Lumbosacral Transitional Disorder as a Missing Link in Symptomatic Scoliosis
Abstract
1. Introduction
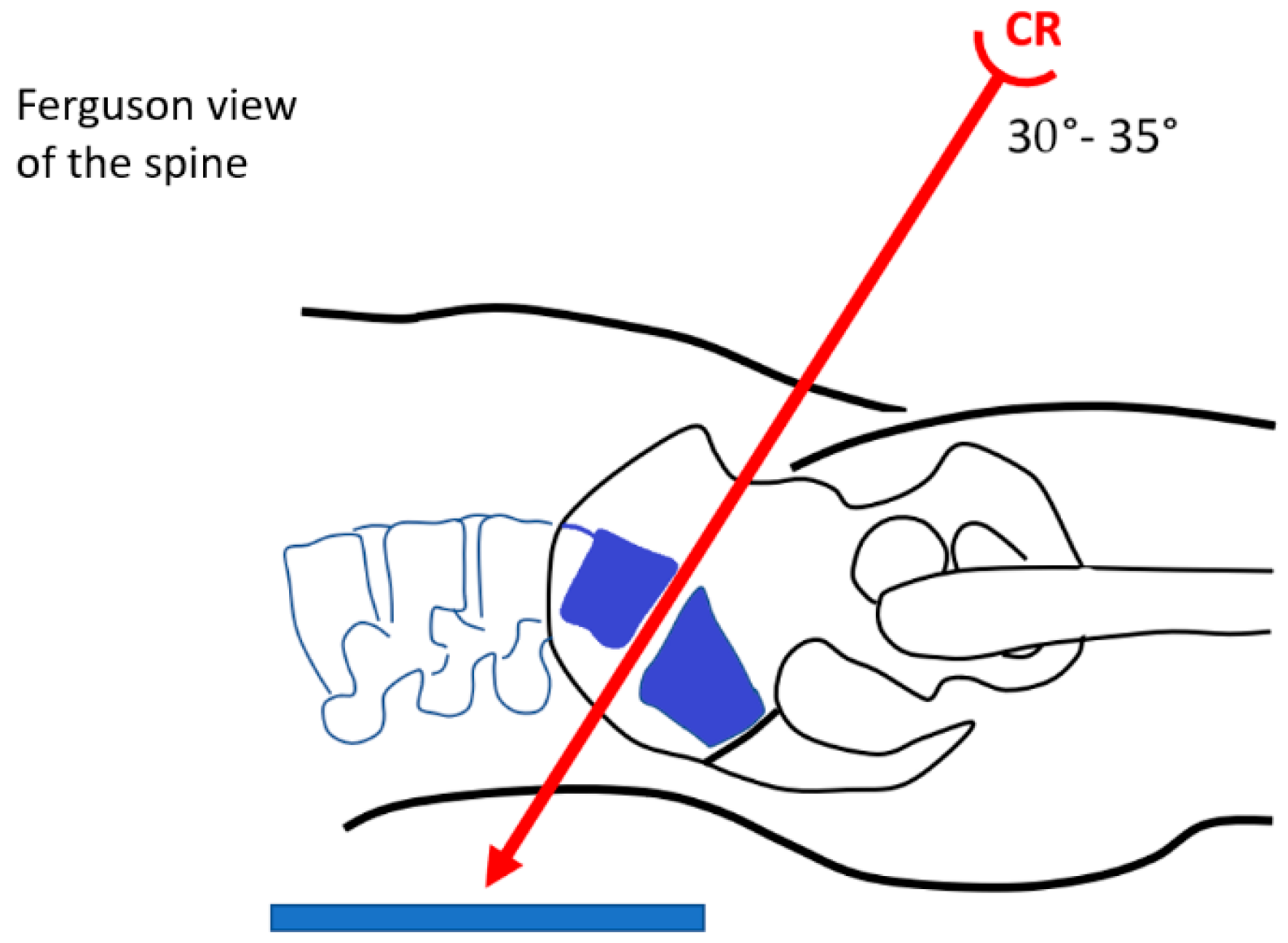
2. Methods
Initial Data at Baseline
3. Results
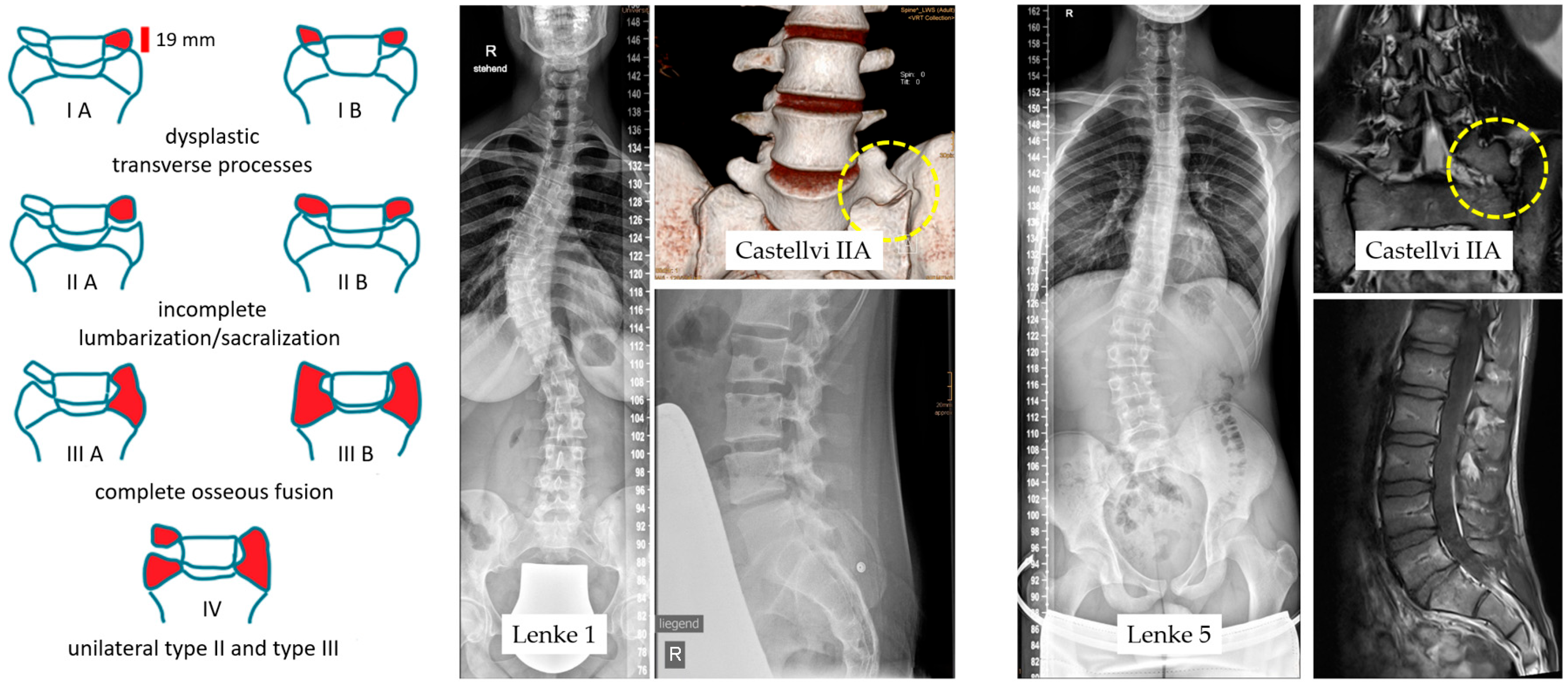
3.1. LSTVs in Castellvi Classification
3.2. Scoliosis Severity
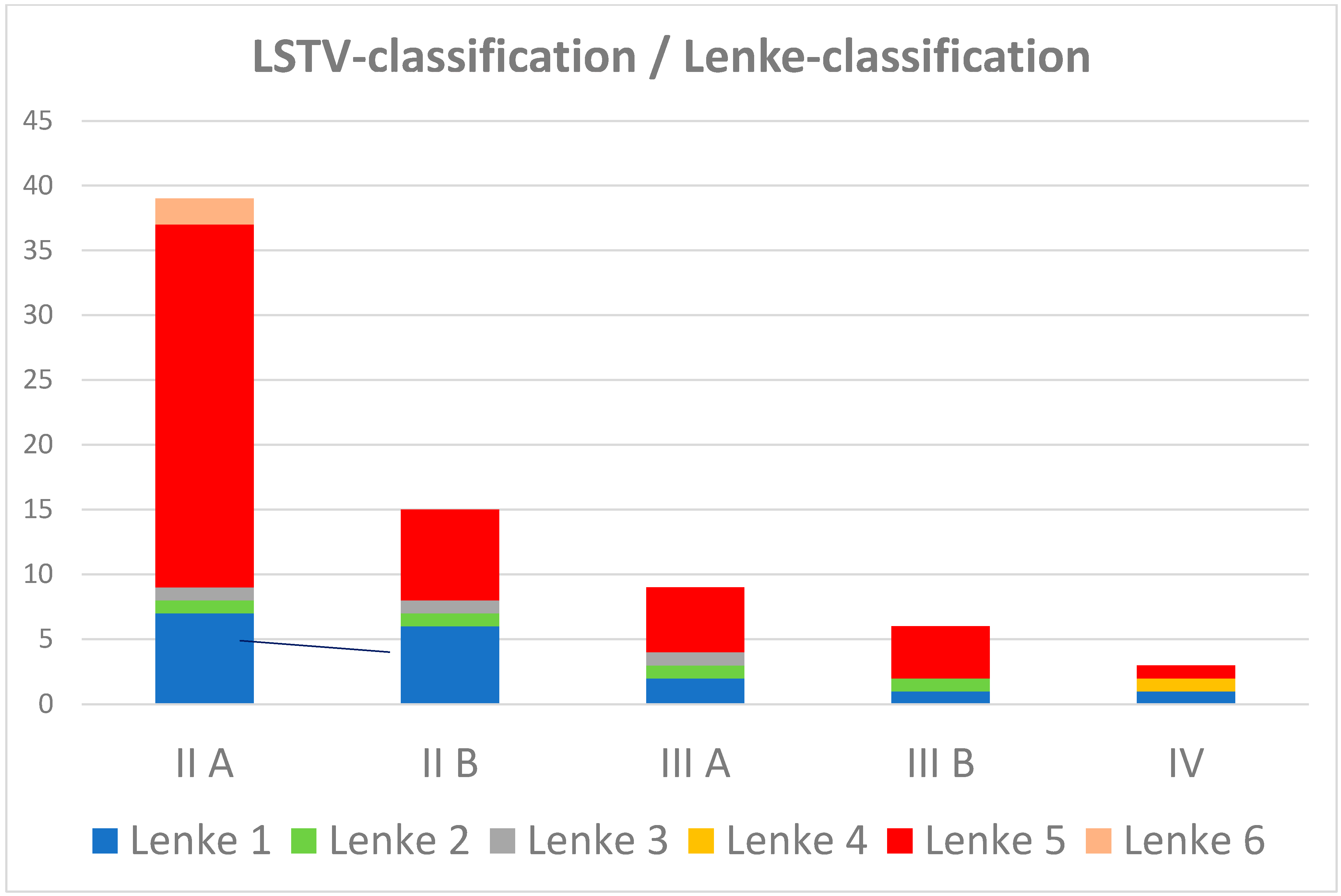
3.3. Curvature Shape in the Lenke Classification
3.4. VMVM Vertical Mid-Vertebral Angle and Diff-VMVA in the Lowest Vertebral Segments
3.5. Low Back Pain
3.6. The Literature
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bertolotti, M. Contributo alla conoscenza dei vizi di differenziazione regionale del rachide con speciale riguardo all assimilazione sacrale della v. lombare. Radiol. Medica 1917, 4, 113–144. [Google Scholar]
- Castellvi, A.E.; Goldstein, L.A.; Chan, D.P. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine 1984, 9, 493–495. [Google Scholar] [CrossRef]
- Hanhivaara, J.; Määttä, J.H.; Karppinen, J.; Niinimäki, J.; Nevalainen, M.T. The Association of Lumbosacral Transitional Vertebrae with Low Back Pain and Lumbar Degenerative Findings in MRI: A Large Cohort Study. Spine 2022, 472, 153–162. [Google Scholar] [CrossRef]
- van der Velde, R.; Ozanian, T.; Dumitrescu, B.; Haslam, J.; Staal, J.; Brett, A.; van den Bergh, J.; Geusens, P. Performance of statistical models of shape and appearance for semiautomatic segmentations of spinal vertebrae T4–L4 on digitized vertebral fracture assessment images. Spine J. 2015, 15, 1248–1254. [Google Scholar] [CrossRef] [PubMed]
- Matson, D.M.; Maccormick, L.M.; Sembrano, J.N.; Polly, J.R.D.W. Sacral Dysmorphism and Lumbosacral Transitional Vertebrae (LSTV) Review. Int. J. Spine Surg. 2020, 14, S14–S19. [Google Scholar] [CrossRef] [PubMed]
