Orofacial Muscle Strength and Associated Potential Factors in Healthy Korean Community-Dwelling Older Adults: A Pilot Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
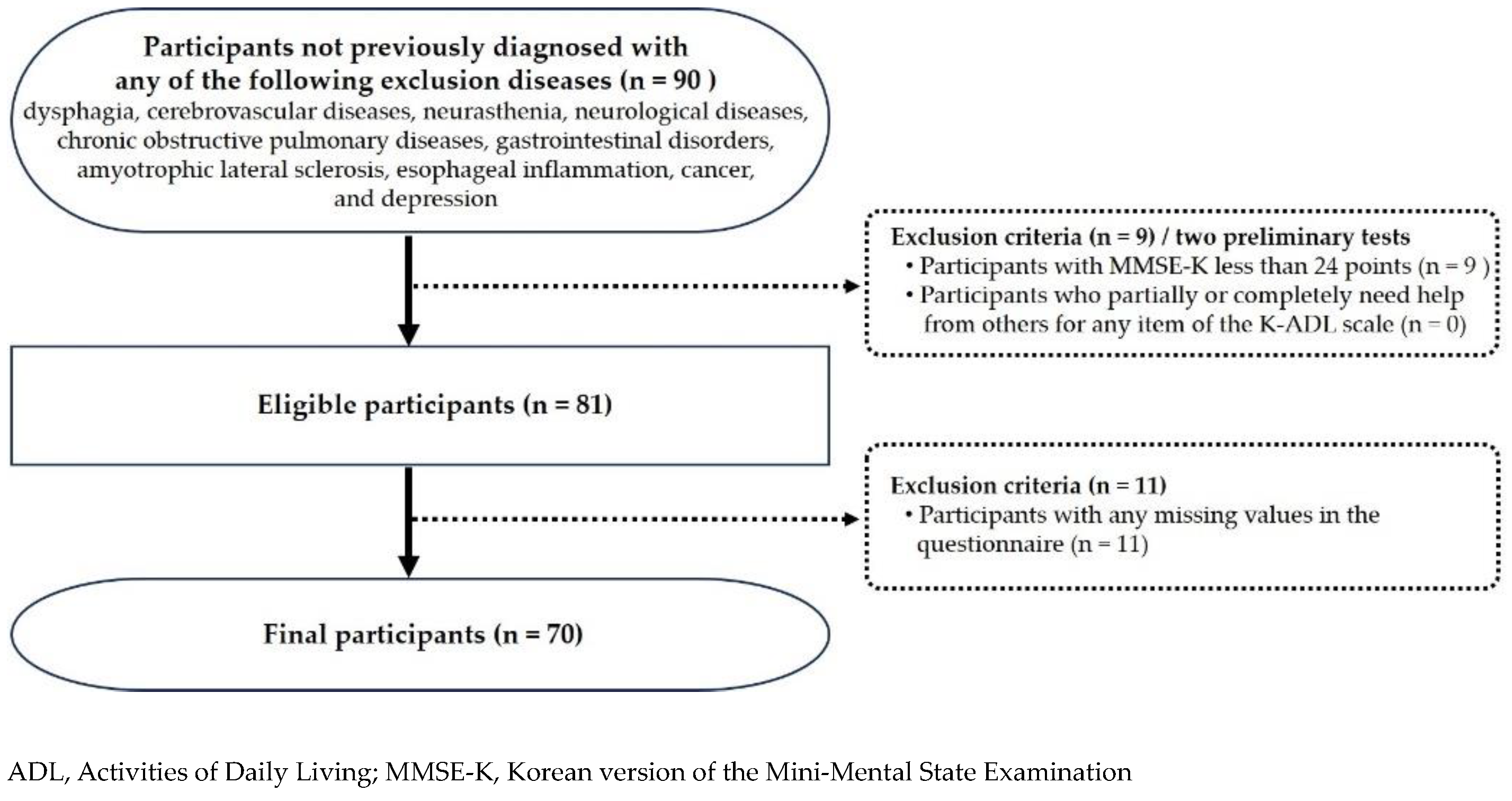
2.1. Participants
2.2. Measurements
2.3. Statistical Analysis
3. Results
3.1. Distribution of Sociodemographic Characteristics and Orofacial Muscle Strength Levels of Participants
3.2. Orofacial Muscle Strength by Sociodemographic Characteristics
3.3. Orofacial Muscle Strength by General Health-Related Characteristics
3.4. Orofacial Muscle Strength by Oral Health Status
3.5. Potential Factors Associated with Orofacial Muscle Strength
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Aging and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 1 May 2024).
- South Korea Ranks Worst in OECD for Poverty in Old Age. Available online: https://english.hani.co.kr/arti/english_edition/e_national/1013419.html (accessed on 30 April 2024).
