Abstract
The prognostic impact of non-obstructive coronary artery disease (CAD) remains controversial. Therefore, the objective of this study is to assess the long-term prognostic significance of non-obstructive CAD using machine learning models. We designed a multicenter retrospective, longitudinal, and observational study that included 3265 patients classified into three groups: 1426 patients with lesions < 20%, 643 patients with non-obstructive CAD (lesions 20–50%), and 1196 patients with obstructive CAD (lesions > 70%). A composite cardiovascular event (acute myocardial infarction, stroke, hospitalization due to heart failure, or cardiovascular-related death) was assessed after a mean follow-up of 43 months. To achieve this, various machine learning models were constructed. The model with the highest accuracy was selected to perform a Shapley Additive Explanations (SHAP) analysis, revealing the contribution of different variables in predicting an event. The SHAP analysis suggested that the percentage of coronary lesion was the most significant predictor of cardiovascular events. None of the models demonstrated adequate capability in predicting the event, showing only a good predictive ability for the absence of an endpoint. In conclusions, this study demonstrates how machine learning techniques may facilitate the development of high-performing models for predicting long-term cardiovascular events in patients undergoing coronary angiography.
1. Introduction
Coronary artery disease is a leading cause of mortality and morbidity worldwide, underscoring the importance of enhancing prevention, early diagnosis, and treatment efforts [1]. Non-obstructive coronary lesions are commonly detected during coronary angiography, whether in acute or chronic coronary syndrome cases. While the extent of atherosclerotic disease is traditionally seen as a marker of elevated ischemic risk, the clinical relevance of non-obstructive lesions and their associated prognostic factors remains contentious [2,3]. Moreover, the evaluation and categorization of coronary artery disease in patients present several challenges that remain unresolved. First, the definition of the presence of coronary artery disease and the classification of its severity are not unequivocal and vary according to different authors and the imaging technique used (computed tomography or invasive angiography) [3]. Second, assessment of the severity of coronary lesions is often performed through visual estimation, which leads to interobserver variability, even among expert cardiologists. Lastly, although various intracoronary diagnostic techniques are available (intravascular ultrasound, optical coherence tomography, fractional flow reserve, and instantaneous wave-free ratio) to mitigate the subjectivity of visual estimation, the implementation of these techniques in daily clinical practice is highly variable across centers and, in many cases, underutilized [4].
Conventional statistical methods have been widely employed to assess the prognostic value of coronary lesions, but these approaches are limited by their inability to capture complex non-linear relationships and high-order interactions [5]. In contrast, machine learning offers advanced capabilities for analyzing these intricate relationships, surpassing the scope of classical statistics [6].
This study aims to assess the long-term prognostic value of non-obstructive coronary artery disease using machine learning models, which are trained on data from patients undergoing coronary angiography for acute or chronic coronary syndrome.
2. Materials and Methods
2.1. Sample Selection, Inclusion and Exclusion Criteria
This is a multicenter and retrospective study including data from eight centers in Spain. The primary aim of this study was to assess the prognostic value associated with the presence of non-obstructive coronary artery disease. The methodology and results of this research have been previously published [7]. The research was performed in compliance with the guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of the Hospital Universitario Virgen de la Victoria (protocol code PI-0090-2017).
Briefly, eligible patients were those above eighteen years of age who underwent coronary angiography due to suspected myocardial ischemia associated with chronic coronary syndrome or acute coronary syndrome, with or without ST-segment elevation. The study included all patients with these characteristics who showed no coronary lesions greater than 50% between January 2011 and December 2015. For each of these patients, another patient with at least one coronary lesion greater than 70% was additionally included. The presence and degree of coronary lesions were determined at each center through visual estimation performed by the cardiologist conducting the coronary angiography. Exclusion criteria were previous revascularization, the presence of a lesion greater than 50% in the left main coronary artery, and the presence of lesions ranging from 50% to 70% in any vessel other than the left main coronary artery in the absence of other lesions greater than 70%.
