Abstract
It is vital for rehabilitating patients to perform as many task-related exercises as possible. These patients often need either force or trajectory assistance in order to perform gait. While this can be provided in the form of traditional gait rehabilitation or currently emerging robot-assisted gait training, there is a need for an affordable means to assist gait training. In this study, we present a passive gait assistance device that is composed of a spring-bar system attached to an elastic cord and a specialized shoe. The shoe has two straps attached such that both plantar and dorsiflexion torque can be applied to the user depending on the angle of the pulling force. The merit of the devices is that it is an affordable means to provide the user with gait assistance while allowing some freedom of one’s foot movement. We show that, with 20 community-dwelling seniors, our system successfully produces plantar flexion and dorsiflexion torque according to the gait cycle. Furthermore, electromyography analysis suggests that plantar flexor demand during the late stance phase and dorsiflexor demand during the swing phase are significantly reduced.
1. Introduction
It has been reported by the World Health Organization that adults should participate in 150 min/week of physical activities to maintain good health [1,2]. However, it is difficult for bedridden patients suffering from muscle atrophy, caused by long-term disuse, to fulfill this requirement [3,4,5,6,7]. This elicits a vicious cycle where the ramifications include, but are not limited to, an increased risk of cancer, cardiovascular diseases, diabetes, and sarcopenia [8,9]. Current strategies to avoid the deconditioning cycle consist mainly of gait exercises provided with assistance from therapists and personal trainers. While effective, limited resources often prevent patients from receiving the required exercise. Furthermore, it is imperative that physiological gait patterns are preserved during these exercises as compensation patterns may lead to gait deficits [10].
Recent advancements have led to the development of gait rehabilitation robots [11,12,13,14,15,16,17,18,19]. These devices are designed to provide assistance by supporting bodyweight, lower limb trajectory control, and, furthermore, quantitative monitoring of the patient. However, studies have shown that full-bodyweight-supporting robot-assisted gait training (RAGT) exhibits lackluster rehabilitative efficacy [20,21,22]. The primary reason behind this is thought to be due to the lack of patient participation [23,24,25]. In order to resolve this issue, more recently, various wearable robots have been incorporated into the exercise regimen [26,27,28,29]. While hard exoskeletons were initially developed to assist patients with total loss of lower extremity function, they are now being utilized for more general RAGT purposes [30,31]. Due to added inertia and the wearability and comfort issues of hard exoskeletons, soft-type exoskeletons comprising textiles and Bowden cables have also been developed to boost users’ mobility [32,33,34,35,36]. However, both types are relatively expensive and require specialist assistance; thus, they have fallen short of being immersed in the rehabilitation scene.
While there exists a plethora of assistive devices, simple rollators do not provide any force or trajectory assistance, and it has been reported that RAGT devices restrict free movement and have an inherent difficulty in providing assist-as-needed control [24,25]. Unpowered exosuits and devices consisting of only passive elements and no actuators have become a popular research topic [37,38,39,40,41]. The main goal of such devices has been lowering the metabolic costs during gait. The strategy behind this is storing and releasing elastic energy among the joints. Collins et al. proposed an ankle orthosis consisting of a spring, rope, and clutch that harvests energy and assists the calf muscle, resulting in reduced metabolic energy during muscle contraction [37]. More recently, Barazesh and Sharbafi proposed a biarticular passive exosuit that is capable of reducing metabolic costs by 10% during gait [42]. These promising results suggest that further research is warranted in the field of passive exosuits.
In this paper, we present a novel apparatus, that can be independently used by the user without external assistance, that attaches to a conventional rollator consisting of only passive elements that aims to support patients with diminished lower extremity capabilities. Our device, unlike traditional rollators, provides force assistance according to the gait cycle while allowing relatively free lower limb movements compared to RAGT devices. This system (Figure 1a) comprises a spring-bar system with an elastic cord that is attached to a specialized shoe which has two straps, one anchored at the heel and one above the metatarsal head. Our device offers plantar flexion torque during the late stance phase which immediately transitions to dorsiflexion torque during the early swing phase. This is vital to accommodate the user’s natural gait patterns, which require plantar flexion torque for gait propulsion and subsequent dorsiflexion torque for swift foot clearance [43]. We provide simulation data, which assisted with optimizing the system’s parameters followed by empirical verification using load cells. Furthermore, we found that, with 20 community-dwelling older adults, our device successfully lowers electromyography (EMG) signals from the soleus during the stance phase and the tibialis anterior (TA) during the swing phase.