- Paik, N.C.; Lim, C.S.; Jang, H.S. Numeric and morphological verification of lumbosacral segments in 8280 consecutive patients. Spine 2013, 38, E573–E578. [Google Scholar] [CrossRef]
- McCulloch, J.A.; Waddell, G. Variation of the lumbosacral myotomes with bony segmental anomalies. J. Bone Jt. Surg. Br. Vol. 1980, 62, 475–480. [Google Scholar] [CrossRef]
- Carrino, J.A.; Campbell, P.D., Jr.; Lin, D.C.; Morrison, W.B.; Schweitzer, M.E.; Flanders, A.E.; Eng, J.; Vaccaro, A.R. Effect of spinal segment variants on numbering vertebral levels at lumbar MR imaging. Radiology 2011, 259, 196–202. [Google Scholar] [CrossRef] [PubMed]
- McGrath, K.A.; Rabah, N.M.; Steinmetz, M.P. Identifying treatment patterns in patients with Bertolotti syndrome: An elusive cause of chronic low back pain. Spine J. 2021, 21, 1497–1503. [Google Scholar] [CrossRef]
- Farshad, M.; Aichmair, A.; Hughes, A.P.; Herzog, R.J.; Farshad-Amacker, N.A. A reliable measurement for identifying a lumbosacral transitional vertebra with a solid bony bridge on a single-slice midsagittal MRI or plain lateral radiograph. Bone Jt. J. 2013, 95, 1533–1537. [Google Scholar] [CrossRef]
- Chalian, M. Prediction of transitional lumbosacral anatomy on magnetic resonance imaging of the lumbar spine. World J. Radiol. 2012, 4, 97–101. [Google Scholar] [CrossRef]
- Tatara, Y.; Niimura, T.; Sekiya, T.; Mihara, H. Changes in Lumbosacral Anatomy and Vertebral Numbering in Patients with Thoracolumbar and/or Lumbosacral Transitional Vertebrae. JBJS Open Access 2021, 6, e20.00167. [Google Scholar] [CrossRef] [PubMed]
- Garg, B.; Mehta, N.; Goyal, A.; Rangaswamy, N.; Upadhayay, A. Variations in the Number of Thoracic and Lumbar Vertebrae in Patients with Adolescent Idiopathic Scoliosis: A Retrospective, Observational Study. Int. J. Spine Surg. 2021, 15, 359–367. [Google Scholar] [CrossRef]