2.2. Patient Classification Based on Coronary Angiography Findings and Follow-Up
Based on the findings observed in coronary angiograms, patients were classified into three groups: normal coronary arteries (absence of lesions or lesions less than 20%), non-obstructive coronary artery disease (lesions between 20% and 50%), and obstructive coronary artery disease (lesions greater than 70%). To validate lesion estimation, 300 randomly selected coronary angiograms were reviewed by two expert cardiologists, and a high agreement was obtained with the initial classification (Kappa = 0.827, 95% confidence interval 0.768–0.882). Figure 1 shows the patient workflow from inclusion to their classification into the three comparison groups of this study. The main clinical data of the patients were collected, and a long-term follow-up (at least 2 years) was conducted, with the primary outcome being a combined event defined as acute myocardial infarction, stroke, admission due to heart failure, or death from cardiovascular causes.
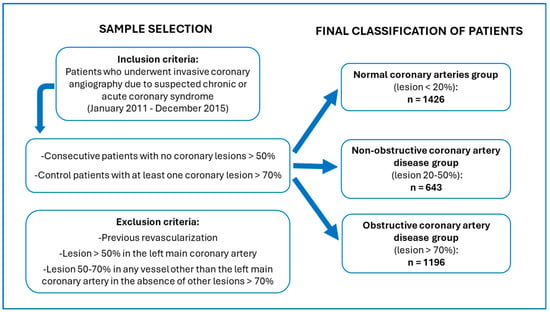
Figure 1.
Patient workflow from inclusion to classification according to the degree of stenosis.
2.3. Development of Predictive Machine Learning Models and Presentation of the Results Obtained
For the present analysis, the coding of different supervised learning models was carried out using the Python programming language. Coding was performed in the Jupyter Notebook tool, allowing the construction of a portfolio explaining the code and data analyses as the models were built.
The models implemented in this study were logistic regression [8], support vector machines [9], decision trees [10], random forests [11], and naive Bayes classifier [12]. The variables evaluated as potential predictors of events included age, sex, diabetes, smoking, hypertension, dyslipidemia, heart failure, kidney failure, atrial fibrillation, extracardiac comorbidity (defined as cerebrovascular disease, peripheral artery disease, or chronic obstructive pulmonary disease), diagnosis after catheterization (categorized into four groups as chest pain of uncertain origin, chronic coronary syndrome, acute coronary syndrome without ST-segment elevation, or acute coronary syndrome with ST-segment elevation; and categorized into three groups as chest pain of uncertain origin, chronic coronary syndrome, and acute coronary syndrome with or without ST-segment elevation), and the degree of coronary artery disease (categorized into three groups as normal coronary arteries, non-obstructive coronary artery disease, and obstructive coronary artery disease; and categorized into two groups as lesions less than 50% versus lesions greater than 70%). The evaluated event was defined similarly to the combined event in our previous work as a composite of acute myocardial infarction, stroke, admission due to heart failure, or death from cardiovascular causes [7].
In each of the artificial intelligence models, the data were divided into a training set and an examination set. A total of 80% of the data was allocated for training each model, while the remaining 20% was used for examination, resulting in an accuracy score for each model. To enhance the predictive capacity and accuracy of the models, ten different data partitions were used in each case with cross-validation, and subsequently, the arithmetic mean of the ten predictions was calculated. To estimate the predictive capacity of the developed models, the following parameters were calculated for each: accuracy, balanced accuracy, recall, precision, F1 score, area under ROC curve, and confusion matrix. Additionally, the contribution of different variables in predicting the combined event was graphically analyzed in the model with the highest accuracy using Shapley Additive Explanations (SHAP). This last step allowed assessment of the prognostic significance of non-obstructive coronary artery disease.
The variables were presented as means (continuous variables) or percentages (qualitative variables). The adjusted covariate levels across the groups, based on the extent of CAD, were calculated using analysis of variance. A polynomial contrast (linear trend) was applied to assess the relationship between the adjusted levels and the severity of CAD. The results of the association study between the degree of coronary lesion and the development of combined events were also presented using classical statistical techniques. A Cox regression model was performed, from which the Hazard Ratio and the 95% confidence interval were calculated for each degree of coronary lesion. We considered a p-value less than 0.05 as significant.
