1. Introduction
Contemporary business environments are becoming more volatile, which can be explained by the turbulent and unpredictable environments in which organizations operate [
1]. The discussion of whether organizations must focus on implementing paradigms and enhancing their capabilities to better adapt to unexpected circumstances started in the early 1990s [
2]. The concept of agility emerged in this discussion as a proposed solution for responding rapidly to unexpected changes.
As a global construct definition, agility is defined as an entity’s ability to respond and react to environmental changes in a rapid and effective manner [
3]. However, the discussion on agility constructs has its foundations in the manufacturing industry. The first agility construct in the management field came from the IACOCCA Institute of Lehigh University, where agile manufacturing was defined as the new emerging manufacturing paradigm that would replace mass production and depicted the common infrastructure needed for agile manufacturing enterprises [
4]. This work was later expanded by Goldman, Nagel, and Preiss [
5], where the definition of agile competitors expanded to general organizations and enterprises of any field. Organizational agility was originally defined as a manufacturing system paradigm with capabilities to meet the rapidly changing needs of the marketplace [
6]. Sharifi and Zhang [
7] expanded on this definition and elaborated a theoretical model for organizational agility, focusing on four dimensions: responsiveness, competency, flexibility, and speed. Researchers have studied this model with structured questionnaires to evaluate organizational agility in service sectors outside of manufacturing [
8,
9].
Despite the focus on organizational agility, the paradigm slowly shifted to other organizational aspects, such as workforce agility. Breu et al. [
10] applied the dimensions of organizational agility to an empirical study of the agile characteristics of the workforce. Their empirical investigation focused on five dimensions of this construct: intelligence, competency, collaboration, culture, and information systems. The workforce agility construct was then defined, and Sherehiy et al. [
2] developed a widely accepted theoretical model that included three dimensions: proactivity, adaptability, and resilience. A later systematic literature from Salmen and Festing [
11] found 31 relevant instruments used to study workforce agility, with 13 scales based on Sherehiy et al. [
2]. This workforce agility model has also seen applications in service industries such as education [
12]. A recent model from Petermann and Zacher [
13] includes ten aggregated dimensions from an extensive literature revision on workforce agility: accepting changes, decision-making, creating transparency, collaboration, reflection, user-centricity, iteration, testing, self-organization, and learning. This model resulted in a more robust fit versus the three-dimensional model from Sherehiy et al. [
2] and the five-dimensional model of Braun et al. [
14]. Despite its successful results, the aggregated model for workforce agility needs further validation in new empirical studies in other sectors outside manufacturing [
15].
Other agility constructs stemming from dynamic capabilities have also been discussed. For example, agility has been defined as an organizational capability for efficiently and effectively redistributing resources to value-creating and value-protecting higher-yield activities despite internal or external challenges [
16]. Following this paradigm shift to capability, other agility constructs have emerged. Agility has also been examined in the context of supply chains, where supply chain agility was argued to be a firm’s supply chain ability to competently counter market changes and satisfy customer demands [
17]. However, there is a lack of consensus on the above definitions and the respective construct dimensions and enablers [
18,
19]. As with the previous cases of agility constructs, the lack of validations calls for more empirical investigations.
Some other agility constructs have been proposed in the literature, such as business agility, operational agility, strategic agility, leadership agility, and customer agility, among others [