- Fields, E.C.; Kensinger, E.A.; Garcia, S.M.; Ford, J.H.; Cunningham, T.J. With age comes well-being: Older age associated with lower stress, negative affect, and depression throughout the COVID-19 pandemic. Aging Ment. Health 2022, 26, 2071–2079. [Google Scholar] [CrossRef] [PubMed]
- Murman, D.L. The impact of age on cognition. Semin. Hear. 2015, 36, 111–121. [Google Scholar] [CrossRef] [PubMed]
- Shallcross, A.J.; Ford, B.Q.; Floerke, V.A.; Mauss, I.B. Getting better with age: The relationship between age, acceptance, and negative affect. J. Pers. Soc. Psychol. 2013, 104, 734–749. [Google Scholar] [CrossRef] [PubMed]
- Korean Academy of Orofacial Pain & Oral Medicine. Dental Management of the Medically Compromised, the Elderly, and the Disabled Patients, 2nd ed.; YENANG Inc.: Seoul, Republic of Korea, 2019; pp. 380–381. [Google Scholar]
- Lamster, I.B.; Asadourian, L.; Del Carmen, T.; Friedman, P.K. The aging mouth: Differentiating normal aging from disease. Periodontology 2000 2016, 72, 96–107. [Google Scholar] [CrossRef]
- Wolff, A.; Joshi, R.K.; Ekström, J.; Aframian, D.; Pedersen, A.M.L.; Proctor, G.; Narayana, N.; Villa, A.; Sia, Y.W.; Aliko, A.; et al. A guide to medications inducing salivary gland dysfunction, xerostomia, and subjective sialorrhea: A systematic review sponsored by the World Workshop on Oral Medicine VI. Drugs R&D 2017, 17, 1–28. [Google Scholar]
- Park, J.S.; You, S.J.; Kim, J.Y.; Yeo, S.G.; Lee, J.H. Differences in orofacial muscle strength according to age and sex in East Asian healthy adults. Am. J. Phys. Med. Rehabil. 2015, 94, 677–686. [Google Scholar] [CrossRef]
- Clark, H.M.; Solomon, N.P. Age and sex differences in orofacial strength. Dysphagia 2012, 27, 2–9. [Google Scholar] [CrossRef]
- Felton, S.M.; Gaige, T.A.; Reese, T.G.; Wedeen, V.J.; Gilbert, R.J. Mechanical basis for lingual deformation during the propulsive phase of swallowing as determined by phase-contrast magnetic resonance imaging. J. Appl. Physiol. 2007, 103, 255–265. [Google Scholar] [CrossRef]
- Byeon, H.W. Effect of orofacial myofunctional exercise on the improvement of dysphagia patients’ orofacial muscle strength and diadochokinetic rate. J. Phys. Ther. Sci. 2016, 28, 2611–2614. [Google Scholar] [CrossRef]
- Liu, X.; Zhang, X.; Feng, Q. Dynamic change in the thickness of the masseter muscle between contraction and relaxation is associated with the masticatory function in older adults: A cross-sectional study. Ann. Palliat. Med. 2022, 11, 3755–3763. [Google Scholar] [CrossRef]
- Mul, K.; Berggren, K.N.; Sills, M.Y.; McCalley, A.; van Engelen, B.G.M.; Johnson, N.E.; Statland, J.M. Effects of weakness of orofacial muscles on swallowing and communication in FSHD. Neurology 2019, 92, e957–e963. [Google Scholar] [CrossRef] [PubMed]
- González-Fernández, M.; Ottenstein, L.; Atanelov, L.; Christian, A.B. Dysphagia after stroke: An overview. Curr. Phys. Med. Rehabil. Rep. 2013, 1, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Doan, T.N.; Ho, W.C.; Wang, L.H.; Chang, F.C.; Nhu, N.T.; Chou, L.W. Prevalence and methods for assessment of oropharyngeal dysphagia in older adults: A systematic review and meta-analysis. J. Clin. Med. 2022, 11, 2605. [Google Scholar] [CrossRef] [PubMed]
- Umay, E.; Eyigor, S.; Bahat, G.; Halil, M.; Giray, E.; Unsal, P.; Unlu, Z.; Tikiz, C.; Vural, M.; Cincin, A.T.; et al. Best practice recommendations for geriatric dysphagia management with 5 Ws and 1H. Ann. Geriatr. Med. Res. 2022, 26, 94–124. [Google Scholar] [CrossRef]