3. Results
3.1. General Characteristics of the Sample
A total of 3265 patients who underwent coronary angiography were included, among which 1426 (43.7%) belonged to the normal coronary arteries group, 643 (19.7%) to the non-obstructive coronary artery disease group, and 1196 (36.6%) to the obstructive coronary artery disease group. The clinical and demographic characteristics of the population have been previously reported [7]. The indication for angiography was chest pain/chronic coronary syndrome in 52.7% of patients and acute coronary syndrome in 47.3%, with 35% suffering from non-ST-segment elevation myocardial infarction and 12.3% from ST-segment elevation myocardial infarction. Table 1 displays the population baseline characteristics, classified according to the degree of coronary lesion.

Table 1.
Baseline-adjusted characteristics of the patient cohort according to the degree of coronary lesion.
3.2. Follow-Up Events
During a median follow-up of 43 months (interquartile range 33–56 months), 412 patients suffered a clinical event (12.6%), with 86 events (6%) in the normal coronary arteries group, 78 (12.1%) in the non-obstructive coronary artery disease group, and 248 (20.7%) in the obstructive coronary artery disease group.
Both non-obstructive and obstructive coronary lesions were independent predictors of the composite endpoint in an adjusted multivariable model with a respective 72% and 171% increase in risk (HR = 1.72, 95% CI: 1.23–2.39 and HR = 2.71, 95% CI: 2.03–3.62; p-trend for the comparison between the three groups < 0.001) [7].
3.3. Performance of the Machine Learning Models
Table 2 shows the model’s performance (logistic regression, support vector machine, decision tree classifier, random forests, and naive Bayes classifier), and Table 3 shows the confusion matrix of the different artificial intelligence models.

Table 2.
Performance exhibited by the various artificial intelligence models developed for predicting the combined event.

Table 3.
Confusion matrix of the different artificial intelligence models.
SHAP values for assessing the prognostic value associated with non-obstructive coronary lesions are presented in Figure 2 and Supplementary Table S1. The degree of coronary lesion (classified into three groups: normal coronary arteries, non-obstructive coronary artery disease, and coronary artery disease) was the most relevant predictor of events during follow-up. Three distinct risk groups were observed, corresponding to the three groups of lesion percentages in patients. Two of these groups, assumed to have obstructive and non-obstructive coronary lesions, had a SHAP value above zero, indicating a positive contribution to event prediction. In contrast, a group of data, assumed to correspond to patients with normal coronary arteries, had a value below zero, contributing to the prediction that the patient would not experience a cardiovascular event.
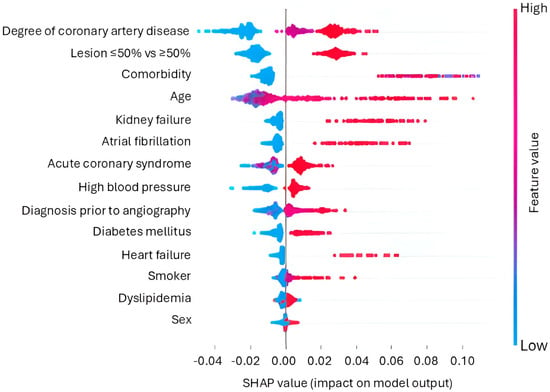
Figure 2.
SHAP model of contribution values.
4. Discussion
This study aims to apply a novel approach to evaluate the prognostic value of non-obstructive coronary artery disease by utilizing various machine learning techniques. The SHAP analysis applied to the model developed using the support vector machine indicates that the presence of non-obstructive coronary artery disease (lesions between 20% and 50%), as opposed to normal coronary arteries (lesions ≤ 20%), emerged as a predictive variable for cardiovascular events in patients undergoing coronary angiography. However, all the machine learning models presented in this work exhibit a very low true positive rate, limiting their validity in predicting cardiovascular events. Leveraging classical statistical techniques, we previously observed a roughly 70% increased risk of cardiovascular events in patients with non-obstructive coronary artery disease compared to patients with normal coronary arteries. Costa et al. previously found that both obstructive and non-obstructive lesions of the left main and proximal left anterior descending coronary arteries were associated with a higher risk of clinical events and benefited from a prolonged dual antiplatelet therapy course [13].
