Comparison of the Fracture Resistance of Provisional Crowns and Fixed Partial Dentures Manufactured with Conventional, Milling, and 3D-Printing Techniques
Abstract
1. Introduction
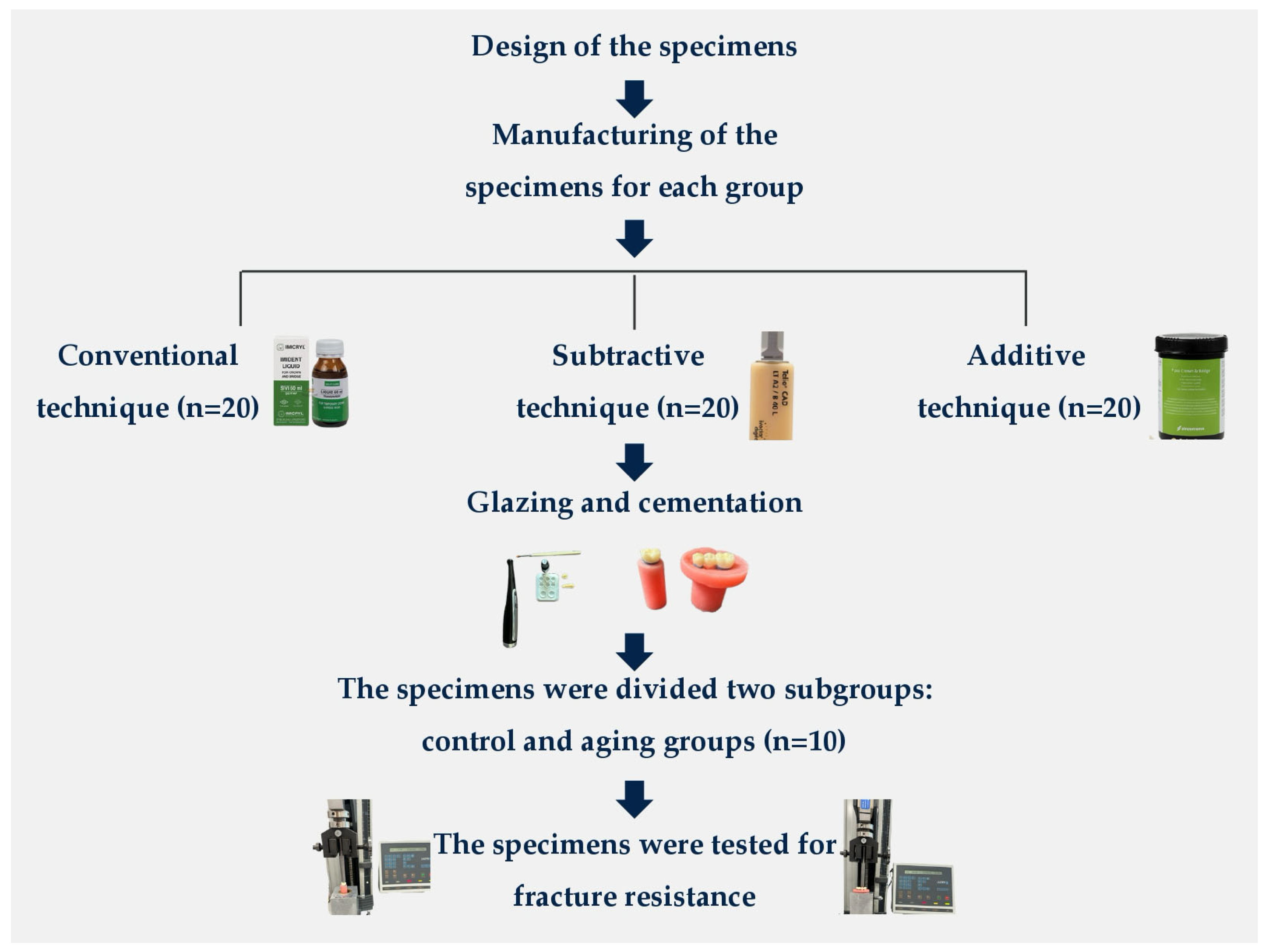
2. Materials and Methods
2.1. Sample Size Calculation
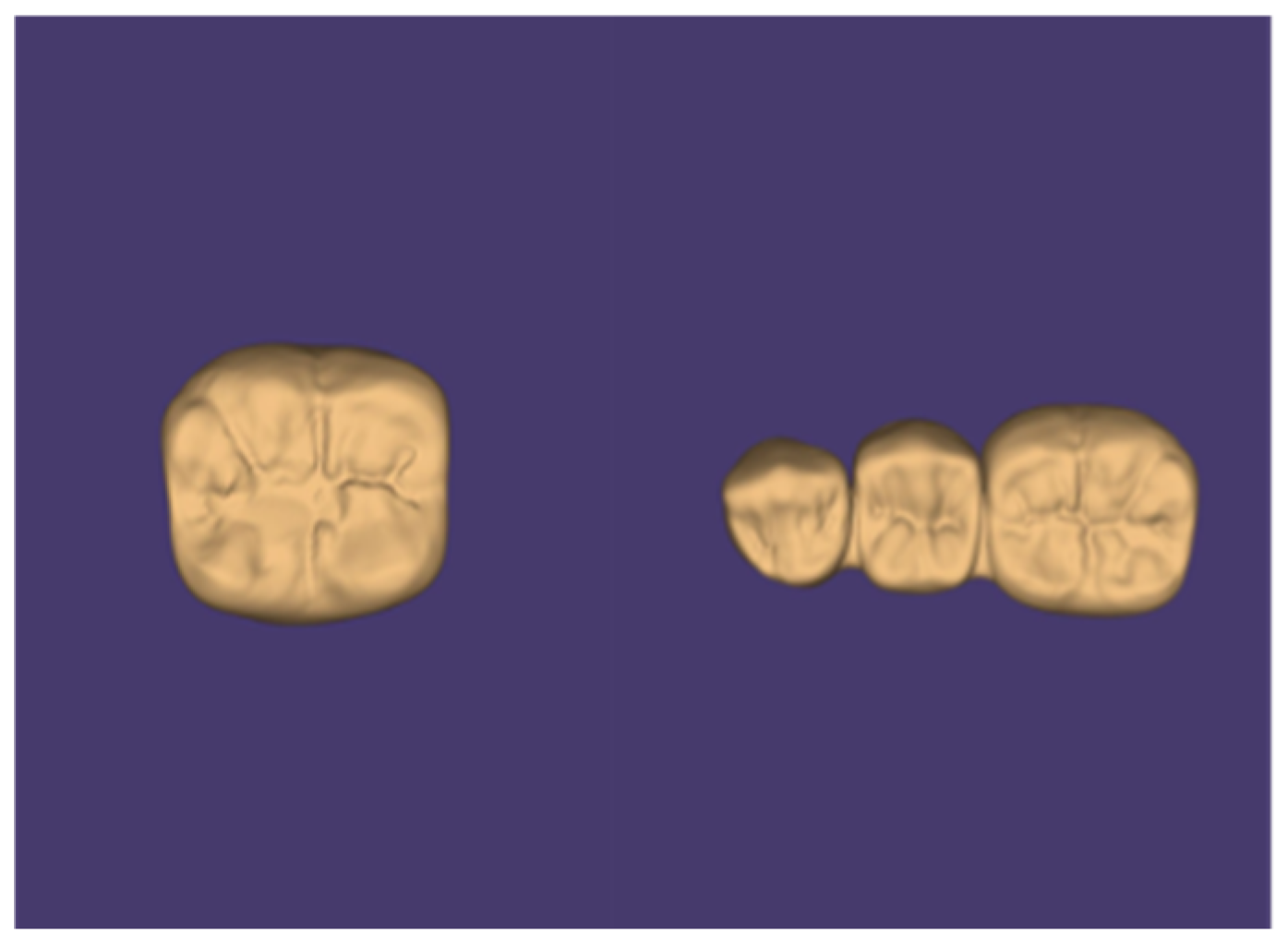
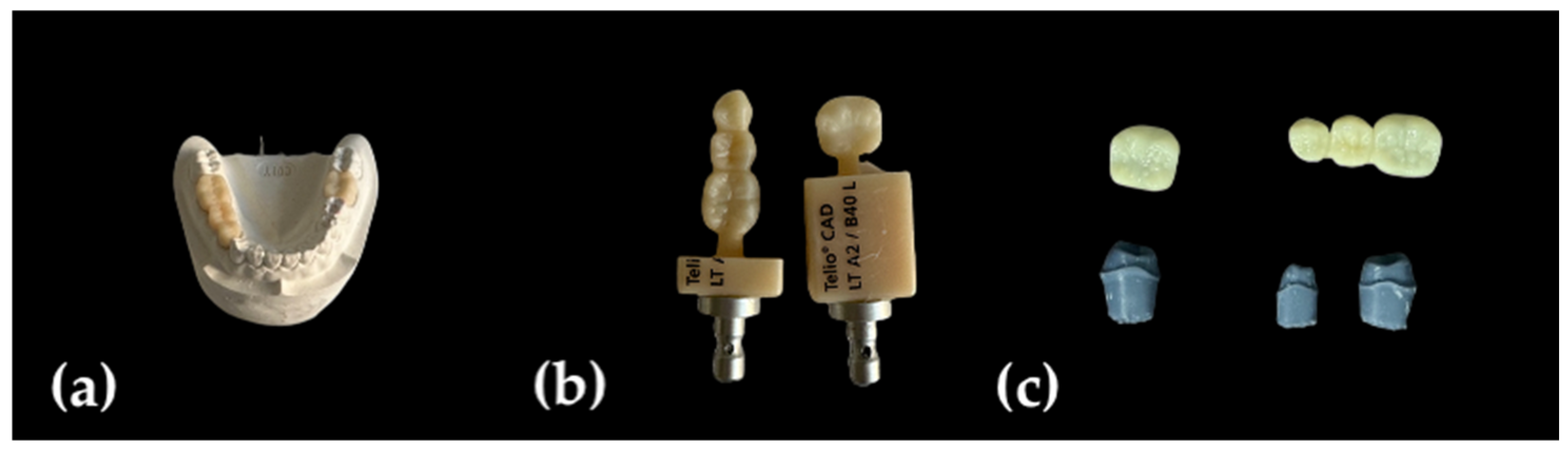
2.2. Specimen Preparation
2.3. Aging and Fracture Resistance Test
2.4. Statistical Analysis
3. Results
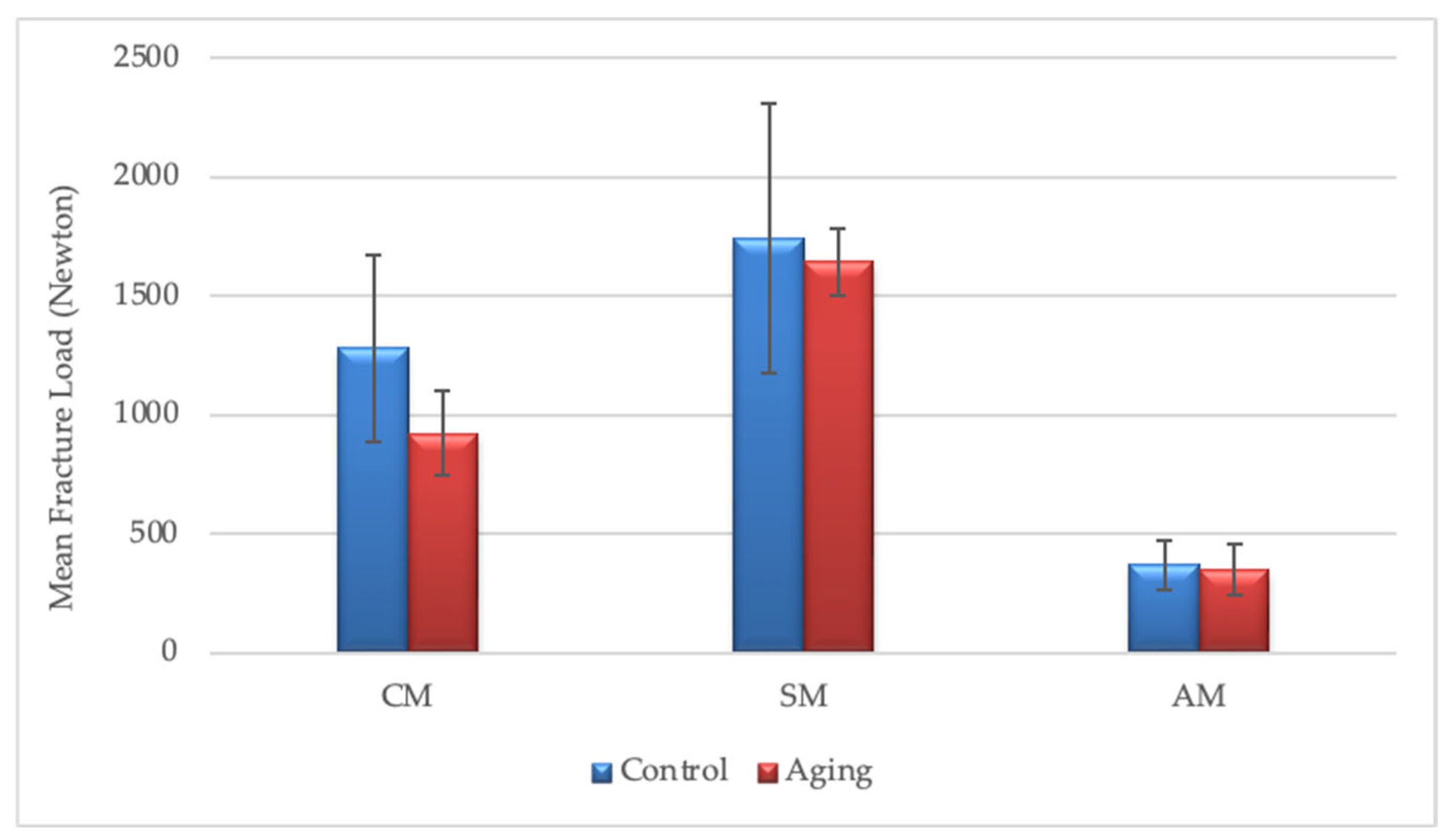
3.1. Fracture Resistance Values of the Crown Groups
3.2. Fracture Resistance Values of the Fixed Partial Denture Groups
4. Discussion
Limitations and Future Perspectives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alkhateeb, R.I.; Algaoud, H.S.; Aldamanhori, R.B.; Alshubaili, R.R.; Alalawi, H.; Gad, M.M. Fracture load of 3D-printed interim three-unit fixed dental prostheses: Impact of printing orientation and post-curing time. Polymers 2023, 15, 1737. [Google Scholar] [CrossRef] [PubMed]
- Reeponmaha, T.; Angwaravong, O.; Angwarawong, T. Comparison of fracture strength after thermo-mechanical aging between provisional crowns made with CAD/CAM and conventional method. J. Adv. Prosthodont. 2020, 12, 218. [Google Scholar] [CrossRef] [PubMed]
- Abad-Coronel, C.; Carrera, E.; Mena Córdova, N.; Fajardo, J.I.; Aliaga, P. Comparative analysis of fracture resistance between CAD/CAM materials for interim fixed prosthesis. Materials 2021, 14, 7791. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Sayed, M.E.; Shetty, M.; Alqahtani, S.M.; Al Wadei, M.H.D.; Gupta, S.G.; Othman, A.A.A.; Alshehri, A.H.; Alqarni, H.; Mobarki, A.H.; et al. Physical and mechanical properties of 3D-printed provisional crowns and fixed dental prosthesis resins compared to CAD/CAM milled and conventional provisional resins: A systematic review and meta-analysis. Polymers 2022, 14, 2691. [Google Scholar] [CrossRef]
- Yao, J.; Li, J.; Wang, Y.; Huang, H. Comparison of the flexural strength and marginal accuracy of traditional and CAD/CAM interim materials before and after thermal cycling. J. Prosthet. Dent. 2014, 112, 649–657. [Google Scholar] [CrossRef]
