomechanical analysis of miniscrew-assisted molar distalization with clear aligners: A three-dimensional finite element study. Eur. J. Orthod. 2024, 46, 1–9. [Google Scholar] [CrossRef]
- Al-Thomali, Y.; Basha, S.; Mohamed, R.N. Pendulum and modified pendulum appliances for maxillary molar distalization in Class II malocclusion—A systematic review. Acta Odontol. Scand. 2017, 75, 394–401. [Google Scholar] [CrossRef]
- Nanda, R.S.; Tosun, Y.S. Biomechanics in Orthodontics: Principles and Practice; Quintessence Publishing Co.: Hanover Park, IL, USA, 2010. [Google Scholar]
- Yassir, Y.A.; Nabbat, S.A.; McIntyre, G.T.; Bearn, D.R. Clinical effectiveness of clear aligner treatment compared to fixed appliance treatment: An overview of systematic reviews. Clin. Oral Investig. 2022, 26, 2353–2370. [Google Scholar] [CrossRef]
- Elshazly, T.M.; Salvatori, D.; Elattar, H.; Bourauel, C.; Keilig, L. Effect of trimming line design and edge extension of orthodontic aligners on force transmission: A 3D finite element study. J. Mech. Behav. Biomed. Mater. 2023, 140, 105741. [Google Scholar] [CrossRef]
- Elshazly, T.M.; Keilig, L.; Salvatori, D.; Chavanne, P.; Aldesoki, M.; Bourauel, C. Effect of trimming line design and edge extension of orthodontic aligners on force transmission: An in vitro study. J. Dent. 2022, 125, 104276. [Google Scholar] [CrossRef] [PubMed]
- Rossini, G.; Schiaffino, M.; Parrini, S.; Sedran, A.; Deregibus, A.; Castroflorio, T. Upper second molar distalization with clear aligners: A finite element study. Appl. Sci. 2020, 10, 7739. [Google Scholar] [CrossRef]
- Cattaneo, P.M.; Dalstra, M.; Melsen, B. Moment-to-force ratio, center of rotation, and force level: A finite element study predicting their interdependency for simulated orthodontic loading regimens. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 681–689. [Google Scholar] [CrossRef] [PubMed]


| Component | Definition | Sign Convention | |
|---|---|---|---|
| Force (X) | Buccolingual | (+) Buccal | (−) Lingual |
| Force (Y) | Mesiodistal | (+) Distal | (−) Mesial |
| Force (Z) | Occlusogingival | (+) Occlusal | (−) Gingival |
| Moment (X) | Angulation | (+) Mesial tipping | (−) Distal tipping |
| Moment (Y) | Inclination | (+) Buccal | (−) Lingual |
| Moment (Z) | Rotation | (+) Distal rotation | (−) Mesial rotation |
| Measurements | Group 1 (Median, IQR) | Group 2 (Median, IQR) | Group 3 (Median, IQR) | Group 4 (Median, IQR) | p-Value | Effect Size (η2) |
|---|---|---|---|---|---|---|
| Fx (N) | 0.31, 0.30 a | 0.57, 0.13 b | 0.56, 0.26 b | 0.46, 0.34 b | H = 30.086 <0.001 *** | 0.284 |
| Fy | 2.01, 1.80 a | 1.56, 1.01 a | 3.11, 0.93 b | 1.83, 0.98 a | H = 46.654 <0.001 *** | 0.194 |
| Fz | −0.60, 0.32 a | −0.88, 0.66 a | −1.23, 0.57 b | −1.33, 0.35 b | H = 59.582 <0.001 *** | 0.088 |
| Mx (Nmm) | 12.38, 6.76 a | 10.27, 7.58 b | 20.83, 4.74 c | 14.50, 5.36 d | H = 65.121 <0.001 *** | 0.536 |
| My | −3.23, 2.95 a | −2.92, 2.55 a | −6.06, 2.52 b | −2.97, 2.28 a | H = 24.937 <0.001 *** | 0.337 |
| Mz | 1.02, 2.51 a | 0.07, 1.78 a,c | 3.70, 3.99 b | −0.57, 2.11 c | H = 43.935 <0.001 *** | 0.238 |
| Mx/Fy ratio | 6.21, 3.55 a | 5.77, 1.72 b | 6.73, 0.98 a | 7.02, 2.10 a | H = 10.807 0.003 ** | 0.319 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, Y.-K.; Jee, M.-J.; Kim, S.-H.; Kim, S.-S.; Park, S.-B.; Kim, Y.-I. A Comparative In Vitro Analysis of Attachment and Enhanced Structural Features for Molar Distalization in Clear Aligner Therapy. Appl. Sci. 2025, 15, 6655. https://doi.org/10.3390/app15126655
Choi Y-K, Jee M-J, Kim S-H, Kim S-S, Park S-B, Kim Y-I. A Comparative In Vitro Analysis of Attachment and Enhanced Structural Features for Molar Distalization in Clear Aligner Therapy. Applied Sciences. 2025; 15(12):6655. https://doi.org/10.3390/app15126655
Chicago/Turabian StyleChoi, Youn-Kyung, Min-Jeong Jee, Sung-Hun Kim, Seong-Sik Kim, Soo-Byung Park, and Yong-Il Kim. 2025. "A Comparative In Vitro Analysis of Attachment and Enhanced Structural Features for Molar Distalization in Clear Aligner Therapy" Applied Sciences 15, no. 12: 6655. https://doi.org/10.3390/app15126655
APA StyleChoi, Y.-K., Jee, M.-J., Kim, S.-H., Kim, S.-S., Park, S.-B., & Kim, Y.-I. (2025). A Comparative In Vitro Analysis of Attachment and Enhanced Structural Features for Molar Distalization in Clear Aligner Therapy. Applied Sciences, 15(12), 6655. https://doi.org/10.3390/app15126655






