Application of the Hyperspectral Imaging Method to Assess the Effectiveness of Permanent Makeup Removal
Abstract
1. Introduction
2. Materials and Methods
3. Results
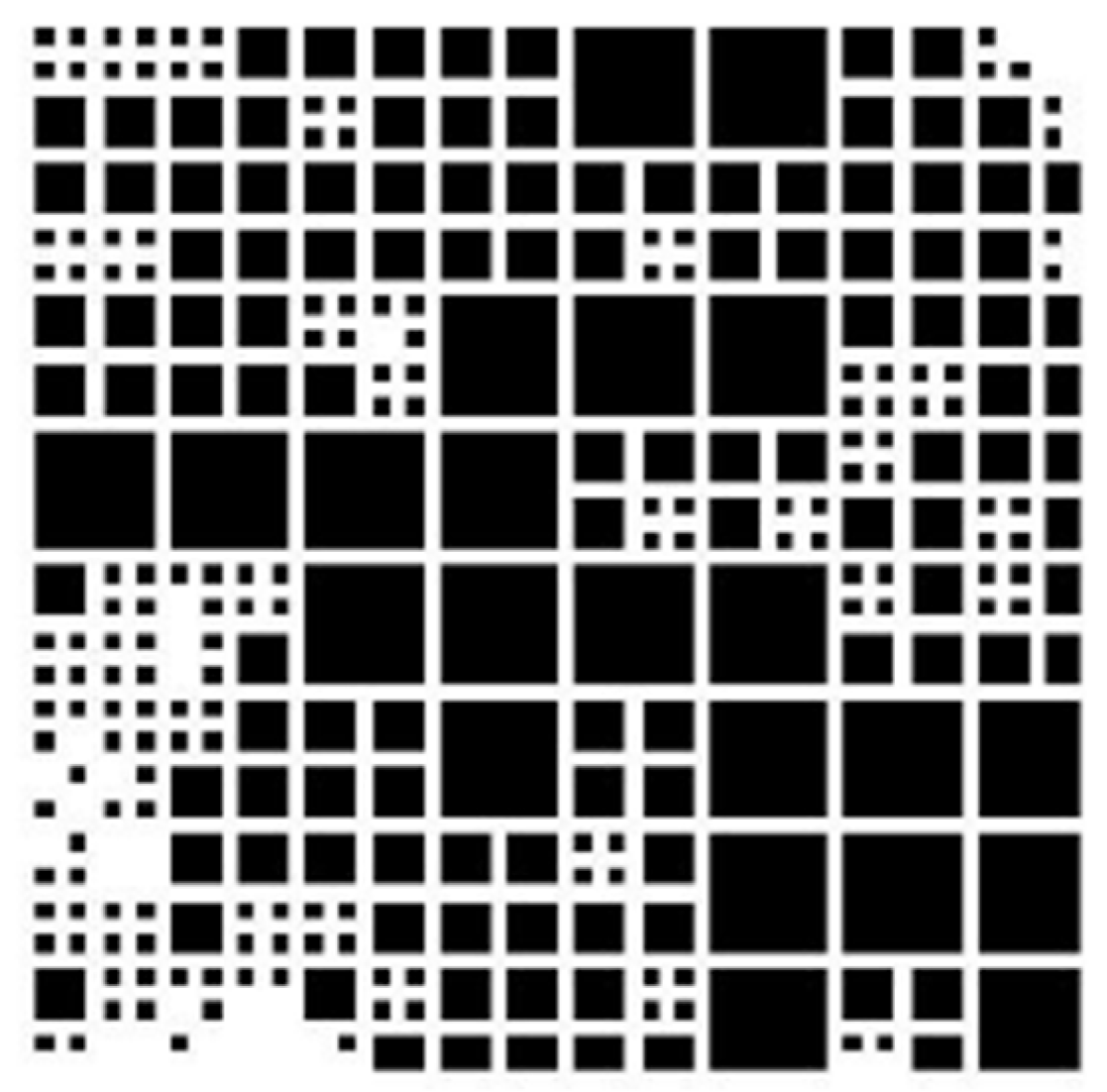
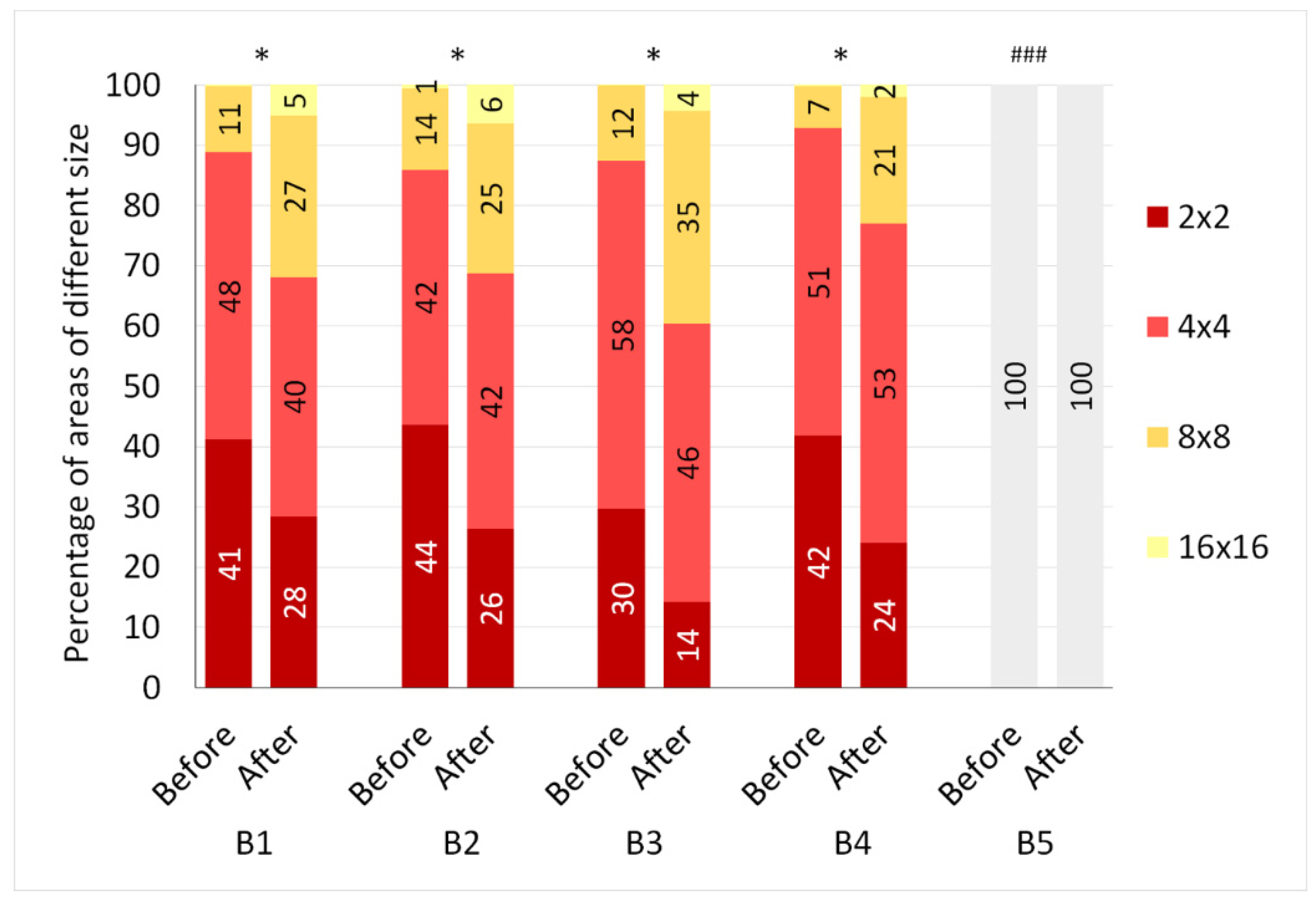
3.1. Quadratic tree Decomposition Analysis
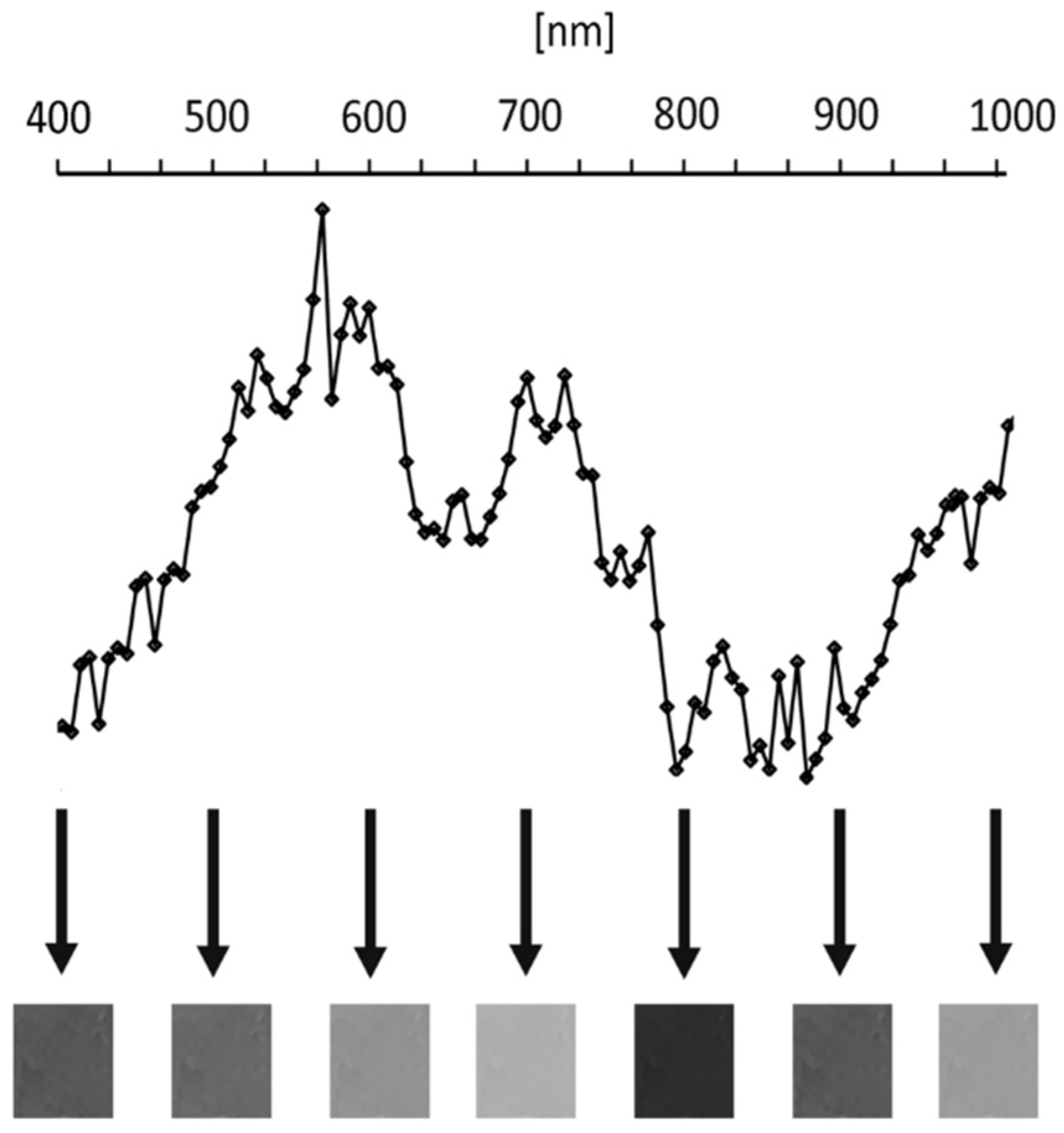
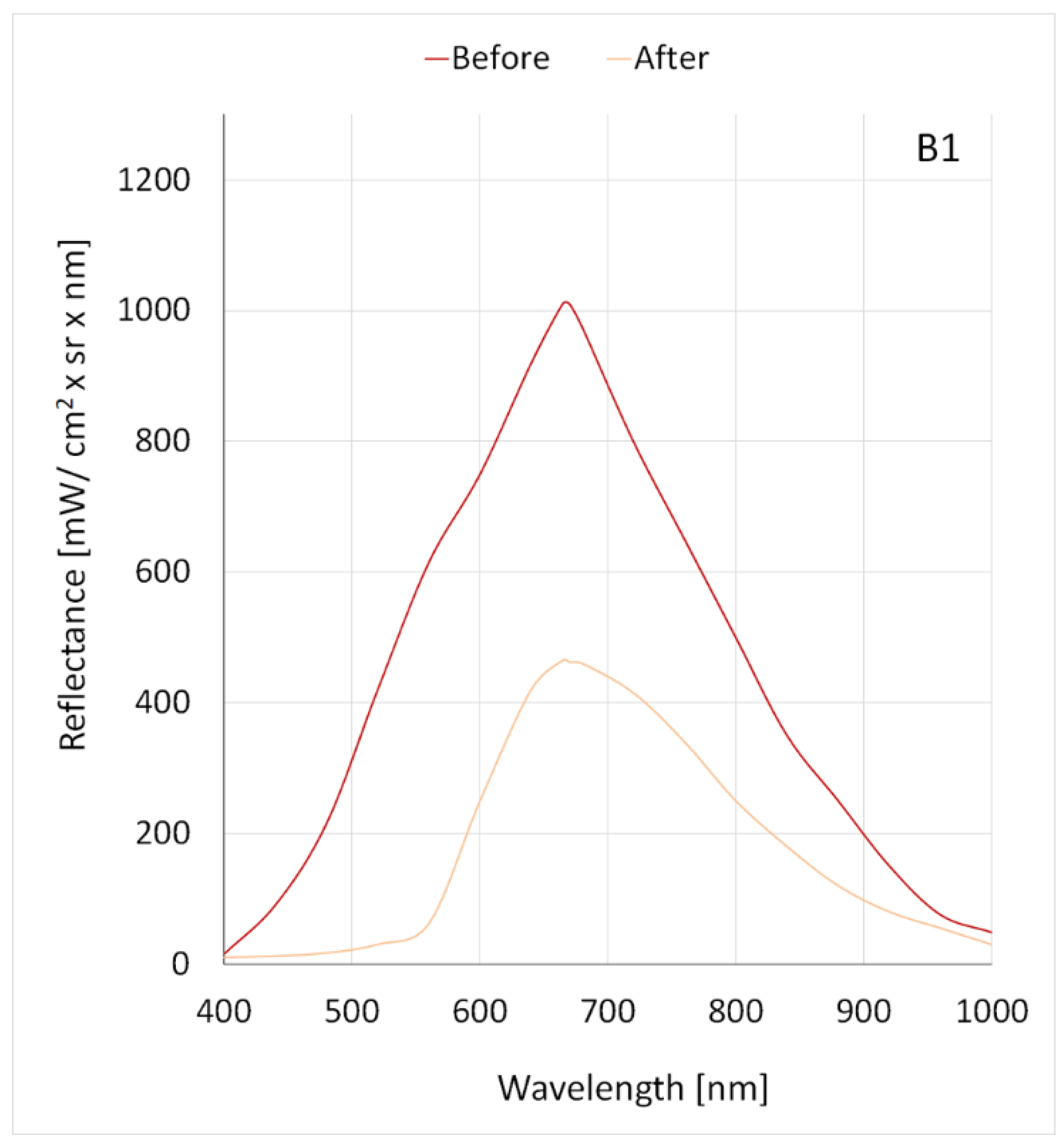
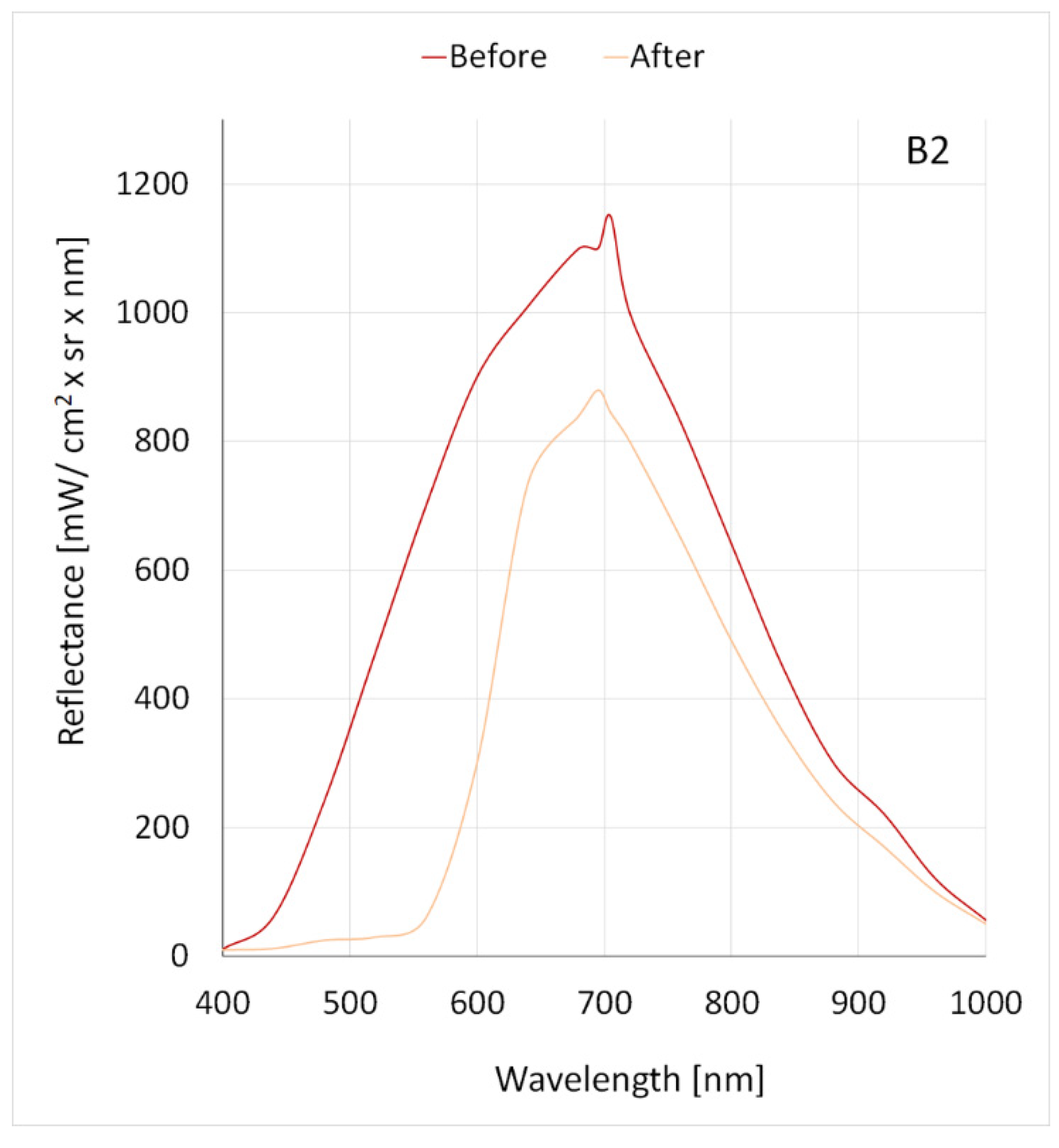
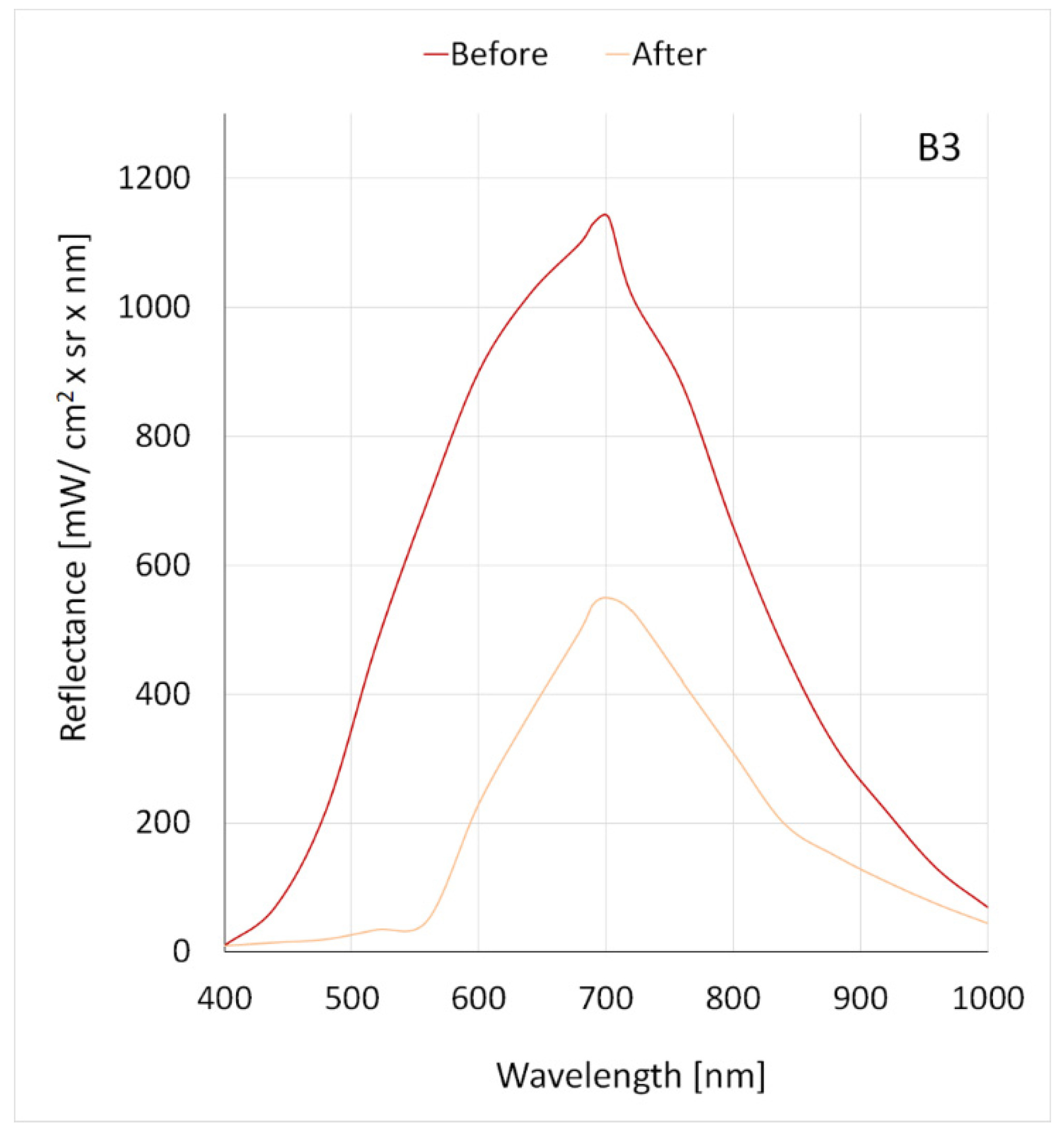
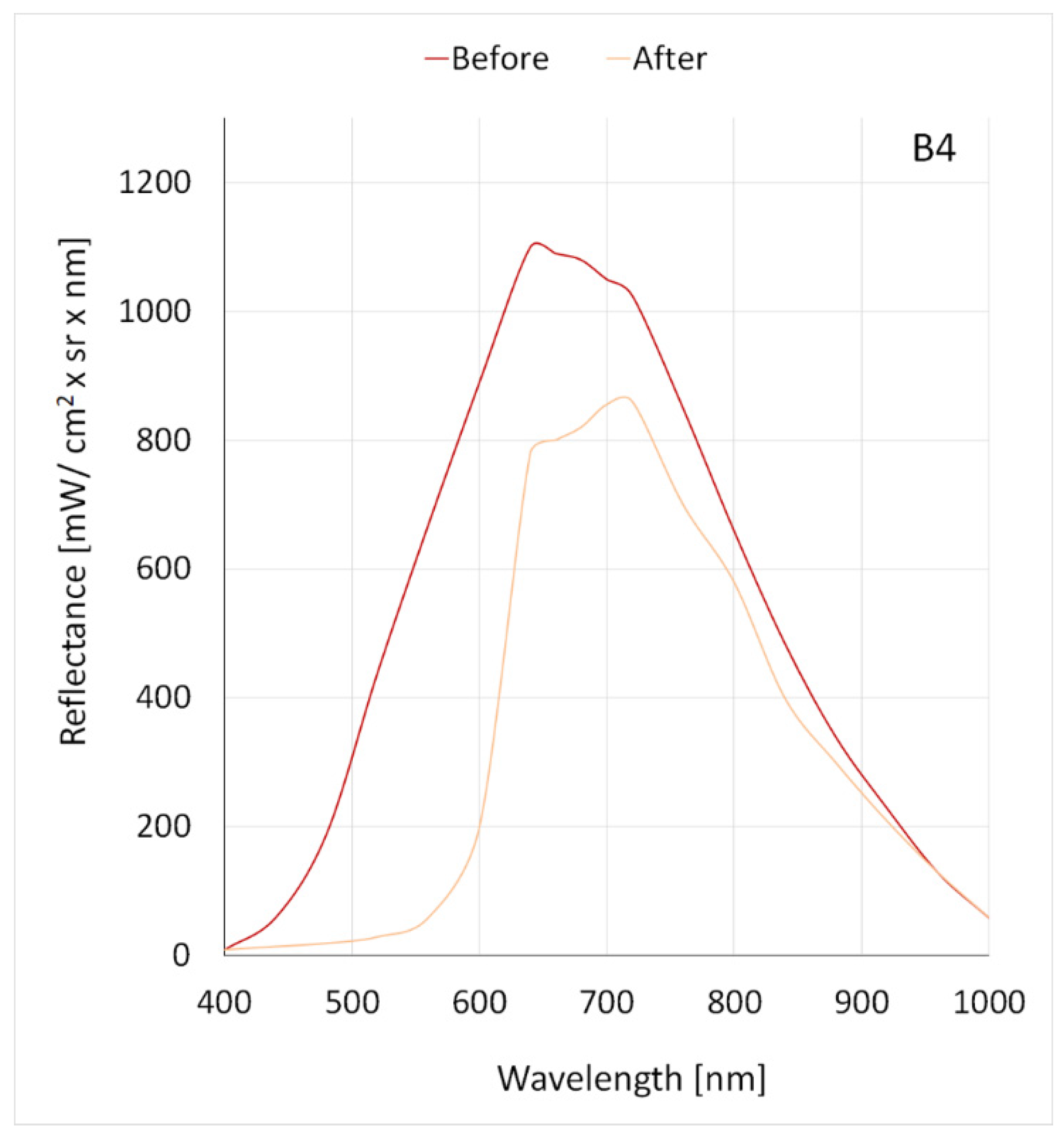
3.2. Reflectance Analysis
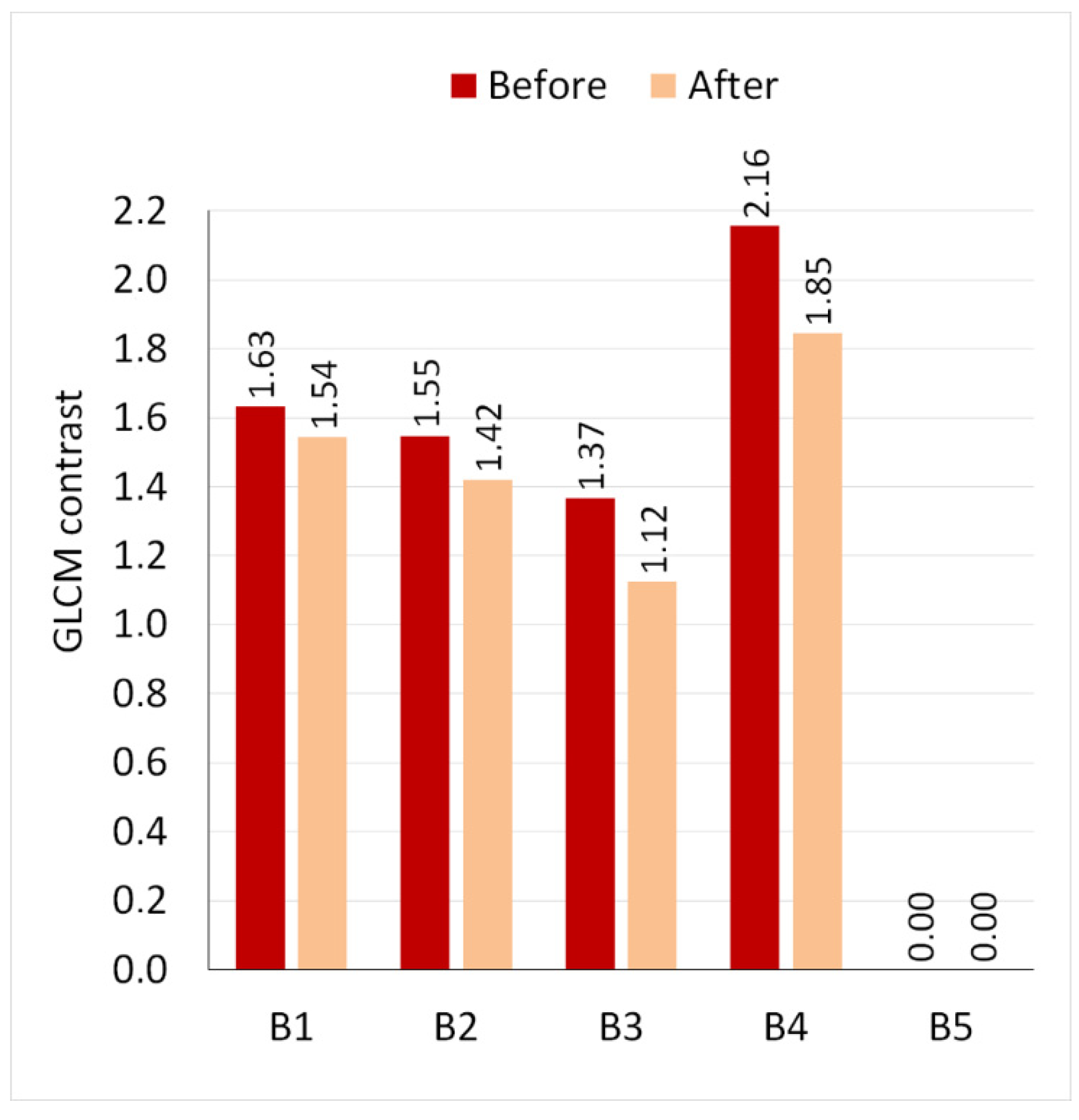
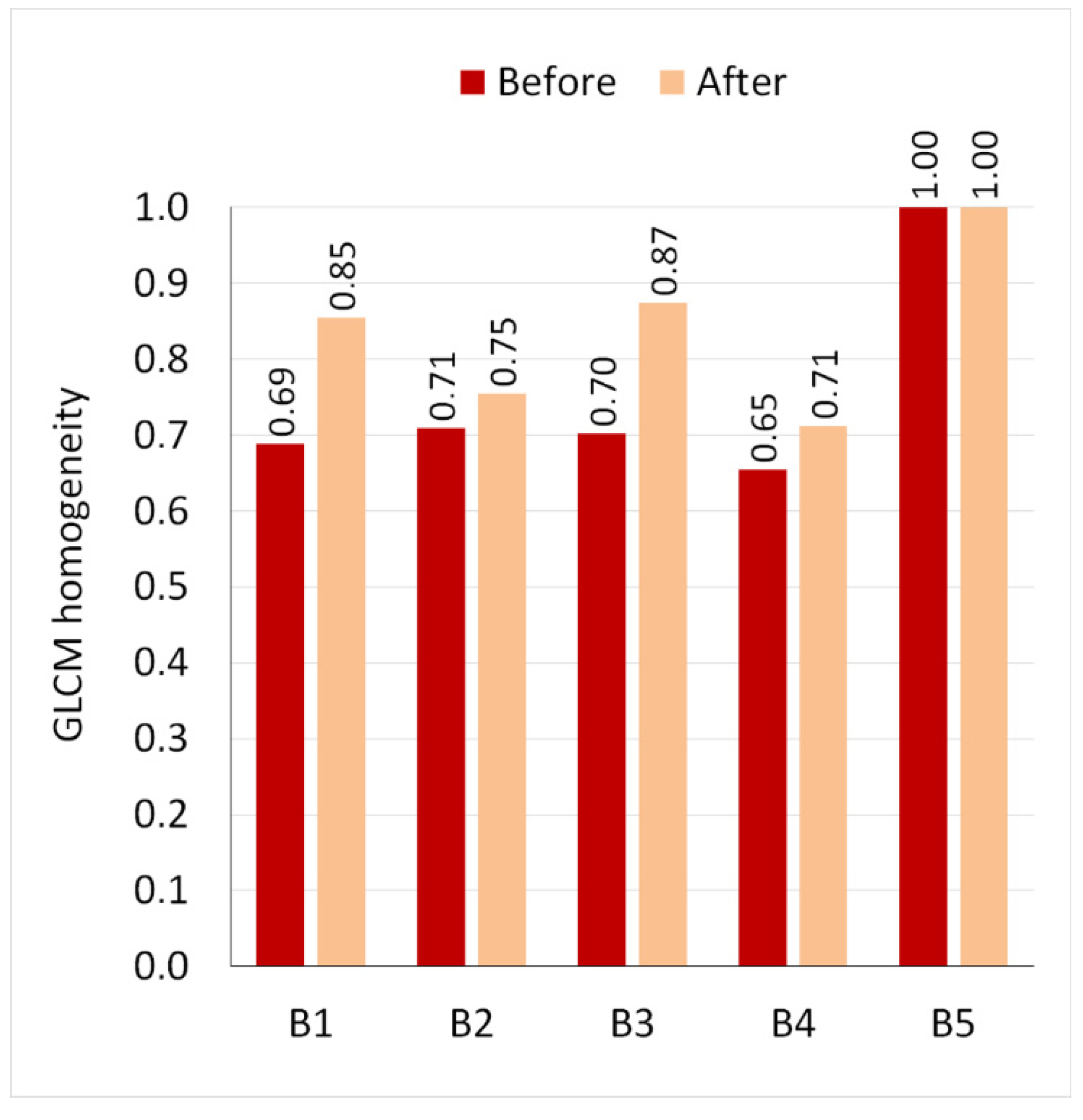
3.3. GLCM Analysis
4. Discussion
5. Conclusions
- The proposed method of hyperspectral imaging allows for a quantitative assessment of the spectral parameters of dyes implanted in pig skin and, thus, optimization of the laser parameters necessary for its removal.
- The laser application causes a decrease in reflectance for all tested dyes except for white. White pigment is the most difficult to remove due to its high reflectivity.
- For all dyes, except for white, a decrease in GLCM contrast and an increase in homogeneity were recorded, which indicates that after laser treatment, dyes are distributed more homogeneously in the skin.
- The increase in the homogeneity of the distribution of dyes after the laser treatment is also confirmed by the quadratic tree decomposition parameters.