- Sadid-Zadeh, R.; Zirkel, C.; Makwoka, S.; Li, R. Fracture strength of interim CAD/CAM and conventional partial fixed dental prostheses. J. Prosthodont. 2021, 30, 720–724. [Google Scholar] [CrossRef]
- Henderson, J.Y.; Korioth, T.V.P.; Tantbirojn, D.; Versluis, A. Failure load of milled, 3D-printed, and conventional chairside-dispensed interim 3-unit fixed dental prostheses. J. Prosthet. Dent. 2022, 127, 275.e1–275.e7. [Google Scholar] [CrossRef]
- Bein, L.; Rauch, A.; Schmidt, M.; Rosentritt, M. In vitro fatigue and fracture testing of temporary materials from different manufacturing processes in implant-supported anterior crowns. Clin. Oral Investig. 2023, 27, 4215–4224. [Google Scholar] [CrossRef]
- Sulaiman, T.A. Materials in digital dentistry: A review. J. Esthet. Restor. Dent. 2020, 32, 171–181. [Google Scholar] [CrossRef]
- Suralik, K.M.; Sun, J.; Chen, C.Y.; Lee, S.J. Effect of fabrication method on fracture strength of provisional implant supported fixed dental prostheses. Prosthesis 2020, 2, 325–332. [Google Scholar] [CrossRef]
- Tian, Y.; Chen, C.; Xu, X.; Wang, J.; Hou, X.; Li, K.; Lu, X.; Shi, H.; Lee, E.S.; Jiang, H.B. A review of 3D printing in dentistry: Technologies, affecting factors, and applications. Scanning 2021, 2021, 9950131. [Google Scholar] [CrossRef] [PubMed]
- Kaiahara, F.H.; Pizi, E.C.G.; Straioto, F.G.; Galvani, L.D.; Kuga, M.C.; Arrué, T.A.; Junior, A.R.; Só, M.V.R.; Pereira, J.R.; Vidotti, H. Influence of Printing Orientation on the Mechanical Properties of Provisional Polymeric Materials Produced by 3D Printing. Polymers 2025, 17, 265. [Google Scholar] [CrossRef]
- Park, S.M.; Park, J.M.; Kim, S.K.; Heo, S.J.; Koak, J.Y. Flexural strength of 3D-printing resin materials for provisional fixed dental prostheses. Materials 2020, 13, 3970. [Google Scholar] [CrossRef]
- Taşın, S.; Ismatullaev, A. Comparative evaluation of the effect of thermocycling on the mechanical properties of conventionally polymerized, CAD-CAM milled, and 3D-printed interim materials. J. Prosthet. Dent. 2022, 127, 173.e1–173.e8. [Google Scholar] [CrossRef]