Over time, different studies have illustrated different applications of AI in clinical settings. One approach that has garnered significant interest is the automatic interpretation of images for diagnosis or prognosis in various pathologies. In this context, several studies have demonstrated that the diagnosis of coronary artery disease can be improved through machine learning algorithms designed for the interpretation of non-invasive cardiac imaging studies (single photon emission computed tomography-myocardial perfusion imaging) [14] or images obtained via invasive coronary angiography [15,16].
Another promising aspect is the development of predictive models for major clinical events under different baseline conditions, basing this prediction on clinical parameters without performing any type of automatic or semi-automatic image analysis. Moreover, in various pathological contexts, AI has shown improved predictive capabilities compared to classical statistical techniques. For instance, Mizarhani et al. compared the utility of AI versus classical statistics in predicting the survival of patients admitted to Intensive Care Units [17]. Similarly, Segar et al. analyzed the predictive capacity of AI models for mortality in hospitalized heart failure patients, outperforming classical statistical methods [18]. Additionally, Abdalrada et al. presented an innovative approach using a two-stage machine learning model for predicting the co-occurrence of diabetes mellitus and cardiovascular disease, showcasing the added value of AI over traditional statistical techniques, which have mainly focused on predicting isolated events based on multiple variables [19]. Similarly, Zhu et al. developed a model using Extreme Gradient Boosting that achieved a high predictive capacity for cardiovascular disease in a large sample of patients with chronic kidney disease [20].
Other studies have also explored the value of machine learning models to predict the development of coronary artery disease (excluding other forms of cardiovascular disease), demonstrating the prognostic value of simple parameters such as the TyG index [21]. A subsequent step currently being undertaken is the development of machine learning models to predict short- or long-term prognosis in established coronary artery disease. A relevant example is the work of Birdal et al., who developed an algorithm using Hierarchical Agglomerative Clustering, which improved the prediction of one-month mortality in patients who had suffered ST-elevation acute coronary syndrome [22]. Another promising application of artificial intelligence in the area of ischemic heart disease is presented by Oikonomou et al., who evaluated two different decision-making strategies for the type of diagnostic approach (anatomical study versus functional study) in cohorts of patients with suspected stable coronary artery disease. The two strategies compared were routine clinical practice versus a decision based on a machine learning algorithm. This algorithm was associated with a lower risk of adverse events [23].
Unlike the aforementioned studies [17,18,19,20,21,22,23], the current research focuses on assessing the prognostic value of a specific clinical variable, namely the presence of non-obstructive coronary artery disease. Consequently, our aim is not to compare the predictive capacity of two different methodological approaches (classical statistics versus AI) but to evaluate the problem from two distinct perspectives to obtain complementary results. The machine learning models we developed for the aforementioned objective exhibited adequate accuracy (ranging from 0.81 for decision trees and naive Bayes classifier to 0.87 for logistic regression and support vector machines) when compared to the performance of other AI models applied to predicting cardiovascular events in the context of coronary and cardiovascular diseases [18,24,25]. However, the results were insufficient for recall (ranging from 0 to 0.33), precision (ranging from 0 to 0.41), and F1-score (ranging from 0 to 0.29) metrics. The confusion matrix confirms that the developed models performed well in classifying patients without events but showed inadequate capability in identifying patients with events.
While acknowledging the limitations of the predictive models developed in this study, the SHAP analysis indicated that non-obstructive coronary disease may be a potential risk factor for the development of cardiovascular disease during follow-up. The consistency observed in the association between non-obstructive coronary artery disease and long-term cardiovascular events, confirmed through various data analysis tools, strengthens the causal relationship between the former and the latter as consistency is widely recognized as an essential criterion for establishing causal relationships [26]. The primary future implication that emerges from these results is that there is stronger scientific evidence supporting the need to enhance research on the efficacy of various therapeutic strategies (diet, exercise, and pharmacological treatment) in patients with a common condition that has previously received very little attention, namely, the presence of non-obstructive coronary artery disease [27].
Regarding the study sample, it is worth noting several peculiarities. Firstly, it included a substantial percentage of both stable and unstable patients, which is rare in studies evaluating the prognostic value of obstructive coronary lesions. Previous works have typically focused on chronic coronary syndrome patients [2,28,29,30,31], with limited evidence for the prognostic value of non-obstructive coronary artery disease in the context of acute coronary syndrome [32,33]. The second peculiarity of the sample lies in its classification into three specified groups (lesions less than 20%, lesions between 20% and 50%, and lesions greater than 70%), excluding patients with borderline lesions (lesions between 50% and 70%), which have been ambiguously considered as obstructive [2] or non-obstructive in the previous literature [28,34].
