Abstract
This scoping review aims to provide a comprehensive summary of the current literature on 3D-printed orthodontic aligners. It was conducted following the Preferred Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines. An electronic literature search was conducted across the PubMed, Embase, and Web of Science databases. After applying the inclusion criteria, a total of 46 eligible studies published until September 2024 were selected for qualitative synthesis. To date, scientific evidence is primarily available for Tera Harz TC (Graphy, Seoul, Republic of Korea), which is the only studied material approved for orthodontic tooth movements. Although additional materials were identified during the literature search, there is a lack of scientific studies regarding their characteristics and clinical use. This review highlights that while material properties and biocompatibility are of critical importance, the clinical efficacy and long-term safety of 3D-printed aligners require further investigation. Many studies exhibit significant variability in testing methodologies, making substantiated comparisons challenging. Moreover, the existing literature primarily comprises in vitro studies, with limited clinical trials assessing the effectiveness of 3D-printed aligners. Given the current gaps in knowledge and the evolving nature of this field, further well-designed controlled clinical studies are necessary to evaluate the clinical performance and safety of 3D-printed aligners. The findings underscore the need for standardized protocols and comprehensive reporting to enhance the reliability of future research in this area.
1. Introduction
As the number of adults undergoing orthodontic treatment is steadily increasing, there is a high demand for less visible treatment options [1,2]. Aligners are transparent, less-visible, removable orthodontic appliances that can be used for the treatment of malocclusions by splitting the movement into various steps. The principle is based on the idea of Kesling in 1945 of moving teeth with removable thermoplastic positioners [3]. Although their clinical efficiency remains limited compared to fixed orthodontic appliances, the introduction of auxiliaries such as attachments and the development of specific treatment protocols for different malocclusions have significantly improved clinical outcomes [4,5,6]. One considerable option is to outsource the set-up (treatment planning) and aligner production to a company [7]. The fast and continuous development of digital technologies in terms of the wide availability of intraoral scanners and the development of appropriate software and 3D printing technologies offer new opportunities to realize the whole workflow in-house [8]. As the state of the art, aligners are manufactured by vacuum-forming thermoplastic sheets over a series of printed models, each representing incremental tooth movements towards the planned outcome [9]. These sheets can be made of polyethylene terephthalate glycol (PETG), polyurethane (PU), or polyethylene (PE) and can be single, double, or triple-layer sheets [10,11]. In recent years, significant advancements have been achieved in the field of additive manufacturing (3D printing), enabling the precise manufacturing of a wide range of materials. In contrast to traditional methods, direct 3D printing of orthodontic aligners represents a new approach in aligner manufacturing that does not require models or a thermoforming process [12]. Initial reports explored the possibility of digitally designing aligners and directly printing them using splint materials [13]. However, the materials were not approved or authorized to perform orthodontic tooth movements. The first scientific studies investigating an approved material for orthodontic aligner treatments, Tera Harz TC-85 (Graphy, Seoul, Republic of Korea), were published in 2022 [14,15]. Many potential advantages of direct 3D printing of orthodontic aligners compared to conventional thermoforming techniques have been suggested [12]. In contrast to thermoforming techniques, it might be possible to control and adjust the aligner thickness individually regarding biomechanical considerations as with different thicknesses the exerted force can be influenced [16]. For direct aligner printing, new materials with shape memory behaviors, so-called 4D printing, have been introduced, which could enable higher thresholds for tooth movement per aligner [17,18,19]. Shape memory polymers (SMPs) are able to alter their macroscopic shape upon a stimulus such as a temperature change [20]. The model-free manufacturing process is potentially more cost-effective and ecological [12,20]. However, there are concerns, particularly regarding biocompatibility, as unprocessed resins are highly toxic, and adverse effects such as possible allergic reactions have been reported [20,21]. While scientific evidence on 3D-printed aligners remains limited, especially regarding clinical trials, the literature on this topic is quickly growing, with new insights from both clinical and experimental studies. This scoping review offers a comprehensive summary of the existing literature on 3D-printed aligners, aiming to enhance understanding of the present state of research by identifying gaps and highlighting potential areas for future investigation.
2. Materials and Methods
This review design adheres to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) [22]. Additionally, Arksey and O’Malley’s framework [23] and the Joanna Briggs Institute (JBI) Reviewer’s Manual for conducting scoping reviews [24] were consulted during the manuscript preparation process.
2.1. Eligibility Criteria
The following selection criteria were applied:
Studies of all designs with the primary aim of investigating any usage of 3D-printed aligners in orthodontics. Due to the novelty of the topic, case series and in vitro studies were included in the qualitative analysis. However, case reports, editorials, and conference abstracts were excluded. Only peer-reviewed manuscripts available in the English language were included.
2.2. Search Strategy and Selection of Evidence
An electronic search was conducted in the PubMed, Embase, and Web of Science databases. The following search strategy was used with specific adaptation for each database (Table 1): (“3D-printed retainer” OR “Three-dimensional printed retainer*” OR “clear orthodontic retainers” OR aligner) AND (4D OR 3D OR dimensional) and (print* OR digital framework OR additive manufacturing). Sets of records from each database were downloaded to the bibliographic software package EndNote® X9.3.1 (Clarivate Analytics, Philadelphia, PA, USA) and merged into one core database to remove duplicates. Additionally, the reference lists of the relevant studies were screened, and the citations were tracked to identify further eligible studies. The last search update was performed on 12 September 2024.

Table 1.
Search strategies with specific adaptations.
Two reviewers (RJ and HS) independently screened the results for relevant titles, keywords, and abstracts. Full texts of the selected studies were then obtained and evaluated for eligibility based on predefined selection criteria by the same reviewers. After full-text reading, the articles not fulfilling the inclusion criteria were excluded, while the remaining were considered for data extraction. Disagreements during the two-stage screening process were resolved by re-reading the studies. If disagreements persisted, an independent third reviewer (MJ) validated the final decision.
2.3. Data Collection Process
The data were collected using a pre-tailored data extraction table. The extracted data included details on study design, primary objectives, methodology, study population, sample size, outcome measures, and key findings related to the research questions. The data collection was performed independently by two reviewers (RJ and HS). Any disagreements between the two reviewers were discussed until a unified decision was reached. Persisting disagreements were resolved via independent validation by a third reviewer (MJ).
2.4. Quality Appraisal and Risk of Bias Assessment
Quality appraisals and risk of bias assessments are optional when conducting a scoping review [22,23] and are typically not performed. As the eligible studies were expected to include various study designs, no quality appraisal or risk of bias assessment was performed.
2.5. Summary Measures and Synthesis of the Results
To address the variations in study design across the included literature, a structured approach was adopted to facilitate comparability. Studies were categorized according to the type of research topic and study design as follows: review articles, clinical studies, and experimental studies on mechanical properties, manufacturing, biocompatibility, and biomechanics. The analysis of the included studies is presented in a narrative form and a structured form and categorized by topic.
