Abstract
VR rehabilitation is a rapidly evolving field, with increasing research and development aimed at improving its effectiveness, accessibility, and integration into mainstream healthcare systems. While there are some commercially available VR rehabilitation programs, their adoption and use in clinical practice are still limited. One of the limitations is defined as cybersickness, which is dependent on human contact with virtual reality products. The purpose of this essay is to raise awareness of the associated elements that contribute to cybersickness in rehabilitation using immersive VR. The common factors that influence the amount of cybersickness are user characteristics and device software and hardware. The Simulator Sickness Questionnaire (SSQ) was used as one of the formal models for determining the variables related to virtual reality sickness. The systematic review of the literature and the meta-analysis were chosen by whether the Simulator Sickness Questionnaire in the articles matched the research criteria. Based on PRISMA guidelines, a systematic review of the literature was conducted. Twenty-six publications from the recent past were totaled, comprising 862 individuals with ages ranging from 19 to 95, and 49% were female. The highest overall SSQ mean score for different kinds of symptoms was determined to be 21.058 for brain injuries, with a 95% confidence interval (CI) of 15.357 to 26.760. Time, content, locomotion, control, and display types were other elements that contributed to cybersickness and had significant p-values in the SNK Q-test. The future direction of immersive VR rehabilitation involves the development of immersive and interactive environments that simulate real-world situations, providing patients with a safe and controlled environment in which to practice new skills and movements.
1. Introduction
Virtual reality (VR) is a rapidly advancing technology that provides an immersive and interactive digital environment for users to experience computer-generated simulations in a realistic and engaging way. This technology has been developing rapidly in recent years and holds significant potential for various applications, including entertainment, healthcare, education, and business [1,2]. Among these topics, using VR for healthcare has been attracting increasing attention in recent years.
Rehabilitation is crucial in clinical and healthcare scenarios as it enables individuals to regain independence, enhance their quality of life, and reach their full potential in daily activities. Conceptually, rehabilitation is a multifaceted process that aims to restore physical, psychological, and social functioning after a period of illness, injury, or addiction. It takes into account the intricate interplay among biological, psychological, and social factors that may affect a person’s capacity to function and achieve their goals. Ultimately, rehabilitation is a process that considers the whole person and their unique circumstances to support them in their journey towards optimal health and well-being.
Manual rehabilitation is deficient in providing consistent and personalized feedback and monitoring. From the user perspective, patients with less motivation and satisfaction mostly result in obsolete applications [3]. What is more, the characteristics of patients may even determine the degree of recovery from physical or physiological sickness [4]. Against this background, many new technologies are seen to be viable options for investigating the possibilities of high-efficiency approaches.
In 2003, Burdea classified virtual reality therapies for rehabilitation as virtual rehabilitation [5]. Since then, virtual rehabilitation has been a significant topic in medical care for the past 20 years. Formally, virtual rehabilitation is a modern approach that utilizes virtual reality technology to deliver therapy, assessment, and training to individuals with various physical and mental conditions. The goal of virtual rehabilitation is to enhance the traditional rehabilitation process by providing an immersive, interactive, and engaging experience that can promote motor and cognitive skills, improve functional outcomes, and enhance the overall quality of life [6,7]. Studying immersive virtual rehabilitation can advance our understanding of the effectiveness and optimal implementation of this novel technology for improving rehabilitation outcomes, particularly in populations with limited access to traditional rehabilitation methods.
Virtual rehabilitation can be divided into different categories based on the types of conditions it aims to address: cognitive impairment, acquired brain damage, and physical inactivity [8,9,10]. Firstly, cognitive impairment might lead to dementia or apathy. This illness exists with memory, language, and judgment issues that are not severe enough for patients to interfere with daily activities [11]. Different from cognitive impairment, acquired brain injuries might be related to head trauma and increase the risk of neural connection problems. Specific symptoms of brain injuries include stroke or Parkinson’s in patients who lack the capacity to care for themselves in daily life [12]. Finally, physical inactivity is more common, and virtual rehabilitation may aid in patients recovering from physical injuries or increase exercise cognitive abilities [13].
Cybersickness is a phenomenon that arises from exposure to immersive virtual environments, causing a range of symptoms, such as nausea, oculomotor, and disorientation. It is a common challenge in VR applications, and its severity can be influenced by several factors. Understanding the underlying mechanisms and factors that contribute to cybersickness is crucial for the development of effective interventions to reduce its impact on users’ experience and promote the safe use of VR technology, especially under virtual rehabilitation scenarios. Specifically, we observed that there can be several influencing factors of cybersickness in virtual rehabilitation. One prominent factor is individual susceptibility, i.e., people with different physiques have different degrees of motion sickness reactions. The duration spent on VR equipment also has a great impact on cybersickness. In addition to user demographic differences, there are several device technological aspects that are associated with cybersickness, including software and hardware.
Research in this field of cybersickness tends to concentrate on its various elements, such as its internal and external origins. Meanwhile, the comprehensive review and meta-analyses of recent studies on cybersickness in immersive virtual rehabilitation contexts are still lacking. Cybersickness is entangled with virtual rehabilitation. On one hand, cybersickness can significantly impact the performance of virtual rehabilitation as it can cause symptoms that interfere with the patient’s ability to engage effectively in therapy. Nausea, oculomotor, and disorientation can decrease motivation, decrease one’s ability to concentrate, and increase fatigue, which can limit the patient’s participation in rehabilitation activities. On the other hand, under specific virtual rehabilitation scenarios, the severity of cybersickness might also be different from regular cases. Therefore, it is crucial to study cybersickness in virtual rehabilitation as it helps in understanding the consequences of cybersickness and helps clinicians and researchers develop effective strategies to minimize its impact and optimize the benefits of virtual rehabilitation for patients.
In this paper, we present a systematic review and meta-analysis of the consequences of cybersickness in immersive virtual rehabilitation. Specifically, we adopted the famous Simulator Sickness Questionnaire (SSQ) as a measure of cybersickness, which has four attributes: nausea, oculomotor, disorientation, and overall scores shown in Table 1. There were sufficient literature review and a series of analyses about the questionnaire. A sufficient literature review and a series of analyses were conducted based on the questionnaire. The review specifically summarizes participant demographics, including age range, user symptoms, and usage condition. As mentioned above, brain injuries, cognitive impairment, and physical inactivity are the primary user symptoms. Additionally, the sorts of VR devices for time, content, locomotion, control, and display are taken into account. Our results can provide guidelines for possible directions for improving the experience of immersive VR rehabilitation.

Table 1.
Simulator Sickness Questionnaire (SSQ) factors.
2. Materials and Methods
2.1. Searching Process
The INPLASY website (http://dx.doi.org/10.37766/inplasy2023.1.0019, accessed on 9 January 2023) has the most recent version of the systematic review procedure. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines were used to conduct this systematic review [14], and the checklist is shown in Appendix B. In this article, a systematic literature search was applied to collect journal and conference articles related to cybersickness in virtual rehabilitation. This search process covered the terms as followed: VR OR virtual reality OR HMDs OR virtual environment AND cybersickness OR simulator sickness OR virtual reality sickness AND rehabilitation OR rehab OR brain injuries OR cognitive impairment OR physical inactivity. Based on the PICO model [15], the qualifying requirements were studied (participants, interventions, comparisons, and outcomes). The included papers mainly focused on the implementation of rehabilitation interventions for patients with mental or physical symptoms to alleviate their helplessness. As shown in Figure 1 and described in Section 1, the symptoms can be divided into three types according to the conditions. Pre- and post-experiments were both used to compare the differences between before and after use in the tests of these papers, in which the four attributes of SSQ were employed to measure the subjects’ cybersickness scores after virtual rehabilitation.
Figure 1.
The main symptoms in immersive VR rehabilitation.