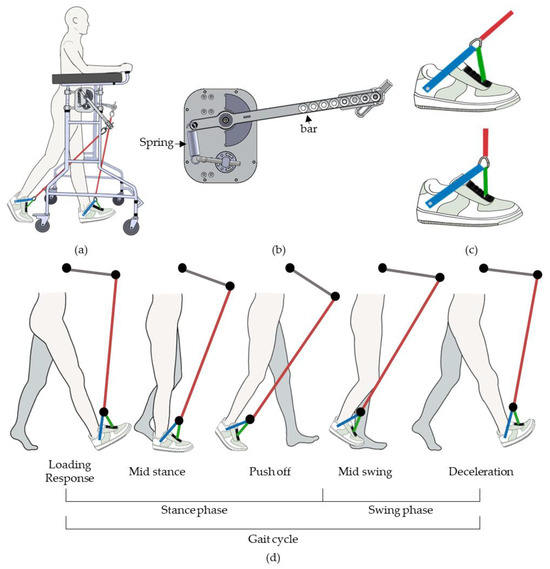
Figure 1.
Passive gait assist system. (a) Overall design. (b) Top view of the spring-bar system (c) Specialized shoe shown with the pulling force of the elastic cord (red line). When the force is at a low angle (top), tension resides in strap 1 (blue line) and slack is present in strap 2 (green line). The opposite tension and slack relationship appears when the force angle is high (bottom). (d) The passive gait assist system during the gait cycle.
2. Materials and Methods
2.1. Passive Gait Assist System
We designed the passive gait assist system to assist with plantar flexion during the late stance phase and dorsiflexion during the swing phase. This was achieved using a specialized shoe, shown in Figure 1b, which consists of straps 1 and 2 anchored at the heel and above the metatarsal, represented as blue and green lines, respectively. When the pulling force is at a low angle, relative to the ground, more tension resides within strap 1 compared to that of strap 2 which provides plantar flexion torque. When the pulling force is at a high angle, the greater tension in strap 2 induces dorsiflexion torque (Figure 1c). Thus, a device that can change the angle of the pulling force in accordance with the gait cycle needed to be implemented. We approached this by adding a spring-bar system (Figure 1b). During late stance, the elastic cord is lengthened and the bar drops, causing tension to reside more in strap 1 than strap 2, which elicits heel-off (HO) torque. When the heel lifts off from the ground, the spring-bar system returns to its original height, which increases the angle eliciting dorsiflexion torque (Figure 1d).
The height at which the spring-bar system is attached can be varied by adjusting the screws. During our treadmill gait experiments, they were adjusted to be 1.05 m from the ground, which is higher than that of overground gait in order to compensate for the height of the treadmill (5 cm). The length of the bar was 36 cm, and the stiffness of the spring was 11.77 N/mm. Also, the free length and stiffness of the elastic cord were 61 cm and 0.18 N/mm, respectively.
2.2. Simulation and Load Cell Verification
We estimated the forces acting on straps 1 and 2 by analyzing a video recording, via an RGB camera, of a healthy participant using the passive gait assist system. We initially obtained the force profile of the elastic cord during the gait cycle by measuring its change in length. This was carried out by marking the two ends of the elastic cord for each frame and then scaling the pixel lengths to mm lengths by normalizing them against the known free length of the elastic cord (Figure 2a). We then applied simple geometry (Figure 2b) to estimate the forces acting on each strap when varying the lengths of straps 1 and 2. The equations for estimating the tension in straps 1 and 2:
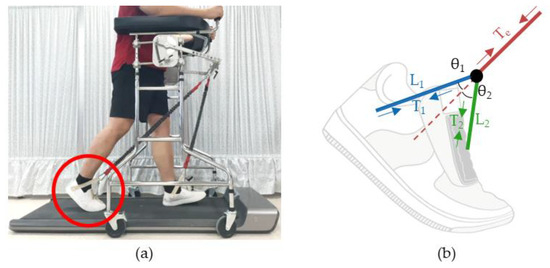
Figure 2.