3. Results
3.1. Overview of Included Studies
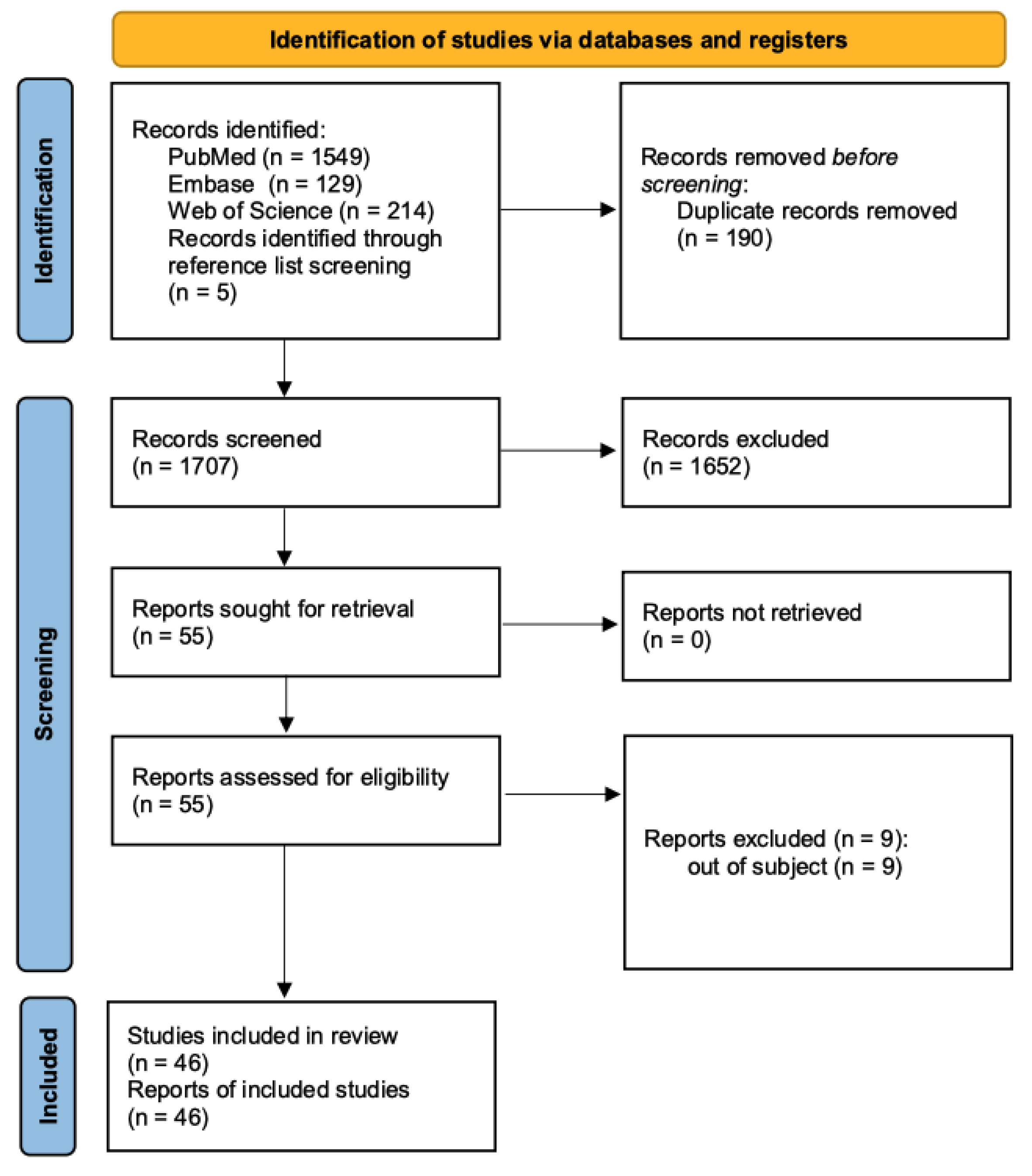
The study selection process is summarized in a PRISMA 2020 flow diagram (Figure 1) [25]. After removing duplicates, the finalized search strategy identified 1674 unique studies. Five additional articles were found through manual searches of specific journals or reference chaining. After title and abstract screening of the remaining records, 55 studies were assessed for eligibility through full-text reading, leading to the exclusion of 13 articles in accordance with the pre-established exclusion criteria. Ultimately, 44 studies were included in this review for data extraction.
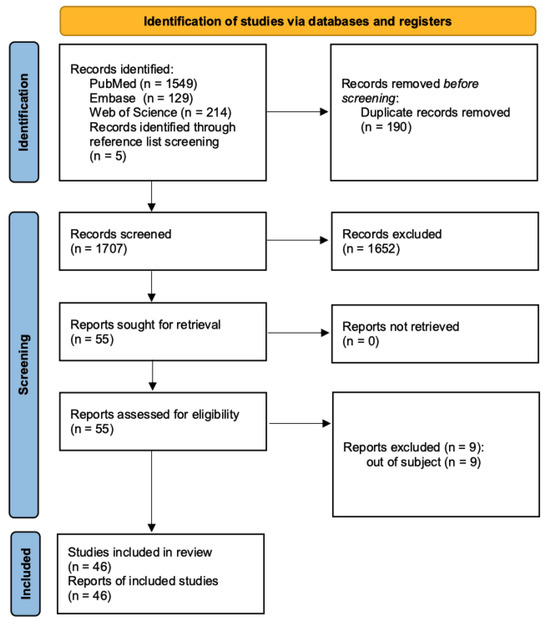
Figure 1.
PRISMA flow diagram.
3.2. Summary of Findings
3.2.1. Review Articles
Of the included review articles, all seven were categorized as narrative reviews, while no scoping or systematic reviews were identified. The earliest reviews focused on introducing the topic, describing the possibility and development of the direct aligner printing process, as well as summarizing the available articles; mostly experimental studies and reports [12,26].
As of the year 2023, no reviews on materials approved for aligner therapy were available. More recent reviews include studies on the material Tera Harz TC-85 (Graphy, Seoul, Republic of Korea), the first approved 3D-printable material to produce aligners for orthodontic treatments involving tooth movements [27,28,29,30]. The most current review included studies up to the year 2023 [30].
The objectives, characteristics, and key findings of the review articles are summarized in Table 2.

Table 2.
Characteristics and main findings of included review articles.
3.2.2. Clinical Trials
The identified clinical studies included four non-randomized trials and one randomized trial [8,16,31,32]. The characteristics and main findings of the included clinical studies are summarized in Table 3.

Table 3.
Characteristics and main findings of included clinical studies.
The clinical studies investigated different aspects of 3D-printed aligners in comparison with thermoformed aligners (industrial or in-house fabricated). Two clinical trials examined the impacts of in vivo ageing on mechanical properties. Can et al. investigated the impact on hardness, indentation modulus, elastic index, and chemical composition and concluded that 3D-printed aligners show higher stability compared to thermoformed aligners [8]. Sayahpour et al. concluded that some mechanical properties, such as Martens hardness and indentation modulus, were stable after one-week of in vivo ageing, whereas other variables such as indentation relaxation and elastic index were prone to ageing and showed significant differences compared to unused controls and thermoformed aligners [31].