- For two tested dyes, a change in the maximum reflectance of radiation in the range of 400–1000 nm was recorded after the laser procedure, which may indicate that the laser treatment may cause a change in the color of the dye.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Naga, L.I.; Alster, T.S. Laser tattoo removal: An Update. Am. J. Clin. Derm. 2017, 18, 59–65. [Google Scholar] [CrossRef] [PubMed]
- De Cuyper, C. Complications of cosmetic tattoos. Curr. Probl. Derm. 2015, 48, 61–70. [Google Scholar]
- Wąsik, A. Microblading. Pomóc naturze. Kosmetol. Estet. 2017, 6, 269–270. [Google Scholar]
- Kumańska, K. Naturalność jest trendy. Kosmetol. Estet. 2019, 8, 693–695. [Google Scholar]
- Kornhaber, R.; Visentin, D.; Thapa, D.K.; West, S.; McKittrick, A.; Haik, J.; Cleary, M. Cosmetic camouflage improves quality of life among patients with skin disfigurement: A systematic review. Body Image 2018, 27, 98–108. [Google Scholar] [CrossRef]
- Sandhu, J.K.; Sharma, P. Skin camouflage therapy. Indian J. Dermatol. Venereol. Leprol. 2022, 88, 718. [Google Scholar] [CrossRef]
- Matuła, A.; Załęska, I.; Lizak, A.; Morawiec, M.; Drąg, J.; Wasylewski, M. The role of cosmetologist in diagnostics and cancer therapy. Kosmetol. Estet. 2018, 7, 445. [Google Scholar]
- Saed, S.; Ibrahim, O.; Bergfeld, W.F. Hair camouflage: A comprehensive review. Int. J. Womens Derm. 2016, 2, 122–127. [Google Scholar] [CrossRef]