- Lee, D.S.; Kim, H.E.; Choi, J.S. Associated with dysphagia risk among older, healthy, community dwelling Korean adults: A pilot study. Healthcare 2024, 12, 267. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, H.-S.; Yun, D.H.; Chon, J.; Han, Y.J.; Yoo, S.D.; Kim, D.H.; Lee, S.A.; Joo, H.I.; Park, J.-S.; et al. The relationship between tongue pressure and oral dysphagia in stroke patients. Ann. Rehabil. Med. 2016, 40, 620–628. [Google Scholar] [CrossRef]
- Saleedaeng, P.; Korwanich, N.; Muangpaisan, W.; Korwanich, K. Effect of dysphagia on the older adults’ nutritional status and meal pattern. J. Prim. Care Commun. Health 2023, 14, 21501319231158280. [Google Scholar] [CrossRef]
- Ney, D.M.; Weiss, J.M.; Kind, A.J.H.; Robbins, J.A. Senescent swallowing: Impact, strategies and interventions. Nutr. Clin. Pract. 2009, 24, 395–413. [Google Scholar] [CrossRef]
- Roy, N.; Stemple, J.; Merrill, R.M.; Thomas, L. Dysphagia in the elderly: Preliminary evidence of prevalence, risk factors, and socioemotional effects. Ann. Otol. Rhinol. Laryngol. 2007, 116, 858–865. [Google Scholar] [CrossRef]
- Nakamori, M.; Ishikawa, K.; Imamura, E.; Yamamoto, H.; Kimura, K.; Ayukawa, T.; Mizoue, T.; Wakabayashi, S. Relationship between tongue pressure and dysphagia diet in patients with acute stroke. PLoS ONE 2021, 16, e0252837. [Google Scholar] [CrossRef]
- Minagi, Y.; Ono, T.; Hori, K.; Fujiwara, S.; Tokuda, Y.; Murakami, K.; Maeda, Y.; Sakoda, S.; Yokoe, M.; Mihara, M.; et al. Relationships between dysphagia and tongue pressure during swallowing in Parkinson’s disease patients. J. Oral Rehabil. 2018, 45, 459–466. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Carmona, R.; Traube, M. Dysphagia in the elderly. Clin. Geriatr. Med. 2014, 30, 43–53. [Google Scholar] [CrossRef] [PubMed]
- Prosiegel, M.; Riecker, A.; Weinert, M.; Dziewas, R.; Lindner-Pfleghar, B.; Stanschus, S.; Warnecke, T. Management of dysphagic patients with acute stroke. Nervenarzt 2012, 83, 1590–1599. [Google Scholar] [CrossRef] [PubMed]
- Keller, K.; Engelhardt, M. Strength and muscle mass loss with aging process. Age and strength loss. Muscles Ligaments Tendons J. 2013, 3, 346–350. [Google Scholar] [CrossRef]
- Kugimiya, Y.; Iwasaki, M.; Ohara, Y.; Motokawa, K.; Edahiro, A.; Shirobe, M.; Watanabe, Y.; Taniguchi, Y.; Seino, S.; Abe, T.; et al. Association between sarcopenia and oral functions in community-dwelling older adults: A cross-sectional study. J. Cachexia Sarcopenia Muscle 2023, 14, 429–438. [Google Scholar] [CrossRef]
- Takano, S.; Yamaguchi, K.; Nakagawa, K.; Yoshimi, K.; Nakane, A.; Okumura, T.; Tohara, H. Effect of isometric exercises on the masseter muscle in older adults with missing dentition: A randomized controlled trial. Sci. Rep. 2021, 11, 7285. [Google Scholar]
- Tashiro, K.; Soutome, S.; Funahara, M.; Kawashita, Y.; Kitamura, M.; Fukuda, H.; Furugen, R.; Iwasaki, T.; Hayashida, H.; Kawasaki, K.; et al. The relationship between dental findings and tongue pressure: A survey of 745 community-dwelling adults and elderly persons in Japan. Gerontology 2021, 67, 517–524. [Google Scholar] [CrossRef]
- Kang, I.W.; Beom, I.G.; Cho, J.Y.; Son, H.R. Accuracy of Korean-Mini-Mental Status Examination Based on Seoul Neuro-Psychological Screening Battery II results. Korean J. Fam. Med. 2016, 37, 177–181. [Google Scholar] [CrossRef]
- Park, J.; Kwon, Y. Standardization of Korean version of Mini-Mental State Examination (MMSE-K) for use in the elderly. Part II. diagnosis validity. J. Korean Neuropsychiatr. Assoc. 1989, 28, 508–513. [Google Scholar]
