Abstract
Background: Dentists administer hundreds of thousands of injections every day without particular concern, but the administration of local anesthetics can cause problems. One event, fortunately uncommon, that is discussed accurately but can cause significant concern is needle breakage. The purpose of this article is to review what has been reported in the literature on this topic to learn about patient symptomatology, management and possible complications. In addition, the case of a 34-year-old patient with needle persistence in the pterygoid space due to accidental rupture during inferior alveolar nerve block (IAN) was reported, for whom non-removal and monitoring over time was chosen. Materials and Methods: A literature search of the PubMed, Scopus, Web of Science and ScienceDirect databases was conducted analyzing anesthetic needle rupture during dental surgery. Results: At the end of the selection process, 17 articles resulted. Asymptomatic subjects were found, as well as those who had several symptoms. No issues were recorded by any of the authors, whether they withdrew the needle or simply monitored the patient. Conclusions: The literature on needle rupture during dental local anesthesia is scarce, and studies report conflicting results on treatment options. Most authors reported removing the fragment; however, others preferred conservative management limited to patient monitoring. No complications were reported in any study.
1. Introduction
Several dental and oral surgical procedures necessitate the use of regional (local) anesthetic [1]. Although some patients may be subjected to systemic inhalation or intravenous sedation, the use of local anesthesia is still necessary, so dental needles are an essential part of dental practice [2,3]. The needle used must be chosen depending on the practitioner’s competence as well as the injection type and depth of penetration required [4,5].
The gauge of the needle is the diameter of its lumen (or hollow tube), which in clinical practice is between 25G and 30G [6,7]. The needle should be long enough to never be positioned less than 5 mm from the hub, as this is the weakest point of the needle and if subjected to stress it could break [8,9,10]. The needle used is chosen according to the injection technique and the anatomical point, and dentists are particularly prepared for the various infiltration methods that the procedure and the area to be anesthetized require [11].
Local anesthesia is a reversible blockage of nerve transmission in a specific location that causes feeling loss. The chemical agents used to create local anesthetic stabilize neuronal membranes by limiting the ionic fluxes necessary for neural impulse propagation [12]. Today’s anesthetics are safe, effective, and may be delivered with little soft tissue irritation and allergic responses [13,14,15,16]. One of the aims of this article is to raise awareness of the risk of needle rupture as a possible complication associated with the use of local anesthetics [17,18,19]. Knowing the dangers of local anesthetic reduces the likelihood of adverse events and leads to better patient care [20]. Albert Niemann extracted the first local anesthetic from coca leaves in the 1860s in Germany [21,22,23,24,25]. Karl Koller, a young ophthalmology resident, was Freud’s youthful colleague [26,27]. Koller was advised by Freud to try cocaine as a local anesthetic [28]. Koller was the first to publish a study on the use of cocaine as a local anesthetic agent in 1884 [29,30]. After Koller’s study, Halsted administered cocaine near a medical student’s mandibular nerve, and the student’s tongue, lower lip, and teeth were numb within a few minutes [25,31]. The Harrison Narcotics Tax Act soon after prohibited the sale and distribution of cocaine in the United States [32]. Alfred Einhorn discovered procaine (Novocain) in 1905, which was a significant development in local anesthetic. Shortly after, adrenaline was added to procaine to boost its effectiveness [33]. A Swedish business created lidocaine in 1949, an amino amide-based local anesthetic with fewer side effects and a deeper anesthetic than Novocain [34,35]. Articaine 4% with epinephrine 1:100,000 and articaine 4% with epinephrine 1:200,000 were approved by the US Food and Drug Administration in 2000. In most countries, lidocaine is the most often used local dental anesthetic [36,37,38].
Dentists administer hundreds of thousands of injections every day without any significant complications. The performance of local anesthesia is associated with anatomical and pharmacological considerations that may cause complications ranging from simple discomfort to the death of the subject [39,40]. Among the clinical manifestations that can rarely be seen is anisocoria, a different width of the two papillae that must be at least 0.4 millimeters observable even when exposed to the same illumination of both eyes after oral surgery [41,42]. Many complications are secondary to anxiety, local anesthetic toxicity or allergies, and in this case can be classified as systemic. In contrast, many others, such as needle rupture, can be termed localized complications that occur as a rare but possible event [39,43].
According to Augello et al., over the past 50 years, a total of 64 cases were discovered in 34 published articles on needle rupture, of which 45, approximately 70 percent, occurred during inferior alveolar nerve injury (IAN) [39].
Pogrel estimated an incidence of 1 needle fracture per 14 million inferior alveolar nerve blocks [2,10]. The scientific literature seems to suggest that needle fracture is more common when administering an inferior alveolar nerve block than with other techniques [44,45].
A case history on the breakage of dental needles was published in 1928 by Blum, who reported the breakage of 65 needles over 10 years [43].
This complication was more frequent before the 1960s due to the use of stiffer, non-disposable needles that were subjected to repeated sterilization cycles that reduced their breaking strength [46].
It is an event that causes a great deal of fear for both doctor and patient. To date, a few cases of needle rupture, although not numerous, without serious complications, such as damage to important anatomical structures, are continually reported because most dentists know the causes of these complications [47].
Needle breakage can be caused by improper technique or sudden movement of the patient when the needle penetrates the tissue or contacts the periosteum or bending the needle several times before its use. The patient’s movement to cause rupture should be in the opposite direction to that of the needle, so that the contact force can eventually either produce defects or break the needle. Therefore, it is essential to inform the patient and warn them against sudden movements during administration [44,48].
