Abstract
The growing popularity of permanent makeup is associated with an increase in the need for treatments that effectively remove pigments from the skin. The risk of the radiation wavelength not being adjusted to the spectral ranges of individual pigments that compose the final color appears because complex dye compositions are used for permanent makeup. Incorrectly selected laser parameters may reduce the effectiveness of the treatment and increase the risk of thermal damage, leading to scarring and discoloration. The aim of the study was to evaluate the effectiveness of laser permanent makeup removal using hyperspectral imaging. Five different dyes were implemented into the skin of the pig’s ear. Then the dyes were removed using a Q-switched Nd:YAG laser. During the study, skin measurements were performed with a hyperspectral camera before and after laser application. The results were analyzed using GLCM, reflectance, and quadratic tree decomposition. Based on the obtained results, it was found that the most difficult dye to remove is white because it is characterized by high reflectivity of electromagnetic radiation. After the dye removal, there was a decrease in reflectance and contrast of GLCM and an increase in homogeneity for all dyes except for white. After the laser application, the pigments were distributed more equally in the skin.
1. Introduction
Permanent makeup correction, commonly called permanent makeup or micropigmentation, can be a cosmetic or medical tattoo type [1,2]. The treatment is invasive and based on the application of pigment particles under the epidermis. Permanent makeup makes it possible to correct facial asymmetry, and it is applied to change the shape, color, or size of the lips and eyebrows, as well as to optically improve the shape of the eye [2,3,4]. However, beautification is not the only purpose of permanent makeup. It is performed to cover scars in patients after injuries, surgeries, or radiotherapy [3,5,6,7]. Micropigmentation is also used in dermatological diseases such as vitiligo or alopecia areata to cover lesions [2,8,9,10]. It also allows to hide nipple reconstruction after mastectomy [11,12].
The growing popularity of permanent makeup is associated with an increase in the need for treatments that effectively remove pigments from the skin in cases of complications (allergies, infections, exacerbation of coexisting dermatoses) or dissatisfaction with the final effect [2,13,14,15]. Permanent makeup removal is difficult due to the unknown pigment composition used to achieve the intended visual effect. A commonly used method of pigment removal is based on a universal Q-switched nanosecond laser: neodymium yttrium-aluminum-garnet (Nd:YAG), which enables effective, targeted removal of dyes often used in makeup [16,17]. The laser generates radiation characterized by a very short pulse (nanoseconds) and high power. Radiation is absorbed by the appropriate pigment (chromophore), depending on the wavelength of laser radiation. It leads to the disintegration of its molecule. The laser permanent makeup removal treatment is based on thermal, photochemical, and photoacoustic phenomena. Then, the lymphatic system removes the small particles of the dye formed as a result of degradation [14,17,18].
The risk of the radiation wavelength not being adjusted to the spectral ranges of individual pigments that compose the final color appears because complex dye compositions are used for permanent makeup, which can give the same color impression during the laser removal procedure. Incorrectly selected laser parameters may reduce the effectiveness of the treatment and increase the risk of thermal damage, leading to scarring and discoloration [14,17]
Digital photographic imaging, which is the most popular method of comparing the results before and after the procedure, can be used to assess the effectiveness of pigment removal from the skin. However, a quantitative comparison is possible only with properly selected camera parameters and under optimal conditions. If the images have different parameters or are taken in a different location, misinterpretation may occur. The main advantage of such a skin imaging method is the low price [19].
Another non-invasive method helpful in assessing the effectiveness of removing skin pigments is colorimetry, which allows the measurement of skin color. The measured skin color is expressed as an xyz value (tristimulus method) and can be converted into a value from the L*a*b color space, which is the most popular way to describe colors [20].
High-frequency ultrasonography (HFU), which is gaining increasing popularity, is an objective method of imaging normal and pathologically changed skin. High-frequency ultrasound scanners equipped with transducers operating in the range of 20–100 MHz enable accurate imaging of the epidermis, dermis, and subcutaneous tissue. Nevertheless, its use in assessing the effectiveness of dye removal is limited due to insufficient USG resolution (the dye particles are too small to be clearly visible in USG) [18]. Another type of imaging skin under the influence of laser light is the presentation of images from a light or electron microscope. However, this method is associated with pain, increased risk of infection and scarring, and significant costs. In addition, it allows the assessment of only a small fragment of the skin, and during the sample preparation, some dye may be displaced [21,22].
However, it should be emphasized that the effectiveness of removing pigments implemented into the skin is often an individual matter because obtaining a satisfactory final effect depends not only on the composition of the pigments, location, and depth but also on the age, skin phototype, general health, medications, and supplements, health history as well as immunity level. Therefore, it is necessary to be able to adjust the laser operating parameters to individual skin characteristics [17]. So, the hyperspectral analysis proposed in this study is free of the disadvantages of other methods.
Hyperspectral imaging (HSI—hyperspectral imaging) as the method of optimizing permanent makeup laser removal may be helpful in improving efficiency and reducing the risk of side effects [14,17].
Hyperspectral imaging is a method that combines two non-invasive techniques: imaging and spectroscopy. As a result, it is possible to determine both the optical (image) and spectral (reflectance/absorption profile) properties of the analyzed objects in relation to each pixel of the image [23].