- Rassman, W.R.; Pak, J.P.; Kim, J.; Estrin, N.F. Scalp micropigmentation: A concealer for hair and scalp deformities. J. Clin. Aesthet. Derm. 2015, 8, 35–42. [Google Scholar]
- Ju, H.J.; Eun, S.H.; Lee, H.N.; Lee, J.H.; Kim, G.M.; Bae, J.M. Micropigmentation for vitiligo on light to moderately colored skin: Updated evidence from a clinical and animal study. J. Derm. 2020, 47, 464–469. [Google Scholar] [CrossRef]
- Uhlmann, N.R.; Martins, M.M.; Piato, S. 3D areola dermopigmentation (nipple-areola complex). Breast J. 2019, 25, 1214–1221. [Google Scholar] [CrossRef] [PubMed]
- Tomita, S.; Mori, K.; Miyawaki, T. Colour change after paramedical pigmentation of the nipple-areola complex. Aesthetic Plast. Surg. 2018, 42, 656–661. [Google Scholar] [CrossRef]
- McILwee, B.E.; Alster, T.S. Treatment of Cosmetic Tattoos: A review and case analysis. Derm. Surg. 2018, 44, 1565–1570. [Google Scholar] [CrossRef]
- Ruprich, M.; Janiczek, M.; Wilczyński, A. Optimization of laser treatment to remove permanent makeup using hyperspectral imager. Kosmetol. Estet. 2016, 5, 299–301. [Google Scholar]
- Tampa, M.; Mitran, M.I.; Mitran, C.I.; Matei, C.; Amuzescu, A.; Buzatu, A.A.; Georgescu, S.R. Viral infections confined to tattoos—A narrative review. Medicina 2022, 58, 342. [Google Scholar] [CrossRef] [PubMed]