This research was conducted in November 2022 based on papers selected from several databases: PubMed, Web of Science, Google Scholar, and Scopus. We collected publications by searching the corresponding websites with the keywords mentioned above. The selected papers were all recent publications written in English. “virtual reality,” “rehabilitation,” “cybersickness,” “Simulator Sickness Questionnaire,” and “immersive environment” were among the most popular heading phrases. The selection criteria included the following: (1) the subjects utilized the virtual reality product; (2) SSQ scales were used in VR rehabilitation; (3) the papers were formal research papers. On the contrary, articles were excluded if: (1) the products were not virtual reality but mixed reality or augmented reality; (2) the papers were dissertations or reports; (3) the articles did not include SSQ scales or did not emphasize rehabilitation; (4) the standard deviations were missing in the results data.
Two independent reviewers examined the research’s eligibility (XL and DBL in the author list of this paper). Additionally, two reviewers separately conducted a risk-of-bias evaluation (YA and RHX in the author list of this paper). Regarding the SSQ results, the following subscale scores have fixed weights: nausea (9.54), oculomotor (7.58), and disorientation (13.92). Meanwhile, 3.74 is unweighted from the overall score. This is a crucial function in SSQ computing, which might significantly affect the study findings. The whole informative search and selection process is shown in Figure 2, together with the PRISMA principles.
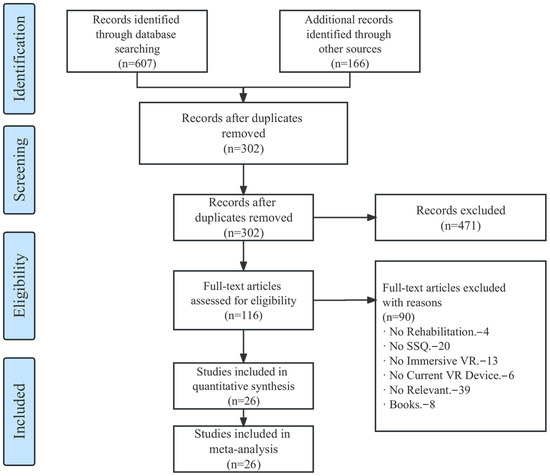
Figure 2.
The PRISMA flow diagram for the systematic review detailing the selection process.
2.2. Data Analysis
To conduct our investigation, which mostly relied on meta-analysis, we employed StataSE 14 [16] and Comprehensive Meta-Analysis (CMA) Version 3 [17] for computation. Specifically, three meta-analysis methods were adopted: SNK-test (Q-test), SMD (forest plot), and pooled mean.
Firstly, each subscale was calculated together with the Q-test variable analysis, also known as the conventional test for heterogeneity. Wi is the weighting factor of the ith, and Yi is the effect size of the ith. M is the average effect size of the number of studies k. In addition, the Q-test in this formula is called the weighted sum of squares (WSS):
At the same time, p-values were utilized to compare the Q-value with a chi-squared distribution. This probability, called the p-value, was employed to represent significant differences between the attributes in the study and the SSQ scores, when the value was lower than 0.05.
Secondly, we studied the STD mean difference (SMD). This is a measure of the effect size used in statistics to quantify the difference between the means of two groups or subgroups. When considering subgroups in this study, the SMDs were calculated in the same way by comparing the means of the three subgroups and dividing by the pooled standard deviation. It was important to ensure that the subgroups were well-defined and that any differences between them were appropriately accounted for. The outcomes with differences are presented in forest plots.
Lastly, the pooled mean was calculated by weighting the mean of each study about cybersickness by the sample size and dividing the sum of the weighted means by the sum of the sample sizes across all collected papers. For each of the overall and subscale SSQ scores, the pooled means of various qualities were calculated, which determined the importance of cybersickness. Calculations were carried out for the pooled impact evaluation, with 95% confidence intervals (CI 95%).
The tools and methods mentioned above were utilized to analyze the following factors. (1) Demographic factors. The age range of the patients was divided into three levels: youths under 30, adults between 30 and 60, and seniors above 60. This form of division was made taking into account the cognitive and motor skills of the user. The amount of data regarding gender differences was insufficient. In addition, there were several different types of patient symptoms related to virtual rehabilitation including physical inactivity, moderate cognitive impairment (MCI), acquired brain injuries. Cybersickness-inducing conditions were also included in the majority of article findings. (2) VR software. We mainly considered the exposure time of the VR device and the content of the VR application as software factors. (3) VR hardware. We identified 4 distinct forms of locomotion, 3 different types of control modes, and 2 types of display modes according to the applications in the collected papers. In the next steps, we calculated all of the elements related to cybersickness. Some of the publications had dropout participants, who experienced uncomfortable visual effects.
3. Results
3.1. Study Identification
We found 607 publications in the research articles that met the search criteria. Additionally, there were 166 articles added from other sources to enhance diversity. After that, 471 submissions were eliminated due to having mismatched subject names or abstracts. In further detail, there were no investigations into cybersickness and virtual rehabilitation. A total of 302 papers were successfully evaluated for eligibility. In this eligibility assessment, 116 studies (n = 116) fulfilled the criteria for inclusion, and 26 publications ultimately completed the measurement requirements for the meta-analysis. Inevitably, some participants dropped out of the studies in the middle, but the dropout rate in the selected publications was low. The outcomes of the search tactics are shown in Figure 2. Table 2 lists the 26 articles that used the cybersickness measures in virtual rehabilitation interventions. Of the 26 articles reporting airsickness, more than 5 publications included more than 3 experimental groups. The SSQ scores for the before, after, and modified periods were computed in several papers. Three of the papers compared different patients, including young, elderly, and older with Parkinson’s disease, in terms of health. Additionally, one of the publications gathered information from more than 100 participants.

Table 2.
Summary of included papers. N denotes number. M denotes male. F denotes female.
3.2. Study Details
Of the 26 items, 20 had both the SSQ total score and the subscale scores, while only 6 papers contained the total score. Therefore, the SSQ total scores in our study contain 26 items, and the SSQ subscale score values for nausea, oculomotor, and disorientation contain 20 items. The data were taken from articles that may have had various experiment settings in the same article. There were 862 people in total that took part in this study. Analysis of the affiliation shows that five papers originated from the USA, five from Germany, three from Australia, two from Norway, two from France, two from China, and two from Korea. Other affiliations included Switzerland, Italy, Denmark, the Netherlands, Belgium, Ireland, and Poland.
These publications have been featured in journals such as Virtual Reality, Medicine, Neuroscience Letters, and Frontiers in Virtual Reality. The primary study areas of the review papers shown on the WOS platform include “Computer Science” (n = 8), “Rehabilitation” (n = 5), “Engineering” (n = 4), and “Imaging Science & Photographic Technology” (n = 3). Devices including the HTC Vive, Oculus, Samsung, PlayStation, and Sony were used in the study tests.
Concerning the ages of the subjects, the participants ranged in age from teenagers (19 years old) to senior adults (95 years old). The adolescent age range (0–30) had around 311 people, with a mean age of 24.4, while the adult age range (30–60) had more than 200 people, with a mean age of 47.58. Additionally, there were 200 older individuals (over 60), with a mean age of 71.55. The amount of data regarding gender differences was insufficient.
After a thorough analysis, the primary goal was to compile the SSQ total and subscale scores for the factors that precipitated cybersickness in the field of virtual rehabilitation. The patients’ specific demography, VR software, and VR hardware are among the most important aspects of the SSQ scores. Multiple metrics are shown from the systematic review in Table 2 and Table 3, and the full names of each abbreviation are included in Appendix A. Figure 3 shows the SSQ total scores forest plot. The Chi-Square Test [44] was then used in this study’s statistical analysis. In the virtual rehabilitation scenario, the characteristics of the causes with the highest degree of heterogeneity were collected and are shown in Table 4 (standard deviation in means = 0.343, 95% CI = 0.245–0.440). Table 5 and Table 6 and Figure 4 show the results of the pooled mean analysis for the overall score (mean = 19.430, 95% CI: 15.678–23.181), nausea (mean = 17.834, 95% CI: 12.723–22.946), oculomotor (mean = 16.365, 95% CI: 11.512–21.218), and disorientation (mean = 21.096 95% CI: 14.059–28.133).