- Shin, J.H. Diagnosis of dementia: Neuropsychological test. Korean J. Fam. Med. 2010, 31, 253–266. [Google Scholar] [CrossRef]
- Kim, E.Y.; Lee, Y.N.; Jeong, E.H.; Chang, S.O. Developing a Korean version of the scale for the observation of agitation in persons with dementia of alzheimer-type. J. Korean Gerontol. Nurs. 2020, 22, 316–325. [Google Scholar] [CrossRef]
- Won, C.W.; Rho, Y.G.; Kim, S.Y.; Cho, B.R.; Lee, Y.S. The validity and reliability of Korean Activities of Daily Living (K-ADL) Scale. J. Korean Geriatr. Soc. 2002, 6, 98–106. [Google Scholar]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G* power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Wiener, R.C.; Wu, B.; Crout, R.; Wiener, M.; Plassman, B.; Kao, E.; McNeil, D. Hyposalivation and xerostomia in dentate older adults. J. Am. Dent. Assoc. 2020, 141, 279–284. [Google Scholar] [CrossRef]
- Bergdahl, M.; Bergdahl, J. Low unstimulated salivary flow and subjective oral dryness: Association with medication, anxiety, depression, and stress. J. Dent. Res. 2000, 79, 1652–1658. [Google Scholar] [CrossRef]
- Samnieng, P.; Ueno, M.; Shinada, K.; Zaitsu, T.; Wright, F.A.; Kawaguchi, Y. Oral health status and chewing ability is related to mini-nutritional assessment results in an older adult population in Thailand. J. Nutr. Gerontol. Geriatr. 2011, 30, 291–304. [Google Scholar] [CrossRef]
- Ueno, M.; Yanagisawa, T.; Shinada, K.; Ohara, S.; Kawaguchi, Y. Category of functional tooth units in relation to the number of teeth and masticatory ability in Japanese adults. Clin. Oral Investig. 2010, 14, 113–119. [Google Scholar] [CrossRef]
- Jung, H.J.; Min, Y.G.; Kim, H.J.; Lee, J.Y.; Lee, E.S.; Kim, B.I.; Ahn, H.J. Factors affecting objective and subjective masticatory ability assessment of Korean elderly people. J. Korean Acad. Oral Health 2018, 42, 216–223. [Google Scholar] [CrossRef]
- Park, J.S.; Oh, D.H.; Chang, M.Y. Effect of expiratory muscle strength training on swallowing-related muscle strength in community-dwelling elderly individuals: A randomized controlled trial. Gerodontology 2017, 34, 121–128. [Google Scholar] [CrossRef]
- Lee, Y.S.; Ryu, J.H.; Baek, S.H.; Lim, W.H.; Yang, I.H.; Kim, T.W.; Jung, S.K. Comparative analysis of the differences in dentofacial morphology according to the tongue and lip pressure. Diagnostics 2021, 11, 503. [Google Scholar] [CrossRef]
- Yitbarek, G.Y.; Alty, J.; Lawler, K.; Goldberg, L.R. Current evidence on the association of tongue strength with cognitive decline in older adults and the known risk factors of frailty, sarcopenia and nutritional health: A scoping review protocol. BMJ Open 2023, 13, e076005. [Google Scholar] [CrossRef] [PubMed]
- The Korean Dysphagia Society. Swallowing Disorders, 1st ed.; Koonja Publishing: Paju-si, Republic of Korea, 2017; pp. 13–145. [Google Scholar]
- Dutra, E.H.; Caria, P.H.; Rafferty, K.L.; Herring, S.W. The buccinator during mastication: A functional and anatomical evaluation in minipigs. Arch. Oral Biol. 2010, 55, 627–638. [Google Scholar] [CrossRef] [PubMed]
- Yoshiko, A.; Hioki, M.; Kanehira, N.; Shimaoka, K.; Koike, T.; Sakakibara, H.; Oshida, Y.; Akima, H. Three-dimensional comparison of intramuscular fat content between young and old adults. BMC Med. Imaging 2017, 17, 12. [Google Scholar] [CrossRef]
- Health AgingBody Composition Study; Delmonico, M.J.; Harris, T.B.; Visser, M.; Park, S.W.; Conroy, M.B.; Velasquez-Mieyer, P.; Boudreau, R.; Manini, T.M.; Nevitt, M.; et al. Longitudinal study of muscle strength, quality, and adipose tissue infiltration. Am. J. Clin. Nutr. 2009, 90, 1579–1585. [Google Scholar] [CrossRef]
