Delirium Prediction Using Machine Learning Interpretation Method and Its Incorporation into a Clinical Workflow
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source and Transparency
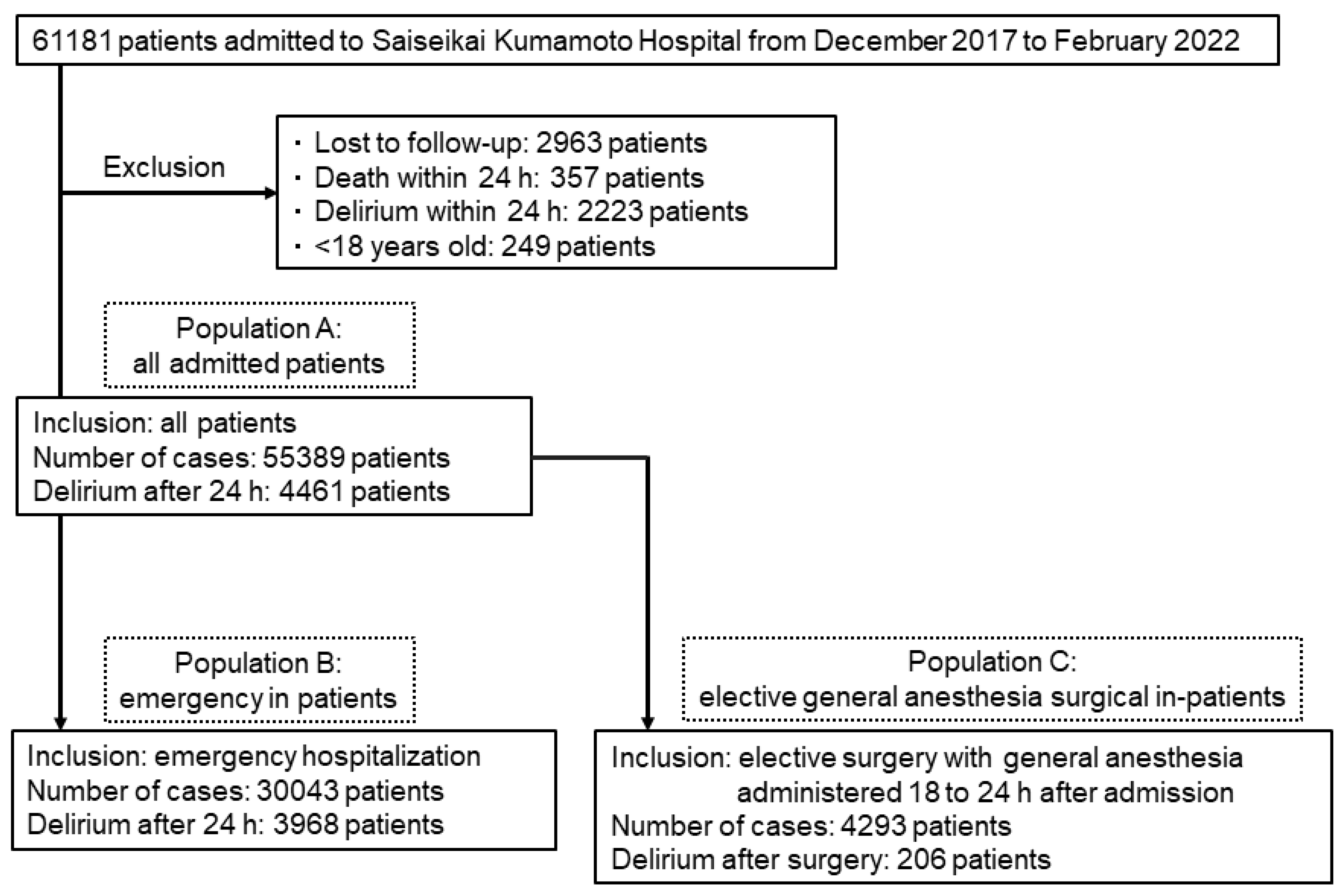
2.2. Study Design and Patients
2.3. Clinical Outcomes
2.4. Predictors
2.5. Development of Prediction Models
2.6. Handling of Missing Data