Table 3.
Summary of included papers. (Continued).
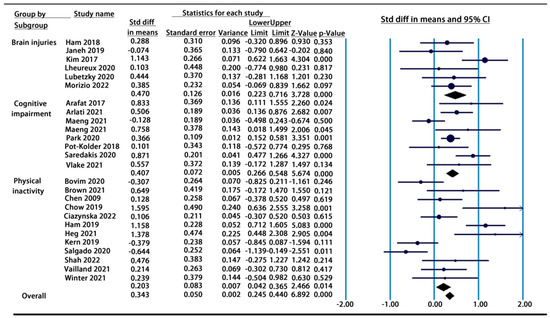
Figure 3.
Forest plot of symptom subgroups for SSQ total scores [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43].

Table 4.
Statistical analysis results for SSQ Scores.

Table 5.
SSQ total scores.

Table 6.
SSQ subscale scores.
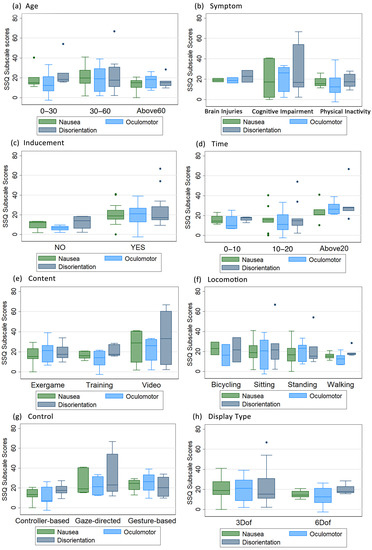
Figure 4.
Boxplots for SSQ subscale scores: (a) Age, (b) Symptom, (c) Inducement, (d) Time, (e) Content, (f) Locomotion, (g) Control, (h) Display Type.
The methodological quality of the research papers was evaluated using the widely adopted risk-of-bias analysis. All of the selected results were assessed according to whether or not the publication included useful SSQ score reference information beneficial to the ongoing endeavor. Publications without subscale scores were considered to have a low level of risk of bias.
3.3. Subject Characters and VR Cybersickness
Table 4 shows that the subject’s age was not relevant for determining the degree of cybersickness in the VR rehabilitation papers. The age range was divided into three groups, as shown in Table 5: 0–30 (teenagers, n = 8, 30.7%), 30–60 (adults, n = 9, 34.6%), and 60 and older (elderly, n = 8, 30.7%). Adult participants were the most susceptible to cybersickness in the total SSQ scores (mean = 20.853, 95% CI: 14.138–27.569), and after they reached the age of 60, their vulnerability to it gradually declined. Table 6 shows that teens had greater nausea (mean = 20.212, 95% CI: 15.977–24.447) and disorientation (mean = 25.868, 95% CI: 15.636–36.101) experience than adults and the elderly. What is more, adults suffered more serious oculomotor symptoms (mean = 17.143, 95% CI: 11.752–22.533) than the others.
There were variations in the symptoms and conditions among the patients who participated in virtual rehabilitation. The Q-value statistical results in Table 4 show that nausea (Q-value = 8.472, p = 0.037, p ≤ 0.05 *), oculomotor (Q-value = 8.552, p = 0.014, p ≤ 0.05 *), and disorientation (Q-value = 10.724, p = 0.005, p ≤ 0.01 **) symptoms and features of the overall SSQ score (Q-value = 6.628, p = 0.036, p ≤ 0.05 *) were all statistically significant. In Table 5, we gathered VR rehabilitation cases for our meta-analysis that mostly addressed brain injuries (n = 7, 26.9%), cognitive impairment (n = 7, 26.9%), and physical inactivity (n = 12, 46.2%). According to the calculated pooled mean, cognitive impairment (mean = 19.242, 95% CI: 11.294–27.189) and physical inactivity (mean = 18.156, 95% CI: 12.778–23.534) had lower scores than brain injuries (mean = 21.058, 95% CI: 15.357–26.760). In order to compare different symptoms, the mean scores, standard deviations, and sample sizes of the previous and post-available data were collected. As shown in the forest plot of the subgroup SSQ total scores in Figure 3, in contrast to cognitive impairment (mean = 0.407, 95% CI: 0.266–0.548) and physical inactivity (mean = 0.203, 95% CI: 0.042–0.365), subjects with brain injuries (mean = 0.470, 95% CI: 0.223–0.716) had a higher strictly standardized mean of virtual reality sickness.
We also took the inducement circumstance into consideration. According to Kenndy’s publication [45], SSQ total scores between 10 and 15 indicate substantial sickness, those of 15 to 20 indicate cause for serious worry, and those of 20 or more indicate a simulation issue. We used this reference as a benchmark and compared it to the original paper descriptions. By doing this, we formed a judgment on the inducement circumstances of each instance. Based on the result box plots shown in Figure 4, the non-induced data obviously stand out and are lower than the induced group.
3.4. VR Software and Cybersickness
In the immersive VR therapies studied, there were three different time durations: 0–10 min (n = 3, 11.5%), 10–20 min (n = 16, 61.5%), and above 20 min (n = 5, 19.5%). From the SNK Q-test, we were able to determine that there was a significant difference between the groups in the duration of VR rehabilitation exposure, which was also reflected in the SSQ scores. The SSQ total scores of times ranging from 0 to 10 min (mean = 14.474), 10 to 20 min (mean = 15.695), and above 20 min (mean = 26.862) are consistent with the trend. In addition, Figure 4 demonstrates that the scores for the three SSQ subscales increased steadily higher over time, excluding the outliers’ values. It is evident that prolonged exposure to a virtual environment screen induced feelings of disorientation (mean = 27.633, 95% CI: 19.786–35.454).
Apart from the condition of time, this study included a total of four different types of rehabilitation content: exercise games (n = 11, 42.3%), training (n = 8, 30.7%), videos (n = 4, 15.4%), and scenes (n = 3, 11.6%). In our research, it was clear that video had the highest mean scores on the SSQ’s overall and subscale scores (total mean score = 35.964, nausea mean = 32.671, oculomotor mean = 21.590, disorientation mean = 31.916). When compared to the exergame and training contents, the boxplot in Figure 4 thoroughly demonstrates the biggest value interval for video material. Additionally, when compared to the video with the highest score, the exergame’s (total mean score = 21.090, 95% CI: 15.695–26.484) mechanism may also heighten the symptoms of cybersickness. Among the four SSQ total score items, the scene (total mean score mean = 14.446, 95% CI: 6.548–22.345) had the lowest coefficients; it exhibited rotational motions along several axes without dynamic influence. Note that since scenes only had SSQ total scores, there are no scene types in Figure 4 and Table 6.
3.5. VR Hardware and Cybersickness
When it comes to hardware factors, in this study, we mainly considered locomotion, control, and display type.
In Table 4, the total SSQ score (Q-value = 7.864, p = 0.020, p ≤ 0.05 *) and disorientation (Q-value = 8.396, p = 0.015, p ≤ 0.05 *) are significantly different among the modes of locomotion. In our study, there were a total of four different modes of locomotion: sitting (n = 6, 23.1%, total mean score = 23.044, 95% CI: 10.847–35.240), standing (n = 7, 26.9%, total mean score = 24.122, 95% CI: 14.779–33.464), walking (n = 11, 42.3%, total mean score = 13.686, 95% CI: 10.173–17.199), and bicycling (n = 2, 7.7%, total mean score = 22.330, 95% CI: 14.310–30.349). Table 6 shows that the bicycling mode had the highest nausea score (mean = 21.491, 95% CI: 14.254–28.727). Meanwhile, standing led to higher oculomotor (mean = 20.162, 95% CI: 10.883–29.441) and disorientation (mean = 22.378, 95% CI: 12.316–32.440) sickness than other locomotion modes. The rankings are shown in Figure 4; the subscale scores of walking were lower than other locomotion.