One study investigated the effects of intraoral ageing on dimensional stability and found no significant effect for either 3D-printed or thermoformed aligners after one week of clinical use [31]. However, they observed an increased thickness of about 0.3 mm compared to the virtual design. After one week of intraoral service, a non-significant increase of about 0.1 mm was observed due to ageing and water absorption. Koletsi et al. studied the surface characteristics of 3D-printed aligners after exposition to an intraoral environment and found that they might be more prone to plaque accumulation and plaque retention due to increased material surface and thus fluid retention capacity compared to thermoformed aligners [32]. Only one study investigated the accuracy of planned tooth movements and reported an overall accuracy of 67.6%. The lowest accuracy was observed for the secondary premolar tip (17.6%), and the highest accuracy was observed for maxillary central incisor torque (100%) [33].
All available clinical trials to date used Tera Harz TC-85; however, to date, no clinical trial has studied aspects of clinical efficiency compared to thermoformed aligners.
3.2.3. Material Properties
- Mechanical properties
Five studies were identified that investigated the mechanical properties of materials for 3D-printed aligners in vitro. The characteristics and main findings of the included studies are summarized in Table 4.

Table 4.
Characteristics and main findings of included studies on mechanical properties.
Test specimens made from Tera Harz TC were able to adapt and activate their shape memory effect under common oral conditions; therefore, they might adapt better to the teeth and better maintain the force level [34]. Compared to thermoformed aligners, they are less stiff under oral conditions. The microhardness of all the tested materials was comparable [34].
Directly printed aligners that were made from Dental LT clear resin (Formlabs, Somerville, MA, USA) and suitably cured showed higher load resistance and lower deformation under compression testing than thermoformed ones (Duran, Scheu, Iserlohn, Germany) [13].
Apart from Tera Harz TC and Dental LT clear resin, other materials for direct printed aligners that were found in the literature included Material X (Envisiontec, Inc.; Dearborn, MI, USA) and OD-Clear TF (3DResyns, Barcelona, Spain). The vacuum-formed aligner materials provided by Align technology (EX30 and LD30, both Align technology, San Jose, CA, USA) showed better mechanical properties than OD-Clear TH in vitro, irrespective of wet or dry testing. The elastic modulus of Material X and LD30 were affected and different by dry or wet environments, respectively [35]. In particular, the residual stress levels of the thermoformed materials were higher than those of the printed materials [35].
Ultimate tensile strength is a parameter that is not so commonly investigated. It describes the stress that results in the rupture of the material tested. Compared to the materials used by Align Technologies, Material X and OD-Clear TH show in vitro lower ultimate tensile strength [35].
Lee et al. investigated various properties of Tera Harz TC compared to a PETG thermoformed material (Easy-Vac gasket, 3A, Medes (Goyang-si, Republic of Korea)) [17]. They found higher yield strength and elastic modulus in the thermoformed group and higher elastic range in the Tera Harz TC group. Tera Harz TC showed higher stress relaxation but maintained the force level after 13 cyclic loads. The amount of stress relaxation in the thermoformed group was smaller and was constant after 13 cyclic loads. In contrast to the thermoformed test specimens, the Tera Harz TC regained its shape after bending at 37 °C, which reflects intraoral conditions. Under the same conditions, the thermoformed material’s deformation was persistent [17].
- Esthetic properties
As aligners are considered to be more esthetic treatment options, the translucency of the material is an important factor. Three studies on esthetic properties were found.
According to Park et al., Tera Harz TC had lower translucency values after isopropyl alcohol (IPA) cleaning, whereas Tera Harz TC after centrifugation was as translucent as the thermoformed materials (Duran, Scheu and CaPro, Scheu, Iserlohn, Germany) [36]. Kim et al. found no difference in translucency after various cleaning processes after printing TC-85 including IPA and centrifugating it at different temperatures and centrifugation times. Only the group without any cleaning appeared to be hazy [37]. Compared to thermoformed aligner materials, 3D-printed ones (Tera Harz TC, and Clear-A, Senertek, Izmir, Turkey) were less resistant to staining and chemical alterations [38].
- Fitting and Thickness
Precise thickness and a good fit are also important factors to consider. Six studies on this topic were identified.
Park et al. found that, in general, the thickness varied in the two thermoformed materials (Duran, Scheu and CaPro, Scheu) and also in the printed groups (Tera Harz TC cleaned with isopropyl alcohol and Tera Harz TC centrifuged). Furthermore, Migliorati et al. (2023) confirmed significant differences in aligner thickness values at different measurement locations within aligners [39]. The thermoformed materials showed lower thicknesses after manufacturing, and the printed ones exhibited an increase in thickness. The authors also found that the thickness was affected by post-processing [36]. The increase in thickness seems to be irrespective of the resin and is in accordance with the findings of Lee at al. (2022) [17] and Edelmann et al. [40].
Dimensional accuracy is a commonly investigated and clinically important property. Considering the geometric accuracy, 3D-printed aligners (Dental LT clear) were superior compared to thermoformed ones made of Duran [13] or Invisacryl Ultra thermal forming material (Great Lakes Dental Technologies, Tonawanda, NY, USA) [41]. This was also true for the Tera Harz TC aligner material, which provided a higher accuracy compared to both Zendura FLX (Zendura Dental, Fremont, CA, USA) and Essix ACE (Dentsply Sirona, Sarsota, FL, USA) [15]. According to Park et al., the lowest gap and therefore the best fit width was found in the multilayer thermoformed group (CaPro) [36].
3.2.4. Impact of Manufacturing on Mechanical Properties and Dimensional Accuracy
Nine studies investigated the impact of different manufacturing parameters on aligner properties. The characteristics and main findings of the included studies on the impact of manufacturing are summarized in Table 5.
Printing at 90° was recommended by Boyer et al. (2021) as being most exact considering dimensional accuracy [42], whereas other authors could not find an impact of print orientation on accuracy [43].
With respect to Tera Harz TC, the recommended post-processing protocol consists of centrifugation, two times for 3 min, and curing in an oxygen-devoid environment (nitrogen) [44]. Washing in ethanol (90%) for 30 s followed by the same curing process (nitrogen) resulted in similar material properties [44]. Different protocols for cleaning (washing in ethanol or IPA for 30 s or washing in IPA for 15 s and distilled water for 15 s) and curing (air) had a negative impact on the flexural modulus and hardness [44] but no impact on the local aligner thickness [39]. Nonetheless, the results highlighted the importance of polymerization under N2 conditions.
The highest degree of conversion was found in the recommended post-processing group, but with no statistically significant differences compared to the other groups [44]. Looking again at different cleaning methods after printing followed by curing under N2, Kim et al. found no significant influence of cleaning methods and centrifugation time on the shape recovery of Tera Harz TC [37].