20]. While such efforts allowed the development of multiple construct definitions and new questionnaires to assess agility better [
20], research in agility has been fragmented, with a lack of consensus on its definitions [
21] and the need for establishing construct validity [
22]. Finally, agility research has primarily concentrated on manufacturing, leaving broad opportunities to explore these constructs in other industries, such as healthcare, which faces many uncertainties and challenges [
23].
In the case of healthcare, Goldman and Graham [
24] describe agility as “the capability to coordinate quickly and efficiently all of the physically and organizationally distributed resources required to create, produce, deliver, and support a constantly changing mix of goods and services” [
24] (p. 1). Agility is essential in the healthcare sector due to its critical nature and strong relationship with organizational performance, such as medical treatment effectiveness and better healthcare outcomes [
25]. While the importance of developing agility in healthcare organizations is well established [
26,
27], previous studies have revealed similar issues that the implementation of agility faces in the manufacturing sector, including multiple construct development, lack of definition consensus, and a need for the validation of existing models and survey questionnaires [
23]. The above gaps in the literature highlight the need for more empirical studies on agility in the healthcare sector [
15,
28]. A synthesis of the existing constructs and definitions of agility should help reduce agility research fragmentation [
21] and identify potential constructs that could be replicated in multiple healthcare organizations. It will also identify the key dimensions associated with the agility construct, which is critical prior to establishing an agility measurement system [
29]. Hence, this systematic literature review focuses on the published empirical studies of agility in the healthcare industry.
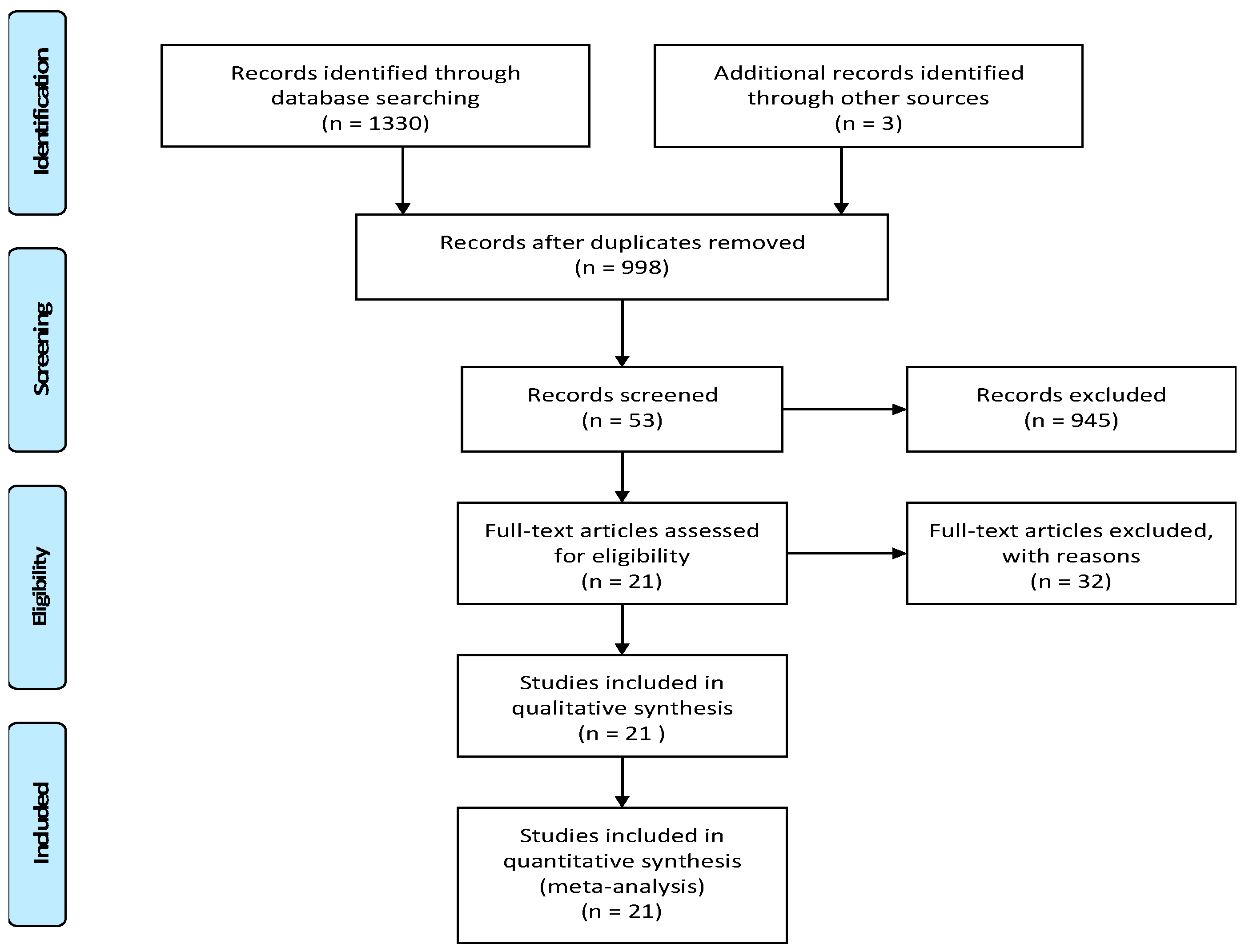
The present study reviewed the agility studies conducted in the healthcare sector with the following main objectives: (1) identify agility constructs applied within the healthcare sector, (2) examine the instruments employed in empirical studies to evaluate agility within healthcare settings, and (3) assess the constructs related to agility in the context of healthcare. This review employed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) to ensure the reliability of the study results. PRISMA consists of a 27-item list and a four-phase flow diagram that help improve the reporting of systematic reviews [
30].
3. Results
Table 2 displays the results of the literature search, presenting a total of 21 articles. The columns in the table compile the extracted information from each paper, facilitating the analysis of their relevance in addressing the research questions posed in this literature review.
Agility within the context of healthcare organizations is a relatively new and promising area of study that holds potential for further development.
Figure 2 illustrates the distribution of the 21 selected articles by their publication year. The oldest publication in this set dates to 2012, while the years 2018, 2019, 2020, and 2022 stand out with the highest number of publications. This increase in publications during these years can be attributed to the initial definition of the term in 1991 [
4] and the subsequent slow adoption of agility concepts within the healthcare industry, which gained momentum in the early 2010s.
Likewise,
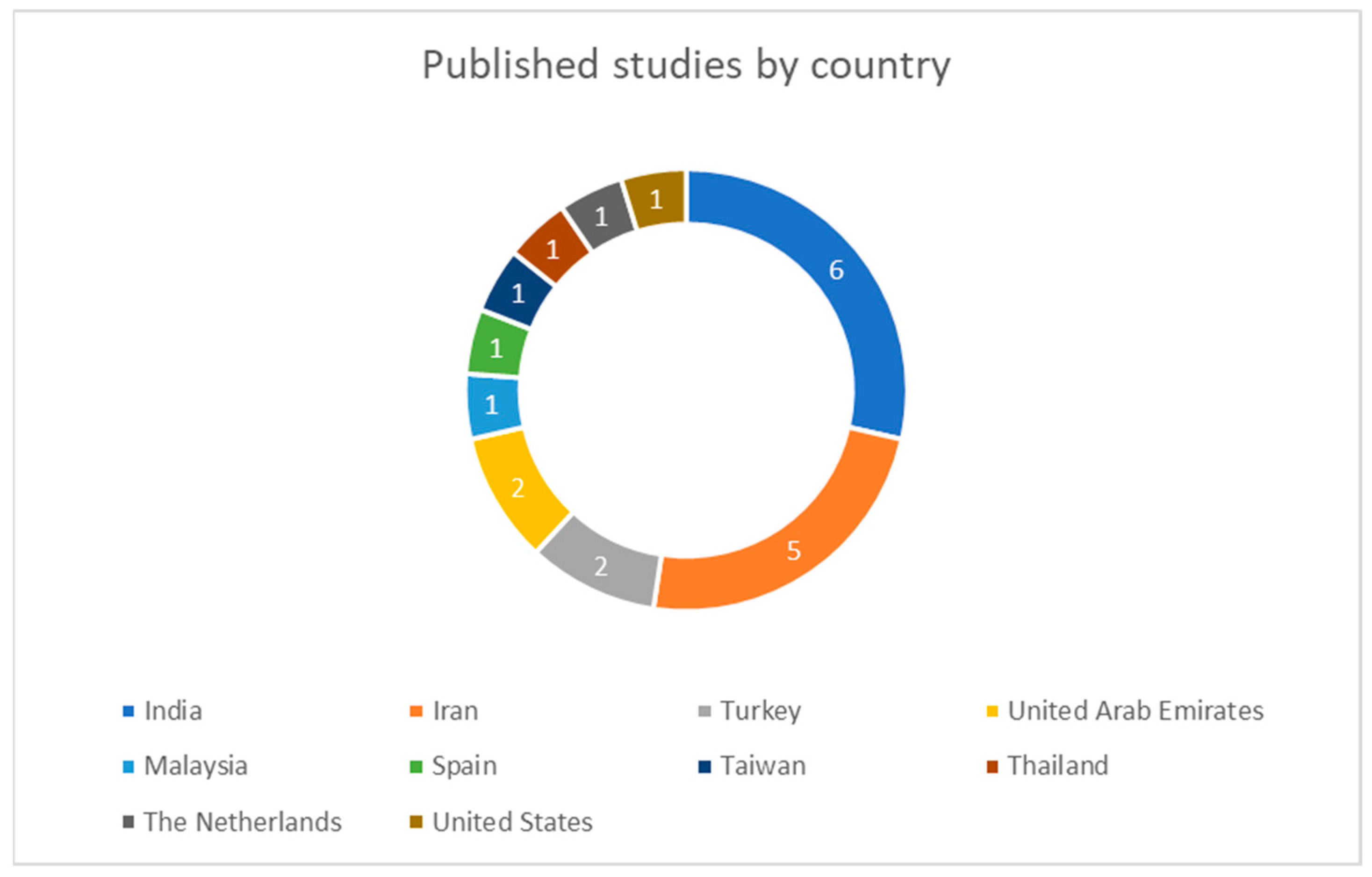
Figure 3 provides an overview of the global distribution of the study locations. Researchers have conducted empirical investigations on agility in the healthcare sector using questionnaires in 10 different countries. Notably, Iran and India have the highest number of questionnaire-based publications, with six and five publications, respectively. Next, the United Arab Emirates and Turkey each have two studies. The remaining countries have contributed only one study each.