- Park, J.; Oh, D.; Chang, M. Comparison of maximal tongue strength and tongue strength used during swallowing in relation to age in healthy adults. J. Phys. Ther. Sci. 2016, 28, 442–445. [Google Scholar] [CrossRef]
- Nakao, Y.; Yamashita, T.; Honda, K.; Katsuura, T.; Hama, Y.; Nakamura, Y.; Ando, K.; Ishikura, R.; Kodama, N.; Uchiyama, Y.; et al. Association among age-related tongue muscle abnormality, tongue pressure, and presbyphagia: A 3D MRI study. Dysphagia 2021, 36, 483–491. [Google Scholar] [CrossRef]
- Doherty, T.J. Invited review: Aging and sarcopenia. J. Appl. Physiol. 2003, 95, 1717–1727. [Google Scholar] [CrossRef]
- Korea Institute for Health and Social Affairs. 2020 National Survey of Older Koreans; Korea Institute for Health and Social Affairs: Sejong, Republic of Korea, 2020; pp. 126–127. [Google Scholar]
- Park, J.S.; You, S.J.; Jeong, C.H. Age and sex differences in orofacial strength of healthy Korean adult. Korea J. Occup. Ther. 2013, 21, 103–116. [Google Scholar]
- Borda, M.G.; Hassan, E.B.; Weon, J.H.; Wakabayashi, H.; Tovar-Rios, D.A.; Oppedal, K.; Aarsland, D.; Duque, G. Muscle volume and intramuscular fat of the tongue evaluated with MRI predict malnutrition in people living with dementia: A 5-year follow-up study. J. Gerontol. A Biol. Sci. Med. Sci. 2022, 77, 228–234. [Google Scholar] [CrossRef]
- Daboul, A.; Schwahn, C.; Bülow, R.; Kiliaridis, S.; Kocher, T.; Klinke, T.; Mundt, T.; Mourad, S.; Völzke, H.; Habes, M.; et al. Influence of age and tooth loss on masticatory muscles characteristics: A population based MR imaging study. J. Nutr. Health Aging 2018, 22, 829–836. [Google Scholar] [CrossRef]
- Huang, Y.F.; Chang, W.H.; Liao, Y.F.; Chen, M.H.; Chang, C.T. Lip and tongue strength associated with chewing patterns in aging population. BMC Oral Health 2023, 23, 848. [Google Scholar] [CrossRef] [PubMed]
- Clark, D.; Kotronia, E.; Ramsay, S.E. Frailty, aging, and periodontal disease: Basic biologic considerations. Periodontology 2000 2021, 87, 143–156. [Google Scholar] [CrossRef] [PubMed]
- Eaton, K.; Ower, P. Practical Periodontics, 1st ed.; Elsevier: St. Louis, MI, USA, 2015; pp. 3–12. [Google Scholar]
- Fouda, S.M.; Gad, M.M.; El Tantawi, M.; Virtanen, J.I.; Sipila, K.; Raustia, A. Influence of tooth loss on mandibular morphology: A cone-beam computed tomography study. J. Clin. Exp. Dent. 2019, 11, e814–e819. [Google Scholar] [CrossRef]
- Yamaguchi, K.; Tohara, H.; Hara, K.; Nakane, A.; Kajisa, E.; Yoshimi, K.; Minakuchi, S. Relationship of aging, skeletal muscle mass, and tooth loss with masseter muscle thickness. BMC Geriatr. 2018, 18, 67. [Google Scholar] [CrossRef]
- Rodakowska, E.; Jamiolkowski, J.; Baginska, J.; Kaminska, I.; Gabiec, K.; Stachurska, Z.; Kondraciuk, M.; Dubatowka, M.; Kaminski, K.A. Oral health–related quality of life and missing teeth in an adult population: A cross-sectional study from Poland. Int. J. Environ. Res. Public Health 2022, 19, 1626. [Google Scholar] [CrossRef]
- Mituuti, C.T.; Bianco, V.C.; Bentim, C.G.; de Andrade, E.C.; Rubo, J.H.; Berretin-Felix, G. Influence of oral health condition on swallowing and oral intake level for patients affected by chronic stroke. Clin. Interv. Aging 2015, 10, 29–35. [Google Scholar] [CrossRef]
- Wang, T.; Feng, X.; Zhou, J.; Gong, H.; Xia, S.; Wei, Q.; Hu, X.; Tao, R.; Li, L.; Qian, F.; et al. Type 2 diabetes mellitus is associated with increased risks of sarcopenia and pre-sarcopenia in Chinese elderly. Sci. Rep. 2016, 6, 38937. [Google Scholar] [CrossRef]