- Torbeck, R.; Bankowski, R.; Henize, S.; Saedi, N. Lasers in tattoo and pigmentation control: Role of the PicoSure® laser system. Med. Devices Evid. Res. 2016, 9, 63–67. [Google Scholar]
- Gemza, K.; Surgiel-Gemza, A. Methods of imaging the effects of laser removal of pigments deposited in the skin, including treatments performed with a picosekond laser. Aesth. Cosmetol. Med. 2020, 9, 383–388. [Google Scholar]
- Kasai, K. Picosecond Laser Treatment for Tattoos and Benign Cutaneous Pigmented Lesions (Secondary publication). Laser Ther. 2017, 26, 274–281. [Google Scholar] [CrossRef]
- Hexsel, D.; Hexsel, C.L.; Dal’Forno, T.; Schilling de Souza, J.; Silva, A.F.; Siega, C. Standardized methods for photography in procedural dermatology using simple equipment. Int. J. Derm. 2017, 56, 444–451. [Google Scholar] [CrossRef]
- Olejnik, A.; Gornowicz-Porowska, J.; Gościńska, J. Analitical methods for testing coemetic products in the past and nowadays. Wiadomości Chem. 2022, 76, 607–633. [Google Scholar]
- Pathania, Y.S.; Apalla, Z.; Salerni, G.; Patil, A.; Grabbe, S.; Goldust, M. Non-invasive diagnostic techniques in pigmentary skin disorders and skin cancer. J. Cosmet. Derm. 2022, 21, 444–450. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Lee, M.H.; Noh, T.K.; Choi, K.H.; Won, C.H.H.; Chang, S.E.; Lee, M.W.; Choi, J.W. Successful treatment of tattoos with a picosecond 735 nm alexandrite laser in Asian skin. Ann. Derm. 2016, 28, 673–675. [Google Scholar] [CrossRef] [PubMed]