Table 3 presents a list of the healthcare organizations where the authors chose to collect data in each study. The authors used a mix of different institutions and did not consistently report the specific types of hospitals or clinics they visited. Nine studies collected data from hospitals, six studies collected data from diverse healthcare organizations, two studies collected data from teaching hospitals, two studies collected data from emergency centers, one study collected data from tertiary care hospitals, and one from intensive care units.
In terms of funding type, five studies included only private institutions, four studies included public institutions, and two studies included both private and public institutions. Ten studies did not specify the institution funding type.
The participants selected for the studies were divided into two groups: medical personnel and administrative staff. Six studies obtained responses from medical personnel, six other studies obtained responses from administrative staff, and the remaining nine studies obtained responses from both medical and administrative staff. The study sample size ranged from 90 to 581 participants.
The authors of the published studies employed various terms to describe the different levels of agility capabilities that healthcare organizations may possess. Some studies have used the terms healthcare agility and hospital agility, but these constructs lack clear definitions. Furthermore, the questionnaires utilized to assess these constructs often originate from more well-defined concepts, such as organizational agility and supply chain agility.
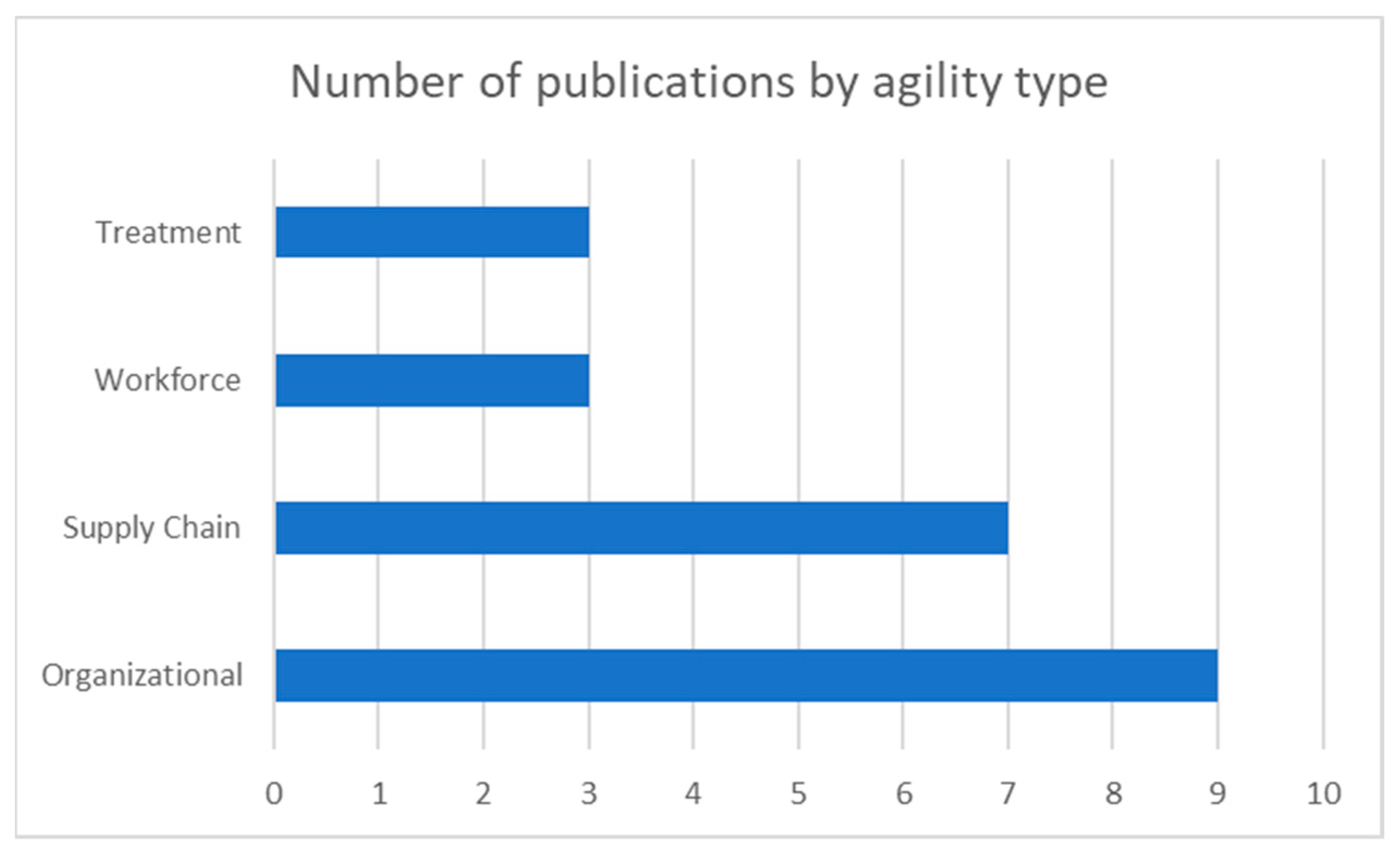
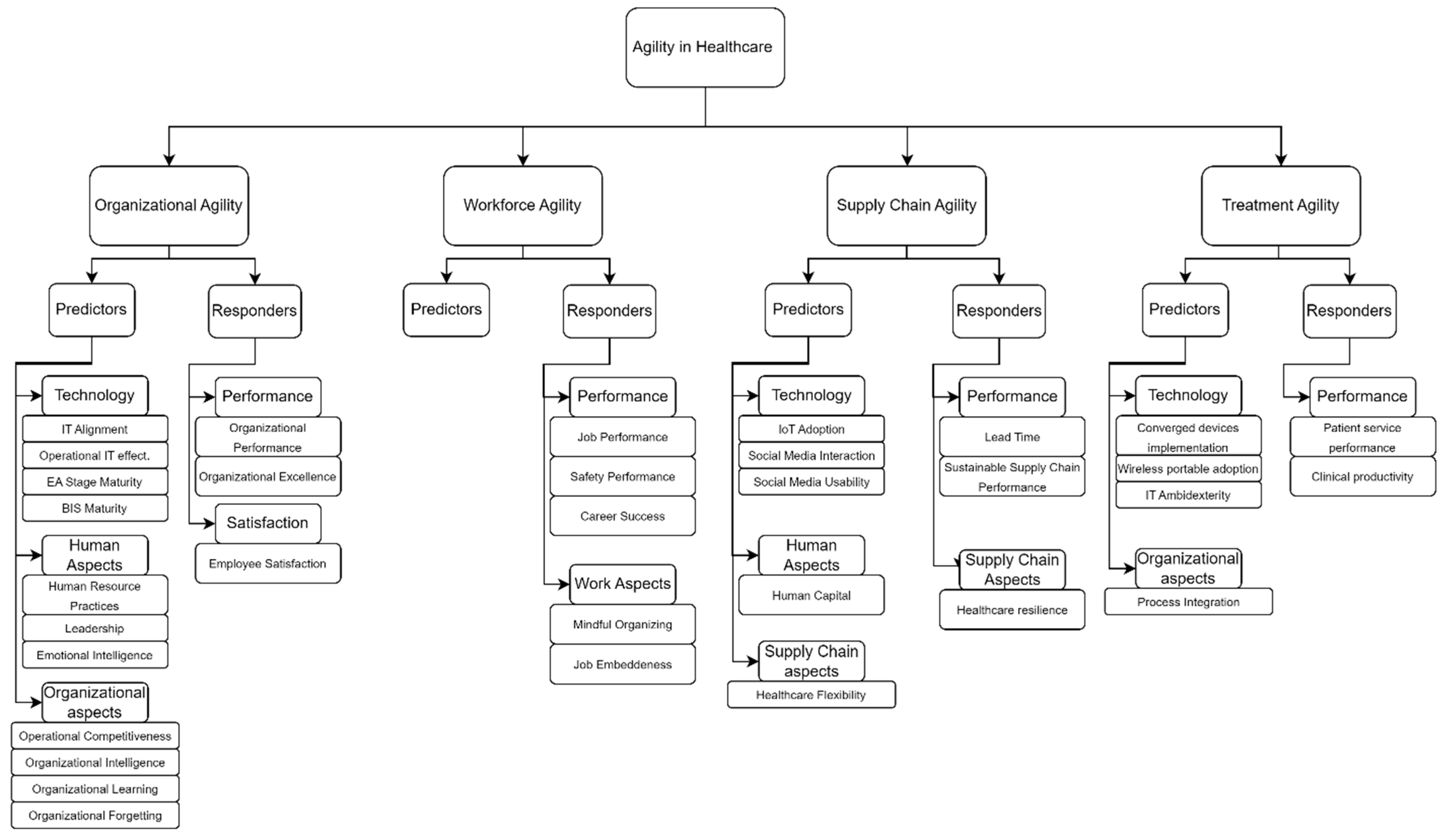
Figure 4 presents an initial quantitative overview of the clustered agility constructs. Among these constructs, organizational agility and supply chain agility emerged as the most frequently studied capabilities within healthcare organizations. This descriptive analysis provides insights into which agility constructs have received the most attention from researchers in the healthcare industry.
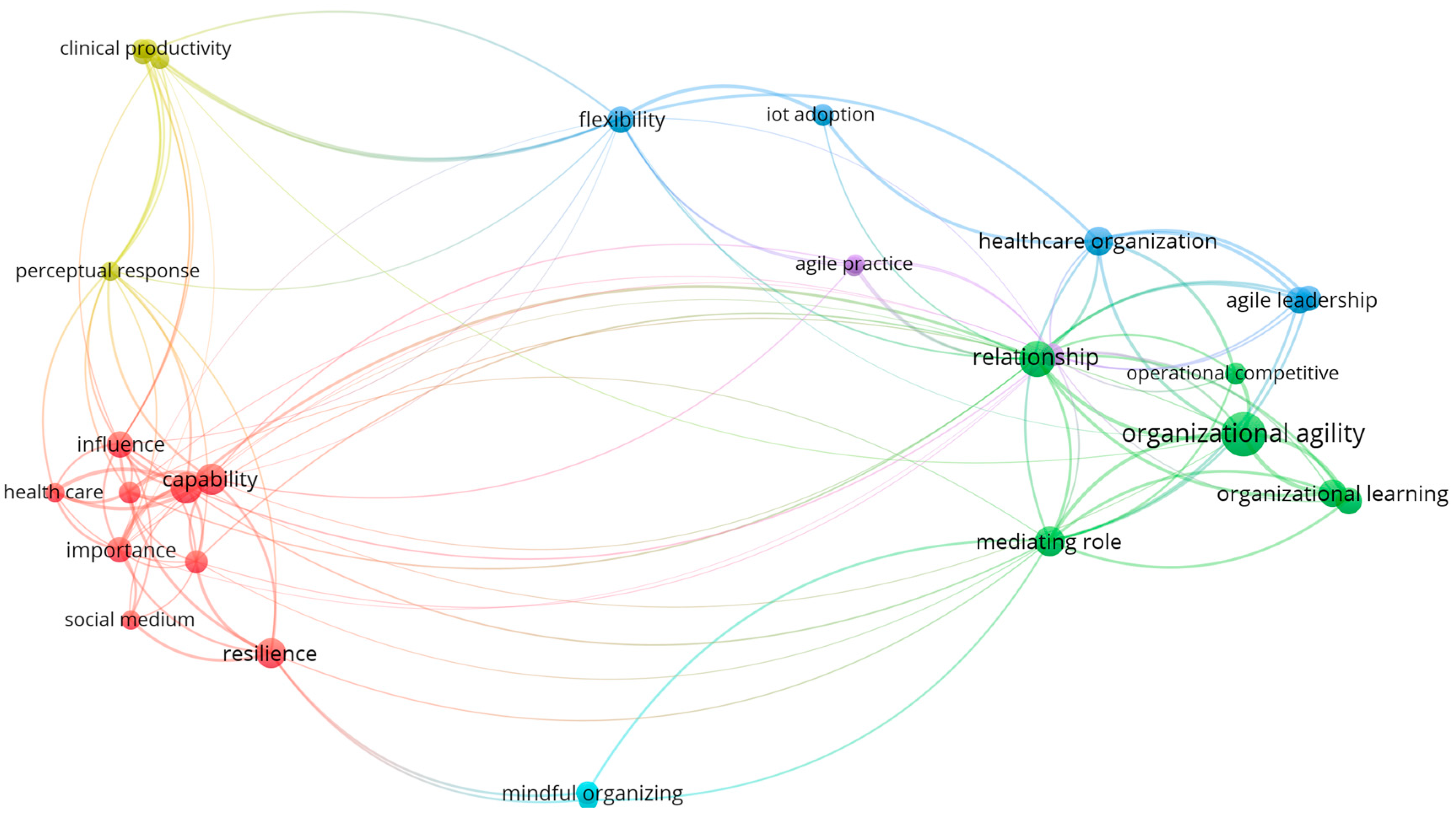
Figure 5 depicts a co-occurrence map of the terms found in the titles and abstracts of the 21 selected papers. In this visualization, nodes represent individual terms, with their sizes reflecting their frequency, and the links indicate co-occurrence patterns. Clusters of the same color group together terms that frequently co-occur.