The hyperspectral camera acquires the image by registering radiation with a specific energy intensity (I) in a specific range of spatial coordinates (x,y) and wavelength (λ). The values of Δx and Δy determine the spatial resolution of the image, while the value of Δλ determines the spectral resolution [24].
As a result, a series of images of the same object is obtained—in this case, pig skin with dyes implanted in it—each recorded at a different wavelength. A complex analysis of the optical spectra of the tested object is possible, as well as the analysis of the entire object using the methods of image analysis and processing in a wide spectral range resulting from the spectral range of the camera.
Molecular hyperspectral imaging, on the other hand, is a technique where each pixel that contains a complete spectral signature in the entire spectral range is additionally analyzed. It is possible to obtain not only a spatial image of the skin with pigments (up to the depth of photon penetration in the spectral range of 400–1000 nm) but also spectral information, which is extremely useful in the quantitative assessment of the content and distribution of pigments [14,25,26].
The aim of the study was to verify the hypothesis about the functionality of a hyperspectral camera to assess the effectiveness of dye removal in permanent makeup.
2. Materials and Methods
The dyes used in permanent makeup were implemented on the skin of the pig’s ear, which is structurally the most similar to human skin. 5 different colors were implemented into the examined skin fragment using a micropigmentation device (Conture-Linner-Duo; Long-Time-Liner, Germany). For lip pigmentation: red shade (B1), light pink shade (B2), nude (B3), and dirty pink shade (B4) were used. The control dye was white (B5) (Figure 1). The characteristics based on RGB, CMYK, and L*a*b* color scales of the dyes used before the laser procedure is shown in Table 1.
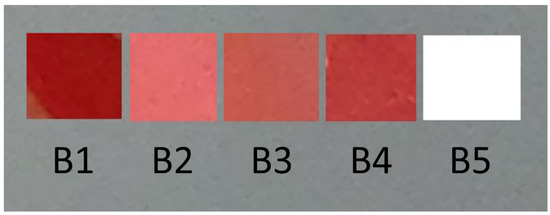
Figure 1.
Dye shades used in the study.

Table 1.
Characteristics of the used dyes (before the laser procedure).
The spectral parameters of the pigments presented on pig skin were studied by hyperspectral imaging using a SPECIM IQ hyperspectral camera (Specim Ltd., Oulu, Finland), characterized by the following technical parameters—spectral resolution: 7 nm; spatial resolution: 512 × 512 pixels; spectral range: 400–1000 nm; dynamic range: 12 bits; number of spectral channels: 86; camera field of view: 31 × 31 degrees. The spectral range of the camera, for which the optical parameters of dyes were identified, coincides with the wavelength range of lasers used in permanent makeup laser removal [23].
Two measurements on the skin were performed using a hyperspectral camera. The first one was performed after pigmentation of the skin with dyes, and the second after using a Q-switched Nd:YAG laser with a wavelength range of 532 nm and 1064 nm. The laser energy was 20 J/cm2. Lighting with a flat spectral characteristic in the camera operating range, i.e., 400–1000 nm, was used to illuminate the tested samples. An exemplary hyperspectral imaging diagram is shown in Figure 2.
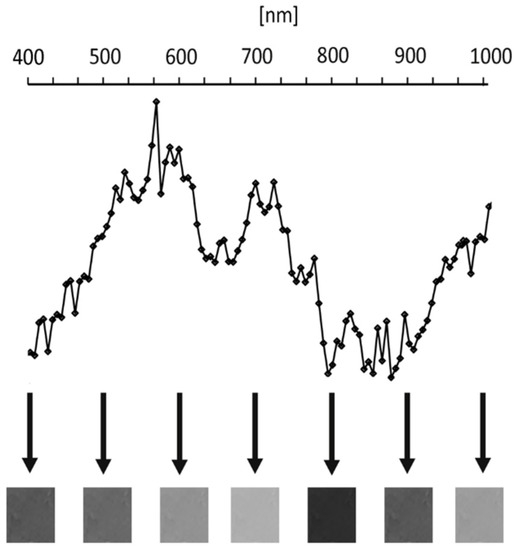
Figure 2.
Schematic diagram of the hyperspectral imaging system.
The analysis of the obtained spectral images was carried out using the Matlab software version 7.11.0.854 (R2010b), which enabled the analysis of GLCM and reflectance as well as the analysis of the homogeneity of the dyes’ distribution. Then, based on the comparison of the results obtained before and after the procedure, the effectiveness of the method was assessed.
The GLCM (Gray level co-occurrence matrix) analysis, a method of quantitative analysis of the skin texture, was also used to analyze the dyes images. The method determines the spatial relation between examined pixel and its adjacent pixels. It provides information about the frequency of occurrence of certain pixels characterized by the same brightness at a certain distance from each other. The parameters describing the GLCM matrix include the distance and angle between the evaluated pairs of pixels. The GLCM analysis was carried out after normalizing the image using Adobe Photoshop Lightroom Classic 2018 8.1 software. The purpose of the normalization was to extend the gray levels from 0 to 255, where 0 means white and 255 means black [24,25,26]. The hyperspectral camera with gray panel is shown in Figure 3, and it allows the measurement of absolute reflectance.

Figure 3.