- McGrath, K.A.; Thompson, N.R.; Fisher, E.; Kanasz, J.; Golubovsky, J.L.; Steinmetz, M.P. Quality-of-life and postoperative satisfaction following pseudoarthrectomy in patients with Bertolotti syndrome. Spine J. 2022, 22, 1292–1300. [Google Scholar] [CrossRef]
- Quinlan, J.F.; Duke, D.; Eustace, S. Bertolotti’s syndrome. A cause of back pain in young people. J. Bone Jt. Surg. Br. 2006, 88, 1183–1186. [Google Scholar] [CrossRef]
- Mahato, N.K. Lumbosacral transitional vertebrae: Variations in low back structure, biomechanics, and stress patterns. J. Chiropr. Med. 2012, 11, 134–135. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lenke, L.G.; Betz, R.R.; Harms, J.; Bridwell, K.H.; Clements, D.H.; Lowe, T.G.; Blanke, K. Adolescent idiopathic scoliosis: A new classification to determine extent of spinal arthrodesis. J. Bone Jt. Surg. Am. 2001, 83, 1169–1181. [Google Scholar] [CrossRef]
- Lee, C.S.; Ha, J.-K.; Kim, D.G.; Hwang, C.J.; Lee, D.-H.; Cho, J.H. The Clinical Importance of Lumbosacral Transitional Vertebra in Patients with Adolescent Idiopathic Scoliosis. Spine 2015, 40, E964–E970. [Google Scholar] [CrossRef]
- Farshad-Amacker, N.A.; Herzog, R.J.; Hughes, A.P.; Aichmair, A.; Farshad, M. Associations between lumbosacral transitional anatomy types and degeneration at the transitional and adjacent segments. Spine J. 2015, 15, 1210–1216. [Google Scholar] [CrossRef]
- Jancuska, J.M.; Spivak, J.M.; Bendo, J.A. A Review of Symptomatic Lumbosacral Transitional Vertebrae: Bertolotti’s Syndrome. Int. J. Spine Surg. 2015, 9, 42. [Google Scholar] [CrossRef]
- Apazidis, A.; Ricart, P.A.; Diefenbach, C.M.; Spivak, J.M. The prevalence of transitional vertebrae in the lumbar spine. Spine J. Off. J. N. Am. Spine Soc. 2011, 11, 858–862. [Google Scholar] [CrossRef]