As for the control aspect, we studied controller-based, gesture-based, and gazed-directed modes. A general controller for virtual rehabilitation equipment in a virtual environment (n = 9, 34.6%, mean = 17.537) was less susceptible to cybersickness. However, there is still proof that the gaze-directed (n = 9, 34.6%, mean = 23.953) and gesture-based control modes (n = 6, 23.1%, mean = 21.451) were significantly more uncomfortable than the typical controller, as shown in the SSQ total scores (Q-value = 21.936, p-value = 0.000, p ≤ 0.001 ***). Additionally, gesture-based training may have resulted in greater oculomotor (mean = 24.669, 95% CI: 10.800–38.538) and disorientation (mean = 20.369, 95% CI: 8.010–32.727) symptoms. These were brought on by the patients’ high vulnerability and high motion degree. The biggest range value in Figure 4 is for gaze-directed. The patient has complete freedom to stare anywhere they choose while traveling with the gaze method. This function causes dizziness and strain on the eyes, which increased the disorientation score (mean = 30.953, 95% CI: 14.490–47.416).
In Table 4, the values for the display types are significant in the total SSQ scores (Q-value = 7.660, p = 0.006, p ≤ 0.01 **), nausea scores (Q-value = 21.058, p = 0.000, p ≤ 0.001 ***), oculomotor scores (Q-value = 16.903, p = 0.000, p ≤ 0.001 ***), and disorientation scores (Q-value = 31.741, p = 0.000, p ≤ 0.001 ***). According to the boxplot, three degrees of freedom (n = 12, 60%) had higher subscale scores on the SSQ than six degrees of freedom (n = 17, 35%).
4. Discussion
The purpose of this systematic review was to gather the current research on cybersickness using SSQ scores, which examine the main consequences of the discomfort experienced. There are many factors related to cybersickness; this paper mainly concentrates on three different aspects, including the subjects’ demographics, software factors, and hardware factors.
4.1. Demographic of Cybersickness
The age of subjects may lead to different levels of virtual reality sickness. It has been found that the elderly may experience eye tiredness much more than adults or the young [46]. However, in our research, the comparison of the experiments for age groups showed that the old were not obviously oversensitive when applying virtual rehabilitation. Compared to older people, younger people and adults might be more available for interaction in virtual environments, if there are no big difficulties when using the devices and completing the tests [47]. The scores of the SSQ were also determined by other factors, such as skills, and not just age. When facing difficult missions, such as bicycling or gesture-based movement, older people might be unable to finish the process. More importantly, the SSQ scores for age might be misleading because of the limited number of cases. This conclusion should be proven by more studies from multiple directions in the future.
In virtual rehabilitation scenarios, symptoms are more important and worthy of attention in virtual environment cybersickness.
Firstly, for brain injuries, it has been shown that using immersive virtual rehabilitation as a treatment option may help individuals with brain injuries train their attention [48,49], which may affect the subject’s ability to learn new motor skills [50]. Studies on the effects of virtual reality on vital “theta waves” in the hippocampus have been beneficial. For instance, virtual reality improved brain activity associated with memory and learning [51] in the treatment of conditions, including Alzheimer’s disease, stroke, traumatic brain injury, and Parkinson’s disease. Virtual reality rehabilitation, therefore, offers possible novel treatments for brain injuries, but the cybersickness evaluation scores are so high that product developers should pay more attention to reducing the side effects [52]. Virtual reality provides a secure setting to enhance rehabilitation, particularly with the declining availability of labor and resources in our aging population.
Secondly, for exam users who have cognitive impairment [53], VR-based treatments have been used as health promotion tools to enhance mobility, prevent falls, and train cognitive skills in people who have dementia and those who are at risk of acquiring dementia. According to studies, virtual rehabilitation technology can be used to improve an individual’s abilities, such as memory and concentration, and to diagnose attention deficit hyperactivity disorder (ADHD) through hand or body involvement. The development of attention skills may delay cognitive aging [54]. A study at the University of Montreal examined the effects of video games on the grey matter in the area of the brain that supports memory formation, and the results demonstrated the value of exercise games in rehabilitation. All symptoms associated with cognitive impairment pointed to the need for tailored interventions and designed approaches to mitigate the negative effects of cybersickness [55,56].
Finally, a study revealed that virtual rehabilitation improved the effectiveness of VR exercise and particularly aided patients with physical inactivity in improving their physical fitness, muscular strength, and balance [57]. However, there were still flaws in the VR rehabilitation of physical inactivity. For instance, in the case of conducting a mission with a set time frame, the poor efficacy of training increased the amount of cybersickness. VR therapy is beneficial for both youth and the elderly who have gait impairment, vestibular issue, multiple sclerosis, spinal cord injury, neck discomfort, or chronic pain. However, when playing the same exercise game or other rehabilitation assignment simultaneously, a serious disease may cause discomfort and worsen physical or mental conditions [58].
There are individual differences in the severity of cybersickness symptoms based on personal medical conditions. The SSQ scores for individuals with brain injuries, cognitive impairment, and physical inactivity indicate more severe cybersickness symptoms in these groups.
4.2. Software Factors of Cybersickness
It can be concluded that as the exposure time of the VR facility increases, so does cybersickness. However, research on exposure to VR suggests that users can have an adjustment period. After about 15–20 min of exposure to a virtual environment, the parameters will return to baseline levels. Risi [59] discovered that repeated VR device exposures during a two-day period did not lower cybersickness levels. Shah [39] and Heg [27] also demonstrated the probability of SSQ deterioration after adjustment. We could not lessen the amount of cybersickness until consumers adapted to the virtual world, but when the interval was too long, it did not make sense. Furthermore, people with brain injuries are unable to spend an excessive amount of time in an immersive virtual world since doing so might have long-lasting side effects [34]. As a matter of fact, duration is one of the key points that leads to varying degrees of cybersickness, and designers should be more concerned about the interaction time in software engineering.
In addition to the time condition, four different types of rehabilitation contents were included in this study. The degree of cybersickness might be simply described by task performance in different types of content, including exergames, training, video, and scenes [60]. A user of virtual reality feels completely immersed in their surroundings since the environment is computer-generated and contains realistic-looking items and situations. An immersive content experience is totally different from passive reading, such as static PDF, stress immersion, and interaction with text [61]. Interactive polls and quizzes, animated data visualizations and infographics, and 3D images and videos are some of the most popular forms of immersive content. As for exergames and training, there are many types of exercise activities related to rehabilitation, including role play, the use of an omnidirectional treadmill, and others. Video was harder for subjects to get used to and resulted in the highest levels of cybersickness. This phenomenon may be caused by high-intensity training that causes one to lose their sense of direction. It has been suggested that exergames and training has relatively smaller degrees of cybersickness than video content.
4.3. Hardware Factors of Cybersickness
The first hardware factor is locomotion. We can easily infer from the SSQ scores that those strategies with artificial continuous movement led to higher SSQ scores than those with discrete movements [62]. For example, sitting may have had a high SSQ score due to the restrictions on the mobility of bodily movement. When it came to walking, there were two basic types of conditions: walking on a treadmill and walking in a real zone. According to Wilson, natural walking without translation causes less illness from cybersickness than added translation movement. Additionally, as a role player, natural walking resulted in lower SSQ scores than teleportation. Bicycling may also cause a significant amount of cybersickness [63].