- Al-Wahadni, A.; Abu Rashed, B.O.; Al-Fodeh, R.; Tabanjah, A.; Hatamleh, M. Marginal and Internal Gaps, Surface Roughness and Fracture Resistance of Provisional Crowns Fabricated with 3D Printing and Milling Systems. Oper. Dent. 2023, 48, 464–471. [Google Scholar] [CrossRef]
- Alghauli, M.A.; Almutairi, S.; Almuzaini, S.; Aljohani, R.; Aljohani, W.; Alqutaibi, A.Y. Properties and behavior of additively manufactured provisional fixed dental prostheses: A systematic review on 3D printing orientations relative to applied materials and postprocessing. J. Esthet. Restor. Dent. 2025, 37, 373–381. [Google Scholar] [CrossRef]
- Digholkar, S.; Madhav, V.N.V.; Palaskar, J. Evaluation of the flexural strength and microhardness of provisional crown and bridge materials fabricated by different methods. J. Indian Prosthodont. Soc. 2016, 16, 328–334. [Google Scholar] [CrossRef]
- Pantea, M.; Ciocoiu, R.C.; Greabu, M.; Ripszky Totan, A.; Imre, M.; Țâncu, A.M.C.; Sfeatcu, R.; Spînu, T.C.; Ilinca, R.; Petre, A.E. Compressive and flexural strength of 3D-printed and conventional resins designated for interim fixed dental prostheses: An in vitro comparison. Materials 2022, 15, 3075. [Google Scholar] [CrossRef]
- Ibrahim, A.; El Shehawy, D.; El-Naggar, G. Fracture resistance of interim restoration constructed by 3D printing versus CAD/CAM technique (In vitro study). Ain Shams Dent. J. 2020, 23, 13–20. [Google Scholar] [CrossRef]
- Karaman, T.; Eser, B.; Altintas, E.; Atala, M.H. Evaluation of the effects of finish line type and width on the fracture strength of provisional crowns. Odontology 2021, 109, 76–81. [Google Scholar] [CrossRef]
- Martín-Ortega, N.; Sallorenzo, A.; Casajús, J.; Cervera, A.; Revilla-León, M.; Gómez-Polo, M. Fracture resistance of additive manufactured and milled implant-supported interim crowns. J. Prosthet. Dent. 2022, 127, 267–274. [Google Scholar] [CrossRef] [PubMed]
- Othman, A.; Sandmair, M.; Alevizakos, V.; von See, C. The fracture resistance of 3D-printed versus milled provisional crowns: An in vitro study. PLoS ONE 2023, 18, e0285760. [Google Scholar] [CrossRef] [PubMed]