User wearing a size 9 (270 mm) shoe participating in treadmill gait movement (a) Image of a subject using the passive gait assist system. (b) The pulling force of the elastic cord distributed among straps 1 and 2.
In order to verify that our simulations indeed reflect the actual forces, we attached load cells (HUMMA, HAIAM ENG., Seoul, Republic of Korea) to the end of the elastic cord and straps 1 and 2.
2.3. Experimental Setup
We recruited participants over the age of 60 and those who had sustained lower-limb injuries in the past 6 months, suffered severe medical conditions, or had a history of such conditions, and individuals with cognitive impairments were not excluded from this study. In total, 20 volunteers (age: 65.6 ± 6.2 years, height: 163.2 ± 7.5 cm, weight: 64.3 ± 9.6 kg, 13 males and 7 females) participated in this study. Each subject performed two rollator gait conditions: with and without the passive gait assist device. Data for both conditions were obtained using a treadmill set at a self-selected comfortable speed. The self-selected speed was chosen by increasing the treadmill speed up to the point at which the participant felt that it matched their typical gait speed. In order to investigate whether our system reduced plantar and dorsiflexor demands, EMG signals were obtained from the tibialis anterior (TA) and soleus (SL) using wireless EMG sensors (Trigno wireless system, Delsys Inc., Natick, MA, USA). In addition, foot pressure insoles (PedarX, Novel GmbH, Munich, Germany) were used to identify heel contact (HC) and toe-off (TO) events such that EMG signals could be assessed according to the stance and swing phase. In order to utilize the HC and TO events, the plantar force data and EMG data needed to be synchronized. This was carried out by applying an impact force to the sole of the shoe, which caused a sharp signal to appear in the plantar force data and the IMU sensor, which co-exists within the EMG sensor. The EMG and foot pressure signals were obtained at a sampling frequency of 1777 and 74 Hz, respectively. The size of the shoe and insoles were determined according to the subject’s foot size.
The participants provided a signed written consent form, and the research ethics of human experiments was ensured by conducting the experiments within the contents approved by the Institutional Review Board of Korea University (IRB No. 2022-0399-01).
2.4. EMG Signal Processing
A fourth-order Butterworth bandpass filter (20 to 500 Hz) was initially applied to the raw EMG data. We then acquired the envelope function by calculating the waveform length (WL). The EMG WL was calculated as shown in the Equation (3) below:
where n is the current sample and N is the window size.
The EMG WL for the SL and TA muscles was divided into stance and swing phases by identifying the HC and TO events, which were obtained by applying a simple threshold on the ground reaction force obtained from the foot pressure insoles. The signals were normalized against the time axis such that the data could be represented as means and standard deviations (S.D.) across percentages of the gait phase. Because we needed to analyze the EMG WL data from the entire group, the EMG WL was further normalized against the maximum EMG WL value observed from the rollator-only gait condition. All data processing was performed using a custom-built MATLAB 2021a (Mathworks Inc., Natick, MA, USA) code.
3. Results
Prior to investigating the changes in muscle activation patterns elicited by the passive gait assist device, we needed to configure the ideal length of straps 1 and 2. For instance, if the difference between strap 1 and strap 2 is too small, tension will still reside in strap 2 even if the pulling angle of the elastic cord is high; this will cause plantar flexion torque to be present during the swing phase. For the opposite case, in which the difference between straps 1 and 2 is large, dorsiflexion torque will be applied during the late stance stage. This was confirmed by our simulation as seen in Figure 3a. The two black lines represent HO and TO during the gait cycle. The red lines represent the total pulling force by the elastic cord and the blue and green lines represent the tension present in straps 1 and 2, respectively. As seen in the bottom left panel of Figure 3a, when strap 2 (90 mm) is relatively shorter than strap 1 (160 mm), there is a significant amount of tension in strap 2 prior to HO. Also, in the top right panel, when strap 2 (130 mm) is comparable in length to strap 1 (140 mm), we observe plantar flexion torque after TO. Thus, our simulation results suggest that the optimal lengths are 160 mm and 110 mm for straps 1 and 2, respectively, with the base of the triangle being 150 mm.