Figure 5 highlights two primary clusters of terms: the red and green clusters. The red cluster comprises nine terms with the highest co-occurrences, including capability, healthcare, healthcare agility, human capital, resilience, and moderating role. The green cluster represents the second-largest group of co-occurring terms, including terms such as organizational agility, organizational learning, mediating role, relationship, and operational competitive capability. A third blue cluster encompasses relevant terms such as healthcare organization, agile leadership, flexibility, and IoT adoption.
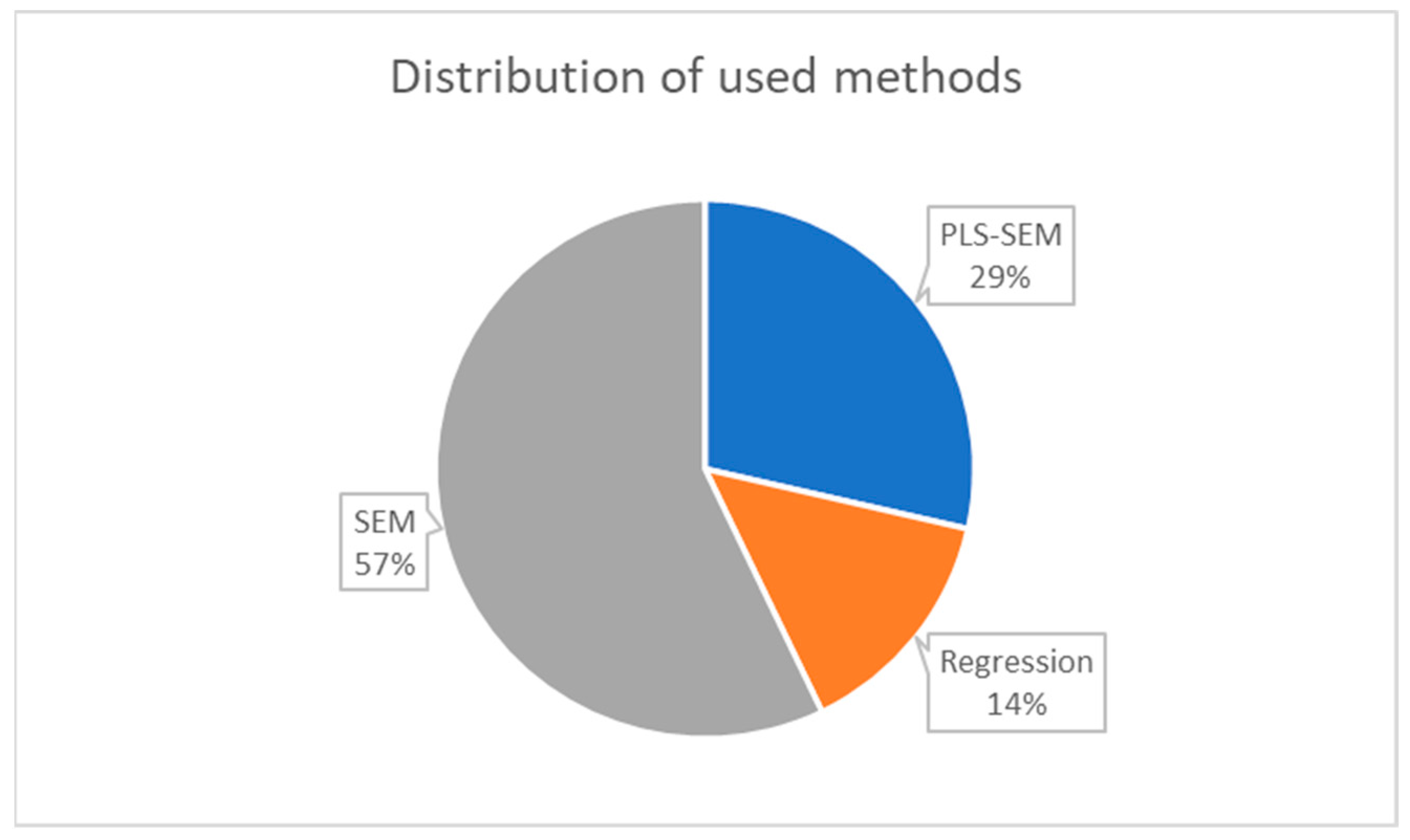
Three main statistical methods have been used to evaluate the questionnaire responses: structural equation modeling (SEM), partial least squares structural equation modeling (PLS-SEM), and multiple regression analysis (regression).
Figure 6 illustrates the distribution of their usage frequencies in the selected papers. SEM was the most preferred statistical method employed in 57% (12 out of 21) of the articles in this systematic review. PLS-SEM was the second preferred method, used in 29% (6 out of 21) papers. Lastly, the selected articles used regression analysis in 14% of cases (3 out of 21).
4. Research Findings
This section addresses the three research questions by examining each of the studies included in the literature review. The section is organized into three subsections: agility constructs, agility instruments, and agility dimensions.
4.1. Agility Constructs
The agility concepts in the 21 articles selected for this study defined agility using multiple constructs. To simplify the analysis, this study grouped the agility constructs into four clusters, as listed in
Table 4: organizational agility, workforce agility, supply chain agility, and treatment agility. Note that one article [
34] looked at two clustered constructs of agility, which were included in both the organizational and supply chain agility constructs.
4.1.1. Organizational Agility
The construct of organizational agility is the most frequently studied clustered construct in the reviewed papers, with a total of nine published studies authored by various researchers. Specifically, seven publications employed organizational agility, while two other publications used relevant definitions for hospital agility and enterprise agility.
Seven publications defined the construct of organizational agility. Bahrami et al. [
8] describe it as the ability to respond quickly and successfully to environmental changes. A similar definition is provided by Kavosi et al. [
9], emphasizing that organizations must adopt an organizational agility paradigm to maintain competitiveness and adapt to change.
Melián-Alzola et al. [
55] discussed organizational agility as a crucial management criterion in hospital units, highlighting its role in responding rapidly and flexibly to changes. Pazhouhan et al. [
57] stress the importance of agility in healthcare organizations, considering their critical mission in maintaining community health and well-being.
Shakhour et al. [
62] incorporate various definitions of organizational agility, proposing it as a key business enabler for competitiveness. They emphasize the role of organizational agility as a sense–response process involving sensing potential threats, real-time decision-making, and responsive actions to mitigate these threats.
Akkaya and Mertz [
37] suggest that organizational agility arises from proactive actions, the rapid implementation of flexible business processes, and effective organizational coordination. Shen et al. [
64] underline the significance of rapid and accurate decision-making processes in achieving organizational agility. They also developed a model to explore the impact of business information system maturity as a hospital agility enabler.