- Stolecka-Warzecha, A.; Chmielewski, Ł.; Wilczyński, S.; Koprowski, R. In vitro hyperspectral analysis of tattoo dyes. Skin Res. Technol. 2023, 29, e13268. [Google Scholar] [CrossRef]
- Wilczyński, S.; Koprowski, R.; Marmion, M.; Duda, P.; Błońska-Fajfrowska, B. The use of hyperspectral imaging in the VNIR (400–1000 nm) and SWIR range (1000–2500 nm) for detecting counterfeit drugs with identical API composition. Talanta 2016, 160, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Koprowski, R.; Wilczyński, S.; Wróbel, Z.; Błońska-Fajfrowska, B. Calibration and segmentation of skin areas in hyperspectral imaging for the needs of dermatology. Biomed. Eng. Online 2014, 13, 113. [Google Scholar] [CrossRef] [PubMed]
- Behmann, J.; Acebron, K.; Emin, D.; Bennertz, S.; Matsubara, S.; Thomas, S.; Bohnenkamp, D.; Kuska, M.T.; Jussila, J.; Salo, H.; et al. Specim IQ: Eval uation of a new, miniaturized handheld hyperspectral camera and its application for plant phenotyping and disease detection. Sensors 2018, 18, 441. [Google Scholar] [CrossRef]
- De la Casa Almeida, M.; Serrano, C.S.; Rejano, J.J. Reliability of texture analysis using co-occurence matrices (glcm) on photographic image in the assessment of cellulite in a Spanish population. J. Eur. Acad. Derm. Venereol. 2015, 29, 315–324. [Google Scholar] [CrossRef]