- Mesinovic, J.; Zengin, A.; De Courten, B.; Ebeling, P.R.; Scott, D. Sarcopenia and type 2 diabetes mellitus: A bidirectional relationship. Diabetes Metab. Syndr. Obes. 2019, 8, 1057–1072. [Google Scholar] [CrossRef]
- Kalyani, R.R.; Corriere, M.; Ferrucci, L. Age-related and disease-related muscle loss: The effect of diabetes, obesity, and other diseases. Lancet Diabetes Endocrinol. 2014, 2, 819–829. [Google Scholar] [CrossRef]
- Rogers, C.R.; Mooney, M.P.; Smith, T.D.; Weinberg, S.M.; Waller, B.M.; Parr, L.A.; Docherty, B.A.; Bonar, C.J.; Reinholt, L.E.; Deleyiannis, F.W.; et al. Comparative microanatomy of the orbicularis oris muscle between chimpanzees and humans: Evolutionary divergence of lip function. J. Anat. 2009, 214, 36–44. [Google Scholar] [CrossRef]
- Fortuna, G.; Whitmire, S.; Sullivan, K.; Alajbeg, I.; Andabak-Rogulj, A.; Pedersen, A.M.L.; Vissink, A.; di Fede, O.; Aria, M.; Jager, D.J.; et al. Impact of medications on salivary flow rate in patients with xerostomia: A retrospective study by the Xeromeds Consortium. Clin. Oral Investig. 2023, 27, 235–248. [Google Scholar] [CrossRef] [PubMed]
- Dawes, C.; Pedersen, A.M.L.; Villa, A.; Ekström, J.; Proctor, G.B.; Vissink, A.; Aframian, D.; McGowan, R.; Aliko, A.; Narayana, N.; et al. The functions of human saliva: A review sponsored by the World Workshop on Oral Medicine VI. Arch. Oral Biol. 2015, 60, 863–874. [Google Scholar] [CrossRef] [PubMed]
- Kugimiya, Y.; Oki, T.; Ohta, M.; Ryu, M.; Kobayashi, K.; Sakurai, K.; Ueda, T. Distribution of lip-seal strength and its relation to oral motor functions. Clin. Exp. Dent. Res. 2021, 7, 1122–1130. [Google Scholar] [CrossRef] [PubMed]
- Takehana, Y.; Masuda, Y.; Kageyama, T.; Okazaki, R.; Murakami, M.; Yamada, K. The relationship between lip-closing force and dental arch morphology in patient with Angle Class I malocclusion. J. Oral Rehabil. 2017, 44, 205–212. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Division | n | % |
|---|---|---|---|
| Sex | male | 17 | 24.3 |
| female | 53 | 75.7 | |
| Age (y) | 65–69 | 20 | 28.6 |
| 70–74 | 15 | 21.4 | |
| 75–79 | 15 | 21.4 | |
| ≥80 | 20 | 28.6 | |
| Education level | ≤elementary school | 32 | 45.7 |
| middle school | 23 | 32.9 | |
| ≥high school | 15 | 21.4 | |
| Economic activity | yes | 23 | 32.9 |
| no | 47 | 67.1 | |
| Living status | alone | 10 | 14.3 |
| with spouse | 32 | 45.7 | |
| with children | 28 | 40.0 | |
| Orofacial muscles | tongue elevation | 44.50 ± 12.00 | |
| Strength † | cheek compression | 23.53 ± 7.03 | |
| lip compression | 15.63 ± 3.91 | ||
| Variables | n | Orofacial Muscles Strength | ||||||
|---|---|---|---|---|---|---|---|---|
| Tongue Elevation | d † (or η2) (p) | Cheek Compression | d † (or η2) (p) | Lip Compression | d † (or η2) (p) | |||
| Sex | male | 17 | 49.59 ± 10.38 | 0.595 | 26.47 ± 6.53 | 0.615 | 17.94 ± 4.76 | 0.743 |
| female | 53 | 42.87 ± 12.11 | (0.044) | 22.58 ± 6.98 | (0.047) | 14.89 ± 3.32 | (0.023) | |
| Age †,‡ (y) | ≤74 | 35 | 50.54 ± 8.79 | 1.159 | 26.20 ± 5.51 | 0.817 | 17.03 ± 2.91 | 0.761 |
| ≥75 | 35 | 38.46 ± 11.82 | (<0.001) | 20.86 ± 7.42 | (<0.001) | 14.23 ± 4.31 | (0.001) | |
| Education | ≤elementary school | 32 | 38.63 ± 12.04 | 0.994 | 21.03 ± 7.58 | 0.679 | 13.75 ± 3.27 | 0.984 |
| level | ≥middle school | 38 | 49.45 ± 9.59 | (<0.001) | 25.63 ± 5.84 | (0.003) | 17.21 ± 3.74 | (<0.001) |
| Economic | yes | 23 | 49.09 ± 10.16 | 0.606 | 26.61 ± 6.01 | 0.700 | 16.48 ± 3.43 | 0.335 |
| activity | no | 47 | 42.26 ± 12.28 | (0.012) | 22.02 ± 7.05 | (0.005) | 15.21 ± 4.10 | (0.091) |