- Rosentritt, M.; Rauch, A.; Hahnel, S.; Schmidt, M. In-vitro performance of subtractively and additively manufactured resin-based molar crowns. J. Mech. Behav. Biomed. Mater. 2023, 141, 105806. [Google Scholar] [CrossRef] [PubMed]
- Elsareef, S.S.; Azer, A.S.; Morsy, N. Evaluation of fracture resistance and marginal fit of implant-supported interim crowns fabricated by conventional, additive and subtractive methods. BMC Oral Health 2024, 24, 852. [Google Scholar] [CrossRef]
- Yıldırım, M.; Aykent, F.; Özdoğan, M.S. Comparison of fracture strength, surface hardness, and color stain of conventionally fabricated, 3D printed, and CAD-CAM milled interim prosthodontic materials after thermocycling. J. Adv. Prosthodont. 2024, 16, 115. [Google Scholar] [CrossRef]
- Tüfekçi, B.B.; Yeşil, Z. Examination of the effect of aging process on marginal fit and fracture strength of temporary crowns prepared from different materials. Heliyon 2024, 10, e26737. [Google Scholar] [CrossRef]
- Reymus, M.; Fabritius, R.; Keßler, A.; Hickel, R.; Edelhoff, D.; Stawarczyk, B. Fracture load of 3D-printed fixed dental prostheses compared with milled and conventionally fabricated ones: The impact of resin material, build direction, post-curing, and artificial aging—An in vitro study. Clin. Oral Investig. 2020, 24, 701–710. [Google Scholar] [CrossRef]
- Nold, J.; Wesemann, C.; Rieg, L.; Binder, L.; Witkowski, S.; Spies, B.C.; Kohal, R.J. Does printing orientation matter? In-vitro fracture strength of temporary fixed dental prostheses after a 1-year simulation in the artificial mouth. Materials 2021, 14, 259. [Google Scholar] [CrossRef]
- Bhambhu, S.; Sahni, S.; Padiyar, N.; Kaurani, P. Comparison of fracture resistance of three-unit provisional fixed dental prostheses fabricated using conventional and digital methods. Int. J. Prosthodont. Restor. Dent. 2023, 12, 59–63. [Google Scholar] [CrossRef]