- Tang, M.; Yang, X.-F.; Yang, S.-W.; Han, P.; Ma, Y.-M.; Yu, H.; Zhu, B. Lumbosacral transitional vertebra in a population-based study of 5860 individuals: Prevalence and relationship to low back pain. Eur. J. Radiol. 2014, 83, 1679–1682. [Google Scholar] [CrossRef]
- Konin, G.P.; Walz, D.M. Lumbosacral transitional vertebrae: Classification, imaging findings, and clinical relevance. AJNR Am. J. Neuroradiol. 2010, 31, 1778–1786. [Google Scholar] [CrossRef]
- Deng, M.; Hui, S.C.N.; Yu, F.W.P.; Lam, T.-P.; Qiu, Y.; Ng, B.K.W.; Cheng, J.C.Y.; Chu, W.C.W. MRI-based morphological evidence of spinal cord tethering predicts curve progression in adolescent idiopathic scoliosis. Spine J. 2015, 15, 1391–1401. [Google Scholar] [CrossRef]
- Chitneni, A.; Kim, R.; Danssaert, Z.; Kumar, S. A Proposed Treatment Algorithm for Low Back Pain Secondary to Bertolotti‘s Syndrome. Pain Physician 2024, 27, E275–E284. [Google Scholar]
- McGrath, K.; Schmidt, E.; Rabah, N.; Abubakr, M.; Steinmetz, M. Clinical assessment and management of Bertolotti Syndrome: A review of the literature. Spine J. 2021, 21, 1286–1296. [Google Scholar] [CrossRef] [PubMed]
- McGrath, K.A.; Lee, J.; Thompson, N.R.; Kanasz, J.; Steinmetz, M.P. Identifying the relationship between lumbar sacralization and adjacent ligamentous anatomy in patients with Bertolotti syndrome and healthy controls. J. Neurosurg. Spine 2022, 37, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Qin, X.; Qiu, Y.; He, Z.; Yin, R.; Liu, Z.; Zhu, Z. Can we stop distally at LSTV-1 for adolescent idiopathic scoliosis with Lenke 1A/2A curves? Spine 2022, 47, 624–631. [Google Scholar] [CrossRef] [PubMed]
- He, Z.; Qin, Z.; Yin, R.; Liu, Z.; Qian, B.; Qiu, Y.; Zhu, Z. The rotation of preoperative-presumed lowest instrumented vertebra: Is it a risk factor for distal adding-on in Lenke 1A/2A curve treated with selective thoracic fusion? Eur. Spine J. 2020, 29, 2054–2063. [Google Scholar] [CrossRef]