For control modes, it is important to note that the gaze-directed samples had higher feelings of discomfort when undergoing the examination. When using the gaze-directed approach, the VR device sets a pointer in the middle of the screen and a target icon (a white cylinder) on the ground in the event that the user’s sight crosses the ground. The patient goes to the desired position by pushing a button. This may increase the difficulty of machine control. In contrast, the SSQ scores decreased in controller-based and gesture-based settings, which means that designers should avoid setting gaze-directed control modes.
For the display type, while patients in VR therapy may gaze about in all directions, three DoF cannot be used to get a closer look at anything in the environment. Patients only have access to one perspective, and thus, no matter how they move or swivel their heads in the actual world, they stay still in the virtual one, with higher SSQ scores reflecting the drawback known as visual–vestibular conflict. The visual and vestibular system “disconnect” results in a sensory conflict in 3D space. Therefore, six DoF motion is the foundation of a better VR rehabilitation experience.
4.4. Strengths, Limitations, and Future Works
This paper explores a new area in immersive virtual reality rehabilitation with SSQ score data collected from more than 862 participants. The results show that factors such as symptoms, inducement condition, exposure time, content, and hardware controls vary widely across multiple variants. This article provides a good example for conducting immersive virtual reality rehabilitation research to benefit the rehabilitation industry. Especially in the face of high artificial medical costs, it is impossible to hire more therapists in the digital age.
One limitation of this research is that the number of influencing factors studied is limited. In addition, due to the limited number of papers included, the conclusions of some factors may require further research and proof.
For further studies, researchers can explore more influencing factors. For example, immersive virtual reality rehabilitation can also be further studied in terms of regional differences, VR equipment, interaction modes, and so on. As the market develops, there are more and more requests for better use of virtual rehabilitation. The results show that the SSQ is a useful analytical measure that provides a large amount of valid data. In addition, two variants of the SSQ have been offered for testing cybersickness in recent research and have become popular, which are named the Cybersickness Questionnaire and the Virtual Reality Sickness Questionnaire. These may overcome the shortcomings of the SSQ, which considers virtual reality as the mian object of study.
5. Conclusions
Cybersickness is a common side effect of immersive virtual reality rehabilitation, which can negatively impact a patient’s experience and potentially limit the effectiveness of treatment. This research evaluated the cybersickness-related aspects of VR rehabilitation, which was achieved by a systematic review of this field and by conducting a meta-analysis of the SSQ scores. For the demographic factors, the SSQ scores of participants’ ages, symptoms, and inducement situations were discussed in this study. We also discussed the VR device software missions’ time lengths and contents. As for the hardware aspect, locomotion, control method, and display type were also taken into consideration. These three categories of characteristics exhibited the cybersickness circumstances that affected how smoothly the experiments operated. With the technological revolution taking place against the immersive backdrop, it is beneficial for us to enhance the rehabilitation mode [64]. Furthermore, by better understanding VR technology, we will be able to create equipment that is particularly useful for rehabilitation [65,66].
With proper design and implementation, cybersickness can be minimized, and the benefits of virtual reality rehabilitation can be fully realized. However, it is difficult to draw firm conclusions supporting the use of VR in rehabilitation from small-scale studies, and future directions should focus on more informative or large-scale studies. The FOV, latency, and realism of immersive VR rehabilitation equipment are improving [67]. Given the advancement of technology, the impact of cybersickness should be further assessed [68]. For better product engineering, rehabilitation symptoms require more attention. Overall, while cybersickness can be a significant issue in immersive virtual reality rehabilitation, it should not discourage the use of this technology in healthcare. With careful attention to design and patient needs, virtual reality can provide a valuable tool for rehabilitation and improved patient outcomes.
Author Contributions
Conceptualization, X.L.; methodology, X.L.; software, Y.A.; validation, D.-B.L., Y.A.; formal analysis, X.L.; investigation, R.-H.X.; resources, X.L.; data curation, X.L.; writing—original draft preparation, X.L.; writing—review and editing, X.L.; visualization, X.L.; supervision, D.-B.L.; project administration, D.-B.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
| Abbreviations | Description | Abbreviations | Description |
| AD-ACL | Activation–Deactivation Adjective Check List | AES | Apathy Evaluation Scale |
| CCT | Computerized Cognitive Training | CERAD-K | A Korean version of the Consortium to Establish a Registry for Alzheimer’s Disease Assessment |
| CET | Cognitive Evaluation Theory | DHI | Dizziness Handicap Inventory |
| IMI | Intrinsic Motivation Inventory | DOF | Degrees of Freedom |
| EDQ | Equipment and Display Questionnaire | GMS | Global Motivation Scale |
| ITC-SOPI | International Test Commission—Sense of Presence Inventory | ICU-VR | ICU-specific VR |
| HMD | Head-Mounted Display | KQOL-AD | Korean Version of Quality of Life—Alzheimer’s Disease |
| GEQ | Game Experience Questionnaire | GDS | Geriatric Depression Scale |
| MCI | Mild Cognitive Impairment | GSR | Galvanic Skin Response |
| NDI | Neck Disability Index | NASA-TLX | NASA Task Load Index |
| QoE | Quality of Experience | RAGT | Robot-Assisted Gait Training |
| VEQ | Virtual Embodiment Questionnaire | SoP | Sense of Presence |
| SP | Spatial Presence | RTLX | Raw Task Load Index |
| SMET | Submaximal Tourniquet Effort Test | PAS | Psychogeriatric Assessment Scale |
| QoE | Quality of Experience | SCR | Skin Conductance Response |
| PQ | Presence Questionnaire | VRSQ | Virtual Reality Symptom Questionnaire |
| UEQ | Experience Questionnaire | USEQ | User Satisfaction Evaluation Questionnaire |
| SS-VAS | Simulator Sickness Visual Analog Scale | VRISE | VR Sickness or Virtual Reality-Induced Symptoms and Effects |
| SSQ | Simulator Sickness Questionnaire | SUS | System Usability Scale |
| VSS | Visual Symptoms Scale | VRCT | Virtual Reality-Based Cognitive Therapy |
| VAS | Visual Analog Scale | TAM | Technology Acceptance Model |
Appendix B
| Section and Topic | Item | Checklist Item | Location Where Item Is Reported |
| TITLE | |||
| Title | 1 | Identify the report as both systematic review and meta-analysis. | Page 1 |
| ABSTRACT | |||