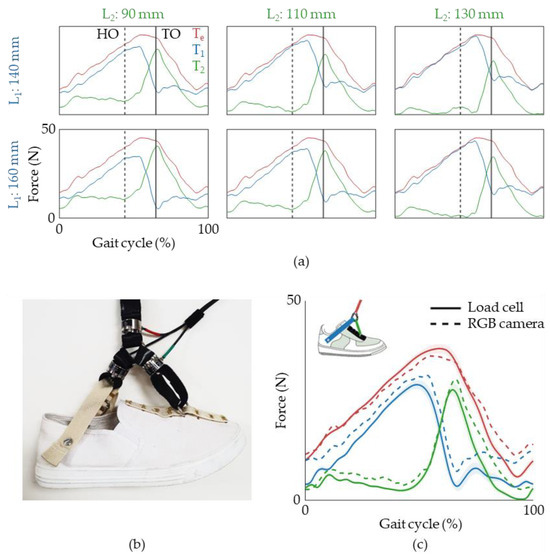
Figure 3.
Force profiles of the passive gait assist device. (a) Simulation of the tension that resides in the elastic cord and straps 1 and 2. HO and TO represent heel-off and toe-off, respectively. (b) Image of load cells attached to the specialized shoe. (c) Data from load cells (solid lines) are plotted with simulated data (dashed lines).
Once we had selected the lengths for straps 1 and 2, we verified whether the simulated tension profiles were indeed what was present in the straps during the gait cycle. We attached three load cells to our system, one at the end of the elastic cord and one on each strap (Figure 3b). We note that the lengths were adjusted such that the length of the strap was 160 mm and 110 mm for straps 1 and 2, including the load cell length. We found that the force profiles obtained from the load cells (Figure 3c, solid lines) and those from the simulated data (Figure 3b, dashed lines) qualitatively matched well with one another. Thus, with our system parameters, we can assert that plantar flexion torque is provided during the late stance and dorsiflexion torque is present during the swing phase.
The next question one might ask is whether this system actually assists the user during gait. It is common for gait-assistive devices to impede the user’s natural gait patterns. The goal is to reduce the amplitude of the EMG signals while maintaining the overall patterns. We evaluated the patterns of two lower-limb muscles (TA and SL) that have well-documented functions during gait. The EMG WL patterns during rollator walking (Figure 4a, black lines) and passive gait assist device-assisted gait (Figure 4a, red lines) qualitatively match each other well. More importantly, we observed a decrease in dorsiflexor EMG WL during the swing phase and the plantar flexor EMG WL during the late stance phase. This agrees well with the initial objective of our system. We went further and analyzed the average EMG WL for SL and TA for the stance and swing phases, respectively (Figure 4b). The results suggest that this effect is not confined to one subject but instead seen across the participant group.
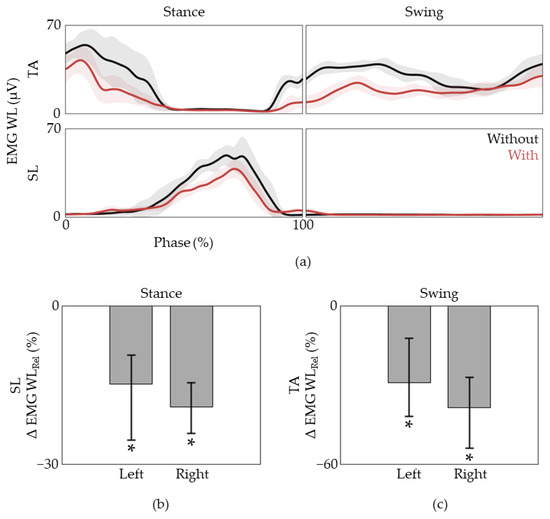
Figure 4.
SL and TA EMG WL analysis during gait. (a) Typical pattern of the SL and TA EMG WL during the stance and swing phases. The mean and S.D. are plotted as a line and shaded area, respectively. (b) The relative difference in SL EMG WL during the stance phase and (c) the TA EMG WL during the swing phase for all subjects. Data are presented as the median (25%, 75%), * p < 0.05, assessed using the Wilcoxon signed-rank test.