This complication frequently occurs during IAN anesthesia when direct and indirect techniques are used, which involve the injection of a local anesthetic to block the IAN. Of the two approaches, the indirect technique is more likely to break the needle because during its execution, the needle makes movements in the tissue context before reaching the target [49,50]. The movements imposed on the needle during the indirect technique result in twisting forces that can cause it to break, especially if the needle is small in diameter. Since one of the most important causes is pain, slow injections should be performed while avoiding inflicting the needle tip on the periosteum. These precautions prevent spontaneous head movements [43].
If needle fragment can be removed from the tissue without surgical intervention, the risk of severe diseases is absent. Needle breakage does not cause any serious problems. Needle fragments that cannot be removed migrate and are incarcerated in the tissue within a few weeks [47,51,52]. Therefore, the recommended needle according to Bedrock et al. should be 35 mm long and 27 gauge for IAN blockage. Many dentists prefer to use small needles to reduce the pain caused by the injection, but the risk of breakage increases since they can be easily deflected during passage through the tissues. It has been shown that there is no difference in the perception of pain produced by 25-, 27- and 30-gauge needles [2,8].
Needle breakage during administration can be attributed to a defective needle. The needle should be carefully inspected before use for irregularities or defects visible to the naked eye. The needle should not be bent before anesthesia. New metal alloys and non-reusable needles have dramatically reduced the incidence of needle breakage in dentistry [44,49,53].
Fear of dental treatment is common in children and the management of the young patient may compromise adequate care and increase the risk of needle breakage due to rapid head movement [51,52]. There are several techniques to reduce the pain caused by anesthetic administration. The most widely used is topical anesthesia, which reduces the pain associated with needle insertion. To overcome fear, one of the most widely used methods is sedation with nitrous oxide. This laughing gas that induces analgesia and anxiolysis, causing depression and euphoria in the central nervous system [51].
The purpose of this article is to review what has been reported in the literature on this topic to learn about patient symptomatology, management and possible complications. In addition, the case of a 34-year-old patient with needle persistence in the pterygoid space due to accidental rupture during inferior alveolar nerve block (IAN) was reported, for whom non-removal and monitoring over time was chosen.
2. Materials and Methods
2.1. Protocol and Registration
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) protocols were followed when conducting this review, and it was submitted to PROSPERO with a temporary number (n. 393680) [54].
2.2. Search Processing
We searched PubMed, Scopus, Web of Science, and ScienceDirect with a constraint on English-language papers from 1 January 2012 through 5 January 2023 that matched our topic. The following Boolean keywords were utilized in the search strategy: “dental” AND “needle” AND “complication”. These terms were chosen because they best described the goal of our inquiry, which was to learn more about needle rupture during a dental loco-regional anesthetic operation.
2.3. Inclusion Criteria
All appropriate trials were assessed by three reviewers using the following selected criteria: (1) Only studies with human subjects; (2) open-access studies that other researchers can access for free; (3) scientific research demonstrating anesthetic needle rupture during dental surgery. Articles in non-English languages and those addressing additional problems besides needle rupture as a complication were eliminated. The PICO model was developed in the following manner:
- Population: human subjects in whom needle rupture had occurred during dental anesthesia. No restrictions on health status, sex and age;
- Intervention: removal of needle;
- Comparison: no removal of needle;
- Outcome: treatment and complications.
2.4. Data Processing
Author disagreements on the choice of article were discussed and settled.
2.5. Article Identification Procedure
The suitability assessment was conducted independently by three reviewers (G.P., C.D.P. and F.P.). In addition, a manual search was conducted to increase the pool of articles for full-text evaluation. Articles written in English that met the inclusion criteria were taken into account, while duplicates and excluded articles were categorized by stating the reasons for exclusion.
2.6. Study Evaluation
The article data were independently evaluated by the reviewers using a special electronic form designed according to the following categories: study model design, patient age, injection technique, cause of breakage, location of fragment, X-ray/imaging, signs and symptoms correlated, whether the needle is removed or not, and complications.
3. Results
A total of 227 publications were identified from the following databases: PubMed (48), Scopus (114), Web of Science (39) and ScienceDirect (26), which led to 171 articles after removing duplicates (56). Analysis of the title and abstract resulted in the exclusion of 136 articles. The writers successfully sought the remaining 35 papers for retrieval and evaluated their eligibility. The approach resulted in the exclusion of 18 articles for being off-topic. The evaluation includes the final 17 papers for qualitative analysis (Figure 1).
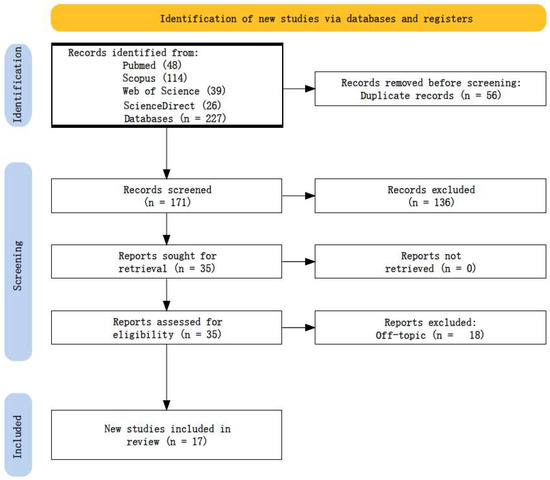
Figure 1.
PRISMA flowchart diagram of the inclusion process.