| Structure summary | 2 | Provide a structured summary including, as applicable: background; objectives; data sources; study eligibility criteria, participants, and interventions; study appraisal and synthesis methods; results; conclusions and implications of key findings. | Page 1 |
| INTRODUCTION | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known. | Page 2 |
| Objectives | 4 | Provide an explicit statement of questions being addressed with reference to participants, interventions, comparisons, outcomes, and study design (PICOS). | Page 2–4 |
| METHODS | |||
| Eligibility criteria | 5 | Present the systematic review registration number. And specify the inclusion and exclusion criteria for the review and how studies were grouped for the syntheses. | Page 4 |
| Information sources | 6 | Specify all databases, registers, websites, organizations, reference lists and other sources searched or consulted to identify studies. | Page 4 |
| Search strategy | 7 | Present the full search strategies for all databases, registers and websites, including any filters and limits used. | Page 4–5 |
| Selection process | 8 | Specify the methods used to decide whether a study met the inclusion criteria of the review, including how many reviewers screened each record and each report retrieved, whether they worked independently, and if applicable, details of automation tools used in the process. | Page 5 |
| Data collection process | 9 | Specify the methods used to collect data from reports, including how many reviewers collected data from each report, whether they worked independently, any processes for obtaining or confirming data from study investigators. | Page 5 |
| Data items | 10 | List and define all outcomes for which data were sought. Specify whether all results that were compatible with each outcome domain in each study were sought (e.g., for all measures, time points, analyses). | Page 5 |
| Study risk of bias assessment | 11 | Specify the methods used to assess risk of bias in the included studies, including details of the tool(s) used, how many reviewers assessed each study and whether they worked independently, and if applicable, details of automation tools used in the process. | Page 5 |
| Effect measures | 12 | Specify for each outcome the effect measure(s) (e.g., risk ratio, mean difference) used in the synthesis or presentation of results. | Page 5 |
| Synthesis methods | 13 | Describe any methods used to explore possible causes of heterogeneity among study results (e.g., subgroup analysis, meta-regression). | Page 5–6 |
| Reporting bias assessment | 14 | Describe any methods used to assess risk of bias due to missing results in a synthesis (arising from reporting biases). | Page 5–6 |
| Certainty assessment | 15 | Describe any methods used to assess certainty (or confidence) in the body of evidence for an outcome. | Page 6 |
| RESULTS | |||
| Study selection | 16 | Describe the results of the search and selection process, from the number of records identified in the search to the number of studies included in the review, ideally using a flow diagram. | Page 7 Figure 2 |
| Study characteristics | 17 | Cite each included study and present its characteristics. | Page 7 |
| Risk of bias in studies | 18 | Present assessments of risk of bias for included study. | Page 14 |
| Results of individual studies | 19 | For all outcomes, present, for each study: (a) summary statistics for each group (where appropriate) and (b) an effect estimate and its precision (e.g., confidence/credible interval), ideally using structured tables or plots. | Table 2 and Table 3 |
| Results of syntheses | 20 | Present results of all statistical syntheses conducted. As meta-analysis was done, present for each the summary estimate and its precision (e.g., confidence/credible interval) and measures of statistical heterogeneity. Comparing the groups and describing the direction of the effect. | Figure 3 and Figure 4 Table 4, Table 5 and Table 6 |
| Reporting biases | 21 | Present results of any assessment of risk of bias across studies (see Item 18). | Page 14 |
| DISCUSSION | |||
| Discussion | 22 | Provide a general interpretation of the results in the context of other evidence and implications of the results for practice, policy, and future research. | Page 20 |
| OTHER INFORMATION | |||
| Registration and protocol | 23 | Provide registration information for the review, including register name and registration number, or state that the review was not registered. | NA |
| Support | 24 | Describe sources of financial or non-financial support for the review, and the role of the funders or sponsors in the review. | NA |
| Competing interests | 25 | Declare any competing interests of review authors. | NA |
| Availability of data, code and other materials | 26 | Report which of the following are publicly available and where they can be found: template data collection forms; data extracted from included studies; data used for all analyses; analytic code; any other materials used in the review. | NA |
| From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71. For more information, visit: http://www.prisma-statement.org/, accessed on 9 January 2023. | |||
References
- Tan, T.F.M.; Li, Y.; Lim, J.S.F.; Gunasekeran, D.V.M.; Teo, Z.L.M.; Ng, W.Y.F.; Ting, D.S. Metaverse and Virtual Health Care in Ophthalmology: Opportunities and Challenges. Asia-Pac. J. Ophthalmol. 2022, 11, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Kye, B.; Han, N.; Kim, E.; Park, Y.; Jo, S. Educational applications of metaverse: Possibilities and limitations. J. Educ. Evaluation Health Prof. 2021, 18, 32. [Google Scholar] [CrossRef] [PubMed]
- Monardo, G.; Pavese, C.; Giorgi, I.; Godi, M.; Colombo, R. Evaluation of Patient Motivation and Satisfaction During Technology-Assisted Rehabilitation: An Experiential Review. Games Health J. 2021, 10, 13–27. [Google Scholar] [CrossRef]
- Petri, K.; Feuerstein, K.; Folster, S.; Bariszlovich, F.; Witte, K. Effects of Age, Gender, Familiarity with the Content, and Exposure Time on Cybersickness in Immersive Head-mounted Display Based Virtual Reality. Am. J. Biomed. Sci. 2020, 12, 107–121. [Google Scholar] [CrossRef]
- Burdea, G.C. Virtual rehabilitation–benefits and challenges. Methods Inf. Med. 2003, 42, 519–523. [Google Scholar]
- Rose, T.; Nam, C.S.; Chen, K.B. Immersion of virtual reality for rehabilitation—Review. Appl. Ergon. 2018, 69, 153–161. [Google Scholar] [CrossRef]
- Calabrò, R.S.; Cerasa, A.; Ciancarelli, I.; Pignolo, L.; Tonin, P.; Iosa, M.; Morone, G. The arrival of the metaverse in neurorehabilitation: Fact, fake or vision? Biomedicines 2022, 10, 2602. [Google Scholar] [CrossRef]
- Kurz, A.; Pohl, C.; Ramsenthaler, M.; Sorg, C. Cognitive rehabilitation in patients with mild cognitive impairment. Int. J. Geriatr. Psychiatry A J. Psychiatry Late Life Allied Sci. 2009, 24, 163–168. [Google Scholar] [CrossRef]
- Teasell, R.; Bayona, N.; Marshall, S.; Cullen, N.; Bayley, M.; Chundamala, J.; Villamere, J.; Mackie, D.; Rees, L.; Hartridge, C.; et al. A systematic review of the rehabilitation of moderate to severe acquired brain injuries. Brain Inj. 2007, 21, 107–112. [Google Scholar] [CrossRef]
- Zelle, D.M.; Klaassen, G.; Van Adrichem, E.; Bakker, S.J.; Corpeleijn, E.; Navis, G. Physical inactivity: A risk factor and target for intervention in renal care. Nat. Rev. Nephrol. 2017, 13, 152–168. [Google Scholar] [CrossRef]