This study has several limitations that must be acknowledged, in addition to those already discussed regarding the performance of the models. Firstly, this is a retrospective study, which carries an inherent risk of biases due to the lack of collection of certain variables and the absence of randomization, primarily leading to confounding factors in the latter case. The assessment of coronary lesion severity relied solely on visual estimation, following the usual clinical practice of the participating centers during the inclusion period. This method introduced interobserver variability, although the concordance between participating centers and expert cardiologists was high. The classification of coronary lesions into three groups without considering other cutoff points between 0% and 50% is another limitation. Additionally, the number of vessels and total number of lesions visualized in angiography were not specified. Patients with lesions between 50% and 70% were excluded, limiting the study’s findings. Nevertheless, this exclusion allowed for the precise definition of patients with obstructive and non-obstructive lesions. Although the established follow-up period was relatively extensive (median of 43 months), a longer follow-up must be conducted to improve our understanding of the prognostic value of non-obstructive lesions. Another limitation pertains to the interpretability of the programming code and learning algorithms. AI models carry the risk of overfitting when based on highly homogenized databases. Hence, cross-validation is essential to reduce the risk of bias. Furthermore, algorithms should consider the inherent heterogeneity of clinical reality, and progress should be made toward less supervised experiments to enhance the applicability of AI in routine clinical practice [35].
5. Conclusions
This study demonstrates how machine learning techniques can be applied to develop predictive models for cardiovascular events in a specific context where significant knowledge gaps still exist, such as non-obstructive coronary artery disease. The analyses suggest the prognostic value of these non-obstructive coronary lesions (20–50%). However, these findings need to be confirmed in future studies, given the limitations of our predictive models. While they showed adequate overall accuracy based on good predictive ability for the absence of the event, they exhibited inadequate predictive capability for the combined event during follow-up.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/app14199079/s1, Supplementary Table S1: range and mean of SHAP values associated with each variable.
Author Contributions
Conceptualization, J.R.-C., F.C., P.L.S.-F., A.d.M.C.-S., M.R.-C., F.J.P.-M. and M.J.-N.; methodology and formal analysis, P.T.-S., M.A.M.-C., K.T.-H. and M.A.M.-M.; writing—original draft preparation, P.T.-S. and J.R.-C.; writing—review and editing, M.A.M.-C., K.T.-H., M.A.M.-M., F.C., P.L.S.-F., A.d.M.C.-S., M.R.-C., F.J.P.-M. and M.J.-N. All authors have read and agreed to the published version of the manuscript.
Funding
This work has received funding from the following organizations: the Servicio Andaluz de Salud, grant number PI 0090/2017 (Consejeria Salud Junta de Andalucia); UMA20-FEDERJA-074 Project funded by Programa Operativo FEDER Andalucía, Consejería de Economía y Conocimiento—Junta de Andalucía and cofunded by European Union; and PI-0131-2020 Project funded by Proyectos de Investigación en Salud, Consejería de Salud—Junta de Andalucía and cofunded by European Union. Dr. Costa is funded by the European Union (ERC, ORACLE, ERC-2023-STG-101117469). Views and opinions expressed are however those of the author(s) only and do not necessarily reflect those of the European Union or the European Research Council. Neither the European Union nor the granting authority can be held responsible for them.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee in Hospital Universitario Virgen de la Victoria (protocol code PI-0090-2017, approval data 17 April 2017).
Informed Consent Statement
Obtaining informed consent was waived by the ethics committee because this was a retrospective study in which an anonymized database was collected.
Data Availability Statement
All anonymized data from this study are available to the research community upon written request to the corresponding authors. The data are not publicly available due to ethical reasons.