According to McCarty et al. (2020), the duration of ultraviolet curing did not influence the accuracy of 3D-printed aligners; therefore, the shorter time duration might be suitable [43].
Jindal et al. investigated the effects of temperatures and time durations of curing in the curing chamber after washing in IPA and drying with compressed air on the compressive resistance and modulus ratio of the Dental LT clear material. They found that all of the different curing conditions resulted in elastic deformation and sustaining a compressive load between 495 and 666N and concluded that appropriate compressive strength could be achieved with a lower temperature and time duration [13].
Storage in ambient air after manufacturing improved the mechanical properties of the same material (Dental LT clear), with the best performance attained after 7 days. The authors recommend giving the aligners to the patients after 7 days of storage [45].
Two studies investigated the impact of 3D printing systems on the mechanical properties of directly printed aligners, and both concluded that different print technologies or even different printers have an influence on the mechanical properties. Therefore, differences in terms of clinical efficacy are to be expected [14,46].

Table 5.
Characteristics and main findings of included studies on the impact of manufacturing.
Table 5.
Characteristics and main findings of included studies on the impact of manufacturing.
| Author, Year | Materials | Mechanical Properties | Printing Direction | Post-Processing | Key Findings |
|---|---|---|---|---|---|
| Jindal et al., 2020 [47] | Dental LT clear | Compressive resistance, modulus ratio | 25° | Washing IPA, air drying, or using compressed air; curing chamber at (a) 80 °C, 20 min; (b) 80 °C, 10 min.; (c) 80 °C, 5 min; (d) 60 °C, 20 min; (e) 40 °C, 20 min; (f) uncured | All curing conditions resulted in elastic deformation, sustaining compressive loads from 495–666N; compressive modulus ranged from 4.46 to 5.90 Appropriate compressive strength could be achieved with a lower temperature and time duration |
| Milovanovic et al., 2021 [45] | Dental LT clear | Tensile, compressive, and three-point bending test after 24 h, 72 h, 120 h, and 168 h of storage at room temperature | Unknown | Rinsing in 99.5% IPA two times for 10 min., drying at room temperature for 40 min, UV post-curing according to the recommendation of Formlabs | Mechanical properties changed with storage time, best performances were expected after 7 days of storage |
| Simunovic et al., 2024 [44] | Tera Harz TC | Flexural modulus, hardness testing, degree of conversion | Unknown | (a) Centrifugation, 2 × 3 min (b) Washed in ethanol (90%), 30 s (c) Washed in IPA, 30 s (d) Washed in IPA, 15 s + distilled water, 15 s Each either followed by polymerization (cure chamber) under ambient air or N2 | Polymerization under ambient air has a negative impact on material properties. Washing in ethanol followed by N2 curing seems to be an equivalent alternative, achieving comparable results Centrifugation + N2 showed the highest degree of conversion, but without statistical differences across groups |
| Kim et al., 2024 [37] | Tera Harz TC | Shape recovery from stress relaxation | 45° | (a) IPA (99.5%), ultrasonic rinsed for 1 min, air drying for 5 min. (b) Centrifugation at 23 °C for 2, 4, and 6 min (c) Centrifugation at 55 °C for 2, 4, and 6 min All followed by 20 min curing under N2 | No impact on shape recovery |
| Zinelis et al., 2022 [14] | Tera Harz TC | Martens hardness, indentation modulus, elastic index | Vertical | Different printers and printing technologies were used. Centrifuged for 3 min, cured for 10 min according to manufacturer’s guidelines | Mechanical properties were dependent on 3D printers |
| Bhardwaj et al., 2024 [46] | Not specified | Martens hardness, indentation modulus, elastic index | Vertical | Different printers and printing technologies were used. Centrifuged for 3 min, cured for 10 min according to manufacturer’s guidelines | Mechanical properties were dependent on 3D printers |
| Boyer et al., 2021 [42] | Grey V4 | 3D deviation analysis | Horizontal 45° Vertical 135° Horizontal upside down 225° Vertical upside down 315° | 2 successive baths of IPA <99% (1 and 10 min), compressed air, drying for 30 min, curing at 60 °C for 30 min | 90° printing orientation showed the highest accuracy |
| McCarty et al., 2020 [43] | Dental LT Clear | 3D deviation analysis | Horizontal 45° Vertical | IPA > 96% 2 min., second IPA bath and sonicated 3 mm (a) no curing or UV light (b) 20 min. UV light at 80 °C (c) 40 min. UV light at 80 °C | Print orientation and curing duration had little effect on dimensional accuracy |
| Migliorati et al., 2023 [39] | Tera Harz TC | Thickness measurement (micro-CT) | 60° | Centrifuged for 5 min+ curing: (a) 15 min under N2 (b) 20 min under N2 (c) 25 min under N2 (d) 30 min under N2 (e) 40 min under N2 (f) 50 min under N2 (g) 30 min Storage in boiling water (100 °C) for 2 min | N2 had a significant effect on thickness; curing time and thickness were not associated |
3.2.5. Biocompatibility
Eight included studies investigated aspects of biocompatibility. The characteristics and main findings of the included studies on biocompatibility are summarized in Table 6. Willi et al. found a high C-C conversion and no BPA release but detected significant urethane dimethacrylate (UDMA) concentrations in water eluents after one week of storage at 37°, raising concerns regarding potential biological reactivity [21]. Three-dimensionally printed aligners were found to be less stain resistant and more susceptible to color changes, and signs of chemical alterations after up to one week of experimental storage in different agents was observed [38]. Pratisinis et al. found no influence on the viability of human gingival fibroblast cells exposed to 3D-printed aligner water eluates, no stimulatory or inhibitory effect on intracellular reactive oxygen species levels, and no xenoestrogenic activity [48]. In contrast, Iodice et al. found a significant cytotoxic effect on cell growth after 72 h. A moderate level of cytotoxicity was detected irrespective of the curing time after immersion in human saliva [49].
One study investigated the addition of chitosan nanoparticles to a printable resin and its effects on cytotoxicity and biofilm formation. However, the material was not approved for orthodontic aligner therapy [50].

Table 6.
Characteristics and main findings of included studies on biocompatibility.
Table 6.