- Valenti, C.; Federici, M.I.; Masciotti, F.; Marinucci, L.; Xhimitiku, I.; Cianetti, S.; Pagano, S. Mechanical properties of 3D printed prosthetic materials compared with milled and conventional processing: A systematic review and meta-analysis of in vitro studies. J. Prosthet. Dent. 2024, 132, 381–391. [Google Scholar] [CrossRef]
- Abad-Coronel, C.; Durán Urdiales, D.; Benalcázar Arias, M.V.; Córdova, A.K.; Medina, M.S.; Bravo Torres, W. Flexural strength, fatigue behavior, and microhardness of three-dimensional (3D)-printed resin material for indirect restorations: A systematic review. Materials 2025, 18, 556. [Google Scholar] [CrossRef] [PubMed]
- Rayyan, M.; Aboushelib, M.; Sayed, N.M.; Ibrahim, A.; Jimbo, R. Comparison of interim restorations fabricated by CAD/CAM with those fabricated manually. J. Prosthet. Dent. 2015, 114, 414–419. [Google Scholar] [CrossRef]
- Karaokutan, I.; Sayin, G.; Kara, O. In vitro study of fracture strength of provisional crown materials. J. Adv. Prosthodont. 2015, 7, 27–31. [Google Scholar] [CrossRef]
- Alp, G.; Murat, S.; Yilmaz, B. Comparison of flexural strength of different CAD/CAM PMMA-based polymers. J. Prosthodont. 2019, 28, e491–e495. [Google Scholar] [CrossRef]
- Ellakany, P.; Fouda, S.M.; Mahrous, A.A.; AlGhamdi, M.A.; Aly, N.M. Influence of CAD/CAM milling and 3D-printing fabrication methods on the mechanical properties of 3-unit interim fixed dental prosthesis after thermo-mechanical aging process. Polymers 2022, 14, 4103. [Google Scholar] [CrossRef]
- Mayer, J.; Stawarczyk, B.; Vogt, K.; Hickel, R.; Edelhoff, D.; Reymus, M. Influence of cleaning methods after 3D printing on two-body wear and fracture load of resin-based temporary crown and bridge material. Clin. Oral Investig. 2021, 25, 5987–5996. [Google Scholar] [CrossRef]
- Alzahrani, S.J.; Hajjaj, M.S.; Azhari, A.A.; Ahmed, W.M.; Yeslam, H.E.; Carvalho, R.M. Mechanical properties of three-dimensional printed provisional resin materials for crown and fixed dental prosthesis: A systematic review. Bioengineering 2023, 10, 663. [Google Scholar] [CrossRef]