4. Discussion
In this study, we present a passive gait assist device that can be attached to a conventional rollator. Our device assists the user’s natural muscular activities, which in turn results in trajectory assistance because the force pulls from the front of the user. This is a considerable improvement when compared to traditional rollators where it is common for the user to drag their feet. Furthermore, unlike rigid exoskeletons, our device allows for relatively free movement in space. This may in turn result in a safer gait rehabilitation environment. We provided both simulated and empirical, via load cells, force profiles that reside within the elastic cord, strap 1, and strap 2. The analysis of EMG data obtained from the SL and TA suggests that our device successfully reduces the lower limb demands without disrupting the user’s natural gait patterns.
While the configuration was not tested, our system is able to change the stiffness of the spring-bar system, the width at which the elastic cords are anchored, the spring constant of the elastic cord, and the length of strap 1 and strap 2. This suggests that this system is highly adjustable and can be set up according to the user’s needs. For instance, we would be able to lessen the elastic force as increases in the user’s lower limb functions occur. Also, because we can independently configure each limb, we believe that it is possible to aid stroke patients. Moreover, we would be able to adjust the length of strap 1 and strap 2 to provide more dorsiflexion torque during the swing phase for the afflicted limb.
There are some limitations that need to be addressed. The experiments were performed by community-dwelling elder adults without any gait impairments. In order to confirm that our passive gait assist device works in practice, further studies with gait-impaired populations such as bedridden, post-stroke, and post-surgery patients need to be conducted. Also, because our device attaches to a conventional rollator, it may be difficult to ambulate non-level surfaces. This hindrance could be inconvenient in real-world situations. Moreover, the EMG levels of only the SL and TA were examined. In order to assess lower-limb gait patterns, a more extensive investigation of the lower limb muscles when using our devices, such as the rectus femoris, vastus medialis, biceps femoris, and gluteus maximus, should be performed.
By comparing the SL and TA EMG patterns during gait with the passive gait assist system with that of rollator gait conditions, we were able to observe that, at least for the tibia muscles, the overall patterns were similar. While conserved, we observed decreases in SL during the stance phase and TA during the swing phase, which is where the respective muscles are active. This decrease in tibia muscle demand should benefit subjects with weakened lower limb functions to perform gait without the help of a physiotherapist. This would allow for more frequent training, as resources are limited, which would in turn result in higher rehabilitative efficacy.
Author Contributions