The hyperspectral camera with a gray panel.
Contrast and homogeneity were used for the analysis in order to obtain two-dimensional images using 14 textural features isolated by Haralicka. Contrast is calculated based on the difference between the highest and lowest values in the color and brightness of the test points. Homogeneous images have contrast values close to or equal to 0. Homogeneity, on the other hand, represents the similarity between specific areas of the images, with values in the range of 0–1. Homogeneity values close to 1 indicate smaller differences between the analyzed set of pixels. It shows that there is an inversely proportional relationship between contrast and homogeneity, i.e., with increasing contrast, a decrease in homogeneity is observed [24,25,26,27,28,29,30].
Another parameter analyzed in the obtained images was reflectance. It determines the power of reflected radiation over the incident radiation at a certain point. High reflectance coefficient values indicate a high amount of reflected radiation, and lower values indicate that the radiation is absorbed. The reflectance was measured according to an external standard, a hyperspectral calibration coupon [25,31].
The quadratic tree decomposition was used to analyze the homogeneity of the dye distribution. This algorithm, also known as QTDECOMP, divides an image of certain dimensions by a power of 2, e.g., 256 × 256. This is a method where a square image is divided into 4 equal-sized square blocks. Then each block is tested to see if it meets the arbitrary criterion of the brightness difference between the blocks. If the criterion is met, the block is not divided any further. If the criterion is not met, the block is subdivided again into 4 blocks. This process is repeated until each block meets the criterion. The final effect of the quadratic tree decomposition can be blocks of different sizes (Figure 4). In this study, the arbitrarily adopted threshold for the difference in brightness was 8 [32].
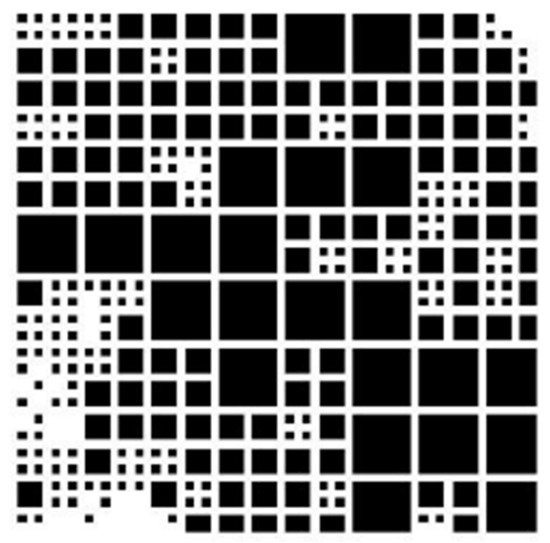
Figure 4.
An example of a quadratic tree decomposition image.
In the statistical analysis of the obtained results, the STATISTICA 13 software was used. The differences in the percentage of homogeneous areas of various sizes based on the quadratic tree decomposition before and after the laser application was carried out using the Chi2 test. The results were considered significant at p < 0.05.
3. Results
3.1. Quadratic tree Decomposition Analysis
Each of the dyes was analyzed by the quadratic tree decomposition algorithm before and after the Q-switched Nd:YAG laser application. All images were divided into 2 × 2, 4 × 4, 8 × 8, and 16 × 16 areas, and their number was calculated. Then, the percentage of areas of a certain size from the total number of areas in the image of each dye was calculated. It was shown that after using the laser, the percentage of large areas (8 × 8 and 16 × 16) increased significantly (p < 0.001) compared to smaller ones (2 × 2 and 4 × 4) in each of the colored dyes (B1–B4) (Figure 5). The B5 white dye was fully homogeneous for the arbitrarily adopted homogeneity criterion, and the use of the laser did not significantly affect its homogeneity.
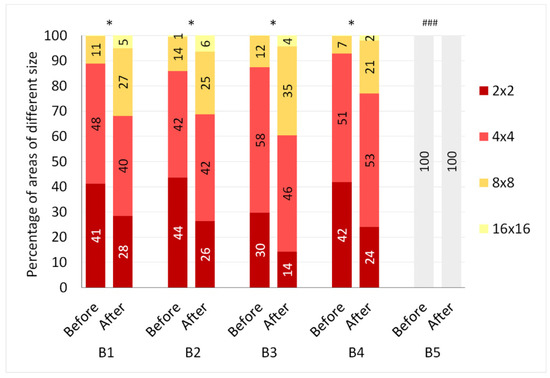
Figure 5.
Percentage of homogeneous areas of different sizes in images of B1–B5 dyes before and after the Q-Switched Nd:YAG laser application; * p < 0.001 (Chi2); ### a fully homogeneous area for an arbitrary homogeneity criterion.
3.2. Reflectance Analysis
The reflectance was tested before and after the Q-switched Nd:YAG laser application. The greatest decrease in reflectance coefficient is observed for the B1 color—red (Figure 6, Table 2). Before the laser application, the maximum reflectance was 1012 mW/cm2 × sr × nm, and after dye removal was 465 mW/cm2 × sr × nm—at a wavelength of 665 nm. In the B2 dye, a smaller decrease in reflectance was found than in the B1 dye. The maximum reflectance changed from 1150 mW/cm2 × sr × nm to 880 mW/cm2 × sr × nm (Figure 7, Table 2).