Conflicts of Interest
Author Mario Antonio Muñoz-Muñoz was employed by the company Technology 2 Client. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Byrne, R.A.; Rossello, X.; Coughlan, J.J.; Barbato, E.; Berry, C.; Chieffo, A.; Claeys, M.J.; Dan, G.-A.; Dweck, M.R.; Galbraith, M.; et al. 2023 ESC Guidelines for the Management of Acute Coronary Syndromes. Eur. Heart J. 2023, 44, 3720–3826. [Google Scholar] [CrossRef] [PubMed]
- Finck, T.; Hardenberg, J.; Will, A.; Hendrich, E.; Haller, B.; Martinoff, S.; Hausleiter, J.; Hadamitzky, M. 10-Year Follow-Up After Coronary Computed Tomography Angiography in Patients With Suspected Coronary Artery Disease. JACC Cardiovasc. Imaging 2019, 12, 1330–1338. [Google Scholar] [CrossRef] [PubMed]
- Radico, F.; Zimarino, M.; Fulgenzi, F.; Ricci, F.; Di Nicola, M.; Jespersen, L.; Chang, S.M.; Humphries, K.H.; Marzilli, M.; De Caterina, R. Determinants of Long-Term Clinical Outcomes in Patients with Angina but without Obstructive Coronary Artery Disease: A Systematic Review and Meta-Analysis. Eur. Heart J. 2018, 39, 2135–2146. [Google Scholar] [CrossRef]
- Lee, J.M.; Choi, K.H.; Koo, B.-K.; Zhang, J.; Han, J.-K.; Yang, H.-M.; Park, K.W.; Song, Y.B.; Hahn, J.-Y.; Choi, S.-H.; et al. Intravascular Ultrasound or Optical Coherence Tomography-Defined Anatomic Severity and Hemodynamic Severity Assessed by Coronary Physiologic Indices. Rev. Esp. Cardiol. 2020, 73, 812–821. [Google Scholar] [CrossRef]
- Bzdok, D.; Altman, N.; Krzywinski, M. Statistics versus Machine Learning. Nat. Methods 2018, 15, 233–234. [Google Scholar] [CrossRef]
- Johnson, K.W.; Torres Soto, J.; Glicksberg, B.S.; Shameer, K.; Miotto, R.; Ali, M.; Ashley, E.; Dudley, J.T. Artificial Intelligence in Cardiology. J. Am. Coll. Cardiol. 2018, 71, 2668–2679. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Capitán, J.; Sánchez-Pérez, A.; Ballesteros-Pradas, S.; Millán-Gómez, M.; Cardenal-Piris, R.; Oneto-Fernández, M.; Gutiérrez-Alonso, L.; Rivera-López, R.; Guisado-Rasco, A.; Cano-García, M.; et al. Prognostic Implication of Non-Obstructive Coronary Lesions: A New Classification in Different Settings. J. Clin. Med. 2021, 10, 1863. [Google Scholar] [CrossRef]
- Cramer, J.S. The Origins of Logistic Regression. SSRN J. 2003, 4, 119. [Google Scholar] [CrossRef]
- Cortes, C.; Vapnik, V. Support-Vector Networks. Mach. Learn. 1995, 20, 273–297. [Google Scholar] [CrossRef]
- Quinlan, J.R. Induction of Decision Trees. Mach. Learn. 1986, 1, 81–106. [Google Scholar] [CrossRef]
- Breiman, L. Random Forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Friedman, N.; Geiger, D.; Goldszmidt, M. Bayesian Network Classifiers. Mach. Learn. 1997, 29, 131–163. [Google Scholar] [CrossRef]
- Costa, F.; Adamo, M.; Ariotti, S.; Ferrante, G.; Navarese, E.P.; Leonardi, S.; Garcia-Garcia, H.; Vranckx, P.; Valgimigli, M. Left Main or Proximal Left Anterior Descending Coronary Artery Disease Location Identifies High-Risk Patients Deriving Potentially Greater Benefit from Prolonged Dual Antiplatelet Therapy Duration. EuroIntervention 2016, 11, e1222–e1230. [Google Scholar] [CrossRef]
- Magboo, V.P.C.; Magboo, M.S.A. SPECT-MPI for Coronary Artery Disease: A Deep Learning Approach. Acta Med. Philipp. 2024, 58, 67–75. [Google Scholar] [CrossRef]