The research shows that 13 articles evaluate patients who were administered inferior alveolar nerve block; in two articles, patients were administered local anesthesia; two other articles do not describe the type of anesthesia performed. It is inferred that less than half of the authors report the absence of symptomatology, one author does not evaluate the presence or absence of symptoms, and the remainder describe symptoms such as acute facial and neck pain, dysphagia, lockjaw, headache, tenderness, tinnitus, hearing loss, oral pain, difficulty opening the mouth, inflammation in the injection area, fever, vomiting, headache, nausea, photo-phono phobia, and nuchal rigidity. Most authors describe cases in which the fragment was eliminated; furthermore, none of the cases evaluated had complications.
4. Discussion
Since the introduction of local anesthesia, the risk of needle breakage during injection has emerged [55]. Despite a long history of challenges associated with needle breakage, the debate over a way to address such instances has persisted. When a break occurs, all medical experts agree that the patient must be alerted immediately, and the episode must be thoroughly documented [56,57]. The patient requires comfort and an immediate referral for treatment to an oral and maxillofacial surgeon [56]. Many case reports are present in the literature. Omori et al. show a case of broken injection needle during the extraction of a lower third molar [39]: the dentist chose to follow up the patient conservatively because it was unclear where the fractured section was located. After the extraction, the patient showed no signs of the presence of a foreign body. Tenderness in the incision persisted after the patient returned to the dentist for suture removal. One week later, due to the use of a 3D CT, the fragment was localized in the ramus of the mandible and was removed from the mucosal side [39]. Brooks et al. and Moore et al. showed dental needles that unusually migrated in the carotid space and were removed with coronal angiogram and CT [49,52]. In the first case, the general dentist asserted that there was no need to retrieve the needle before dismissing the patient. The patient manifested severe pain and dysphagia a few weeks later. After using conventional retrieval methods without success, Brooks et al. turned to the neurosurgical team. The needle was removed from the right internal carotid artery using endovascular surgery along with digital subtraction angiography [49]. In addition, Moore et al. referred the patient to vascular surgery and otolaryngology, where the fragment that migrated into the jugular foramen was removed. The authors emphasize that any foreign object that can pass through the upper digestive tract mucosa may be able to penetrate into nearby tissues, particularly the vasculature, and inflict further harm [58,59,60,61]. Another case of migration in a noble structure is presented by Casey et al.: the fractured needle migrated and penetrated the cochlea, causing hearing loss that fortunately improved after the removal of the fragment [53]. Despite some clinicians recommending removal of the needle as soon as possible to avoid complications from needle migration into important head and neck structures, other clinicians believe that broken needles should be treated similarly to small, noninfected root tips [62,63]; scar tissue will form around them and fibrosis will prevent complications [64]. Goulart et al. prefer a conservative approach, monitoring the asymptomatic patient and leaving the fractured needle in the posterior cervical area to avoid surgical intervention and its relative risks such as vessel injury [46]. Practitioners who support this course of therapy must keep a careful eye on the patient to make sure any issues are identified and dealt with as soon as possible [62,65,66].
Many authors suggest removing a broken needle to prevent pain, facial trismus, infection and migration of the foreign body [39,46,67]. At the moment of rupture, the dentist must not panic, urge the patient not to move and keep the mouth open. If the fragment is visible, an attempt can be made to remove it with forceps. On the other hand, if the needle has been lost and is no longer visible or cannot be extracted easily, one must always urge the patient to remain calm and proceed without cutting [8]. The data should then be entered into the medical record and the patient should be referred to the maxillofacial surgeon. Removal is essential because broken needles can migrate into the head and neck, damaging adjacent vital anatomical structures [46,67].
The localization of the fragment can be achieved using two- or three-dimensional image approaches such as image-guided navigation using computed tomography (CT); magnetic resonance angiography (MRI); ultrasound examination [39,48,68,69,70].
Since iron was removed from the iron alloy used to make dental needles to enhance its mechanical qualities, electromagnets can no longer be utilized to locate dental needles [65,66,71]. For pinpointing the needle position, two plain film radiographs—a panoramic or lateral cephalometric radiograph combined with a postero-anterior (PA) radiograph with 2–3 needle locations—may be useful. However, radiographs do not present the same level of accuracy as a CT scan [72]. Another proposed possibility is stereotactic imaging with two localizing needles. It has been recommended to employ intraoperative ultrasound imaging to locate foreign things in the neck, but sadly, its application in a tiny mouth cavity may be restricted [62]. For removing the foreign body, an intraoperative navigation system can also be used for an image-guided surgery as successfully shown by Gerbino et al., Schorn et al. and Stein et al. [50,67,73].
Two unusual cases of Brooks et al. and Moore et al. show dental needles that migrated in the carotid space and were removed with coronal angiogram and CT [49,52].
As described by these case reports, tenderness, dysphagia, discomfort, and trismus are among the symptoms that patients may mention, while some may be wholly asymptomatic [39,49,74].
Complications such as paresthesia are not described in the literature, and in the most of case series presented in this review, the fragment was successfully removed [39,40,43,44,45,47,48,49,50,51,52,53,67,74] (Table 1).

Table 1.
Studies included for qualitative analysis.
By being diligent and knowledgeable about all the factors that enhance the likelihood of needle breakage, practitioners can lower the occurrence of needle breakage providing an injection only with the patient’s complete agreement and involvement, considering that quick movements have been linked to needle breakage [26,62,75]. Risk for needle fracture increases in noncooperative patients, as in the case described by Chybicki et al., where a sudden movement of a 6-year-old autistic patient occurred during the injection with a computer-controlled local anesthesia device [51]. The same occurred in the case of Bagattoni et al. during the treatment of a patient affected by KBG syndrome [68].