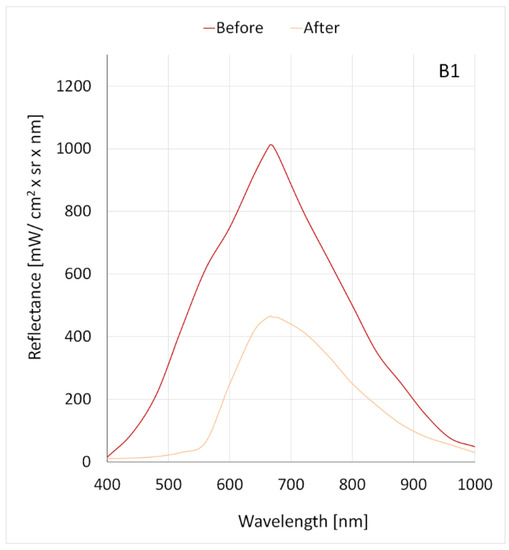
Figure 6.
The correlation between the reflectance and the wavelength for the B1 dye before and after the Q-Switched Nd:YAG laser application.

Table 2.
Characteristics of the B1-B5 dye reflectance curves before and after the laser application.
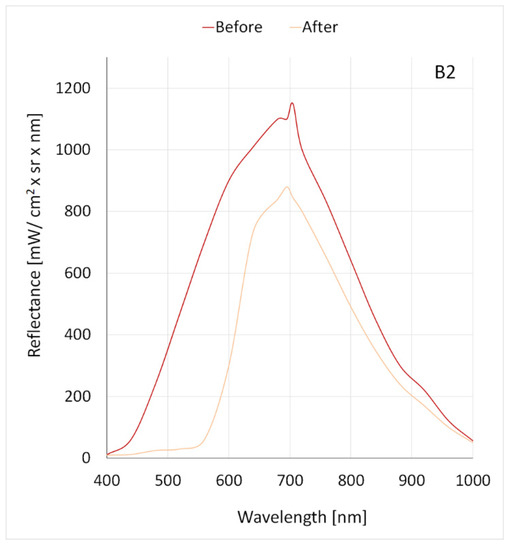
Figure 7.
The correlation between the reflectance and the wavelength for the B2 dye before and after the use of the Q-Switched Nd:YAG laser.
The second largest difference in reflectance before and after the laser application applied to dye B3, in which a decrease in maximum reflectance from 1140 mW/cm2 × sr × nm to 550 mW/cm2 × sr × nm was observed at a wavelength of 702 nm (Figure 8, Table 2). For the B4 dye, the maximum reflectance decreased from 1110 mW/cm2 × sr × nm to 860 mW/cm2 × sr × nm (Figure 9, Table 2). Dye B4, among other dyes, was characterized by the smallest difference in reflectance before and after the laser application.
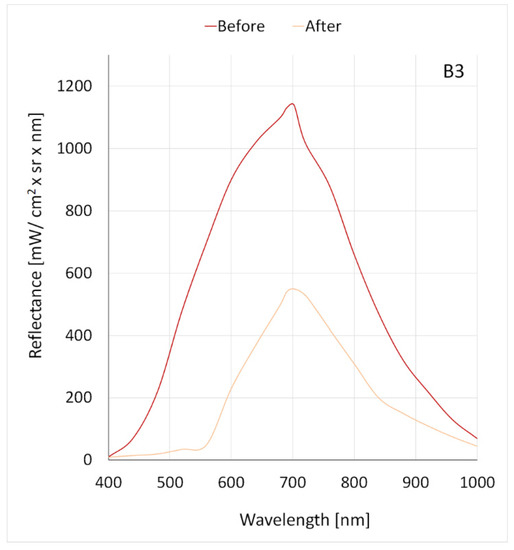
Figure 8.
The correlation between the reflectance and the wavelength for the B3 dye before and after the use of the Q-Switched Nd:YAG laser.
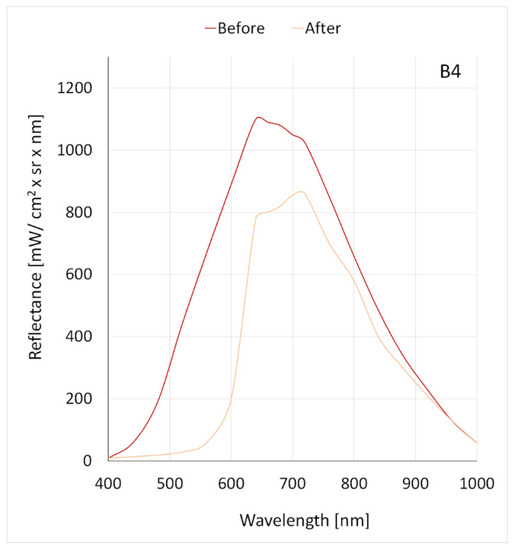
Figure 9.
The correlation between the reflectance and the wavelength for the B4 dye before and after the use of the Q-Switched Nd:YAG laser.
Regarding B5 white dye, a minimum difference in reflectance was observed; the maximum value of coefficient decreased from 1240 mW/cm2 × sr × nm to 1200 mW/cm2 × sr × nm at a wavelength of 665 nm (Figure 10, Table 2).