- Lee, C.-K.; Hong, J.-W.; Wu, C.-L.; Hou, J.-M.; Lin, Y.-A.; Huang, K.-C.; Tseng, P.-H. Real-Time Coronary Artery Segmentation in CAG Images: A Semi-Supervised Deep Learning Strategy. Artif. Intell. Med. 2024, 153, 102888. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Partinen, A.; Thurnhofer-Hemsi, K.; Rodríguez-Capitán, J.; Molina-Ramos, A.I.; Palomo, E.J. Coronary Artery Disease Classification With Different Lesion Degree Ranges Based on Deep Learning. IEEE Access 2024, 12, 69229–69239. [Google Scholar] [CrossRef]
- Mirzakhani, F.; Sadoughi, F.; Hatami, M.; Amirabadizadeh, A. Which Model Is Superior in Predicting ICU Survival: Artificial Intelligence versus Conventional Approaches. BMC Med. Inf. Decis. Mak. 2022, 22, 167. [Google Scholar] [CrossRef]
- Segar, M.W.; Hall, J.L.; Jhund, P.S.; Powell-Wiley, T.M.; Morris, A.A.; Kao, D.; Fonarow, G.C.; Hernandez, R.; Ibrahim, N.E.; Rutan, C.; et al. Machine Learning-Based Models Incorporating Social Determinants of Health vs Traditional Models for Predicting In-Hospital Mortality in Patients With Heart Failure. JAMA Cardiol. 2022, 7, 844–854. [Google Scholar] [CrossRef]
- Abdalrada, A.S.; Abawajy, J.; Al-Quraishi, T.; Islam, S.M.S. Machine Learning Models for Prediction of Co-Occurrence of Diabetes and Cardiovascular Diseases: A Retrospective Cohort Study. J. Diabetes Metab. Disord. 2022, 21, 251–261. [Google Scholar] [CrossRef]
- Zhu, H.; Qiao, S.; Zhao, D.; Wang, K.; Wang, B.; Niu, Y.; Shang, S.; Dong, Z.; Zhang, W.; Zheng, Y.; et al. Machine Learning Model for Cardiovascular Disease Prediction in Patients with Chronic Kidney Disease. Front. Endocrinol. 2024, 15, 1390729. [Google Scholar] [CrossRef]
- Mirjalili, S.R.; Soltani, S.; Meybodi, Z.H.; Marques-Vidal, P.; Firouzabadi, D.D.; Eshraghi, R.; Restrepo, D.; Ghoshouni, H.; Sarebanhassanabadi, M. Which Surrogate Insulin Resistance Indices Best Predict Coronary Artery Disease? A Machine Learning Approach. Cardiovasc. Diabetol. 2024, 23, 214. [Google Scholar] [CrossRef] [PubMed]
- Birdal, O.; İpek, E.; Saygı, M.; Doğan, R.; Pay, L.; Tanboğa, I.H. Cluster Analysis of Clinical, Angiographic, and Laboratory Parameters in Patients with ST-Segment Elevation Myocardial Infarction. Lipids Health Dis. 2024, 23, 166. [Google Scholar] [CrossRef] [PubMed]
- Oikonomou, E.K.; Aminorroaya, A.; Dhingra, L.S.; Partridge, C.; Velazquez, E.J.; Desai, N.R.; Krumholz, H.M.; Miller, E.J.; Khera, R. Real-World Evaluation of an Algorithmic Machine-Learning-Guided Testing Approach in Stable Chest Pain: A Multinational, Multicohort Study. Eur. Heart J.—Digit. Health 2024, 5, 303–313. [Google Scholar] [CrossRef]
- Forrest, I.S.; Petrazzini, B.O.; Duffy, Á.; Park, J.K.; Marquez-Luna, C.; Jordan, D.M.; Rocheleau, G.; Cho, J.H.; Rosenson, R.S.; Narula, J.; et al. Machine Learning-Based Marker for Coronary Artery Disease: Derivation and Validation in Two Longitudinal Cohorts. Lancet 2023, 401, 215–225. [Google Scholar] [CrossRef]
- Motwani, M.; Dey, D.; Berman, D.S.; Germano, G.; Achenbach, S.; Al-Mallah, M.H.; Andreini, D.; Budoff, M.J.; Cademartiri, F.; Callister, T.Q.; et al. Machine Learning for Prediction of All-Cause Mortality in Patients with Suspected Coronary Artery Disease: A 5-Year Multicentre Prospective Registry Analysis. Eur. Heart J. 2017, 38, 500–507. [Google Scholar] [CrossRef]