- Kim, O.; Pang, Y.; Kim, J.-H. The effectiveness of virtual reality for people with mild cognitive impairment or dementia: A meta-analysis. BMC Psychiatry 2019, 19, 219. [Google Scholar] [CrossRef]
- Cullen, N.; Chundamala, J.; Bayley, M.; Jutai, J. The efficacy of acquired brain injury rehabilitation. Brain Inj. 2007, 21, 113–132. [Google Scholar] [CrossRef]
- Dębska, M.; Polechoński, J.; Mynarski, A.; Polechoński, P. Enjoyment and Intensity of Physical Activity in Immersive Virtual Reality Performed on Innovative Training Devices in Compliance with Recommendations for Health. Int. J. Environ. Res. Public Health 2019, 16, 3673. [Google Scholar] [CrossRef]
- Takkouche, B.; Norman, G. Prisma statement. Epidemiology 2011, 22, 128. [Google Scholar] [CrossRef]
- Eriksen, M.B.; Frandsen, T.F. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: A systematic review. J. Med. Libr. Assoc. 2018, 106, 420–431. [Google Scholar] [CrossRef]
- Rebenitsch, L.; Owen, C. Individual variation in susceptibility to cybersickness. In Proceedings of the 27th annual ACM Symposium on User Interface Software and Technology, Honolulu, HI, USA, 5–8 October 2014; pp. 309–317. [Google Scholar]
- Bruck, S.; Watters, P.A. Estimating Cybersickness of Simulated Motion Using the Simulator Sickness Questionnaire (SSQ): A Controlled Study. In Proceedings of the 2009 6th International Conference on Computer Graphics, Imaging and Visualization, Tianjin, China, 11–14 August 2009; pp. 486–488. [Google Scholar] [CrossRef]
- Arafat, I.M. Cybersickness in Persons with Multiple Sclerosis. Ph.D. Thesis, The University of Texas at San Antonio, San Antonio, TX, USA, 2019. [Google Scholar]
- Arlati, S.; Di Santo, S.G.; Franchini, F.; Mondellini, M.; Filiputti, B.; Luchi, M.; Ratto, F.; Ferrigno, G.; Sacco, M.; Greci, L. Acceptance and Usability of Immersive Virtual Reality in Older Adults with Objective and Subjective Cognitive Decline. J. Alzheimer’s Dis. 2021, 80, 1025–1038. [Google Scholar] [CrossRef]
- Bovim, L.P.; Gjesdal, B.E.; Mæland, S.; Aaslund, M.K.; Bogen, B. The impact of motor task and environmental constraints on gait patterns during treadmill walking in a fully immersive virtual environment. Gait Posture 2020, 77, 243–249. [Google Scholar] [CrossRef]
- Brown, P.; Powell, W. Pre-Exposure Cybersickness Assessment Within a Chronic Pain Population in Virtual Reality. Front. Virtual Real. 2021, 2, 67. [Google Scholar] [CrossRef]
- Chen, C.-H.; Jeng, M.-C.; Fung, C.-P.; Doong, J.-L.; Chuang, T.-Y. Psychological benefits of virtual reality for patients in rehabilitation therapy. J. Sport Rehabil. 2009, 18, 258–268. [Google Scholar] [CrossRef]
- Chowdhury, T.; Ferdous, S.; Peck, T.; Quarles, J. Virtual ability simulation: Applying rotational gain to the leg to increase confidence during physical rehabilitation. In Proceedings of the ICAT-EGVE 2019-International Conference on Artificial Reality and Telexistence and Eurographics Symposium on Virtual Environments, Tokyo, Japan, 11–13 September 2019. [Google Scholar]
- Ciążyńska, J.; Janowski, M.; Maciaszek, J. Effects of a Modern Virtual Reality 3D Head-Mounted Display Exergame on Simulator Sickness and Immersion Under Specific Conditions in Young Women and Men: Experimental Study. JMIR Serious Games 2022, 10, e41234. [Google Scholar] [CrossRef]
- Hamzeheinejad, N.; Straka, S.; Gall, D.; Weilbach, F.; Latoschik, M.E. Immersive Robot-Assisted Virtual Reality Therapy for Neurologically-Caused Gait Impairments. In Proceedings of the 2018 IEEE Conference on Virtual Reality and 3D User Interfaces (VR), Tuebingen/Reutlingen, Germany, 18–22 March 2018; pp. 565–566. [Google Scholar] [CrossRef]
- Hamzeheinejad, N.; Roth, D.; Götz, D.; Weilbach, F.; Latoschik, M.E. Physiological effectivity and user experience of immersive gait rehabilitation. In Proceedings of the 2019 IEEE Conference on Virtual Reality and 3D User Interfaces (VR), Osaka, Japan, 23–27 March 2019; pp. 1421–1429. [Google Scholar]
- Høeg, E.R.; Bruun-Pedersen, J.R.; Cheary, S.; Andersen, L.K.; Paisa, R.; Serafin, S.; Lange, B. Buddy biking: A user study on social collaboration in a virtual reality exergame for rehabilitation. Virtual Real. 2021, 27, 1–18. [Google Scholar] [CrossRef]
- Janeh, O.; Fründt, O.; Schönwald, B.; Gulberti, A.; Buhmann, C.; Gerloff, C.; Steinicke, F.; Pötter-Nerger, M. Gait Training in Virtual Reality: Short-Term Effects of Different Virtual Manipulation Techniques in Parkinson’s Disease. Cells 2019, 8, 419. [Google Scholar] [CrossRef] [PubMed]
- Kern, F.; Winter, C.; Gall, D.; Kathner, I.; Pauli, P.; Latoschik, M.E. Immersive Virtual Reality and Gamification Within Procedurally Generated Environments to Increase Motivation During Gait Rehabilitation. In Proceedings of the 26th IEEE Conference on Virtual Reality and 3D User Interfaces, VR 2019, Osaka, Japan, 25–29 March 2017; pp. 500–509. [Google Scholar] [CrossRef]
- Kim, A.; Darakjian, N.; Finley, J.M. Walking in fully immersive virtual environments: An evaluation of potential adverse effects in older adults and individuals with Parkinson’s disease. J. Neuroeng. Rehabil. 2017, 14, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Lubetzky, A.V.; Kelly, J.; Wang, Z.; Gospodarek, M.; Fu, G.; Sutera, J.; Hujsak, B.D. Contextual sensory integration training via head mounted display for individuals with vestibular disorders: A feasibility study. Disabil. Rehabil. Assist. Technol. 2020, 17, 74–84. [Google Scholar] [CrossRef]
- Lheureux, A.; LeBleu, J.; Frisque, C.; Sion, C.; Stoquart, G.; Warlop, T.; Detrembleur, C.; Lejeune, T. Immersive Virtual Reality to Restore Natural Long-Range Autocorrelations in Parkinson’s Disease Patients’ Gait During Treadmill Walking. Front. Physiol. 2020, 11, 572063. [Google Scholar] [CrossRef]
- Maeng, S.; Hong, J.P.; Kim, W.-H.; Kim, H.; Cho, S.-E.; Kang, J.M.; Na, K.-S.; Oh, S.-H.; Park, J.W.; Bae, J.N.; et al. Effects of Virtual Reality-Based Cognitive Training in the Elderly with and without Mild Cognitive Impairment. Psychiatry Investig. 2021, 18, 619–627. [Google Scholar] [CrossRef]
- Morizio, C.; Compagnat, M.; Boujut, A.; Labbani-Igbida, O.; Billot, M.; Perrochon, A. Immersive Virtual Reality during Robot-Assisted Gait Training: Validation of a New Device in Stroke Rehabilitation. Medicina 2022, 58, 1805. [Google Scholar] [CrossRef]
- Park, S.; Lee, G. Full-immersion virtual reality: Adverse effects related to static balance. Neurosci. Lett. 2020, 733, 134974. [Google Scholar] [CrossRef]
- Pot-Kolder, R.; Veling, W.; Counotte, J.; Van Der Gaag, M. Anxiety Partially Mediates Cybersickness Symptoms in Immersive Virtual Reality Environments. Cyberpsychology Behav. Soc. Netw. 2018, 21, 187–193. [Google Scholar] [CrossRef]
- Salgado, D.P.; Flynn, R.; Naves, E.L.M.; Murray, N. The Impact of Jerk on Quality of Experience and Cybersickness in an Immersive Wheelchair Application. In Proceedings of the 2020 Twelfth International Conference on Quality of Multimedia Experience, Athlone, Ireland, 26–28 May 2020; pp. 1–6. [Google Scholar] [CrossRef]
- Saredakis, D.; Keage, H.A.; Corlis, M.; Loetscher, T. Using Virtual Reality to Improve Apathy in Residential Aged Care: Mixed Methods Study. J. Med. Internet Res. 2020, 22, e17632. [Google Scholar] [CrossRef]