Conceptualization, J.K., N.K. and S.-J.K.; methodology, J.K., S.K. and S.P.; software, Y.K. and J.M.; validation, J.K., Y.K., S.K. and S.-J.K.; formal analysis, J.K.; investigation, Y.K.; resources, S.-J.K.; data curation, J.K. and Y.K.; writing—original draft preparation, J.K.; writing—review and editing, J.K. and S.-J.K.; visualization, Y.K. and J.M.; supervision, S.-J.K.; project administration, S.-J.K.; funding acquisition, S.-J.K. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Korea Medical Device Development Fund grant funded by the Korean government (the Ministry of Science and ICT, the Ministry of Trade, Industry and Energy, the Ministry of Health and Welfare, and the Ministry of Food and Drug Safety) (project number: 1711138408, RS-2020-KD000189) and the Intramural Program (project no. K1804361) of Korea University.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Korea University (IRB No. 2022-0399-01 on 26 December 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 Guidelines on Physical Activity and Sedentary Behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide Trends in Insufficient Physical Activity from 2001 to 2016: A Pooled Analysis of 358 Population-Based Surveys with 1.9 Million Participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef] [PubMed]
- Campos, A.; Cortés, E.; Martins, D.; Ferre, M.; Contreras, A. Development of a Flexible Rehabilitation System for Bedridden Patients. J. Braz. Soc. Mech. Sci. Eng. 2021, 43, 361. [Google Scholar] [CrossRef]
- Cardoso, R.; Parola, V.; Neves, H.; Bernardes, R.A.; Duque, F.M.; Mendes, C.A.; Pimentel, M.; Caetano, P.; Petronilho, F.; Albuquerque, C.; et al. Review Physical Rehabilitation Programs for Bedridden Patients with Prolonged Immobility: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 6420. [Google Scholar] [CrossRef] [PubMed]
- Wall, B.T.; Dirks, M.L.; Van Loon, L.J.C. Skeletal Muscle Atrophy during Short-Term Disuse: Implications for Age-Related Sarcopenia. Ageing Res. Rev. 2013, 12, 898–906. [Google Scholar] [CrossRef]
- Memme, J.M.; Slavin, M.; Moradi, N.; Hood, D.A. Mitochondrial Bioenergetics and Turnover during Chronic Muscle Disuse. Int. J. Mol. Sci. 2021, 22, 5179. [Google Scholar] [CrossRef]
- Bao, W.; Yang, J.; Li, M.; Chen, K.; Ma, Z.; Bai, Y.; Xu, Y. Prevention of Muscle Atrophy in ICU Patients without Nerve Injury by Neuromuscular Electrical Stimulation: A Randomized Controlled Study. BMC Musculoskelet. Disord. 2022, 23, 780. [Google Scholar] [CrossRef]
- Wei, S.; Nguyen, T.T.; Zhang, Y.; Ryu, D.; Gariani, K. Sarcopenic Obesity: Epidemiology, Pathophysiology, Cardiovascular Disease, Mortality, and Management. Front. Endocrinol. 2023, 14, 1185221. [Google Scholar] [CrossRef]
- Qiao, Y.S.; Chai, Y.H.; Gong, H.J.; Zhuldyz, Z.; Stehouwer, C.D.A.; Zhou, J.B.; Simó, R. The Association Between Diabetes Mellitus and Risk of Sarcopenia: Accumulated Evidences From Observational Studies. Front. Endocrinol. 2021, 12, 782391. [Google Scholar] [CrossRef]
- Kuo, A.D.; Donelan, J.M. Dynamic Principles of Gait and Their Clinical Implications. Phys. Ther. 2010, 90, 157–174. [Google Scholar] [CrossRef]
- Gassert, R.; Dietz, V. Rehabilitation Robots for the Treatment of Sensorimotor Deficits: A Neurophysiological Perspective. J. Neuroeng. Rehabil. 2018, 15, 46. [Google Scholar] [CrossRef] [PubMed]
- Tang, X.; Wang, X.; Ji, X.; Zhou, Y.; Yang, J.; Wei, Y.; Zhang, W. A Wearable Lower Limb Exoskeleton: Reducing the Energy Cost of Human Movement. Micromachines 2022, 13, 900. [Google Scholar] [CrossRef] [PubMed]
- Banala, S.; Agrawal, S.; Scholz, J. Robot assisted gait training with active leg exoskeleton (ALEX). IEEE Trans. Neur. Syst. Rehab. Eng. 2009, 17, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Bernhardt, M.; Frey, M.; Colombo, G.; Riener, R. Hybrid force-position control yields cooperative behaviour of the rehabilitation robot LOKOMAT. In Proceedings of the 9th International Conference on Rehabilitation Robotics, Chicago, IL, USA, 28 June–1 July 2005; pp. 536–539. [Google Scholar]