Characteristics and main findings of included studies on biocompatibility.
| Author, Year | Objective | Study Design | Material(s) Investigated | Intervention Method | Primary Outcomes | Key Findings |
|---|---|---|---|---|---|---|
| (Kumar 2019) [51] | To evaluate the cytotoxicity of 3D-printed materials compared to thermoformed aligners | In vitro (cell culture) | Tera Harz TC85A resin Invisalign®, Dental LT®, Accura 60® | Cell viability after exposure to 3D-printed aligners using MTT assay over four time intervals (days 1, 3, 5, 7). | Cell viability | Invisalign® showed the least cytotoxicity, while Accura 60® was the most cytotoxic; toxicity decreased over time for all materials |
| Pratsinis et al. (2022) [48] | To assess the cytotoxicity, antioxidative activity, and estrogenicity of 3D-printed aligners | In vitro (Cell culture) | Tera Harz TC85A resin | Ten sets of aligners immersed in sterile deionized water for 14 days, followed by MTT assays and E-screen tests on human gingival fibroblasts and breast cancer cell lines, ROS assay | Cell viability, intracellular ROS levels, estrogenicity | No cytotoxicity or estrogenic effects observed; no significant ROS changes detected |
| (Raszewski et al. 2022) [52] | To evaluate mechanical properties and biocompatibility of 3D-printed aligner material with bioactive components | In vitro (cell culture) | 3D-printed acrylic material with Biomin C bioactive glass | Addition of bioactive glasses (Biomin C) to acrylic monomers, followed by 3D printing and testing for ion release, flexural strength, and cytotoxicity | Ion release, cell viability | Released Ca2+ and PO43− ions for 42 days. 10% Biomin C samples showed >85% cell viability |
| (Taher and Rasheed 2023) [50] | To examine the impact of chitosan nanoparticles on the biocompatibility of 3D-printed aligners | In vitro | 3D-printed acrylic resin (unspecified) | 3D-printed aligners with varying concentrations of chitosan nanoparticles (2%, 3%, 5%) | Cell viability and antibiofilm activity | Chitosan-modified aligners showed significant antibiofilm activity and no cytotoxicity at concentrations of up to 5% |
| (Nakano et al. 2019) [53] | To develop biocompatible resins for 3D printing of direct aligners with optimized safety profiles and mechanical properties | In vitro | Acrylic-epoxy hybrid light-curing resin | Cytotoxicity (LDH test), proliferation (WST1 test), and mechanical testing of acrylic-epoxy hybrid light-curing resins | Cell viability, mechanical properties | Low cytotoxicity was observed, but 3D-printed aligners were fragile in the middle section, indicating the need for improved mechanical properties before clinical application |
| (Willi et al. 2023) [21] | To quantitatively assess leaching from a 3D-printed aligners | In vitro | Tera Harz TC85A resin | Aligner samples immersed in double-distilled water for 1 week at 37 °C; eluates analyzed for UDMA and BPA using liquid chromatography/mass spectrometry | Detection levels of UDMA and BPA in water eluents | UDMA was detected in all samples, whereas BPA was not detected. Potential concerns were raised due to variability in UDMA leaching |
| (Simunovic et al. 2024) [38] | To evaluate the color and chemical stability of 3D-printed aligners exposed to various beverages | In vitro | Tera Harz TC85A resin | Aligner samples exposed to coffee, tea, and red wine for 14 days, with color change measured using the NBS rating system, chemical changes via ATR-FTIR spectroscopy | Color stability, chemical stability | Significant color change observed in aligner samples exposed to red wine. Minor chemical alterations were detected |
| (Iodice et al. 2024) [49] | To investigate the cytotoxicity of 3D-printed aligners under different curing times | In vitro | Tera Harz TC85A resin | Cell viability assessed after exposure to 3D-printed aligners produced using different curing times | Cell viability after exposure to 3D-printed aligners | Cytotoxicity correlated with longer curing times. Saliva influenced cell viability results |
3.2.6. Biomechanics
Three studies investigated biomechanical aspects in terms of force and moment generation or FEM analysis. Forces and moments generated in vitro by directly printed Aligners from TC-85 (Graphy) were found to be lower, more consistent, and predictable compared to thermoformed Aligners made from ATMOS (American Orthodontics, Sheboygan, WI, UAS) or Zendura FLX (Bay Materials, Fremont, CA, USA) [54]. Grant et al. measured in vitro forces and moments generated by TC-85 printed aligners and found that variations in thickness changed the amount of force and moments, but in a complex and unpredictable pattern. Nevertheless, they concluded with the possibility to improve anchorage by increasing aligner thickness where anchorage is needed, therefore reducing side effects [55].
The mechanical behavior using a Finite Element Analysis (FEA) of directly printed aligners (Dental LT resin, Formlabs (Somerville, MA, USA)) compared to vacuum formed ones (Duran and Durasoft, both Scheu (Iserlohn, Germany)) seemed to be comparable in terms of stress distribution, whereas the geometrical accuracy was higher in the directly printed material [47].
4. Discussion
This scoping review provides an updated summary of the current literature on in vitro and clinical studies, as well as existing review articles on 3D-printed aligners. Recent research has expanded significantly, covering various aspects of this novel approach for aligner manufacturing. In comparison to previous reviews, which provided narrative overviews of selected studies, this scoping review is the first to use a structured search strategy to systematically identify the available evidence regarding 3D-printed aligners and includes studies up to September 2024.
To date, scientific data are only available for one material that has been approved to perform orthodontic tooth movements or aligner treatments, Tera Harz TC (Graphy, Seoul, Republic of Korea). Although other approved materials indicated for aligner manufacturing, such as Dental Clear Aligner (DCA, LuxCreo Inc., Chicago, IL, USA), were identified while conducting this review, no scientific studies were available. Other frequently studied materials, such as Dental LT clear (Formlabs, Somerville, MA, USA), are approved for intraoral use but are not intended to perform tooth movements. As more materials are expected to be approved or authorized for this indication, investigations of non-approved materials regarding aligner therapy do not appear to be justified, except for regulatory studies.
The most prevalently studied aspect of 3D-printed aligners is the evaluation of their material properties. Numerous studies have investigated the mechanical characteristics of 3D-printed aligner materials compared to thermoformed ones, such as shape recovery, hardness, and thickness. These properties may directly affect the performance of aligners in clinical settings. In terms of dimensional accuracy, the current evidence suggests that 3D-printed materials seem to be superior to thermoformed appliances [13,15]. However, there was an overall increase in the dimensions of the 3D-printed aligners compared to the virtually planned dimensions [13,15].
Relaxation was found to be higher for 3D-printed Tera Harz TC than in the thermoformed group [17]. Relaxation is a commonly investigated parameter to evaluate the material’s ability to maintain the force level and should therefore be low. Shape recovery seems to be superior in aligners printed using Tera Harz TC compared to thermoformed ones [17]. Given the heterogeneity of available studies, the results are not comparable given the various investigated parameters using different methodologies.