- Yin, R.; Qin, X.; He, Z.; Liu, Z.; Qiu, Y.; Zhu, Z. Which thoracic curves are at the greater risk for distal adding-on: Comparison between typical and atypical Lenke 1A curves. Eur. Spine J. 2021, 30, 1865–1871. [Google Scholar] [CrossRef] [PubMed]
- Bai, J.; Chen, K.; Wei, Q.; Chen, Z.; Chen, Y.; Ni, H.; Zhao, Y.; Li, M. Selecting the LSTV as the Lower Instrumented Vertebra in the Treatment of Lenke Types 1A and 2A Adolescent Idiopathic Scoliosis: A Minimal 3-year Follow-up. Spine 2018, 43, E390–E398. [Google Scholar] [CrossRef]
- Yin, R.; Qin, X.; Shi, B.; He, Z.; Qian, B.; Qiu, Y.; Zhu, Z. Distal Adding-on Phenomenon in Scoliosis Secondary to Chiari Malformation Type I: Incidence and Risk Factors. Spine 2021, 46, E491–E497. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Bai, H.; Liu, C.; Zhao, Y.; Feng, Y.; Li, T.; Wang, X.; Zhang, Y.; Lei, W.; Zhao, X.; et al. Distal Adding-On Phenomenon in Lenke IA and Lenke IIA: Risk Analysis and Selection of the Lowest Instrumented Vertebra. World Neurosurg. 2020, 136, e171–e180. [Google Scholar] [CrossRef] [PubMed]
- Murphy, J.S.; Upasani, V.V.; Yaszay, B.; Bastrom, T.P.; Bartley, C.E.; Samdani, A.; Lenke, L.G.; Newton, P.O. Predictors of Distal Adding-on in Thoracic Major Curves With AR Lumbar Modifiers. Spine 2017, 42, E211–E218. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.H.; Hyun, S.J.; Lee, C.H.; Kim, K.J. The Last Touched Vertebra on Supine Radiographs Can Be the Optimal Lower Instrumented Vertebra in Adolescent Idiopathic Scoliosis Patients. Neurospine 2022, 19, 236–243. [Google Scholar] [CrossRef] [PubMed]
- Fidan, F.; Çay, N.; Asiltürk, M.; Veizi, E. The incidence of congenital lumbosacral malformations in young male Turkish military school candidates population. J. Orthop. Sci. 2021, 27, 1167–1171. [Google Scholar] [CrossRef]