- Odrzywołek, W.; Deda, A.; Zdrada, J.; Wilczyński, S.; Błońska-Fajfrowska, B.; Lipka-Trawińska, A. Quantitative evaluation of the effectiveness of chemical peelings in reducing acne lesions based on grey-level co-occurrence matrix (GLCM). Clin. Cosmet. Investig. Derm. 2022, 15, 1873–1882. [Google Scholar] [CrossRef]
- Maktabdar Oghaz, M.; Maarof, M.A.; Rohani, M.F.; Zainal, A.; Shaid, S.Z.M. An optimized skin texture model using gray-level co-occurrence matrix. Neural. Comput. Appl. 2019, 31, 1835–1853. [Google Scholar] [CrossRef]
- Dhruv, B.; Mittal, N.; Modi, M. Study of Haralick’s and GLCM texture analysis on 3D medical images. Int. J. Neurosci. 2019, 129, 350–362. [Google Scholar] [CrossRef]
- Lu, G.; Fei, B. Medical hyperspectral imaging: A review. J. Biomed. Opt. 2014, 19, 10901. [Google Scholar] [CrossRef] [PubMed]
- Głowacz, A.; Głowacz, A.; Głowacz, Z. Recognition of monochrome thermal images of synchronous motor with the application of quadtree decomposition and backpropagation neural network. Eksploat. I Niezawodn. Maint. Reliab. 2014, 16, 92–96. [Google Scholar]
- Bożek, A.; Reich, A. Assessment of the severity of atopic dermatitis. Przegl. Derm. 2016, 103, 479–485. [Google Scholar] [CrossRef]
- Meng, X.; Xu, C. Progress and prospect of non-invasive detection techniques i the therapeutic evaluation of melasma. Chin. Med. J. 2020, 133, 2104–2106. [Google Scholar] [CrossRef] [PubMed]