- Farris, R.J.; Quintero, H.A.; Goldfarb, M. Preliminary Evaluation of a Powered Lower Limb Orthosis to Aid Walking in Paraplegic Individuals. IEEE Trans. Neural Syst. Rehabil. Eng. 2011, 19, 652–659. [Google Scholar] [CrossRef] [PubMed]
- Zeilig, G.; Weingarden, H.; Zwecker, M.; Dudkiewicz, I.; Bloch, A.; Esquenazi, A. Safety and Tolerance of the ReWalkTM Exoskeleton Suit for Ambulation by People with Complete Spinal Cord Injury: A Pilot Study. J. Spinal Cord Med. 2012, 35, 96–101. [Google Scholar] [CrossRef] [PubMed]
- Gancet, J.; Ilzkovitz, M.; Motard, E.; Nevatia, Y.; Letier, P.; de Weerdt, D.; Cheron, G.; Hoellinger, T.; Seetharaman, K.; Petieau, M.; et al. MINDWALKER: Going one step further with assistive lower limbs exoskeleton for SCI condition subjects. In Proceedings of the 4th IEEE RAS EMBS International Conference on Biomedical Robotics and Biomechatronics (BioRob), Rome, Italy, 24–27 June 2012; pp. 1794–1800. [Google Scholar]
- Shi, D.; Zhang, W.; Zhang, W.; Ding, X. A Review on Lower Limb Rehabilitation Exoskeleton Robots. Chin. J. Mech. Eng. (Engl. Ed.) 2019, 32, 74. [Google Scholar] [CrossRef]
- De Luca, A.; Bellitto, A.; Mandraccia, S.; Marchesi, G.; Pellegrino, L.; Coscia, M.; Leoncini, C.; Rossi, L.; Gamba, S.; Massone, A.; et al. Exoskeleton for Gait Rehabilitation: Effects of Assistance, Mechanical Structure, and Walking Aids on Muscle Activations. Appl. Sci. 2019, 9, 2868. [Google Scholar] [CrossRef]
- Hornby, T.G.; Campbell, D.D.; Kahn, J.H.; Demott, T.; Moore, J.L.; Roth, H.R. Enhanced Gait-Related Improvements after Therapist- versus Robotic-Assisted Locomotor Training in Subjects with Chronic Stroke: A Randomized Controlled Study. Stroke 2008, 39, 1786–1792. [Google Scholar] [CrossRef]
- Hidler, J.; Nichols, D.; Pelliccio, M.; Brady, K.; Campbell, D.D.; Kahn, J.H.; Hornby, T.G. Multicenter Randomized Clinical Trial Evaluating the Effectiveness of the Lokomat in Subacute Stroke. Neurorehabil. Neural Repair. 2009, 23, 5–13. [Google Scholar] [CrossRef]
- Pennycott, A.; Wyss, D.; Vallery, H.; Klamroth-Marganska, V.; Riener, R. Towards more effective robotic gait training for stroke rehabilitation: A review. J. Neuroeng. Rehabil. 2012, 9, 65. [Google Scholar] [CrossRef]
- Androwis, G.J.; Pilkar, R.; Ramanujam, A.; Nolan, K.J. Electromyography Assessment during Gait in a Robotic Exoskeleton for Acute Stroke. Front. Neurol. 2018, 9, 630. [Google Scholar] [CrossRef]
- Kim, J.; Kim, Y.; Kim, S.J. Biomechanical Task-Based Gait Analysis Suggests ReWalk Gait Resembles Crutch Gait. Appl. Sci. 2022, 12, 2574. [Google Scholar] [CrossRef]
- Swank, C.; Wang-Price, S.; Gao, F.; Almutairi, S. Walking with a Robotic Exoskeleton Does Not Mimic Natural Gait: A within-Subjects Study. JMIR Rehabil. Assist. Technol. 2019, 6, e11023. [Google Scholar] [CrossRef] [PubMed]
- Haufe, F.L.; Kober, A.M.; Wolf, P.; Riener, R.; Xiloyannis, M. Learning to Walk with a Wearable Robot in 880 Simple Steps: A Pilot Study on Motor Adaptation. J. Neuroeng. Rehabil. 2021, 18, 157. [Google Scholar] [CrossRef] [PubMed]
- Martini, E.; Crea, S.; Parri, A.; Bastiani, L.; Faraguna, U.; McKinney, Z.; Molino-Lova, R.; Pratali, L.; Vitiello, N. Gait Training Using a Robotic Hip Exoskeleton Improves Metabolic Gait Efficiency in the Elderly. Sci. Rep. 2019, 9, 7157. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, A.; Vreede, K.S.; Häglund, V.; Kawamoto, H.; Sankai, Y.; Borg, J. Gait training early after stroke with a new exoskeleton–the hybrid assistive limb: A study of safety and feasibility. J. NeuroEng. Rehabil. 2014, 11, 92. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Kim, J.; Lim, B.; Lee, H.J.; Kim, Y.H. Exercise with a Wearable Hip-Assist Robot Improved Physical Function and Walking Efficiency in Older Adults. Sci. Rep. 2023, 13, 7269. [Google Scholar] [CrossRef] [PubMed]