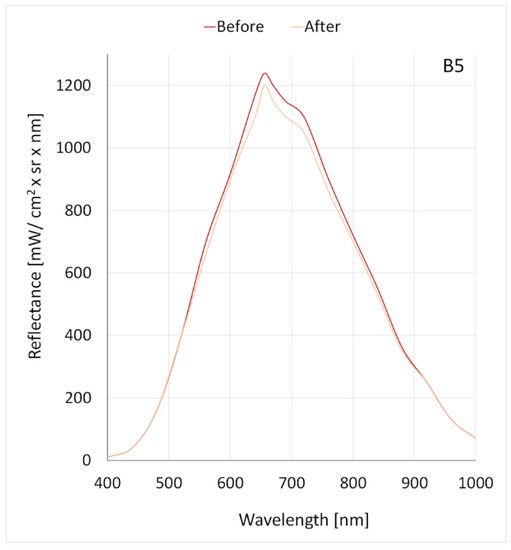
Figure 10.
The correlation between the reflectance and the wavelength for the B5 dye before and after the use of the Q-Switched Nd:YAG laser.
The maximum reflectance of all four used color dyes, B1, B2, B3, and B4, before using the laser was in the range of 1000–1200 mW/cm2 × sr × nm (Table 2). In all four dyes, after using the laser, there was a large decrease in maximum reflectance exceeding 20% (dye B2 and B4) and 50% (dye B1 and B3) of the initial value. On the other hand, in the white dye, the initial reflectance exceeded 1200 mW/cm2 × sr × nm, and after using the laser, the reduction of the maximum reflectance was small, amounting to 3.2%.
The laser application caused a change in the wavelength for maximum reflectance in the two tested dyes (B2 and B4) (Figure 7 and Figure 9, Table 2). In the B2 dye, the wavelength value was reduced from 705 nm to 695 nm for maximum reflectance, and in the B4 dye, the wavelength value was increased from 640 nm to 730 nm.
3.3. GLCM Analysis
ROIs (Region of interest) were determined for GLCM analysis, covering the central part of the dyed skin, in which the contrast and homogeneity before and after the Q-switched Nd:YAG laser application were compared. For B1–B4 dyes, a decrease in GLCM contrast was observed. For the B5 dye, the contrast before the application was 0 and did not change after the laser treatment (Figure 11).
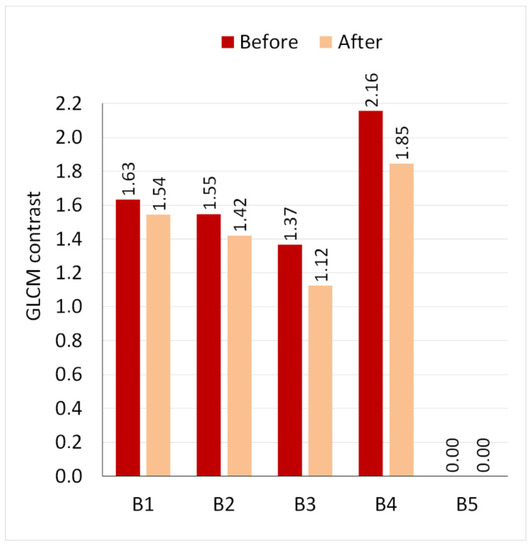
Figure 11.
Contrast in GLCM analysis before and after laser application.
Image homogeneity for B1, B2, B3, and B4 dyes increased after laser application. The white B5 dye did not change its color; therefore, its homogeneity also did not change (Figure 12).
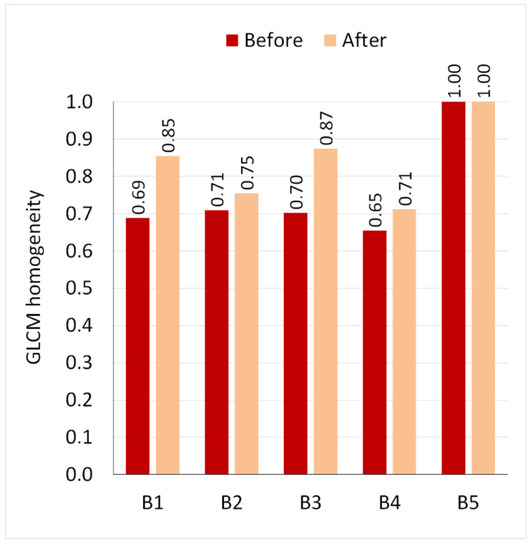
Figure 12.
Homogeneity in GLCM analysis before and after laser application.