Multiple injections should not be performed using the same needle. The needles become blunter with usage, increasing the discomfort of each consecutive injection for the patient and necessitating greater force to puncture the tissue; the chance of the needle breaking rises with higher pressure [55,62].
Smaller needles are believed by some clinicians to be more prone to breaking. Since most breaking happens with 30-gauge or smaller needles, some authors advise using at least a 27-gauge needle for all blocks [55,62,64,65,76]. Also to be noted is that most patients are unable to distinguish between a 27-gauge and 30-gauge needle [17,77]. Any benefit from puncturing the tissue with a smaller needle is lost due to the fact that injection pressure is frequently more uncomfortable with a 30-gauge needle [17,78].
The needle–hub junction is a needle’s weakest point [72,79]. In order to prevent being buried to the hub, a needle must be long enough [55]. A needle should never be put into the tissue past a bend or up to the hub since this creates an additional point of vulnerability to the needle and the vulnerable hub [17]. By following this guideline, it may be ensured that if a needle does break, it will be simple to remove because part of it will be poking out of the tissue. Shah et al. recommend avoiding soft tissue palpation as it may cause migration of the needle if it disappears under the mucosa. In addition, the dentists should advise the patient the importance of avoiding mouth opening and closing maneuvers to minimize needle migration [80]. Knowledge of the pertinent anatomy in great detail is necessary for proper technique application [17,56].
It should be considered that this review does not receive any funding, so the authors included only open-access studies and this can represent a limitation. In addition, as a large case report of studies on this topic was not found, it was not possible to perform a detailed search with targeted keywords, nor a careful selection by assessing the quality of the included studies. Finally, only the occurrence of needle breakage during anesthesia in the dental field was analyzed without information about the breakage of needles in general. The items included are schematized in Table 1. Further researches could investigate this topic, which is a possible occurrence in all areas of medicine.
5. Case Report
A 34-year-old man came to the authors’ attention, reporting that seven years before he underwent a conservative treatment of the right mandibular second molar by his general dentist. During the IAN block, a dental needle was accidentally fractured and the dentist failed to recover the fragment. At our examination, the needle was not visible or palpable clinically and the patient experienced no pain, dysphagia, or right inferior alveolar nerve paresthesia.
A latero-lateral skull teleradiography (Figure 2) and Cone Beam Computed Tomography (CBCT) with 3D volume-rendered images depicted the needle in the bundle of the lateral pterygoid space that measures about 24 mm (Figure 3A,B and Figure 4A,B). The patient was informed of the risks and advantages of having the needle surgically removed vs leaving it in place. The patient came to our attention seven years after the needle fracture. Several cases of broken needle migration over time show that it is preferable to remove the broken needle as quickly as possible. Therefore, the patient was informed that the disadvantage of non-removal is the migration of the needle, while the removal can be difficult due to the poor precision of its location. The patient chose conservative treatment so the authors organized follow-up with a CBCT every year to monitor the fragment.
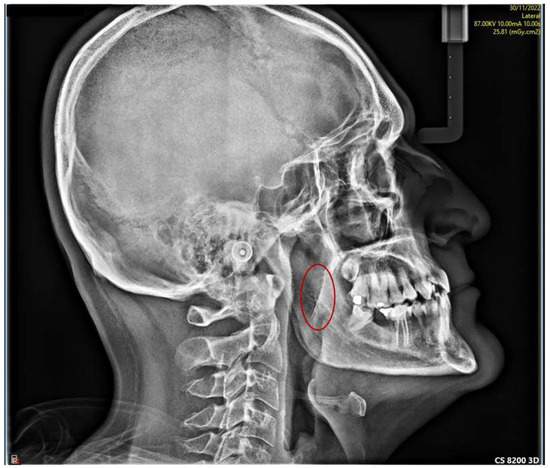
Figure 2.
Latero-lateral skull teleradiography showing the fractured needle (red circle).
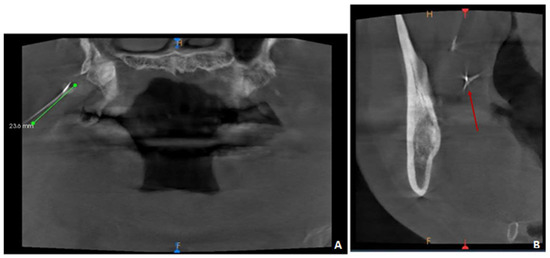
Figure 3.
(A) CBCT views with the fragment measure (23.6 mm); (B) CBCT views with part of a needle visualized in the right pterygomandibular space (red arrow). Scattering effect due to the presence of metal.
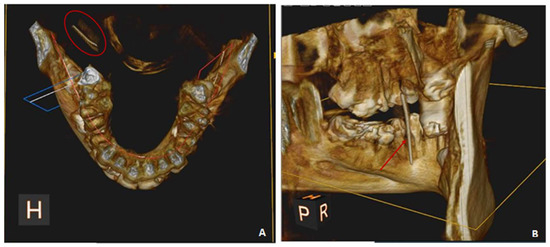
Figure 4.
(A) Reproduction of a three-dimensional image of the facial bone showing the fractured needle (red circle); (B) other projection of a three-dimensional image of the facial bone showing the fractured needle (red arrow).
6. Conclusions
Poor patient compliance, rapid patient head movements, application of excessive force during injection, angular or directional changes in needle insertion may increase the risk of needle pre-curvature and needle fracture. No complications after fragment removal were detected. Knowledge of the pertinent anatomy in great detail is necessary for proper technique application. Every effort must be made to avoid the uncommon but significant consequence of a broken needle during dental treatment. In the event that a needle breaks, the practitioner must inform the patient and perform the necessary radiographs, thoroughly document the situation, and refer the patient to an oral surgeon right away for care.