| Living | alone | 10 | 42.30 ± 12.36 a,b | 0.138 | 21.50 ± 7.01 | 0.074 | 14.40 ± 4.00 ab | 0.152 |
| status | with spouse | 32 | 49.25 ± 10.25 a | (0.007) | 25.59 ± 6.52 | (0.076) | 17.28 ± 3.97 a | (0.004) |
| with children | 28 | 39.86 ± 12.05 b | 21.89 ± 7.19 | 14.18 ± 3.11 b | ||||
| Variables | n | Orofacial Muscle Strength | ||||||
|---|---|---|---|---|---|---|---|---|
| Tongue Elevation | d † (or η2) (p) | Cheek Compression | d † (or η2) (p) | Lip Compression | d † (or η2) (p) | |||
| Smoking | non-smoker | 58 | 43.91 ± 12.33 | 0.038 | 23.38 ± 7.23 | 0.024 | 15.55 ± 3.89 | 0.053 |
| smoker (former) | 8 | 50.63 ± 10.94 | (0.274) | 26.00 ± 6.84 | (0.447) | 17.50 ± 3.74 | (0.162) | |
| smoker (current) | 4 | 40.75 ± 4.19 | 20.75 ± 2.36 | 13.00 ± 3.65 | ||||
| Alcohol | non-drinker | 51 | 42.25 ± 12.30 a | 0.111 | 22.22 ± 7.09 | 0.085 | 15.22 ± 3.77 | 0.060 |
| consumption | drinker (1 glass) | 2 | 48.00 ± 1.41 a,b | (0.021) | 28.00 ± 0.00 | (0.052) | 20.00 ± 0.00 | (0.130) |
| drinker (≥2 glasses) | 16 | 51.63 ± 9.04 b | 26.69 ± 6.05 | 16.63 ± 4.25 | ||||
| No. of systemic | 0 | 10 | 44.50 ± 13.92 | 0.0001 | 25.30 ± 7.73 | 0.022 | 17.70 ± 3.09 | 0.100 |
| diseases | 1–2 | 33 | 44.36 ± 12.70 | (0.995) | 23.97 ± 7.39 | (0.468) | 16.15 ± 4.20 | (0.030) |
| ≥3 | 27 | 44.67 ± 10.78 | 22.33 ± 6.34 | 14.22 ± 3.40 | ||||
| Hypertension | no | 23 | 41.35 ± 11.55 | 0.397 | 25.13 ± 7.35 | 0.337 | 16.30 ± 4.44 | 0.246 |
| yes | 47 | 46.04 ± 12.03 | (0.125) | 22.74 ± 6.80 | (0.184) | 15.30 ± 3.63 | (0.316) | |
| Diabetes | no | 49 | 45.45 ± 12.90 | 0.279 | 24.08 ± 7.29 | 0.269 | 16.43 ± 3.76 | 0.717 |
| yes | 21 | 42.29 ± 9.47 | (0.316) | 22.24 ± 6.35 | (0.318) | 13.76 ± 3.68 | (0.008) | |
| Hyperlipidemia | no | 34 | 43.15 ± 12.08 | 0.385 | 23.65 ± 7.65 | 0.031 | 15.88 ± 4.07 | 0.124 |
| yes | 36 | 45.78 ± 11.94 | (0.363) | 23.42 ± 6.50 | (0.892) | 15.39 ± 3.80 | (0.602) | |
| Osteoporosis | no | 56 | 44.91 ± 12.41 | 0.178 | 23.71 ± 6.84 | 0.123 | 15.84 ± 4.01 | 0.281 |
| yes | 14 | 42.86 ± 10.42 | (0.571) | 22.79 ± 7.96 | (0.662) | 14.79 ± 3.51 | (0.372) | |
| Cardiovascular | no | 55 | 45.84 ± 11.80 | 0.529 | 23.87 ± 7.18 | 0.233 | 16.18 ± 3.78 | 0.678 |
| disease | yes | 15 | 39.60 ± 11.79 | (0.074) | 22.27 ± 6.51 | (0.437) | 13.60 ± 3.83 | (0.023) |
| Variables | n | Orofacial Muscles Strength | ||||||
|---|---|---|---|---|---|---|---|---|
| Tongue Elevation | d † (or η2) (p) | Cheek Compression | d † (or η2) (p) | Lip Compression | d † (or η2) (p) | |||
| Mastication | comfortable (fair) | 50 | 46.58 ± 11.47 | 0.620 | 24.72 ± 6.93 | 0.571 | 16.42 ± 3.62 | 0.725 |
| discomfort | uncomfortable | 20 | 39.30 ± 11.98 | (0.021) | 20.55 ± 6.50 | (0.024) | 13.65 ± 4.01 | (0.007) |
| Pronunciation | comfortable (fair) | 64 | 45.81 ± 11.46 | 1.414 | 24.03 ± 6.85 | 0.830 | 16.00 ± 3.83 | 1.365 |
| discomfort | uncomfortable | 6 | 30.50 ± 8.57 | (0.002) | 18.17 ± 7.25 | (0.050) | 11.67 ± 2.33 | (0.009) |
| Perceived oral | good | 26 | 45.81 ± 12.93 | 0.040 | 25.12 ± 6.76 | 0.069 | 17.31 ± 3.99 a | 0.191 |
| health status | fair | 27 | 45.89 ± 11.02 | (0.255) | 23.96 ± 7.18 | (0.091) | 15.74 ± 3.40 a | (<0.001) |
| poor | 17 | 40.29 ± 11.70 | 20.41 ± 6.56 | 12.88 ± 3.12 b | ||||
| History of | no | 47 | 46.98 ± 11.28 | 0.646 | 24.72 ± 6.65 | 0.520 | 16.53 ± 3.88 | 0.758 |
| toothache | yes | 23 | 39.43 ± 12.06 | (0.012) | 21.09 ± 7.29 | (0.041) | 13.78 ± 3.35 | (0.005) |
| No. of remaining | 0–9 | 13 | 31.69 ± 11.96 a | 0.276 | 18.15 ± 7.03 a | 0.156 | 13.31 ± 3.81 a | 0.097 |