4. Discussion
There is currently no gold standard for assessing the effectiveness of laser dye removal. Qualitative scales are the most commonly used. These studies are based on expert evaluation of images before and after the laser dye removal procedure. It should be noted, however, that qualitative studies have a number of disadvantages, including that it depends on the expert’s experience, they do not allow for a quantitative assessment of the effectiveness, and they do not allow the comparison of the effectiveness of the procedure in relation to different dyes, themes, colors. In addition, photos taken with the use of digital cameras are most often evaluated, which means that the method and quality of lighting can significantly affect the assessment of the results. Even a small change in the color temperature of the light illuminating the skin will bring significant differences in the assessment. Hyperspectral imaging is devoid of the above-mentioned disadvantages. It is independent of expert evaluation and is quantitative and repeatable. The color of the dye is significant and has a significant impact on the subjective perception of the effectiveness of permanent makeup removal. Importantly, the color of the analyzed spots (pixels) depends on the type of incident light. Thus, simple methods of statistical analysis and methods of image analysis and processing do not work well in recognizing skin/dye characteristics. In hyperspectral imaging, color is represented by the radiation reflection vector over a wide range of wavelengths. This gives a definitely different set of information than the three-component RGB system and allows for a multi-faceted and multi-perspective analysis of the assessed objects (skin surface) and, thus, very high accuracy in mapping skin/pigment features [21,33,34].
A relatively new method of acquiring image data is hyperspectral imaging. It provides much more information about the examined object compared to traditional digital photography because a hyperspectral image consists of several hundred individual images recorded at precisely-defined wavelengths. Data can be recorded in a wide range of electromagnetic radiation—from ultraviolet through the visible range to infrared [24].
HSI has been used in the diagnosis of precancerous conditions, squamous cell carcinoma of the cervix, and gastric cancer. It is also useful for assessing tissue oxygenation in ischemic wounds and for assessing the risk of foot ulceration in diabetes [35]. It is also used to measure the content of skin chromophores: melanin and hemoglobin [36].
Apart from being used for medical research, the hyperspectral camera can be used to present the effect of cosmetic procedures, such as permanent makeup removal. Selective absorption of laser energy by the dye is a prerequisite for its effective removal without damaging the adjacent structures [25]. Regarding the variety of colors used in permanent makeup, the most effective wavelength should be selected so that the maximum level of dye absorption coincides with the wavelength of the laser. The proposed method of hyperspectral imaging allowed for a quantitative assessment of the spectral parameters of the dyes used in the study and, thus, for optimization of the laser parameters necessary for their removal.
Rupich et al. [14] used hyperspectral imaging to select the most effective type of laser for removing the red pigment of permanent lip makeup. The minimum reflectance observed in the cited study occurred for the wavelength of 487 nm, and the maximum was observed in the range of 700–800 nm. While selecting the wavelength, it was important to determine the minimum reflectance. The higher the reflectance, the more radiation is reflected from the skin surface [14]. On the other hand, in this study, for all tested dyes, the maximum reflectance values were reached at the wavelength range of 640–730 nm, while the highest absorption of radiation energy, manifested by the lowest reflectance values, occurred in the spectral range of 400–500 nm. This confirms the choice of the Q-switched Nd:YAG laser (532 nm) as the most effective for red dye removal. Other lasers operating in the Q-switched mode: ruby (694 nm) and alexandrite (755 nm) show lower efficiency in removing this pigment.
HSI was also used to assess the effectiveness of the Q-switched Nd:YAG laser in removing the five tested dyes from the skin. After a properly performed procedure, according to the assumption, the reflectance should decrease because less dye remains in the skin. The laser application caused a decrease in reflectance for all tested dyes except for white. White pigment is the most difficult to remove due to its high reflectivity. The greatest decrease in reflectance was observed for the B1 dye (red shade), which is the closest to red. The change in wavelength at which the reflectance maximum occurred for two dyes (B2 and B4), manifested by a visible change in their color, indicates that this type of treatment may cause discoloration of the pigment used in permanent makeup.
Another determinant of the effectiveness of laser permanent makeup removal is the increase in homogeneity and decrease in GLCM contrast for all the analyzed colors except for white. These parameters change indicates a more uniform distribution of red pigments after laser treatment. Due to the fact that the amount of pigment in the skin has decreased, the skin has acquired a shade closer to natural.
The increase in the homogeneity of the distribution of dyes after the laser treatment is also confirmed by the quadratic tree decomposition parameters. An increase in the percentage of larger areas and a decrease in small areas was observed after the laser treatment in all tested shades of red, which indicates an increase in image homogeneity.
In conclusion, objective skin measurements are more reliable compared to subjective visual assessment. The hyperspectral imaging method is an effective and non-invasive technique of both optimizing the laser wavelength and assessing the effectiveness of removing permanent makeup pigments from the skin. The HSI method can contribute to the increase in the safety and effectiveness of laser treatments, which will reduce its number and enable the achievement of satisfactory results. Therefore, it is necessary to continue research in order to optimize other parameters of the laser, such as pulse width (msec) and energy density (J/cm2), to the individual characteristics of the skin. However, a significant limitation in the widespread use of this method is its high price.
5. Conclusions
The following conclusions can be drawn from the conducted research:
- The proposed method of hyperspectral imaging allows for a quantitative assessment of the spectral parameters of dyes implanted in pig skin and, thus, optimization of the laser parameters necessary for its removal.
- The laser application causes a decrease in reflectance for all tested dyes except for white. White pigment is the most difficult to remove due to its high reflectivity.
- For all dyes, except for white, a decrease in GLCM contrast and an increase in homogeneity were recorded, which indicates that after laser treatment, dyes are distributed more homogeneously in the skin.
- The increase in the homogeneity of the distribution of dyes after the laser treatment is also confirmed by the quadratic tree decomposition parameters.