Author Contributions
Conceptualization, A.M.I., A.D.I., G.M., F.P., A.P. and C.D.P.; methodology, G.P., V.S., N.C. and A.M.; software, F.I., B.R. and G.D.; validation, D.D.V., F.P., F.I. and G.D.; formal analysis, A.D.I., F.P., A.P., D.D.V., F.I. and G.D.; resources, A.D.I., A.M.I., G.M., C.D.P., A.M. and V.S.; data curation, G.M., G.D., F.I., V.S. and C.D.P.; writing—original draft preparation, A.D.I., A.M.I., F.P., D.D.V., N.C., F.I. and G.D.; writing—review and editing, N.C., A.P., V.S., G.M., B.R., G.P. and A.P.; visualization, G.P., C.D.P., B.R., A.M., A.P. and N.C.; supervision, A.D.I., A.M.I., F.P., G.M., D.D.V., F.I. and G.D.; project administration, B.R., A.P., F.I. and G.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| CBCT | cone beam computer tomography |
| CT | computed tomography |
| IAN | inferior alveolar nerve |
| LL | latero-lateral teleradiography |
| MRI | magnetic resonance angiography |
| OPT | orthopantomogram |
| PA | postero-anterior |
References
- St George, G.; Morgan, A.; Meechan, J.; Moles, D.R.; Needleman, I.; Ng, Y.-L.; Petrie, A. Injectable Local Anaesthetic Agents for Dental Anaesthesia. Cochrane Database Syst. Rev. 2018, 7, CD006487. [Google Scholar] [CrossRef] [PubMed]
- Taylor, G.D.; Campbell, C. A Clinical Guide to Needle Desensitization for the Paediatric Patient. Dent. Update 2015, 42, 373–374. [Google Scholar] [CrossRef] [PubMed]
- Sokhov, S.T.; Topolnitskiy, O.Z.; Bogaevskaya, O.Y.; Kosareva, N.V. Medical solution to needle breakage during local anesthesia. Stomatologiia 2019, 98, 29–32. [Google Scholar] [CrossRef]
- Mundiya, J.; Woodbine, E. Updates on Topical and Local Anesthesia Agents. Oral Maxillofac. Surg. Clin. N. Am. 2022, 34, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Malamed, S.F.; Reed, K.; Poorsattar, S. Needle Breakage: Incidence and Prevention. Dent. Clin. N. Am. 2010, 54, 745–756. [Google Scholar] [CrossRef]
- Makwana, M.; Walsh, S. Patient Safety: Needle Breakage. Br. Dent. J. 2017, 222, 140. [Google Scholar] [CrossRef]
- Lee, T.Y.T.; Zaid, W.S. Broken Dental Needle Retrieval Using a Surgical Navigation System: A Case Report and Literature Review. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2015, 119, e55–e59. [Google Scholar] [CrossRef]
- Lee, H.-S. Recent Advances in Topical Anesthesia. J. Dent. Anesth. Pain Med. 2016, 16, 237–244. [Google Scholar] [CrossRef]
- Hartmann, A.; Lawall, T.; Philipp, L.; Daubländer, M. Needle Tip Deformation in Local Dental Anesthesia—A Technical Note. J. Mech. Behav. Biomed. Mater. 2022, 126, 105034. [Google Scholar] [CrossRef]
- Alameeri, A.A.; AlShamsi, H.A.; Murad, A.; Alhammadi, M.M.; Alketbi, M.H.; AlHamwi, A.; Rawi, N.H.A.; Kawas, S.A.; Mohammed, M.M.; Shetty, S.R. The Feasibility of Needleless Jet Injection versus Conventional Needle Local Anesthesia during Dental Procedures: A Systematic Review. J. Korean Assoc. Oral Maxillofac. Surg. 2022, 48, 331–341. [Google Scholar] [CrossRef]
- Acham, S.; Truschnegg, A.; Rugani, P.; Kirnbauer, B.; Reinbacher, K.E.; Zemann, W.; Kqiku, L.; Jakse, N. Needle Fracture as a Complication of Dental Local Anesthesia: Recommendations for Prevention and a Comprehensive Treatment Algorithm Based on Literature from the Past Four Decades. Clin. Oral Investig. 2019, 23, 1109–1119. [Google Scholar] [CrossRef] [PubMed]
- The Gow-Gates Mandibular Block: Further Understanding. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2516150/ (accessed on 21 February 2023).
- Atlas of Minor Oral Surgery|WorldCat.Org. Available online: https://www.worldcat.org/it/title/atlas-of-minor-oral-surgery/oclc/728663388 (accessed on 21 February 2023).