- Rothman, K.J.; Greenland, S. Causation and Causal Inference in Epidemiology. Am. J. Public. Health 2005, 95 (Suppl. S1), S144–S150. [Google Scholar] [CrossRef]
- Casolo, G.; Gabrielli, D.; Colivicchi, F.; Murrone, A.; Grosseto, D.; Gulizia, M.M.; Di Fusco, S.; Domenicucci, S.; Scotto di Uccio, F.; Di Tano, G.; et al. ANMCO POSITION PAPER: Prognostic and Therapeutic Relevance of Non-Obstructive Coronary Atherosclerosis. Eur. Heart J. Suppl. 2021, 23, C164–C175. [Google Scholar] [CrossRef] [PubMed]
- Nakazato, R.; Arsanjani, R.; Achenbach, S.; Gransar, H.; Cheng, V.Y.; Dunning, A.; Lin, F.Y.; Al-Mallah, M.; Budoff, M.J.; Callister, T.Q.; et al. Age-Related Risk of Major Adverse Cardiac Event Risk and Coronary Artery Disease Extent and Severity by Coronary CT Angiography: Results from 15 187 Patients from the International Multisite CONFIRM Study. Eur. Heart J. Cardiovasc. Imaging 2014, 15, 586–594. [Google Scholar] [CrossRef]
- Schulman-Marcus, J.; Hartaigh, B.Ó.; Gransar, H.; Lin, F.; Valenti, V.; Cho, I.; Berman, D.; Callister, T.; DeLago, A.; Hadamitzky, M.; et al. Sex-Specific Associations Between Coronary Artery Plaque Extent and Risk of Major Adverse Cardiovascular Events: The CONFIRM Long-Term Registry. JACC Cardiovasc. Imaging 2016, 9, 364–372. [Google Scholar] [CrossRef]
- Ouellette, M.L.; Löffler, A.I.; Beller, G.A.; Workman, V.K.; Holland, E.; Bourque, J.M. Clinical Characteristics, Sex Differences, and Outcomes in Patients With Normal or Near-Normal Coronary Arteries, Non-Obstructive or Obstructive Coronary Artery Disease. J. Am. Heart Assoc. 2018, 7, e007965. [Google Scholar] [CrossRef]
- Jespersen, L.; Abildstrom, S.Z.; Hvelplund, A.; Madsen, J.K.; Galatius, S.; Pedersen, F.; Hojberg, S.; Prescott, E. Burden of Hospital Admission and Repeat Angiography in Angina Pectoris Patients with and without Coronary Artery Disease: A Registry-Based Cohort Study. PLoS ONE 2014, 9, e93170. [Google Scholar] [CrossRef] [PubMed]
- Bugiardini, R.; Manfrini, O.; De Ferrari, G.M. Unanswered Questions for Management of Acute Coronary Syndrome: Risk Stratification of Patients with Minimal Disease or Normal Findings on Coronary Angiography. Arch. Intern. Med. 2006, 166, 1391–1395. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.J.; Zhang, L.L.; Elmariah, S.; Han, H.Y.; Zhou, Y.J. Prevalence and Prognosis of Nonobstructive Coronary Artery Disease in Patients Undergoing Coronary Angiography or Coronary Computed Tomography Angiography: A Meta-Analysis. Mayo Clin. Proc. 2017, 92, 329–346. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.H.; Park, G.-M.; Lee, S.-W.; Yun, S.-C.; Kim, Y.-H.; Cho, Y.-R.; Park, H.W.; Suh, J.; Yang, D.H.; Kang, J.-W.; et al. Long-Term Prognostic Value of Coronary CT Angiography in Asymptomatic Type 2 Diabetes Mellitus. JACC Cardiovasc. Imaging 2016, 9, 1292–1300. [Google Scholar] [CrossRef]
- Nicolosi, G.L. Artificial Intelligence in Cardiology: Why So Many Great Promises and Expectations, but Still a Limited Clinical Impact? J. Clin. Med. 2023, 12, 2734. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).