- Shah, S.H.H.; Karlsen, A.S.T.; Solberg, M.; Hameed, I.A. A social vr-based collaborative exergame for rehabilitation: Codesign, development and user study. Virtual Real. 2022, 1–18. [Google Scholar] [CrossRef]
- Tyrrell, R.; Sarig-Bahat, H.; Williams, K.; Williams, G.; Treleaven, J. Simulator sickness in patients with neck pain and vestibular pathology during virtual reality tasks. Virtual Real. 2017, 22, 211–219. [Google Scholar] [CrossRef]
- Vailland, G.; Devigne, L.; Pasteau, F.; Nouviale, F.; Fraudet, B.; Leblong, E.; Babel, M.; Gouranton, V. VR based Power Wheelchair Simulator: Usability Evaluation through a Clinically Validated Task with Regular Users. In Proceedings of the 2021 IEEE Virtual Reality and 3D User Interfaces, Lisbon, Portugal, 27 March–1 April 2021; pp. 420–427. [Google Scholar] [CrossRef]
- Vlake, J.H.B.; Wils, E.-J.M.; van Bommel, J.M.; Korevaar, T.I.M.M.; Gommers, D.M.; van Genderen, M.E.M. Virtual Reality Tailored to the Needs of Post-ICU Patients: A Safety and Immersiveness Study in Healthy Volunteers. Crit. Care Explor. 2021, 3, e0388. [Google Scholar] [CrossRef]
- Winter, C.; Kern, F.; Gall, D.; Latoschik, M.E.; Pauli, P.; Käthner, I. Immersive virtual reality during gait rehabilitation increases walking speed and motivation: A usability evaluation with healthy participants and patients with multiple sclerosis and stroke. J. Neuroeng. Rehabil. 2021, 18, 1–14. [Google Scholar] [CrossRef]
- Tallarida, R.J.; Murray, R.B.; Tallarida, R.J.; Murray, R.B. Chi-square test. Man. Pharmacol. Calc. Comput. Programs 1987, 140–142. [Google Scholar]
- Kennedy, R.; Drexler, J.; Compton, D.; Stanney, K.; Lanham, D.; Harm, D. Configural scoring of simulator sickness, cybersickness and space adaptation syndrome: Similarities and differences. Virtual Adapt. Environ. Appl. Implic. Hum. Perform. Issues 2003, 2003, 247. [Google Scholar]
- Dilanchian, A.T.; Andringa, R.; Boot, W.R. A Pilot Study Exploring Age Differences in Presence, Workload, and Cybersickness in the Experience of Immersive Virtual Reality Environments. Front. Virtual Real. 2021, 2, 736793. [Google Scholar] [CrossRef]
- Xu, W.; Liang, H.-N.; Yu, K.; Baghaei, N. Effect of gameplay uncertainty, display type, and age on virtual reality exergames. In Proceedings of the 2021 CHI Conference on Human Factors in Computing Systems, Yokohama, Japan, 8–13 May 2021; pp. 1–14. [Google Scholar]
- Pietrzak, E.; Pullman, S.; McGuire, A. Using Virtual Reality and Videogames for Traumatic Brain Injury Rehabilitation: A Structured Literature Review. Games Health J. 2014, 3, 202–214. [Google Scholar] [CrossRef]
- Rose, F.D.; Brooks, B.M.; Rizzo, A.A. Virtual Reality in Brain Damage Rehabilitation: Review. CyberPsychology Behav. 2005, 8, 241–262. [Google Scholar] [CrossRef]
- Patel, M.; Snyder, A.R.; Baham, M.; Sheridan, C.A.; Brown, A.; Asarnow, R.; Babikian, T.; Choe, M.; Giza, C. Brief Autonomic Assessment in Concussion Clinic. Neurology 2020, 95, S4–S5. [Google Scholar] [CrossRef]
- Huang, H.-M.; Rauch, U.; Liaw, S.-S. Investigating learners’ attitudes toward virtual reality learning environments: Based on a constructivist approach. Comput. Educ. 2010, 55, 1171–1182. [Google Scholar] [CrossRef]
- Moraes, T.M.; Zaninotto, A.L.; Neville, I.S.; Hayashi, C.Y.; Paiva, W.S. Immersive virtual reality in patients with moderate and severe traumatic brain injury: A feasibility study. Health Technol. 2021, 11, 1035–1044. [Google Scholar] [CrossRef]
- Coyle, H.; Traynor, V.; Solowij, N. Computerized and Virtual Reality Cognitive Training for Individuals at High Risk of Cognitive Decline: Systematic Review of the Literature. Am. J. Geriatr. Psychiatry 2014, 23, 335–359. [Google Scholar] [CrossRef] [PubMed]
- Cushman, L.A.; Stein, K.; Duffy, C.J. Detecting navigational deficits in cognitive aging and Alzheimer disease using virtual reality. Neurology 2008, 71, 888–895. [Google Scholar] [CrossRef]
- Tuena, C.; Serino, S.; Stramba-Badiale, C.; Pedroli, E.; Goulene, K.M.; Stramba-Badiale, M.; Riva, G. Usability of an Embodied CAVE System for Spatial Navigation Training in Mild Cognitive Impairment. J. Clin. Med. 2023, 12, 1949. [Google Scholar] [CrossRef]
- Mondellini, M.; Arlati, S.; Gapeyeva, H.; Lees, K.; Märitz, I.; Pizzagalli, S.L.; Otto, T.; Sacco, M.; Teder-Braschinsky, A. User Experience during an Immersive Virtual Reality-Based Cognitive Task: A Comparison between Estonian and Italian Older Adults with MCI. Sensors 2022, 22, 8249. [Google Scholar] [CrossRef]
- García-Muñoz, C.; Cortés-Vega, M.-D.; Heredia-Rizo, A.M.; Martín-Valero, R.; García-Bernal, M.-I.; Casuso-Holgado, M.J. Effectiveness of vestibular training for balance and dizziness rehabilitation in people with multiple sclerosis: A systematic review and meta-analysis. J. Clin. Med. 2020, 9, 590. [Google Scholar] [CrossRef]
- Norouzi-Gheidari, N.; Hernandez, A.; Archambault, P.S.; Higgins, J.; Poissant, L.; Kairy, D. Feasibility, Safety and Efficacy of a Virtual Reality Exergame System to Supplement Upper Extremity Rehabilitation Post-Stroke: A Pilot Randomized Clinical Trial and Proof of Principle. Int. J. Environ. Res. Public Health 2019, 17, 113. [Google Scholar] [CrossRef]
- Risi, D.; Palmisano, S. Effects of postural stability, active control, exposure duration and repeated exposures on HMD induced cybersickness. Displays 2019, 60, 9–17. [Google Scholar] [CrossRef]
- Servotte, J.-C.; Goosse, M.; Campbell, S.H.; Dardenne, N.; Pilote, B.; Simoneau, I.L.; Guillaume, M.; Bragard, I.; Ghuysen, A. Virtual reality experience: Immersion, sense of presence, and cybersickness. Clin. Simul. Nurs. 2020, 38, 35–43. [Google Scholar] [CrossRef]
- Chandra, A.N.R.; El Jamiy, F.; Reza, H. A Systematic Survey on Cybersickness in Virtual Environments. Computers 2022, 11, 51. [Google Scholar] [CrossRef]
- Saint-Aubert, J.; Cogné, M.; Bonan, I.; Launey, Y.; Lécuyer, A. Influence of user posture and virtual exercise on impression of locomotion during vr observation. IEEE Trans. Vis. Comput. Graph. 2022, 14, 8. [Google Scholar] [CrossRef]
- Mittelstaedt, J.; Wacker, J.; Stelling, D. Effects of display type and motion control on cybersickness in a virtual bike simulator. Displays 2018, 51, 43–50. [Google Scholar] [CrossRef]
- Petrigna, L.; Musumeci, G. The Metaverse: A New Challenge for the Healthcare System: A Scoping Review. J. Funct. Morphol. Kinesiol. 2022, 7, 63. [Google Scholar] [CrossRef]
- Yang, J.O.; Lee, J.S. Utilization exercise rehabilitation using metaverse (vr· ar· mr· xr). Korean J. Sport Biomech. 2021, 31, 249–258. [Google Scholar]
- Garavand, A.; Aslani, N. Metaverse phenomenon and its impact on health: A scoping review. Inform. Med. Unlocked 2022, 32, 101029. [Google Scholar] [CrossRef]
- Garrido, L.E.; Frías-Hiciano, M.; Moreno-Jiménez, M.; Cruz, G.N.; García-Batista, Z.E.; Guerra-Peña, K.; Medrano, L.A. Focusing on cybersickness: Pervasiveness, latent trajectories, susceptibility, and effects on the virtual reality experience. Virtual Real. 2022, 26, 1347–1371. [Google Scholar] [CrossRef]
- Stanney, K.; Lawson, B.D.; Rokers, B.; Dennison, M.; Fidopiastis, C.; Stoffregen, T.; Weech, S.; Fulvio, J.M. Identifying Causes of and Solutions for Cybersickness in Immersive Technology: Reformulation of a Research and Development Agenda. Int. J. Human-Comput. Interact. 2020, 36, 1783–1803. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).