The idea to vary aligner thickness depending on whether movement or anchorage is needed [55] is interesting. But, it needs to be borne in mind that integrating this aspect is very complex, and it becomes even more complex with increasing numbers of teeth that need to be moved. Furthermore, there is agreement in the available literature that thickness increases during the printing process [17,36,40]. In general, manufacturing techniques, including the 3D printing process, the printer itself, and post-processing procedures, have been identified as critical factors not only for ensuring the material properties [14,46] but also for achieving high monomer conversion. It should be noted that the manufacturer’s recommendation for post-processing of Tera Harz TC-85 has changed since its introduction to the market. Post-processing plays a crucial role in reducing the risk of adverse effects associated with residual monomers, particularly UDMA, as these substances may pose biocompatibility concerns [21]. Interestingly, extended post-curing time was shown to positively correlate with cytotoxicity [49]. Validated protocols and the manufacturers’ recommendations should be strictly followed during production of 3D printed aligners. Biocompatibility is a central consideration when evaluating materials for intraoral use, especially for 3D-printed aligners, since 3D-printable resins are highly toxic before printing and post-processing [56]. An ideal aligner material would exhibit no carcinogenic, teratogenic, cytotoxic, or genotoxic characteristics. This is particularly important because aligners are usually changed every week or every two weeks over a period of several months, resulting in an increased cumulative dose of potentially harmful substances compared to other 3D-printed appliances such as orthodontic retainers or occlusal splints [21]. With an average of between 60 and 80 aligners observed per case, the cumulative effects are of particular concern [57]. In addition, potentially toxic levels might be underestimated given the use in a clinical environment and oral conditions that may influence material behavior [32]. Reports on adverse effects such as oral mucosa irritation and swelling have been observed and should be reported in future studies [49]. Further biocompatibility studies are needed to examine cumulative dose aspects and should include long-term cell viability tests and extended observational clinical studies.
In addition to in vitro studies, the first results of clinical studies were included in this review, although only one pilot study investigated the clinical efficiency in terms of the accuracy of orthodontic tooth movements [33]. Migliorati et al. found that 3D-printed aligners made from Tera Harz TC-85 showed a promising overall accuracy of 67.6%, but the accuracy of certain directions was considerably lower, such as the accuracy of secondary premolar tip movements, which was reported as 17.6%. Further, well-designed clinical studies are necessary to draw conclusions on the clinical effectiveness of 3D-printed aligners. Considering the limitations of the existing studies, the included review articles were all narrative, potentially introducing selection bias. Especially regarding the clinical studies, there are limitations to be aware of. Most of them are in vitro studies of mechanical behaviour after intraoral service. Only Migliorati et al. (2024) investigated the clinical outcomes of aligner treatment, but they used a small sample size and no control group. In general, many studies are not comparable, since many different parameters were investigated. There is only one study that compared 3D-printed aligner material to triple-layer sheets, although they should be the reference, as they seem to be superior in comparison to single-layer sheets [58].
5. Implications for Clinical Practice and Research
The potential of 3D-printed clear aligners to enhance customization and improve sustainability and efficiency in orthodontic treatment is significant. Yet, the effectiveness and biocompatibility of these appliances remain a critical area for further investigation. Clinicians using 3D-printed aligners should be aware that current evidence on the practical effectiveness of these appliances is sparse, and the rapidly evolving research should be closely followed. For example, manufacturer recommendations for the fabrication protocol of materials like Tera-Harz have already changed since their initial introduction. With the increasing number of available studies and their variability, the need for standardized protocols and detailed reporting in future research has become apparent. Due to the heterogeneity of the available studies and the methods used, it is not possible to draw substantiated conclusions about most of the aspects investigated, including a comparison of the efficacy and safety of thermoformed and 3D-printed aligners. Well-designed randomized controlled studies are imperative regarding clinical efficiency, tooth movement accuracy, and adverse effects.
6. Conclusions
Although the available evidence on 3D-printed aligners is rapidly increasing, particularly in terms of material properties and biocompatibility, there are still significant research gaps regarding their clinical performance and safety. Further research, particularly randomized controlled clinical trials, are essential to assess their benefits and disadvantages in comparison to thermoformed aligners and to eventually enable the safe and predictable application of this technology.
Author Contributions
R.J.: Reviewer 1, investigation, writing—original draft preparation; K.B.: conceptualization, supervision, writing—review and editing; M.J.R.: methodology, validation, data curation, writing—original draft preparation, visualization; H.S.: Reviewer 2, investigation, writing—original draft preparation. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Melsen, B. Northcroft lecture: How has the spectrum of orthodontics changed over the past decades? J. Orthod. 2011, 38, 134–143. [Google Scholar] [CrossRef] [PubMed]
- Rosvall, M.D.; Fields, H.W.; Ziuchkovski, J.; Rosenstiel, S.F.; Johnston, W.M. Attractiveness, acceptability, and value of orthodontic appliances. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 276.e1–276.e12, Discussion 276–277. [Google Scholar] [CrossRef] [PubMed]
- Kesling, H.D. The philosophy of the tooth positioning appliance. Am. J. Orthod. Oral. Surg. 1945, 31, 297–304. [Google Scholar] [CrossRef]