Hospital agility is closely related to the previously discussed organizational agility. Abdi et al. [
34] regard agility as a crucial business capability for hospitals. They emphasize its importance for medical treatments, highlighting that hospital organizations need a dynamic structure capable of adapting to potential changes in the industry’s environment. This concept is closely tied to organizational agility, as the authors define their latent construct as a business capability.
Finally, one selected paper focused on the construct of enterprise agility. Bradley et al. [
40] define enterprise agility as an organization’s capacity to sense changes in the environment and respond promptly to them, driven by information technologies. Considering this definition and that enterprises typically denote lucrative organizations, this review incorporated the term “enterprise agility” into the construct of organizational agility.
Based on the above review, it can be concluded that organizational agility has a solid foundation in its definition and applications. Nonetheless, there are still a few similar terms associated with it. In the healthcare sector, organizational agility refers to an organization’s dynamic capability, regardless of its size, to promptly sense and respond to changes and uncertainties.
4.1.2. Workforce Agility
In line with the dynamic capability framework introduced by Teece et al. [
16], Saleem et al. [
60] offered an interpretation of workforce agility as contingent on employees’ agile behaviors. They further deconstruct this construct into three distinct subdimensions, namely proactivity, adaptability, and resilience. Proactivity denotes the capacity for individuals to initiate actions in response to a dynamically changing environment. Adaptability encompasses the ability to modify one’s behavior to align with evolving circumstances. At the same time, resilience represents the aptitude to cope effectively with stressful events and recover from the most adverse situations [
60].
While the existing literature undeniably acknowledges and establishes a robust foundation for workforce agility, it is pertinent to consider two additional constructs within the healthcare context. This integrated construct synthesis amalgamates human resources agility and agile leadership notions with the overarching concept of workforce agility.
Goodarzi et al. [
49] initially examined this construct by referring to it as the organizational agility of human resources but subsequently terming it human resource agility. The authors emphasized the pivotal role of human resource agility in fostering organizational agility, emphasizing the need for internal agility enablers within the organization [
43]. While the study does not explicitly define the construct, it identifies five key dimensions of human resource agility: intelligence and awareness, competency, knowledge management, empowerment culture, and information systems.
More recently, Akkaya [
35] conducted a study exploring the influence of agile leadership on career performance success, focusing on the mediating role of job embeddedness. In this article, agile leadership is characterized as a set of strategies that impact career success in achieving desired outcomes [
37]. Agile leadership emerges from adopting employee-empowerment initiatives designed to address unpredictable working scenarios, establishing a clear link to workforce agility. The authors further deconstruct agile leadership into six key dimensions: result-oriented, teamwork-oriented, competency, flexibility, quickness, and change-oriented.
While there is a notable absence of extensive research, precise definitions, and consensus regarding the construct of workforce agility, all three authors approach agility as the capability of healthcare workers to effectively respond to changes in a timely manner. This perspective aligns with earlier definitions of agility explored within this review and sets the stage for a deeper examination of workforce agility in the healthcare sector. Within this study, workforce agility is defined as the dynamic capability of employees to promptly sense and respond to changes in their medical work environment and the evolving needs of their patients.
4.1.3. Supply Chain Agility
Supply chain agility was the subject of seven published empirical investigations, positioning it as the second most extensively studied agility construct within the healthcare context. Notably, while these studies employed different construct names to refer to this latent variable, they consistently share foundational similarities in their definitions. Researchers often interchangeably refer to supply chain agility as hospital agility, agile practices in the supply chain, healthcare agility, and medical chain agility.
Abdi et al. [
34] expounded upon agility as the capacity of supply chains to swiftly respond to market fluctuations and customer demands. Similarly, Alzoubi et al. [
38] asserted that supply chain agility entails vigilance and rapid responsiveness. This involves practices like comprehensive information sharing among all stakeholders, enabling them to anticipate, identify, and exploit market opportunities. Given the imperative to address critical patient needs and intricate processes, the adoption of agile practices is strongly advocated within hospital supply chains [
38,
50].
Mandal [
50] offered a definition of healthcare agility as the capacity of healthcare supply chains to enhance the flow of patients through healthcare supply chains by delivering customized healthcare services rapidly. Five fundamental antecedents associated with supply chain agility encompass alertness, accessibility, decisiveness, swiftness, and flexibility [
50]. Additionally, healthcare agility has been characterized by the ability to concurrently excel in operational capabilities, encompassing quality, delivery, flexibility, and cost management, all orchestrated in a coordinated manner [
45]. Chakraborty et al. [
45] further underscored that healthcare agility can be gauged by an organization’s ability to promptly address patient needs and provide healthcare services during periods of market turbulence, even in the face of limited resources such as medical staff, instruments, and medications. This underscores the importance of supply chain considerations and the advantages of adopting the Internet of Things. Lastly, Rungsrisawat and Jermsittiparsert [
59] emphasized the significance of human capital in nurturing supply chain agility, a notion previously supported by Mandal [
50].
Mandal et al. [
25] also introduced the concept of medical chain agility, defining it as the dynamic capability of healthcare supply chains to respond to changes in patients’ treatment needs and provide rapid responses. Consequently, the construct of medical chain agility pertains to the capacity to deliver necessary healthcare services to patients promptly [
25].
Despite supply chain agility being the second most extensively examined construct in the literature, it exhibits a broader array of terminology compared to organizational agility. Curiously, none of the articles explicitly identify the latent variable in their model as supply chain agility, although their foundational concepts and construct definitions draw from the supply chain agility literature [
47]. This divergence underscores the absence of a consensus regarding this construct, thereby highlighting an opportunity for strengthening this latent variable. Building upon earlier definitions and within the context of healthcare, we propose the following definition for the supply chain agility construct: the capacity of supply chain members to adeptly sense and promptly respond to shifts within the healthcare industry and evolving patient needs.
4.1.4. Treatment Agility
Among the selected papers, three investigated the concept of treatment agility, wherein agility construct transitions from the organizational level to the process-entity level. Chakraborty and Mandal [
44] introduce the notion of care delivery agility, defining it as the degree to which clinicians exhibit proficiency in clinical diagnosis, enabling agile decision-making. The authors emphasize the critical importance of timely and accurate treatment within the modern healthcare ecosystem, where lives are at stake [
44]. Furthermore, treatment agility is regarded as a dynamic capability for healthcare organizations to enhance their competitive advantage, signifying an ability to adapt to volatile, dynamic, and constantly evolving service requirements [
48]. In a distinct vein, Van de Wetering et al. [
69] examined patient agility, characterizing it as a dynamic capability that empowers hospital departments to effectively sense and respond to patient needs. In the context of medical treatment, agility is centered on rapid adaptability and responsiveness to patient requirements.
4.2. Agility Instruments
This review extracted all the literature related to developing questionnaires/instruments used to measure the agility constructs in the healthcare industry. Through the 21 empirical studies collected in this literature review, only 4 publications [
8,
9,
57,
60] used existing questionnaires to study their respective agility constructs.