- Holmer, A.; Tetschke, F.; Marotz, J.; Malberg, H.; Markgraf, W.; Thiele, C.; Kulcke, A. Oxygenation and perfusion monitoring with a hyperspectral camera system for chemical based tissue analysis of skin and organs. Physiol. Meas. 2016, 37, 2064–2078. [Google Scholar] [CrossRef]
- Nkengne, A.; Robic, J.; Seroul, P.; Gueheunneux, S.; Jomier, M.; Vie, K. SpectraCam®: A new polarized hyperspectral imaging system for repeatable and reproducible in vivo skin quantification of melanin, total hemoglobin, and oxygen saturation. Ski. Res. Technol. 2018, 24, 99–107. [Google Scholar] [CrossRef]
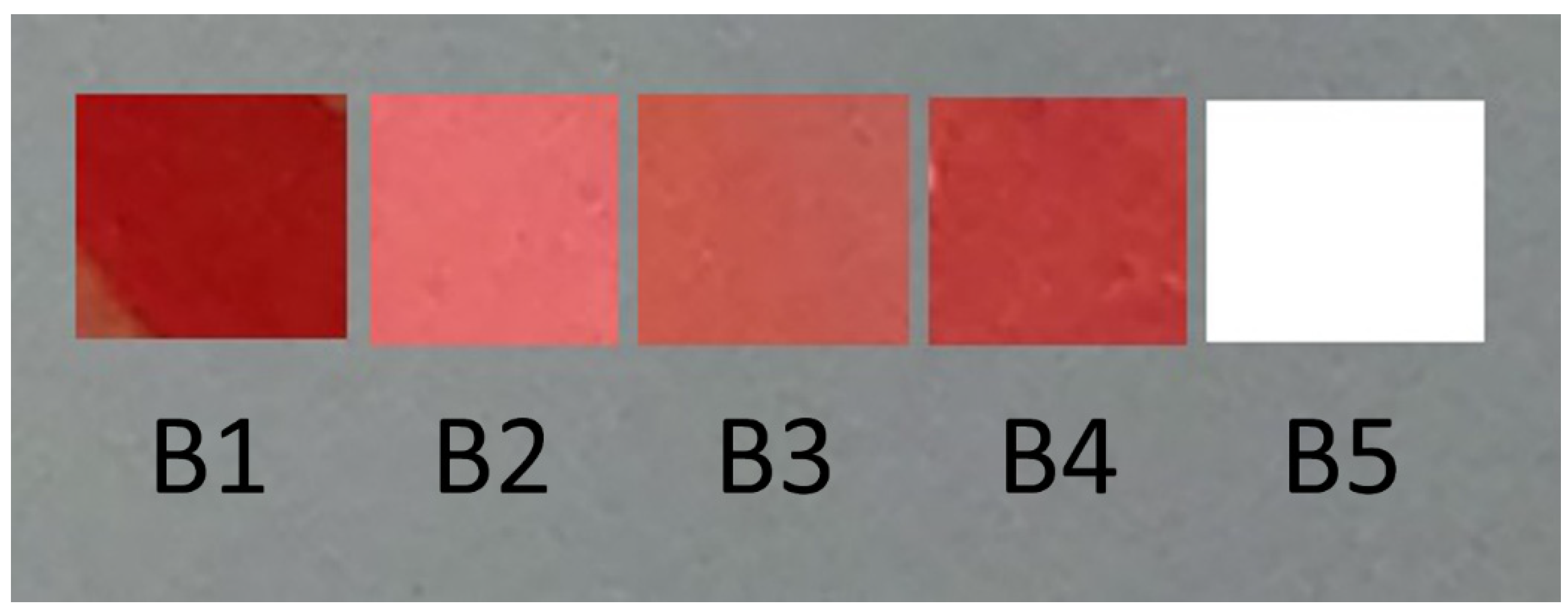


| RGB | L*a*b | CMYK | |
|---|---|---|---|
| B1 | 154; 22; 19 | 34; 52; 40 | 25; 100; 100; 23 |
| B2 | 227; 108; 110 | 61; 47; 22 | 7; 71; 49; 0 |
| B3 | 195; 87; 78 | 51; 44; 27 | 18; 78; 70; 25 |
| B4 | 43; 57; 54 | 43; 51; 52 | 21; 91; 84; 10 |
| B5 | 255; 255; 255 | 100; 0; 0 | 0; 0; 0; 0 |
| B1 | B2 | B3 | B4 | B5 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Before | After | Before | After | Before | After | Before | After | Before | After | |
| Maximum reflectance [mW/cm2 × sr × nm] | 1012 | 465 | 1150 | 880 | 1140 | 550 | 1100 | 860 | 1240 | 1200 |
| Decrease in maximum reflectance [%] | 54.1 | 23.5 | 51.8 | 21.8 | 3.2 | |||||
| Wavelength at maximum reflectance [nm] | 665 | 665 | 705 | 695 | 702 | 702 | 640 | 730 | 665 | 665 |