- For two tested dyes, a change in the maximum reflectance of radiation in the range of 400–1000 nm was recorded after the laser procedure, which may indicate that the laser treatment may cause a change in the color of the dye.
Author Contributions
Conceptualization, M.K., B.K.-Ś., A.B. and W.P.; methodology, B.K.-Ś., M.K., A.B., M.H.-P., R.K. and W.P.; software, R.K. and M.H.-P.; validation, A.B., R.K. and K.J.; formal analysis, A.B., M.K. and B.K.-Ś.; investigation M.K., B.K.-Ś. and W.P.; resources, S.W.; data curation, M.K., B.K.-Ś., K.J. and W.P.; writing—original draft preparation, M.K., B.K.-Ś., W.P., A.L. and M.H.-P.; writing—review and editing, M.K., B.K.-Ś., A.B., A.L. and S.W.; visualization, A.B., K.J. and M.H.-P.; supervision, S.W.; project administration, A.B.; funding acquisition, S.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Medical University of Silesia, University Funds.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Bioethics Committee of the Medical University of Silesia (PCN/CBN/0022/KB1/27/III/16/17/21).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Naga, L.I.; Alster, T.S. Laser tattoo removal: An Update. Am. J. Clin. Derm. 2017, 18, 59–65. [Google Scholar] [CrossRef] [PubMed]
- De Cuyper, C. Complications of cosmetic tattoos. Curr. Probl. Derm. 2015, 48, 61–70. [Google Scholar]
- Wąsik, A. Microblading. Pomóc naturze. Kosmetol. Estet. 2017, 6, 269–270. [Google Scholar]
- Kumańska, K. Naturalność jest trendy. Kosmetol. Estet. 2019, 8, 693–695. [Google Scholar]
- Kornhaber, R.; Visentin, D.; Thapa, D.K.; West, S.; McKittrick, A.; Haik, J.; Cleary, M. Cosmetic camouflage improves quality of life among patients with skin disfigurement: A systematic review. Body Image 2018, 27, 98–108. [Google Scholar] [CrossRef]
- Sandhu, J.K.; Sharma, P. Skin camouflage therapy. Indian J. Dermatol. Venereol. Leprol. 2022, 88, 718. [Google Scholar] [CrossRef]
- Matuła, A.; Załęska, I.; Lizak, A.; Morawiec, M.; Drąg, J.; Wasylewski, M. The role of cosmetologist in diagnostics and cancer therapy. Kosmetol. Estet. 2018, 7, 445. [Google Scholar]
- Saed, S.; Ibrahim, O.; Bergfeld, W.F. Hair camouflage: A comprehensive review. Int. J. Womens Derm. 2016, 2, 122–127. [Google Scholar] [CrossRef]
- Rassman, W.R.; Pak, J.P.; Kim, J.; Estrin, N.F. Scalp micropigmentation: A concealer for hair and scalp deformities. J. Clin. Aesthet. Derm. 2015, 8, 35–42. [Google Scholar]
- Ju, H.J.; Eun, S.H.; Lee, H.N.; Lee, J.H.; Kim, G.M.; Bae, J.M. Micropigmentation for vitiligo on light to moderately colored skin: Updated evidence from a clinical and animal study. J. Derm. 2020, 47, 464–469. [Google Scholar] [CrossRef]
- Uhlmann, N.R.; Martins, M.M.; Piato, S. 3D areola dermopigmentation (nipple-areola complex). Breast J. 2019, 25, 1214–1221. [Google Scholar] [CrossRef] [PubMed]
- Tomita, S.; Mori, K.; Miyawaki, T. Colour change after paramedical pigmentation of the nipple-areola complex. Aesthetic Plast. Surg. 2018, 42, 656–661. [Google Scholar] [CrossRef]
- McILwee, B.E.; Alster, T.S. Treatment of Cosmetic Tattoos: A review and case analysis. Derm. Surg. 2018, 44, 1565–1570. [Google Scholar] [CrossRef]
- Ruprich, M.; Janiczek, M.; Wilczyński, A. Optimization of laser treatment to remove permanent makeup using hyperspectral imager. Kosmetol. Estet. 2016, 5, 299–301. [Google Scholar]
- Tampa, M.; Mitran, M.I.; Mitran, C.I.; Matei, C.; Amuzescu, A.; Buzatu, A.A.; Georgescu, S.R. Viral infections confined to tattoos—A narrative review. Medicina 2022, 58, 342. [Google Scholar] [CrossRef] [PubMed]
- Torbeck, R.; Bankowski, R.; Henize, S.; Saedi, N. Lasers in tattoo and pigmentation control: Role of the PicoSure® laser system. Med. Devices Evid. Res. 2016, 9, 63–67. [Google Scholar]
- Gemza, K.; Surgiel-Gemza, A. Methods of imaging the effects of laser removal of pigments deposited in the skin, including treatments performed with a picosekond laser. Aesth. Cosmetol. Med. 2020, 9, 383–388. [Google Scholar]
- Kasai, K. Picosecond Laser Treatment for Tattoos and Benign Cutaneous Pigmented Lesions (Secondary publication). Laser Ther. 2017, 26, 274–281. [Google Scholar] [CrossRef]