- Chiu, C.K.; Chin, T.F.; Chung, W.H.; Chan, C.Y.W.; Kwan, M.K. Variations in the Number of Vertebrae, Prevalence of Lumbosacral Transitional Vertebra and Prevalence of Cervical Rib Among Surgical Patients with Adolescent Idiopathic Scoliosis: An Analysis of 998 Radiographs. Spine 2024, 49, 64–70. [Google Scholar] [CrossRef]

| Age Average | Cobb Angle Average | Cobb Angle Range | Scoliosis Treatment | |
|---|---|---|---|---|
| Children Risser 0–4 n-42 | 13.3 years | 24.3° | 11°–55° | n-10 brace |
| Adult Risser 5 n-30 | 31.4 years | 32.4° | 12°–66° | n-7 (bracing at childhood) |
| n-2 (dorsal spine fusion) | ||||
| Malformations | ||||
| Risser 0–4 n-42 | n-9 patient | vertebrae (n-4), rib malformation (n-2), syringomyelia (n-1), longitudinal radiation defect (n-1), congenital clubfoot (n-1), cartilaginous exostosis disease (n-1) | ||
| Risser 5 n-30 | n-5 patient | vertebrae (n-2), rib malformation (n-2), sacral cyst (n-1), spina bifida (n-1) | ||
| Genetic | n-1 mother and daughter | |||
| n-1 twins | ||||
| Castellvi Classification | Total Data | Male | Female | |||
|---|---|---|---|---|---|---|
| n-72 | 19.4% | n-14 | 80.6% | n-58 | ||
| IIA | 54.2% | n-39 | 11.1% | n-8 | 43.1% | n-31 |
| IIB | 20.8% | n-15 | 5.6% | n-4 | 15.3% | n-11 |
| IIIA | 12.5% | n-9 | 1.4% | n-1 | 11.1% | n-8 |
| IIIB | 9.7% | n-7 | 1.4% | n-1 | 8.3% | n-6 |
| IV | 2.8% | n-2 | 2.8% | n-2 | ||
| Castellvi Classification | Extent of Curvature Cobb Angle | Average of Curvature Cobb Angle | |
|---|---|---|---|
| IIA | n-39 | 12–46° | 26.4° |
| IIB | n-15 | 21–42° | 27.1° |
| IIIA | n-9 | 16–66° | 35.0° |
| IIIB | n-7 | 12–60° | 25.4° |
| IV | n-2 | 38–40° | 39.0° |
| Lenke | lumbar Spine Modifier | Chronic Low Back Pain | |||||