| teeth | 10–19 | 14 | 50.00 ± 9.85 b | (<0.001) | 26.71 ± 6.03 b | (0.003) | 15.21 ± 3.66 ab | (0.033) |
| ≥20 | 43 | 46.58 ± 10.01 b | 24.12 ± 6.56 b | 16.47 ± 3.80 b | ||||
| No. of functional | ≤6 | 17 | 36.47 ± 12.92 a | 0.152 | 19.59 ± 5.93 a | 0.105 | 14.29 ± 4.41 | 0.085 |
| tooth units | 7–9 | 8 | 49.75 ± 11.19 b | (0.004) | 23.75 ± 6.06 ab | (0.024) | 13.75 ± 2.31 | (0.051) |
| ≥10 | 45 | 46.60 ± 10.52 b | 24.98 ± 7.12 b | 16.47 ± 3.75 | ||||
| Use of dentures | no | 49 | 47.02 ± 10.34 a | 0.210 | 24.73 ± 6.50 a | 0.105 | 16.35 ± 3.91 a | 0.100 |
| upper or lower jaw | 8 | 47.63 ± 11.05 a | (<0.001) | 23.75 ± 9.31 ab | (0.025) | 15.25 ± 3.88 ab | (0.029) | |
| upper and lower jaw | 13 | 33.08 ± 12.45 b | 18.85 ± 5.90 b | 13.15 ± 3.05 b | ||||
| Denture | no | 49 | 47.02 ± 10.34 a | 0.155 | 24.73 ± 6.50 a | 0.103 | 16.35 ± 3.91 a | 0.095 |
| discomfort | use, comfortable | 4 | 48.75 ± 7.58 a | (0.003) | 25.50 ± 8.22 a | (0.026) | 15.75 ± 5.18 a | (0.036) |
| use, uncomfortable | 17 | 36.24 ± 13.88 b | 19.59 ± 7.19 b | 13.53 ± 2.98 b | ||||
| Unstimulated | <0.1 mL/min | 32 | 39.41 ± 11.70 | 0.840 | 22.28 ± 7.66 | 0.326 | 13.88 ± 3.81 | 0.895 |
| salivary flow rate | ≥0.1 mL/min | 38 | 48.79 ± 10.59 | (<0.001) | 24.58 ± 6.36 | (0.175) | 17.11 ± 3.39 | (<0.001) |
| Orofacial Muscle Strength | B (95% CI) | p-Value * | VIF | |
|---|---|---|---|---|
| Anterior tongue elevation 1 | ||||
| Age (≥75) | −9.177 (−13.685; −4.669) | <0.001 | 1.079 | F = 18.810 (<0.001), |
| No. of remaining teeth (0–9) | −11.011 (−16.923; −5.099) | <0.001 | 1.135 | Adj. R2 = 0.440, |
| Pronunciation discomfort (uncomfortable) | −9.931 (−17.884; −1.977) | 0.015 | 1.067 | Durbin-Watson = 1.888 |
| Cheek compression 2 | ||||
| Age (≥75) | −4.186 (−7.216; −1.157) | 0.007 | 1.072 | F = 8.268 (<0.001), |
| No. of remaining teeth (0–9) | −4.798 (−8.707; −0.889) | 0.017 | 1.080 | Adj. R2 = 0.240, |
| Mastication discomfort (uncomfortable) | −3.445 (−6.703; −0.187) | 0.039 | 1.013 | Durbin-Watson = 1.528 |
| Lip compression 3 | ||||
| Sex (female) | −2.272 (−4.227; −0.317) | 0.023 | 1.414 | |
| Education level (≥middle school) | 1.690 (−0.049; 3.428) | 0.057 | 1.509 | F = 11.476 (<0.001), |
| Diabetes (yes) | −2.228 (−3.831; −0.625) | 0.007 | 1.086 | Adj. R2 = 0.432, |
| Perceived oral health status (good) | 1.374 (0.393; 2.355) | 0.007 | 1.157 | Durbin-Watson = 1.458 |
| Unstimulated salivary flow rate | 11.514 (1.139; 21.889) | 0.030 | 1.187 | |
| (continuous) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, D.-S.; Kim, J.-Y.; Choi, J.-S. Orofacial Muscle Strength and Associated Potential Factors in Healthy Korean Community-Dwelling Older Adults: A Pilot Cross-Sectional Study. Appl. Sci. 2024, 14, 10560. https://doi.org/10.3390/app142210560
Lee D-S, Kim J-Y, Choi J-S. Orofacial Muscle Strength and Associated Potential Factors in Healthy Korean Community-Dwelling Older Adults: A Pilot Cross-Sectional Study. Applied Sciences. 2024; 14(22):10560. https://doi.org/10.3390/app142210560
Chicago/Turabian StyleLee, Da-Som, Ji-Youn Kim, and Jun-Seon Choi. 2024. "Orofacial Muscle Strength and Associated Potential Factors in Healthy Korean Community-Dwelling Older Adults: A Pilot Cross-Sectional Study" Applied Sciences 14, no. 22: 10560. https://doi.org/10.3390/app142210560
APA StyleLee, D.-S., Kim, J.-Y., & Choi, J.-S. (2024). Orofacial Muscle Strength and Associated Potential Factors in Healthy Korean Community-Dwelling Older Adults: A Pilot Cross-Sectional Study. Applied Sciences, 14(22), 10560. https://doi.org/10.3390/app142210560