- Keßler, A.; Hickel, R.; Ilie, N. In vitro investigation of the influence of printing direction on the flexural strength, flexural modulus and fractographic analysis of 3D-printed temporary materials. Dent. Mater. J. 2021, 40, 641–649. [Google Scholar] [CrossRef]
- Turksayar, A.A.D.; Donmez, M.B.; Olcay, E.O.; Demirel, M.; Demir, E. Effect of printing orientation on the fracture strength of additively manufactured 3-unit interim fixed dental prostheses after aging. J. Dent. 2022, 124, 104155. [Google Scholar] [CrossRef]
- Al-Dulaijan, Y.A.; Alsulaimi, L.; Alotaibi, R.; Alboainain, A.; Akhtar, S.; Khan, S.Q.; Al-Ghamdi, M.; Gad, M.M. Effect of printing orientation and postcuring time on the flexural strength of 3D-printed resins. J. Prosthodont. 2023, 32, 45–52. [Google Scholar] [CrossRef]
- Paranna, S.; Thosar, N.; Kanitkar, A. Effect of build orientation on mechanical and physical properties of additively manufactured resins using digital light processing technology in dentistry: A systematic review. J. Contemp. Dent. Pract. 2024, 25, 892. [Google Scholar] [CrossRef]
- Elmokadem, M.I.; Haggag, K.M.; Mohamed, H.R. Effect of thermo-mechanical cycling on fracture resistance of different CAD/CAM crowns: An in vitro study. J. Contemp. Dent. Pract. 2024, 25, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Tahayeri, A.; Morgan, M.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Legaz, J.; Sailer, I.; Mojon, P.; Lee, H.; Karasan, D. Mechanical properties of additively manufactured and milled interim 3-unit fixed dental prostheses. J. Prosthodont. 2023, 32, 234–243. [Google Scholar] [CrossRef]
- Sabbah, A.; Romanos, G.; Delgado-Ruiz, R. Impact of layer thickness and storage time on the properties of 3D-printed dental dies. Materials 2021, 14, 509. [Google Scholar] [CrossRef]
- Aktaş, N.; Akın, Y.; Ocak, M.; Atabek, D.; Bankoğlu Güngör, M. Marginal and internal adaptation and absolute marginal discrepancy of 3D-printed, milled, and prefabricated crowns for primary molar teeth: An in vitro comparative study. BMC Oral Health 2025, 25, 575. [Google Scholar] [CrossRef]