Table 5 summarizes these findings. These publications employed three questionnaires:
Organizational Agility questionnaire by Sharifi and Zhang [
7], which was used in [
8,
9];
Organizational Agility questionnaire by Spitzer [
58], which was used in [
57];
Workforce Agility questionnaire by Sherehiy and Karwowski [
61], which was used in [
60].
Among the remaining 17 studies, 13 publications formulated their questionnaires based on the existing literature. Meanwhile, three publications [
25,
34,
49] developed their questionnaires without providing background information, and one study [
38] did not report the questionnaire used. The subsequent tables (
Table 6,
Table 7,
Table 8 and
Table 9) serve as a concise summary of the literature referenced in the development of the questionnaires, categorized according to the clustered constructs outlined in
Table 4. Each table provides an overview of the dimensions incorporated by the respective authors in their questionnaires, along with citations referencing the sources employed.
When empirically assessing the organizational agility construct, researchers have generally considered four dimensions: responsiveness, competence, flexibility, and speed. This alignment was observed in the work of four authors [
8,
9,
34,
55]. However, Pazhouhan et al. [
57] offered a distinct perspective, evaluating organizational agility through three dimensions: total quality management, human resource management, and change management. Bradley et al. [
40] adopted a two-dimensional approach, focusing on market responsiveness and external relationship management. Meanwhile, Shakhour et al. [
62] subdivided organizational agility into two subdimensions, namely, sensing agility and acting agility, derived from a three-strategic task process encompassing sensing, decision-making, and acting. In their empirical investigation, Shakhour et al. [
62] found evidence supporting the existence of sensing agility (involving the detection and monitoring of events impacting the business environment) and responding agility (involving a series of actions taken in response to events in the business environment).
The construct of supply chain agility has garnered more empirical attention in healthcare than workforce agility. However, it is noteworthy that no single author has chosen to fully adopt an existing questionnaire, with most measurement developments drawing inspiration from Gligor et al. [
47]. This instrument assesses supply chain agility across five dimensions: responsiveness, proactivity, equipment, realignment, and customization. Although there is limited evidence to reach a consensus on using this instrument, it serves as a valuable starting point. Future questionnaires designed for studying supply chain agility in the healthcare sector should consider incorporating these dimensions as a foundational framework.
Similar to the workforce agility construct, there is a limited pool of studies examining questionnaire dimensions, with only three studies available for analysis. Within this constrained context, the dimensions of “Responsiveness” and “Speed of Treatment” exhibit some co-occurrences but warrant further exploration. Notably, a recommendation can be made to consider adapting Robert and Grover’s [
56] firms’ customer agility questionnaire, as featured in Van de Wetering et al.’s work [
69]. It is worth mentioning that the Robert and Grover questionnaire is also referenced in the literature about other constructs, such as organizational agility [
55]. Additionally, the sensing and responding dimensions featured in Shakhour et al.’s study [
62] offer potential insights for further exploration.
In addressing question 2 of this review, it becomes evident that replicability in the use of questionnaires for studying agility in the healthcare construct remains challenging to establish. While researchers have repeatedly turned to the Sharifi and Zhang questionnaire for organizational agility, with its dimensions of responsiveness, competitiveness, flexibility, and speed, which have found applications in various contexts, verified questionnaires have not been consistently adopted. Instead, researchers have often chosen to create new questionnaires, extracting dimensions from existing ones or employing measurement items corresponding to the literature. This diversity results in a lack of consistency, not only in the constructs’ definitions but also in the measurements provided. Nevertheless, each questionnaire, dimension, and item employed contributes to the field’s validity and understanding. Future research endeavors hold the potential to enhance agility questionnaires by incorporating these extracted dimensions.
4.3. Agility Models in the Healthcare Industry
The preceding synthesis analysis laid the foundations for the four agility constructs and shed light on potential observable variables that can infer these constructs at different cluster levels. In essence, we have identified which variables can explain agility. However, a crucial aspect remains to be explored—understanding what enables agility and what agility, in turn, enables. This pertains to the empirical agility models in the 21 selected papers.
Table 10,
Table 11,
Table 12 and
Table 13 provide concise summaries of the models featured in these papers to address this question. Latent variables within each model have been meticulously documented, organized by agility level, and categorized as predictors (variables with a positive effect on agility, essentially independent variables of agility), responders (variables positively influenced by agility, effectively serving as dependent variables of agility), mediators (variables that mediate the impact of another variable on agility), and moderators (variables that moderate the relationship).
Furthermore, the “variable order” column specifies the variable level, where an order one variable denotes a reflective construct, while order two signifies a formative construct. The “path coefficient” column quantifies the strength of the relationship between the two variables, representing the extent to which the predictor may elucidate the results of the responder. Finally, the “significance” column underscores whether the relationship holds statistical significance. For this analysis, a significance level of 0.05 was selected as the baseline threshold.
5. Discussion
This study addressed three questions pertinent to empirical studies on agility in the healthcare sector, aiming to bridge research gaps identified in prior studies. Specifically, we examined (1) agility constructs developed within the healthcare sector, (2) the surveys employed to study these agility constructs, and (3) other constructs significant to agility definitions in healthcare models.
To our knowledge, this is the first systematic literature review tailored to the healthcare field. While Patri and Suresh [
23] presented a review on healthcare agility, it did not adhere to a systematic literature review protocol. The research into agility, as highlighted in this study, has seen substantial growth between 2018 and 2022, as illustrated in
Figure 2. Patri and Suresh [
23] focused on the literature available up to 2017, identifying only 4 of the 21 studies as survey-based. Our current study enriches this domain by spotlighting 21 survey-based research projects in the healthcare sector, further building upon the existing literature.
Unlike the other recent literature reviews that have focused on specific agility constructs, such as organizational agility [
21,
28,
70], workforce agility [
2,
11,
26,
71], and supply chain agility [
3,
17,
18,
19], this study stands apart by undertaking a comprehensive examination of all empirically studied agility constructs within the healthcare sector. It presents foundational insights into the four identified agility constructs in the healthcare domain: organizational agility, workforce agility, supply chain agility, and treatment agility.
Table 14 consolidates these construct levels and their proposed definitions, laying the groundwork for a discussion on a multi-dimensional agility model.
While extensive reviews cover multiple agility constructs in the literature, they do not necessarily align with these four major ones. For example, Haider et al. [
20] have proposed additional agility constructs like business agility, strategic agility, and operational agility. However, it is important to note that this study primarily focuses on research conducted in areas beyond healthcare. Although there is potential for expanding research and gathering empirical evidence to assess the presence of these other constructs in healthcare, current research directions have yet to take that path. To mitigate issues related to construct proliferation, it is advisable to prioritize the validation of the existing constructs and their associated models [
28].