- AlMogbel, A.; Alshawy, E.S.; Alhusainy, A. Efficacy of clear aligner therapy over conventional fixed appliances in controlling orthodontic movement: A systematic review. J. Orthod. Sci. 2024, 13, 23. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.K.; Kanwal, B.; Shqaidef, A.; Alswairki, H.J.; Alfawzan, A.A.; Alabdullatif, A.I.; Aalmunif, A.N.; Aljrewey, S.H.; Alothman, T.A.; Shrivastava, D.; et al. A Systematic Review and Network Meta-Analysis on the Impact of Various Aligner Materials and Attachments on Orthodontic Tooth Movement. J. Funct. Biomater. 2023, 14, 209. [Google Scholar] [CrossRef] [PubMed]
- Jedliński, M.; Mazur, M.; Greco, M.; Belfus, J.; Grocholewicz, K.; Janiszewska-Olszowska, J. Attachments for the Orthodontic Aligner Treatment-State of the Art-A Comprehensive Systematic Review. Int. J. Env. Res. Public. Health 2023, 20, 4481. [Google Scholar] [CrossRef]
- Kuo, E.; Miller, R.J. Automated custom-manufacturing technology in orthodontics. Am. J. Orthod. Dentofac. Orthop. 2003, 123, 578–581. [Google Scholar] [CrossRef]
- Can, E.; Panayi, N.; Polychronis, G.; Papageorgiou, S.N.; Zinelis, S.; Eliades, G.; Eliades, T. In-house 3D-printed aligners: Effect of in vivo ageing on mechanical properties. Eur. J. Orthod. 2022, 44, 51–55. [Google Scholar] [CrossRef]
- Sabbagh, H.; Heger, S.M.; Stocker, T.; Baumert, U.; Wichelhaus, A.; Hoffmann, L. Accuracy of 3D Tooth Movements in the Fabrication of Manual Setup Models for Aligner Therapy. Materials 2022, 15, 3853. [Google Scholar] [CrossRef]
- Golkhani, B.; Weber, A.; Keilig, L.; Reimann, S.; Bourauel, C. Variation of the modulus of elasticity of aligner foil sheet materials due to thermoforming. J. Orofac. Orthop. 2022, 83, 233–243. [Google Scholar] [CrossRef]
- Daniele, V.; Macera, L.; Taglieri, G.; Spera, L.; Marzo, G.; Quinzi, V. Color Stability, Chemico-Physical and Optical Features of the Most Common PETG and PU Based Orthodontic Aligners for Clear Aligner Therapy. Polymers 2021, 14, 14. [Google Scholar] [CrossRef] [PubMed]
- Tartaglia, G.M.; Mapelli, A.; Maspero, C.; Santaniello, T.; Serafin, M.; Farronato, M.; Caprioglio, A. Direct 3D Printing of Clear Orthodontic Aligners: Current State and Future Possibilities. Materials 2021, 14, 1799. [Google Scholar] [CrossRef] [PubMed]
- Jindal, P.; Juneja, M.; Siena, F.L.; Bajaj, D.; Breedon, P. Mechanical and geometric properties of thermoformed and 3D printed clear dental aligners. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 694–701. [Google Scholar] [CrossRef] [PubMed]
- Zinelis, S.; Panayi, N.; Polychronis, G.; Papageorgiou, S.N.; Eliades, T. Comparative analysis of mechanical properties of orthodontic aligners produced by different contemporary 3D printers. Orthod. Craniofac Res. 2022, 25, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Koenig, N.; Choi, J.Y.; McCray, J.; Hayes, A.; Schneider, P.; Kim, K.B. Comparison of dimensional accuracy between direct-printed and thermoformed aligners. Korean J. Orthod. 2022, 52, 249–257. [Google Scholar] [CrossRef]
- Sayahpour, B.; Eslami, S.; Stuhlfelder, J.; Buhling, S.; Dahmer, I.; Goteni, M.; Kopp, S.; Nucci, L. Evaluation of thickness of 3D printed versus thermoformed aligners: A prospective in vivo ageing experiment. Orthod. Craniofac Res. 2024, 27, 831–838. [Google Scholar] [CrossRef]
- Lee, S.Y.; Kim, H.; Kim, H.J.; Chung, C.J.; Choi, Y.J.; Kim, S.J.; Cha, J.Y. Thermo-mechanical properties of 3D printed photocurable shape memory resin for clear aligners. Sci. Rep. 2022, 12, 6246. [Google Scholar] [CrossRef]
- Kantaros, A.; Ganetsos, T.; Petrescu, F.I.T. Transforming Object Design and Creation: Biomaterials and Contemporary Manufacturing Leading the Way. Biomimetics 2024, 9, 48. [Google Scholar] [CrossRef]
- Kantaros, A.; Ganetsos, T. From Static to Dynamic: Smart Materials Pioneering Additive Manufacturing in Regenerative Medicine. Int. J. Mol. Sci. 2023, 24, 15748. [Google Scholar] [CrossRef]
- Bichu, Y.M.; Alwafi, A.; Liu, X.; Andrews, J.; Ludwig, B.; Bichu, A.Y.; Zou, B. Advances in orthodontic clear aligner materials. Bioact. Mater. 2023, 22, 384–403. [Google Scholar] [CrossRef]
- Willi, A.; Patcas, R.; Zervou, S.K.; Panayi, N.; Schatzle, M.; Eliades, G.; Hiskia, A.; Eliades, T. Leaching from a 3D-printed aligner resin. Eur. J. Orthod. 2023, 45, 244–249. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Bmj 2021, 372, n71. [Google Scholar] [CrossRef]
- Maspero, C.; Tartaglia, G.M. 3D Printing of Clear Orthodontic Aligners: Where We Are and Where We Are Going. Materials 2020, 13, 5204. [Google Scholar] [CrossRef]
- Goracci, C.; Juloski, J.; D’Amico, C.; Balestra, D.; Volpe, A.; Juloski, J.; Vichi, A. Clinically Relevant Properties of 3D Printable Materials for Intraoral Use in Orthodontics: A Critical Review of the Literature. Materials 2023, 16, 2166. [Google Scholar] [CrossRef]
- Panayi, N.C. Directly Printed Aligner: Aligning with the Future. Turk. J. Orthod. 2023, 36, 62–69. [Google Scholar] [CrossRef]
- Slaymaker, J.; Hirani, S.; Woolley, J. Direct 3D printing aligners—Past, present and future possibilities. Br. Dent. J. 2024, 236, 401–405. [Google Scholar] [CrossRef]
- Narongdej, P.; Hassanpour, M.; Alterman, N.; Rawlins-Buchanan, F.; Barjasteh, E. Advancements in Clear Aligner Fabrication: A Comprehensive Review of Direct-3D Printing Technologies. Polymers 2024, 16, 371. [Google Scholar] [CrossRef]
- Sayahpour, B.; Zinelis, S.; Polychronis, G.; Eliades, T.; Goteni, M.; Kopp, S.; Eslami, S. Effects of intraoral aging on mechanical properties of directly printed aligners vs. thermoformed aligners: An in vivo prospective investigation. Eur. J. Orthod. 2024, 46, cjad063. [Google Scholar] [CrossRef] [PubMed]
- Koletsi, D.; Panayi, N.; Laspos, C.; Athanasiou, A.E.; Zinelis, S.; Eliades, T. In vivo aging-induced surface roughness alterations of Invisalign((R)) and 3D-printed aligners. J. Orthod. 2023, 50, 352–360. [Google Scholar] [CrossRef] [PubMed]
- Migliorati, M.; Drago, S.; Castroflorio, T.; Pesce, P.; Battista, G.; Campobasso, A.; Gastaldi, G.; Valvecchi, F.F.; Mari, A. Accuracy of orthodontic movements with 3D printed aligners: A prospective observational pilot study. Korean J. Orthod. 2024, 54, 160–170. [Google Scholar] [CrossRef] [PubMed]
- Atta, I.; Bourauel, C.; Alkabani, Y.; Mohamed, N.; Kimbe, H.; Alhotan, A.; Ghoneima, A.; Elshazly, T. Physiochemical and mechanical characterisation of orthodontic 3D printed aligner material made of shape memory polymers (4D aligner material). J. Mech. Behav. Biomed. Mater. 2024, 150, 106337. [Google Scholar] [CrossRef] [PubMed]