- Park, G.M.; Cho, S.H.; Hong, J.T.; Kim, D.H.; Shin, J.C. Effects and Safety of Wearable Exoskeleton for Robot-Assisted Gait Training: A Retrospective Preliminary Study. J. Pers. Med. 2023, 13, 676. [Google Scholar] [CrossRef] [PubMed]
- Dijkers, M.P.; Akers, K.G.; Dieffenbach, S.; Galen, S.S. Systematic Reviews of Clinical Benefits of Exoskeleton Use for Gait and Mobility in Neurologic Disorders: A Tertiary Study. Arch Phys. Med. Rehabil. 2021, 102, 300–313. [Google Scholar] [CrossRef] [PubMed]
- Haufe, F.L.; Schmidt, K.; Duarte, J.E.; Wolf, P.; Riener, R.; Xiloyannis, M. Activity-Based Training with the Myosuit: A Safety and Feasibility Study across Diverse Gait Disorders. J. Neuroeng. Rehabil. 2020, 17, 135. [Google Scholar] [CrossRef]
- Wang, Z.; Yang, C.; Ding, Z.; Yang, T.; Guo, H.; Jiang, F.; Tian, B. Study on the Control Method of Knee Joint Human–Exoskeleton Interactive System. Sensors 2022, 22, 1040. [Google Scholar] [CrossRef]
- Asbeck, A.T.; Schmidt, K.; Galiana, I.; Wagner, D.; Walsh, C.J. Multi-Joint Soft Exosuit for Gait Assistance. In Proceedings of the 2015 IEEE International Conference on Robotics and Automation (ICRA), Seattle, WA, USA, 26–30 May 2015; pp. 6197–6204. [Google Scholar]
- Awad, L.N.; Esquenazi, A.; Francisco, G.E.; Nolan, K.J.; Jayaraman, A. The ReWalk ReStoreTM Soft Robotic Exosuit: A Multi-Site Clinical Trial of the Safety, Reliability, and Feasibility of Exosuit-Augmented Post-Stroke Gait Rehabilitation. J. Neuroeng. Rehabil. 2020, 17, 80. [Google Scholar] [CrossRef] [PubMed]
- Xiloyannis, M.; Alicea, R.; Georgarakis, A.M.; Haufe, F.L.; Wolf, P.; Masia, L.; Riener, R. Soft Robotic Suits: State of the Art, Core Technologies, and Open Challenges. IEEE Trans. Robot. 2022, 38, 1343–1362. [Google Scholar] [CrossRef]
- Collins, S.H.; Bruce Wiggin, M.; Sawicki, G.S. Reducing the Energy Cost of Human Walking Using an Unpowered Exoskeleton. Nature 2015, 522, 212–215. [Google Scholar] [CrossRef]
- Zhang, B.; Liu, T.; Zhang, B.; Pecht, M.G. Recent Development of Unpowered Exoskeletons for Lower Extremity: A Survey. IEEE Access 2021, 9, 138042–138056. [Google Scholar] [CrossRef]
- Zhou, T.; Xiong, C.; Zhang, J.; Chen, W.; Huang, X. Regulating Metabolic Energy among Joints during Human Walking Using a Multiarticular Unpowered Exoskeleton. IEEE Trans. Neural Syst. Rehabil. Eng. 2021, 29, 662–672. [Google Scholar] [CrossRef]
- Xie, L.; Huang, G.; Huang, L.; Cai, S.; Li, X. An Unpowered Flexible Lower Limb Exoskeleton: Walking Assisting and Energy Harvesting. IEEE/ASME Trans. Mechatron. 2019, 24, 2236–2247. [Google Scholar] [CrossRef]
- Etenzi, E.; Borzuola, R.; Grabowski, A.M. Passive-Elastic Knee-Ankle Exoskeleton Reduces the Metabolic Cost of Walking. J. Neuroeng. Rehabil. 2020, 17, 104. [Google Scholar] [CrossRef]
- Barazesh, H.; Sharbafi, M.A. A Biarticular Passive Exosuit to Support Balance Control Can Reduce Metabolic Cost of Walking. Bioinspir. Biomim. 2020, 15, 036009. [Google Scholar] [CrossRef]
- Perry, J.; Davids, J.R. Gait analysis: Normal and pathological function. J. Pediatr. Orthop. 1992, 12, 815. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).