- Hexsel, D.; Hexsel, C.L.; Dal’Forno, T.; Schilling de Souza, J.; Silva, A.F.; Siega, C. Standardized methods for photography in procedural dermatology using simple equipment. Int. J. Derm. 2017, 56, 444–451. [Google Scholar] [CrossRef]
- Olejnik, A.; Gornowicz-Porowska, J.; Gościńska, J. Analitical methods for testing coemetic products in the past and nowadays. Wiadomości Chem. 2022, 76, 607–633. [Google Scholar]
- Pathania, Y.S.; Apalla, Z.; Salerni, G.; Patil, A.; Grabbe, S.; Goldust, M. Non-invasive diagnostic techniques in pigmentary skin disorders and skin cancer. J. Cosmet. Derm. 2022, 21, 444–450. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Lee, M.H.; Noh, T.K.; Choi, K.H.; Won, C.H.H.; Chang, S.E.; Lee, M.W.; Choi, J.W. Successful treatment of tattoos with a picosecond 735 nm alexandrite laser in Asian skin. Ann. Derm. 2016, 28, 673–675. [Google Scholar] [CrossRef] [PubMed]
- Stolecka-Warzecha, A.; Chmielewski, Ł.; Wilczyński, S.; Koprowski, R. In vitro hyperspectral analysis of tattoo dyes. Skin Res. Technol. 2023, 29, e13268. [Google Scholar] [CrossRef]
- Wilczyński, S.; Koprowski, R.; Marmion, M.; Duda, P.; Błońska-Fajfrowska, B. The use of hyperspectral imaging in the VNIR (400–1000 nm) and SWIR range (1000–2500 nm) for detecting counterfeit drugs with identical API composition. Talanta 2016, 160, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Koprowski, R.; Wilczyński, S.; Wróbel, Z.; Błońska-Fajfrowska, B. Calibration and segmentation of skin areas in hyperspectral imaging for the needs of dermatology. Biomed. Eng. Online 2014, 13, 113. [Google Scholar] [CrossRef] [PubMed]
- Behmann, J.; Acebron, K.; Emin, D.; Bennertz, S.; Matsubara, S.; Thomas, S.; Bohnenkamp, D.; Kuska, M.T.; Jussila, J.; Salo, H.; et al. Specim IQ: Eval uation of a new, miniaturized handheld hyperspectral camera and its application for plant phenotyping and disease detection. Sensors 2018, 18, 441. [Google Scholar] [CrossRef]
- De la Casa Almeida, M.; Serrano, C.S.; Rejano, J.J. Reliability of texture analysis using co-occurence matrices (glcm) on photographic image in the assessment of cellulite in a Spanish population. J. Eur. Acad. Derm. Venereol. 2015, 29, 315–324. [Google Scholar] [CrossRef]
- Odrzywołek, W.; Deda, A.; Zdrada, J.; Wilczyński, S.; Błońska-Fajfrowska, B.; Lipka-Trawińska, A. Quantitative evaluation of the effectiveness of chemical peelings in reducing acne lesions based on grey-level co-occurrence matrix (GLCM). Clin. Cosmet. Investig. Derm. 2022, 15, 1873–1882. [Google Scholar] [CrossRef]
- Maktabdar Oghaz, M.; Maarof, M.A.; Rohani, M.F.; Zainal, A.; Shaid, S.Z.M. An optimized skin texture model using gray-level co-occurrence matrix. Neural. Comput. Appl. 2019, 31, 1835–1853. [Google Scholar] [CrossRef]
- Dhruv, B.; Mittal, N.; Modi, M. Study of Haralick’s and GLCM texture analysis on 3D medical images. Int. J. Neurosci. 2019, 129, 350–362. [Google Scholar] [CrossRef]
- Lu, G.; Fei, B. Medical hyperspectral imaging: A review. J. Biomed. Opt. 2014, 19, 10901. [Google Scholar] [CrossRef] [PubMed]
- Głowacz, A.; Głowacz, A.; Głowacz, Z. Recognition of monochrome thermal images of synchronous motor with the application of quadtree decomposition and backpropagation neural network. Eksploat. I Niezawodn. Maint. Reliab. 2014, 16, 92–96. [Google Scholar]
- Bożek, A.; Reich, A. Assessment of the severity of atopic dermatitis. Przegl. Derm. 2016, 103, 479–485. [Google Scholar] [CrossRef]
- Meng, X.; Xu, C. Progress and prospect of non-invasive detection techniques i the therapeutic evaluation of melasma. Chin. Med. J. 2020, 133, 2104–2106. [Google Scholar] [CrossRef] [PubMed]
- Holmer, A.; Tetschke, F.; Marotz, J.; Malberg, H.; Markgraf, W.; Thiele, C.; Kulcke, A. Oxygenation and perfusion monitoring with a hyperspectral camera system for chemical based tissue analysis of skin and organs. Physiol. Meas. 2016, 37, 2064–2078. [Google Scholar] [CrossRef]
- Nkengne, A.; Robic, J.; Seroul, P.; Gueheunneux, S.; Jomier, M.; Vie, K. SpectraCam®: A new polarized hyperspectral imaging system for repeatable and reproducible in vivo skin quantification of melanin, total hemoglobin, and oxygen saturation. Ski. Res. Technol. 2018, 24, 99–107. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).