- Lai, Y.C.; Yang, C.C.; Levon, J.A.; Chu, T.M.G.; Morton, D.; Lin, W.S. The effects of additive manufacturing technologies and finish line designs on the trueness and dimensional stability of 3D-printed dies. J. Prosthodont. 2023, 32, 519–526. [Google Scholar] [CrossRef]

| Material | Content | Brand | Manufacturer | Lot Number |
|---|---|---|---|---|
| PMMA powder and liquid | Powder: PMMA Liquid: Methyl methacrylate (MMA) | Imicryl | Imident, Konya, Türkiye | B601, B633 |
| PMMA block | PMMA 99.5% and Pigments (<1.0%) | Telio CAD | Ivoclar Vivadent, Schaan, Liechtenstein | Z04ZG3, Z04F2C |
| Methacrylate resin | Acrylic resin urethane dimethacrylate (UDMA) 2,2-bis(acryloyloxymethyl)butyl acrylate; trimethylolpropane triacrylate Diphenyl(2,4,6-trimethylbenzoyl) phosphine oxide) | P pro Crown & Bridge | Straumann, Basel, Switzerland | 250415A |
| Source of Variation | Degrees of Freedom (df) | Sum of Squares (SS) | Mean of Squares (MS) | F | p |
|---|---|---|---|---|---|
| Manufacturing Method | 2 | 17,859,090.3 | 8,929,545.16 | 127.984 | <0.001 |
| Aging | 1 | 371,044.301 | 371,044.301 | 5.318 | 0.025 |
| Manufacturing Method × Aging | 2 | 312,515.861 | 156,257.930 | 2.240 | 0.116 |
| Error | 54 | 3,767,631.35 | 69,770.951 | - | - |
| Total | 59 | 22,310,281.8 | - | - | - |
| Production Method | Aging | ||
|---|---|---|---|
| Applied | Not Applied | ||
| Conventional Manufacturing | Mean ± SD | 924.03 ± 325.56 | 1280.48 ± 357.61 |
| Median (Q1–Q3) | 851.99 (701.75–1019.89) | 1284.15 (1006.55–1599.73) | |
| Min–Max | 530.79–1708.83 | 645.30–1688.23 | |
| Subtractive Manufacturing | Mean ± SD | 1645.41 ± 346.82 | 1741.82 ± 200.64 |
| Median (Q1–Q3) | 1597.78 (1433.04–1725.63) | 1675.99 (1585.92–1810.34) | |
| Min–Max | 1293.02–2481.09 | 1551.66–2220.96 | |
| Additive Manufacturing | Mean ± SD | 350.59 N ± 108.91 | 369.56 ± 111.13 |
| Median (Q1–Q3) | 377 (236.25–422.56) | 367.08 (293.52–457.48) | |
| Min–Max | 192.7–516.17 | 212.5–533.02 | |
| Source of Variation | Degrees of Freedom (df) | Sum of Squares (SS) | Mean of Squares (MS) | F | p |
|---|---|---|---|---|---|
| Manufacturing Method | 2 | 3,084,537.24 | 1,542,268.62 | 23.758 | <0.001 |