- Wawersik, J. History of Anesthesia in Germany. J. Clin. Anesth. 1991, 3, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Uckan, S.; Cilasun, U.; Erkman, O. Rare Ocular and Cutaneous Complication of Inferior Alveolar Nerve Block. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2006, 64, 719–721. [Google Scholar] [CrossRef] [PubMed]
- Ogle, O.E.; Mahjoubi, G. Local Anesthesia: Agents, Techniques, and Complications. Dent. Clin. N. Am. 2012, 56, 133–148. [Google Scholar] [CrossRef]
- Malamed, S.F. Handbook of Local Anesthesia; Elsevier Health Sciences: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Renton, T.; Adey-Viscuso, D.; Meechan, J.G.; Yilmaz, Z. Trigeminal Nerve Injuries in Relation to the Local Anaesthesia in Mandibular Injections. Br. Dent. J. 2010, 209, E15. [Google Scholar] [CrossRef]
- Ring, M.E. The History of Local Anesthesia. J. Calif. Dent. Assoc. 2007, 35, 275–282. [Google Scholar] [CrossRef]
- Pogrel, M.A.; Schmidt, B.L.; Sambajon, V.; Jordan, R.C.K. Lingual Nerve Damage Due to Inferior Alveolar Nerve Blocks: A Possible Explanation. J. Am. Dent. Assoc. 2003, 134, 195–199. [Google Scholar] [CrossRef]
- Pogrel, M.A. Broken Local Anesthetic Needles: A Case Series of 16 Patients, with Recommendations. J. Am. Dent. Assoc. 2009, 140, 1517–1522. [Google Scholar] [CrossRef]
- Pogrel, M.A.; Thamby, S. Permanent Nerve Involvement Resulting from Inferior Alveolar Nerve Blocks. J. Am. Dent. Assoc. 2000, 131, 901–907. [Google Scholar] [CrossRef]
- Pogrel, M.A.; Bryan, J.; Regezi, J. Nerve Damage Associated with Inferior Alveolar Nerve Blocks. J. Am. Dent. Assoc. 1995, 126, 1150–1155. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Malcangi, G.; Semjonova, A.; Inchingolo, A.M.; Patano, A.; Coloccia, G.; Ceci, S.; Marinelli, G.; Di Pede, C.; Ciocia, A.M.; et al. Oralbiotica/Oralbiotics: The Impact of Oral Microbiota on Dental Health and Demineralization: A Systematic Review of the Literature. Children 2022, 9, 1014. [Google Scholar] [CrossRef] [PubMed]
- von Arx, T.; Lozanoff, S.; Zinkernagel, M. Ophthalmologic Complications after Intraoral Local Anesthesia. Swiss Dent. J. 2014, 124, 784–806. [Google Scholar] [PubMed]
- Marinho, R.O. Abducent Nerve Palsy Following Dental Local Analgesia. Br. Dent. J. 1995, 179, 69–70. [Google Scholar] [CrossRef] [PubMed]
- Carl Koller and Cocaine. Br. J. Ophthalmol. 1928, 12, 262–263. [CrossRef]
- Kronman, J.H.; Kabani, S. The Neuronal Basis for Diplopia Following Local Anesthetic Injections. Oral Surg. Oral Med. Oral Pathol. 1984, 58, 533–534. [Google Scholar] [CrossRef] [PubMed]
- Kravitz, N.D. The Use of Compound Topical Anesthetics: A Review. J. Am. Dent. Assoc. 2007, 138, 1333–1339; quiz 1382. [Google Scholar] [CrossRef]
- Sambrook, P.J.; Goss, A.N. Severe Adverse Reactions to Dental Local Anaesthetics: Prolonged Mandibular and Lingual Nerve Anaesthesia. Aust. Dent. J. 2011, 56, 154–159. [Google Scholar] [CrossRef]
- Jackson, D.; Chen, A.H.; Bennett, C.R. Identifying True Lidocaine Allergy. J. Am. Dent. Assoc. 1994, 125, 1362–1366. [Google Scholar] [CrossRef]
- Pippi, R.; Spota, A.; Santoro, M. Medicolegal Considerations Involving Iatrogenic Lingual Nerve Damage. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2018, 76, 1651.e1–1651.e13. [Google Scholar] [CrossRef]
- Buckenmaier, C.C.; Bleckner, L.L. Anaesthetic Agents for Advanced Regional Anaesthesia: A North American Perspective. Drugs 2005, 65, 745–759. [Google Scholar] [CrossRef]
- Goldenberg, A.S. Transient Diplopia from a Posterior Alveolar Injection. J. Endod. 1990, 16, 550–551. [Google Scholar] [CrossRef] [PubMed]
- Joshi, A.; Jain, A.; Chimote, M.M. Etiology and Pathophysiological Pathways of Ocular Complications Associated with Local Dental Anesthesia and Odontogenic Infections: A Systematic Review. J. Maxillofac. Oral Surg. 2022, 21, 648–667. [Google Scholar] [CrossRef] [PubMed]
- Garisto, G.A.; Gaffen, A.S.; Lawrence, H.P.; Tenenbaum, H.C.; Haas, D.A. Occurrence of Paresthesia after Dental Local Anesthetic Administration in the United States. J. Am. Dent. Assoc. 2010, 141, 836–844. [Google Scholar] [CrossRef]
- Gaffen, A.S.; Haas, D.A. Retrospective Review of Voluntary Reports of Nonsurgical Paresthesia in Dentistry. J. Can. Dent. Assoc. 2009, 75, 579. [Google Scholar]
- Bonifacio, C.C. The Efficacy of Articaine and Lidocaine Local Anaesthetic in Child Patients. Evid. Based Dent. 2018, 19, 105–106. [Google Scholar] [CrossRef] [PubMed]