|---|---|---|---|---|---|---|---|
| A | B | C | |||||
| 1 | 25.0% | n-18 | n-7 | n-7 | n-4 | 9.7% | n-7 |
| 2 | 4.2% | n-3 | |||||
| 3 | 4.2% | n-3 | |||||
| 4 | 1.4% | n-1 | |||||
| 5 | 62.5% | n-45 | n-10 | n-13 | n-22 | 32.9% | n-23 |
| 6 | 2.8% | n-2 | |||||
| Vertical Mid-Vertebral Angle | |||
|---|---|---|---|
| VMVA S1-L5 | 30.2° | n-72 | |
| VMVA L5-L4 | 18.8° | n-72 | |
| Diff-VMVA | 11.5° | n-72 | |
| Castellvi Classification | |||
| IIA | Diff-VMVA | 12.4° | n-54 |
| IIB | |||
| IIIA | Diff-VMVA | 9.3° | n-16 |
| IIIB | |||
| IV | Diff-VMVA | 5.5° | n-2 |
| Castellvi Classification | Low Back Pain Total | Low Back Pain Male | Low Back Pain Female | |||
|---|---|---|---|---|---|---|
| 48.6% | n-35 | 8.3% | n-6 | 40.3% | n-29 | |
| IIA | 27.8% | n-21 | ||||
| IIB | 9.7% | n-7 | ||||
| IIIA | 4.2% | n-3 | ||||
| IIIB | 5.5% | n-4 | ||||
| IV | 1.4% | n-1 | ||||
| Symptom-free Total | Symptom-free Male | Symptom-free Female | ||||
| 51.4% | n-37 | 9.7% | n-7 | 41.7% | n-30 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Landauer, F.; Trieb, K. Lumbosacral Transitional Disorder as a Missing Link in Symptomatic Scoliosis. Appl. Sci. 2024, 14, 2499. https://doi.org/10.3390/app14062499
Landauer F, Trieb K. Lumbosacral Transitional Disorder as a Missing Link in Symptomatic Scoliosis. Applied Sciences. 2024; 14(6):2499. https://doi.org/10.3390/app14062499
Chicago/Turabian StyleLandauer, Franz, and Klemens Trieb. 2024. "Lumbosacral Transitional Disorder as a Missing Link in Symptomatic Scoliosis" Applied Sciences 14, no. 6: 2499. https://doi.org/10.3390/app14062499
APA StyleLandauer, F., & Trieb, K. (2024). Lumbosacral Transitional Disorder as a Missing Link in Symptomatic Scoliosis. Applied Sciences, 14(6), 2499. https://doi.org/10.3390/app14062499