| Aging | 1 | 1,163,758.04 | 1,163,758.03 | 17.927 | <0.001 |
| Manufacturing Method × Aging | 2 | 1,558,295.57 | 779,147.79 | 12.003 | <0.001 |
| Error | 54 | 3,505,416.69 | 64,915.124 | --- | --- |
| Total | 59 | 9,312,007.54 | --- | --- | --- |
| Production Method | Aging | ||
|---|---|---|---|
| Applied | Not Applied | ||
| Conventional Manufacturing | Mean ± SD | 585.06 ± 96.77 | 695.60 ± 140.97 |
| Median (Q1–Q3): | 587.99 (558.60–602.55) | 724.68 (579.76–815.65) | |
| Min–Max | 432.10–802.09 | 450.27–858.72 | |
| Subtractive Manufacturing | Mean ± SD | 561.63 ± 140.21 | 1291.13 ± 564.15 |
| Median (Q1–Q3): | 592.71 (457.94–656.56) | 993.20 (917.29–1692.83) | |
| Min–Max | 277.86–745.65 | 765.62–2447.01 | |
| Additive Manufacturing | Mean ± SD | 373.29 ± 107.24 | 368.87 ± 104.04 |
| Median (Q1–Q3): | 377.54 (260.90–441.06) | 372.11 (331.33–459.85) | |
| Min–Max | 214.48–542.61 | 189.48–479.42 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Güney, B.; Nalbant, A.D.; Bankoğlu Güngör, M. Comparison of the Fracture Resistance of Provisional Crowns and Fixed Partial Dentures Manufactured with Conventional, Milling, and 3D-Printing Techniques. Appl. Sci. 2025, 15, 6539. https://doi.org/10.3390/app15126539
Güney B, Nalbant AD, Bankoğlu Güngör M. Comparison of the Fracture Resistance of Provisional Crowns and Fixed Partial Dentures Manufactured with Conventional, Milling, and 3D-Printing Techniques. Applied Sciences. 2025; 15(12):6539. https://doi.org/10.3390/app15126539
Chicago/Turabian StyleGüney, Beyza, Asude Dilek Nalbant, and Merve Bankoğlu Güngör. 2025. "Comparison of the Fracture Resistance of Provisional Crowns and Fixed Partial Dentures Manufactured with Conventional, Milling, and 3D-Printing Techniques" Applied Sciences 15, no. 12: 6539. https://doi.org/10.3390/app15126539
APA StyleGüney, B., Nalbant, A. D., & Bankoğlu Güngör, M. (2025). Comparison of the Fracture Resistance of Provisional Crowns and Fixed Partial Dentures Manufactured with Conventional, Milling, and 3D-Printing Techniques. Applied Sciences, 15(12), 6539. https://doi.org/10.3390/app15126539