| Wavelength change at maximum reflectance | No | Yes | No | Yes | No | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kamińska, M.; Krusiec-Świdergoł, B.; Pawełczyk, W.; Hartman-Petrycka, M.; Banyś, A.; Jonderko, K.; Lebiedowska, A.; Koprowski, R.; Wilczyński, S. Application of the Hyperspectral Imaging Method to Assess the Effectiveness of Permanent Makeup Removal. Appl. Sci. 2023, 13, 2330. https://doi.org/10.3390/app13042330
Kamińska M, Krusiec-Świdergoł B, Pawełczyk W, Hartman-Petrycka M, Banyś A, Jonderko K, Lebiedowska A, Koprowski R, Wilczyński S. Application of the Hyperspectral Imaging Method to Assess the Effectiveness of Permanent Makeup Removal. Applied Sciences. 2023; 13(4):2330. https://doi.org/10.3390/app13042330
Chicago/Turabian StyleKamińska, Magdalena, Beata Krusiec-Świdergoł, Weronika Pawełczyk, Magdalena Hartman-Petrycka, Anna Banyś, Krzysztof Jonderko, Agata Lebiedowska, Robert Koprowski, and Sławomir Wilczyński. 2023. "Application of the Hyperspectral Imaging Method to Assess the Effectiveness of Permanent Makeup Removal" Applied Sciences 13, no. 4: 2330. https://doi.org/10.3390/app13042330
APA StyleKamińska, M., Krusiec-Świdergoł, B., Pawełczyk, W., Hartman-Petrycka, M., Banyś, A., Jonderko, K., Lebiedowska, A., Koprowski, R., & Wilczyński, S. (2023). Application of the Hyperspectral Imaging Method to Assess the Effectiveness of Permanent Makeup Removal. Applied Sciences, 13(4), 2330. https://doi.org/10.3390/app13042330