- Omori, M.; Nakano, H.; Okae, A.; Yonenaga, T.; Yamamoto, K.; Yamamoto, N.; Nakajima, Y.; Ueno, T. A Case of the Accidental Insertion of a Broken Injection Needle for Local Anesthesia That Was Removed after a Week. J. Oral Maxillofac. Surg. Med. Pathol. 2021, 33, 434–437. [Google Scholar] [CrossRef]
- Lee, J.; Park, M.W.; Kim, M.K.; Kim, S.M.; Seo, K.-S. The Surgical Retrieval of a Broken Dental Needle: A Case Report. J. Dent. Anesth. Pain Med. 2015, 15, 97. [Google Scholar] [CrossRef]
- Inchingolo, F.; Tatullo, M.; Abenavoli, F.M.; Marrelli, M.; Inchingolo, A.D.; Villabruna, B.; Inchingolo, A.M.; Dipalma, G. Severe Anisocoria after Oral Surgery under General Anesthesia. Int. J. Med. Sci. 2010, 7, 314–318. [Google Scholar] [CrossRef]
- Farahmand, M.M.; Danesteh, H.; Mohamadkhani, H.; Eftekharian, H.R. Transient Benign Unilateral Dilated Pupil after Pathologic Oral Surgery under General Anesthesia: A Case Report. Adv. Oral Maxillofac. Surg. 2023, 9, 100390. [Google Scholar] [CrossRef]
- Rahman, D.N. Case Report: Management of Broken Dental Needles in Practice. J. Ir. Dent. Assoc. 2013, 59, 241–245. [Google Scholar]
- Bailey, E.; Rao, J.; Saksena, A. Case Report: Fractured Needle in the Pterygomandibular Space Following Administration of an Inferior Dental Nerve Block. Dent. Update 2015, 42, 270–272. [Google Scholar] [CrossRef] [PubMed]
- Erdil, A.; Demirsoy, M.S.; Çolak, S. Fractured Needle as an Unusual Complication of the Lingual Nerve Block: A Case Report. J. Dent. Anesth. Pain Med. 2022, 22, 315. [Google Scholar] [CrossRef]
- Goulart, D.R.; Harber, R.; Botelho, M.R.; de Moraes, M. Migration of a Broken Dental Needle into the Posterior Cervical Space. Oral Surg. 2016, 9, 252–257. [Google Scholar] [CrossRef]
- Kim, J.-H.; Moon, S.-Y. Removal of a Broken Needle Using Three-Dimensional Computed Tomography: A Case Report. J. Korean Assoc. Oral Maxillofac. Surg. 2013, 39, 251. [Google Scholar] [CrossRef]
- de Oliveira E Britto Villalobos, M.I.; Leite, T.C.G.F.; Barra, S.G.; da Cunha Werneche, D.T.P.; Manzi, F.R.; Cardoso, C.A.E.A. Radiographic and Computed Tomography Monitoring of a Fractured Needle Fragment in the Mandibular Branch. Imaging Sci. Dent. 2017, 47, 63. [Google Scholar] [CrossRef]
- Brooks, J.; Murphy, M.T. A Novel Case of a Broken Dental Anesthetic Needle Transecting the Right Internal Carotid Artery. J. Am. Dent. Assoc. 2016, 147, 739–742. [Google Scholar] [CrossRef]
- Stein, K.M. Use of Intraoperative Navigation for Minimally Invasive Retrieval of a Broken Dental Needle. J. Oral Maxillofac. Surg. 2015, 73, 1911–1916. [Google Scholar] [CrossRef] [PubMed]
- Chybicki, D.; Lipczyńska-Lewandowska, M.; Torbicka, G.; Janas-Naze, A. Computer-Controlled Local Anesthesia Complication: Surgical Retrieval of a Broken Dental Needle in Noncooperative Autistic Paediatric Patient. Case Rep. Dent. 2020, 2020, 6686736. [Google Scholar] [CrossRef]
- Moore, K.; Khan, N.R.; Michael, L.M.; Arthur, A.S.; Hoit, D. Republished: Endovascular Retrieval of Dental Needle Retained in the Internal Carotid Artery. J. Neurointerv. Surg. 2017, 9, e26. [Google Scholar] [CrossRef]
- Casey, J.T.; Lupo, J.E.; Jenkins, H.A. Retained Dental Needle Migration Across the Skull Base to the Cochlea Presenting as Hearing Loss. Otol. Neurotol. 2015, 36, e42–e45. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Ethunandan, M.; Tran, A.L.; Anand, R.; Bowden, J.; Seal, M.T.; Brennan, P.A. Needle Breakage Following Inferior Alveolar Nerve Block: Implications and Management. Br. Dent. J. 2007, 202, 395–397. [Google Scholar] [CrossRef] [PubMed]
- Zeltser, R.; Cohen, C.; Casap, N. The Implications of a Broken Needle in the Pterygomandibular Space: Clinical Guidelines for Prevention and Retrieval. Pediatr. Dent. 2002, 24, 153–156. [Google Scholar] [PubMed]
- Orr, D.L. The Broken Needle: Report of Case. J. Am. Dent. Assoc. 1983, 107, 603–604. [Google Scholar] [CrossRef] [PubMed]
- Woodhouse, J.B.; Uberoi, R. Techniques for Intravascular Foreign Body Retrieval. Cardiovasc. Intervent. Radiol. 2013, 36, 888–897. [Google Scholar] [CrossRef] [PubMed]
- Osinubi, O.A.; Osiname, A.I.; Pal, A.; Lonsdale, R.J.; Butcher, C. Foreign Body in the Throat Migrating through the Common Carotid Artery. J. Laryngol. Otol. 1996, 110, 793–795. [Google Scholar] [CrossRef] [PubMed]