- Shirey, N.; Mendonca, G.; Groth, C.; Kim-Berman, H. Comparison of mechanical properties of 3-dimensional printed and thermoformed orthodontic aligners. Am. J. Orthod. Dentofac. Orthop. 2023, 163, 720–728. [Google Scholar] [CrossRef]
- Park, S.Y.; Choi, S.H.; Yu, H.S.; Kim, S.J.; Kim, H.; Kim, K.B.; Cha, J.Y. Comparison of translucency, thickness, and gap width of thermoformed and 3D-printed clear aligners using micro-CT and spectrophotometer. Sci. Rep. 2023, 13, 10921. [Google Scholar] [CrossRef]
- Kim, J.E.; Mangal, U.; Yu, J.H.; Kim, G.T.; Kim, H.; Seo, J.Y.; Cha, J.Y.; Lee, K.J.; Kwon, J.S.; Choi, S.H. Evaluation of the effects of temperature and centrifugation time on elimination of uncured resin from 3D-printed dental aligners. Sci. Rep. 2024, 14, 15206. [Google Scholar] [CrossRef]
- Simunovic, L.; Cekalovic Agovic, S.; Maric, A.J.; Bacic, I.; Klaric, E.; Uribe, F.; Mestrovic, S. Color and Chemical Stability of 3D-Printed and Thermoformed Polyurethane-Based Aligners. Polymers 2024, 16, 1067. [Google Scholar] [CrossRef]
- Migliorati, M.; Drago, S.; Lagazzo, A.; Campobasso, A.; Battista, G.; Kerberger, R.; Drescher, D.; Becker, K. Effect of Curing Time and Nitrogen Generator Usage on Direct 3D-Printed Aligners Thicknesses—An In Vitro Micro-CT Study. Appl. Sci. 2023, 13, 11952. [Google Scholar] [CrossRef]
- Edelmann, A.; English, J.D.; Chen, S.J.; Kasper, F.K. Analysis of the thickness of 3-dimensional-printed orthodontic aligners. Am. J. Orthod. Dentofac. Orthop. 2020, 158, e91–e98. [Google Scholar] [CrossRef]
- Spangler, T.; Ammoun, R.; Carrico, C.K.; Bencharit, S.; Tufekci, E. The effect of crowding on the accuracy of 3-dimensional printing. Am. J. Orthod. Dentofac. Orthop. 2023, 164, 879–888. [Google Scholar] [CrossRef] [PubMed]
- Boyer, R.A.; Kasper, F.K.; English, J.D.; Jacob, H.B. Effect of print orientation on the dimensional accuracy of orthodontic aligners printed 3-dimensionally. Am. J. Orthod. Dentofac. Orthop. 2021, 160, 732–742 e731. [Google Scholar] [CrossRef] [PubMed]
- McCarty, M.C.; Chen, S.J.; English, J.D.; Kasper, F. Effect of print orientation and duration of ultraviolet curing on the dimensional accuracy of a 3-dimensionally printed orthodontic clear aligner design. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 889–897. [Google Scholar] [CrossRef] [PubMed]
- Šimunović, L.; Jurela, A.; Sudarević, K.; Bačić, I.; Haramina, T.; Meštrović, S. Influence of Post-Processing on the Degree of Conversion and Mechanical Properties of 3D-Printed Polyurethane Aligners. Polymers 2024, 16, 17. [Google Scholar] [CrossRef]
- Milovanovic, A.; Sedmak, A.; Golubovic, Z.; Mihajlovic, K.Z.; Zurkic, A.; Trajkovic, I.; Milosevic, M. The effect of time on mechanical properties of biocompatible photopolymer resins used for fabrication of clear dental aligners. J. Mech. Behav. Biomed. Mater. 2021, 119, 104494. [Google Scholar] [CrossRef] [PubMed]
- Bhardwaj, A.; Mishra, K.; Pandey, A.; Kirtiwar, D.; Kharche, A.; Agaldiviti, P. Mechanical Properties of 3D Printed Orthodontic Aligners Produced by Different Commercially Available Printers—An In-Vitro Study. J. Pharm. Bioallied Sci. 2024, 16, S1431–S1432. [Google Scholar] [CrossRef]
- Jindal, P.; Worcester, F.; Siena, F.L.; Forbes, C.; Juneja, M.; Breedon, P. Mechanical behaviour of 3D printed vs thermoformed clear dental aligner materials under non-linear compressive loading using FEM. J. Mech. Behav. Biomed. Mater. 2020, 112, 104045. [Google Scholar] [CrossRef]
- Pratsinis, H.; Papageorgiou, S.N.; Panayi, N.; Iliadi, A.; Eliades, T.; Kletsas, D. Cytotoxicity and estrogenicity of a novel 3-dimensional printed orthodontic aligner. Am. J. Orthod. Dentofac. Orthop. 2022, 162, e116–e122. [Google Scholar] [CrossRef]
- Iodice, G.; Ludwig, B.; Polishchuk, E.; Petruzzelli, R.; Di Cunto, R.; Husam, S.; Farella, M. Effect of post-printing curing time on cytotoxicity of direct printed aligners: A pilot study. Orthod. Craniofac Res. 2024. [Google Scholar] [CrossRef]
- Taher, B.B.; Rasheed, T.A. The Impact of Adding Chitosan Nanoparticles on Biofilm Formation, Cytotoxicity, and Certain Physical and Mechanical Aspects of Directly Printed Orthodontic Clear Aligners. Nanomaterials 2023, 13, 2649. [Google Scholar] [CrossRef]
- Kumar, S.M. Cytotoxicity of 3D Printed Materials: An In Vitro Study. Master’s thesis, The Tamil Nadu Dr. M.G.R. Medical University, Chennai, India, 2019. [Google Scholar]
- Raszewski, Z.; Chojnacka, K.; Kulbacka, J.; Mikulewicz, M. Mechanical Properties and Biocompatibility of 3D Printing Acrylic Material with Bioactive Components. J. Funct. Biomater. 2022, 14, 13. [Google Scholar] [CrossRef]
- Nakano, H.; Kato, R.; Kakami, C.; Okamoto, H.; Mamada, K.; Maki, K. Development of Biocompatible Resins for 3D Printing of Direct Aligners. J. Photopolym. Sci. Technol. 2019, 32, 209–216. [Google Scholar] [CrossRef]
- McKay, A.; McCray, J.; Bankhead, B.; Lee, M.M.; Miranda, G.; Adel, S.M.; Kim, K.B. Forces and moments generated during extrusion of a maxillary central incisor with clear aligners: An in vitro study. BMC Oral. Health 2023, 23, 495. [Google Scholar] [CrossRef] [PubMed]
- Grant, J.; Foley, P.; Bankhead, B.; Miranda, G.; Adel, S.M.; Kim, K.B. Forces and moments generated by 3D direct printed clear aligners of varying labial and lingual thicknesses during lingual movement of maxillary central incisor: An in vitro study. Prog. Orthod. 2023, 24, 23. [Google Scholar] [CrossRef] [PubMed]
- Reichl, F.X.; Esters, M.; Simon, S.; Seiss, M.; Kehe, K.; Kleinsasser, N.; Folwaczny, M.; Glas, J.; Hickel, R. Cell death effects of resin-based dental material compounds and mercurials in human gingival fibroblasts. Arch. Toxicol. 2006, 80, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Kravitz, N.D.; Dalloul, B.; Zaid, Y.A.; Shah, C.; Vaid, N.R. What percentage of patients switch from Invisalign to braces? A retrospective study evaluating the conversion rate, number of refinement scans, and length of treatment. Am. J. Orthod. Dentofac. Orthop. 2023, 163, 526–530. [Google Scholar] [CrossRef]
- Elshazly, T.M.; Bourauel, C.; Ismail, A.M.; Ghoraba, O.; Chavanne, P.; Elattar, H.; Alhotan, A. Effect of thermomechanical ageing on force transmission by orthodontic aligners made of different thermoformed materials: An experimental study. Orthod. Craniofac Res. 2024. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).