In addition to the challenges identified in construct development, the research has also underscored the need for empirical studies validating the current theoretical constructs of agility. This study has cataloged 21 empirical investigations of agility constructs within the healthcare sector. This observation aligns with the findings of prior authors. There is a pressing need to explore alternative agility models, but equally important is the validation of the existing theoretical dimensions underpinning agility. Despite the limited research on this subject matter, it remains possible to draw meaningful conclusions regarding agility in healthcare that can enhance the replicability and validity of agility models.
When it comes to instrument adoption and the development of the selected empirical studies, one of the important observations is the need for replicability of the questionnaires used. Most papers (17 out of 21) created their own questionnaires. Among the four agility constructs identified in this review, only Sharifi and Zhang’s Organizational Agility questionnaire demonstrates robust validity. Two authors have replicated this instrument, and four others have cited it as part of their questionnaires. In the supply chain agility construct, the questionnaires appear to replicate and support the dimensions established in Gligor and Holcomb’s theoretical construct [
47]: responsiveness, proactivity, equipment, realignment, and customization. However, researchers should conduct further investigations to validate these dimensions, as the number of studies (three out of five) is still relatively limited.
In the context of workforce agility, Sherehiy and Karwowski’s three-dimensional questionnaire [
61] is used in Saleem et al.’s study [
60], but the other two papers on workforce agility employed different questionnaires. Therefore, it is advisable to consider using more robust and validated questionnaires, such as the aggregated model for workforce agility proposed by Petermann and Zacher [
15]. However, it is worth noting that this model has not yet been tested in healthcare settings.
As for treatment agility, this construct is still in its early stages of development, with no replication observed for the questionnaires used. However, dimensions like “speed of treatment” and “accommodations” are included in two of the three studies [
44,
48], and Roberts and Grover’s questionnaire [
56] serves as a valuable reference for treatment agility. This emerging construct warrants further research and the development of more robust questionnaires.
Table 15 summarizes the recommended instruments for each of the four agility levels.
Figure 7 provides a comprehensive summary of the agility models explored in the questionnaire-based studies, categorizing the corresponding latent variables into predictors and responders for each of the four agility constructs. The figure also groups the latent variables listed in
Table 10,
Table 11,
Table 12 and
Table 13 based on their themes and associates them with the respective agility construct. It is important to note that this analysis excluded latent variables listed as mediators and moderators.
The evidence from empirical studies suggests that human factors and information technologies impact the agility of healthcare organizations. Models have shown that agile organizations tend to perform better in various areas. Improvements in the human dimension and technology aspects of healthcare organizations may lead to better agility, which in turn can improve overall performance. Therefore, we advise that healthcare decision-makers focus on enhancing their human dimensions and technology aspects to improve their organization’s agility.
Figure 8 outlines the theoretical framework.
The study findings reveal that all four agility constructs incorporate dependent variables in their empirical models within the healthcare domain. However, only three of the four constructs include any predictors of agility. Despite the differences among these constructs, a common pattern emerges—each agility construct features a performance-oriented latent variable set as a responder. Additionally, a form of technology-oriented predictor exists for the constructs of organizational agility, supply chain agility, and treatment agility.
Notably, this analysis highlights an intriguing gap: no questionnaire-based empirical study has investigated the enablers of workforce agility. Drawing from the trends observed in the other constructs, it raises an intriguing question—do any technology-related constructs impact workforce agility? Further exploration in this direction could yield valuable insights.
Like any other research endeavor, this study is subject to certain limitations. Its scope is highly specific, focusing solely on empirical investigations of agility constructs within the healthcare sector. The authors’ choice of keywords and databases further restricts the study’s scope, potentially overlooking other existing empirical investigations in healthcare agility. In addition, the study exclusively concentrated on peer-reviewed publications utilizing multivariate analysis derived from survey responses. This constraint had repercussions for the relatively small sample size in the study. All the captured studies were cross-sectional studies; there are no longitudinal studies of agility in the healthcare context. Despite these limitations, it is important to note that the primary objective of this review was to identify explicitly defined agility constructs in healthcare. Finally, while the study provides a qualitative synthesis of group constructs and latent variables, it must comprehensively examine the construct dimensions and models observed. A robust meta-analysis could enhance our knowledge by facilitating the development of more refined theoretical models and improved instruments for evaluating agility constructs in healthcare.
6. Conclusions
The empirical research on agility in the healthcare industry has room for improvement. Despite a lack of consensus in agility construct definitions, empirical studies have revealed four major levels of agility in the healthcare sector: organizational agility, workforce agility, supply chain agility, and treatment agility. The research in healthcare agility also needs more consensus on standard questionnaires. Sharifi and Zhang’s questionnaire for organizational agility [
7] has yet to be consistently used or referenced in the measurement items across the selected studies.
Although some authors have referred to other questionnaires, the validity of these instruments beyond their original studies remains to be determined. These questionnaires were often adapted from other industries. However, similarities among the dimensions and items used in these questionnaires remain evident. The above suggests the possibility of developing focused questionnaires for each clustered healthcare agility construct.
While agility models in the four suggested constructs lack replication, they exhibit notable similarities. Performance-oriented latent variables have consistently emerged as significant responders in all four constructs of agility. Additionally, technology-oriented latent variables have been explored in three agility constructs and identified as significant enablers of agility, apart from the workforce agility construct, which currently lacks significant predictors.
This study contributes to the existing literature by addressing several key aspects within the healthcare sector. Firstly, it introduces four agility constructs for examination, bridging the gaps in the current body of knowledge. Secondly, it identified and analyzed the instruments and dimensions employed in empirical investigations within the sector. Thirdly, the study acknowledges the theoretical models relevant to healthcare agility and highlights areas where further research is needed.
Future research endeavors should prioritize establishing relationships between these agility models. Specifically, it is essential to determine whether healthcare agility can be compartmentalized into four distinct constructs or whether a more comprehensive, multi-dimensional healthcare agility model is viable. This question warrants a dedicated study for thorough exploration.
Moreover, the healthcare industry would benefit from an increased focus on empirical studies to validate the effectiveness of each questionnaire and its associated model. To this end, conducting empirical research that assesses the technological enablers of workforce agility is strongly recommended. Such studies will provide valuable insights and enhance the credibility of the proposed models in real-world healthcare settings. Similarly, researchers must consider conducting longitudinal studies in agility to verify the cause–effect relationships in the theoretical models.
The review of survey studies on agility in healthcare can offer several tangible benefits to healthcare practitioners, patients, and society. First, the findings from agility studies can inform practitioners how healthcare practices can be improved. Second, the results of agility studies can be used to improve healthcare delivery concerning patients’ needs and lead to greater patient satisfaction. Finally, agile healthcare practices can help reduce costs due to inefficiencies and improve the quality of healthcare delivery available to the general public.