- Tang, I.P.; Singh, S.; Shoba, N.; Rahmat, O.; Shivalingam, S.; Gopala, K.G.; Khairuzzana, B. Migrating Foreign Body into the Common Carotid Artery and Internal Jugular Vein—A Rare Case. Auris. Nasus. Larynx 2009, 36, 380–382. [Google Scholar] [CrossRef]
- Carroll, M.I.; Ahanchi, S.S.; Kim, J.H.; Panneton, J.M. Endovascular Foreign Body Retrieval. J. Vasc. Surg. 2013, 57, 459–463. [Google Scholar] [CrossRef]
- Bedrock, R.D.; Skigen, A.; Dolwick, M.F. Retrieval of a Broken Needle in the Pterygomandibular Space. J. Am. Dent. Assoc. 1999, 130, 685–687. [Google Scholar] [CrossRef]
- Augello, M.; von Jackowski, J.; Grätz, K.W.; Jacobsen, C. Needle Breakage during Local Anesthesia in the Oral Cavity—A Retrospective of the Last 50 Years with Guidelines for Treatment and Prevention. Clin. Oral Investig. 2011, 15, 3–8. [Google Scholar] [CrossRef]
- Cameron, M.; Phillips, B. Snookered! Facial Infection Secondary to Occult Foreign Body. Int. J. Oral Maxillofac. Surg. 2006, 35, 373–375. [Google Scholar] [CrossRef]
- Thompson, M.; Wright, S.; Cheng, L.H.H.; Starr, D. Locating Broken Dental Needles. Int. J. Oral Maxillofac. Surg. 2003, 32, 642–644. [Google Scholar] [CrossRef] [PubMed]
- Moore, U.J.; Fanibunda, K.; Gross, M.J. The Use of a Metal Detector for Localisation of a Metallic Foreign Body in the Floor of the Mouth. Br. J. Oral Maxillofac. Surg. 1993, 31, 191–192. [Google Scholar] [CrossRef] [PubMed]
- Gerbino, G.; Zavattero, E.; Berrone, M.; Berrone, S. Management of Needle Breakage Using Intraoperative Navigation Following Inferior Alveolar Nerve Block. J. Oral Maxillofac. Surg. 2013, 71, 1819–1824. [Google Scholar] [CrossRef] [PubMed]
- Bagattoni, S.; D’Alessandro, G.; Marzo, G.; Piana, G. Needle Breakage during an Inferior Alveolar Nerve Block in a Child with KBG Syndrome: A Case Report. Eur. Arch. Paediatr. Dent. 2018, 19, 125–128. [Google Scholar] [CrossRef]
- Holmes, P.-J.; Miller, J.R.; Gutta, R.; Louis, P.J. Intraoperative Imaging Techniques: A Guide to Retrieval of Foreign Bodies. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2005, 100, 614–618. [Google Scholar] [CrossRef]
- Floridi, C.; Nocchi-Cardim, L.; De Chiara, M.; Ierardi, A.M.; Carrafiello, G. Intravascular Foreign Bodies: What the Radiologist Needs to Know. Semin. Ultrasound. CT MR 2015, 36, 73–79. [Google Scholar] [CrossRef]
- Chittenden, H.B.; Chandra, A.; Sandy, C.J. Use of an Electromagnet to Retrieve a Broken Fascia Needle during Frontalis Sling Surgery. Ophthal. Plast. Reconstr. Surg. 2005, 21, 469–470. [Google Scholar] [CrossRef]
- Marks, R.B.; Carlton, D.M.; McDonald, S. Management of a Broken Needle in the Pterygomandibular Space: Report of Case. J. Am. Dent. Assoc. 1984, 109, 263–264. [Google Scholar] [CrossRef]
- Schorn, L.; Sproll, C.; Depprich, R.; Kübler, N.R.; Rana, M.; Singh, D.D.; Lommen, J. Navigated Recovery of Fractured Dental Injection Needles: Case Report and Suggestions for Management during Pandemic Crises. Case Rep. Dent. 2021, 2021, 8820381. [Google Scholar] [CrossRef]
- Sandre, L.B.; de Paula e Silva, E.; Izidro, A.E.R.; Neto, W.M.P.; da Costa Moraes, C.A.; da Rosa, E.L.S. Observational and Descriptive Analysis of Broken Dental Needles: A Case Series. Oral Maxillofac. Surg. 2022, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Armfield, J.M.; Heaton, L.J. Management of Fear and Anxiety in the Dental Clinic: A Review. Aust. Dent. J. 2013, 58, 390–407; quiz 531. [Google Scholar] [CrossRef] [PubMed]
- Pietruszka, J.F.; Hoffman, D.; McGivern, B.E. A Broken Dental Needle and Its Surgical Removal: A Case Report. N. Y. State Dent. J. 1986, 52, 28–31. [Google Scholar] [PubMed]
- Fuller, N.P.; Menke, R.A.; Meyers, W.J. Perception of Pain to Three Different Intraoral Penetrations of Needles. J. Am. Dent. Assoc. 1979, 99, 822–824. [Google Scholar] [CrossRef] [PubMed]
- Dojcinovic, I.; Hugentobler, M.; Richter, M. Needle breakage: A rare and potentially dangerous complication during local anaesthesia. Rev. Stomatol. Chir. Maxillofac. 2007, 108, 222–224. [Google Scholar] [CrossRef]
- Ng, S.Y.; Songra, A.K.; Bradley, P.F. A New Approach Using Intraoperative Ultrasound Imaging for the Localization and Removal of Multiple Foreign Bodies in the Neck. Int. J. Oral Maxillofac. Surg. 2003, 32, 433–436. [Google Scholar] [CrossRef]
- Shah, A.; Mehta, N.; Von Arx, D.P. Fracture of a Dental Needle during Administration of an Inferior Alveolar Nerve Block. Dent. Update 2009, 36, 20–22. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).