2.7. Assessment of Prediction Models
2.8. Confirmation of Predictive Contributors Using the Mchine Learning Interpretation Method
2.9. Statistical Methods
3. Results
3.1. Patient Characteristics
3.2. Performance of Delirium Prediction Models Based on XGBoost
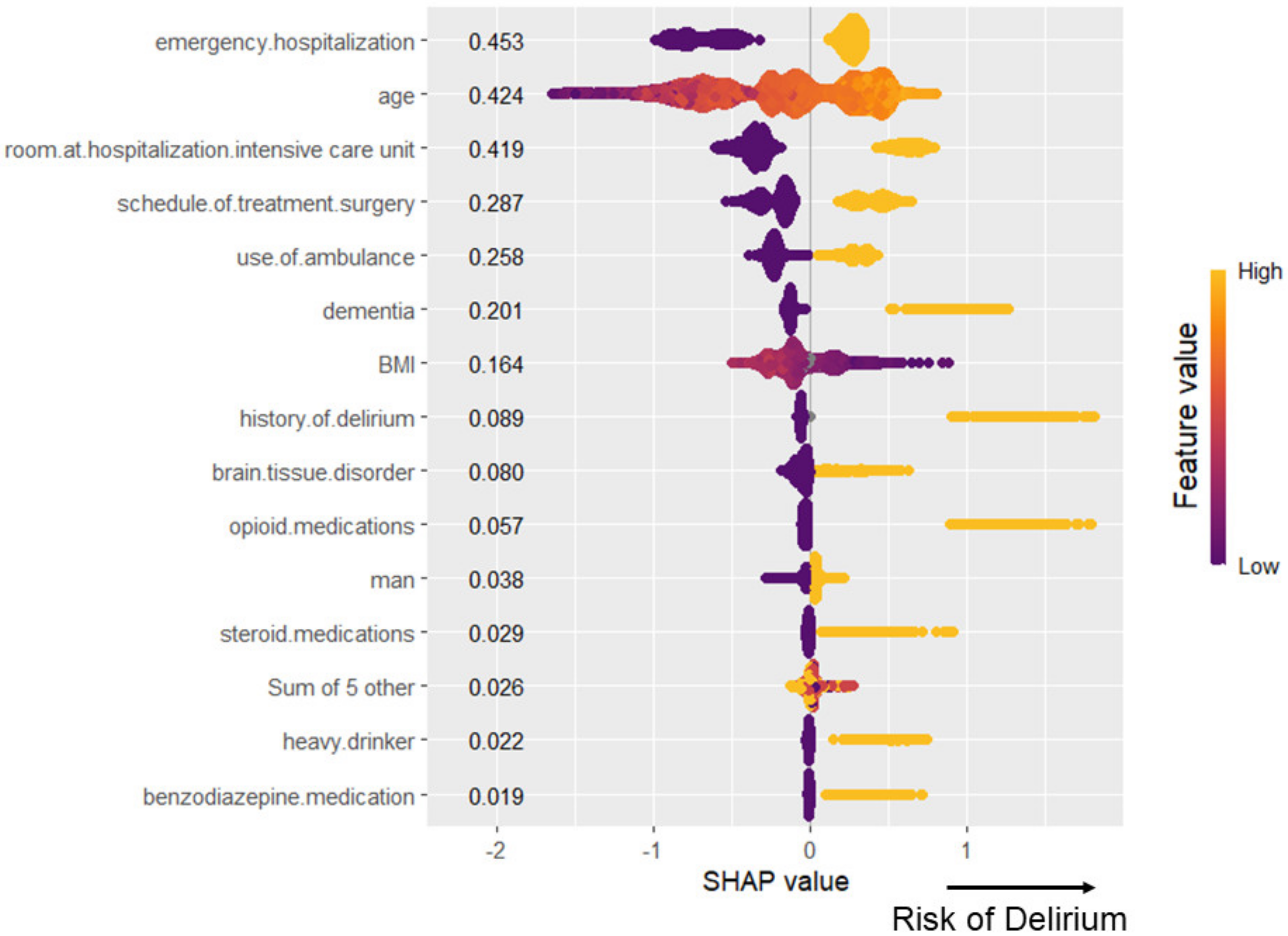
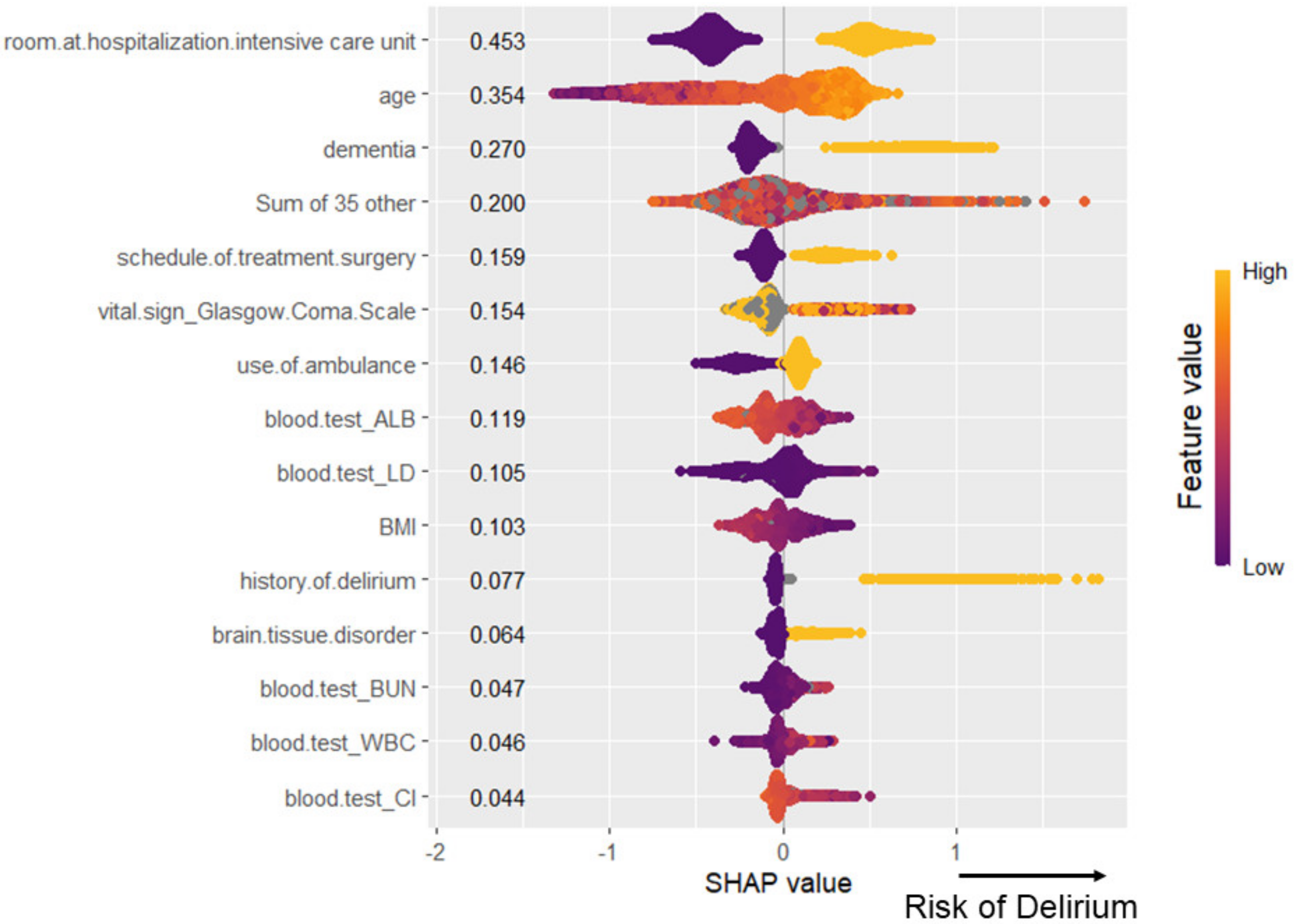
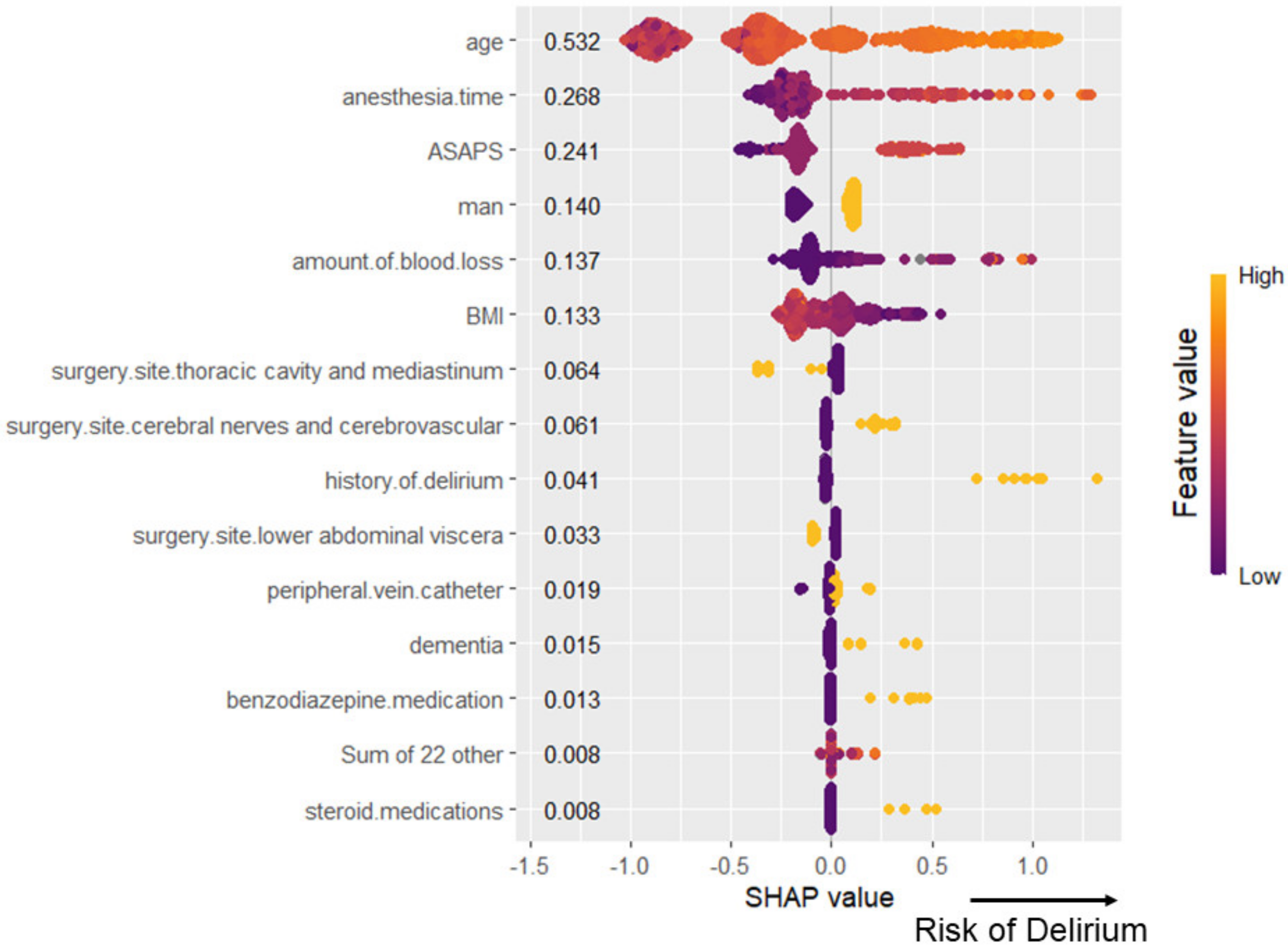
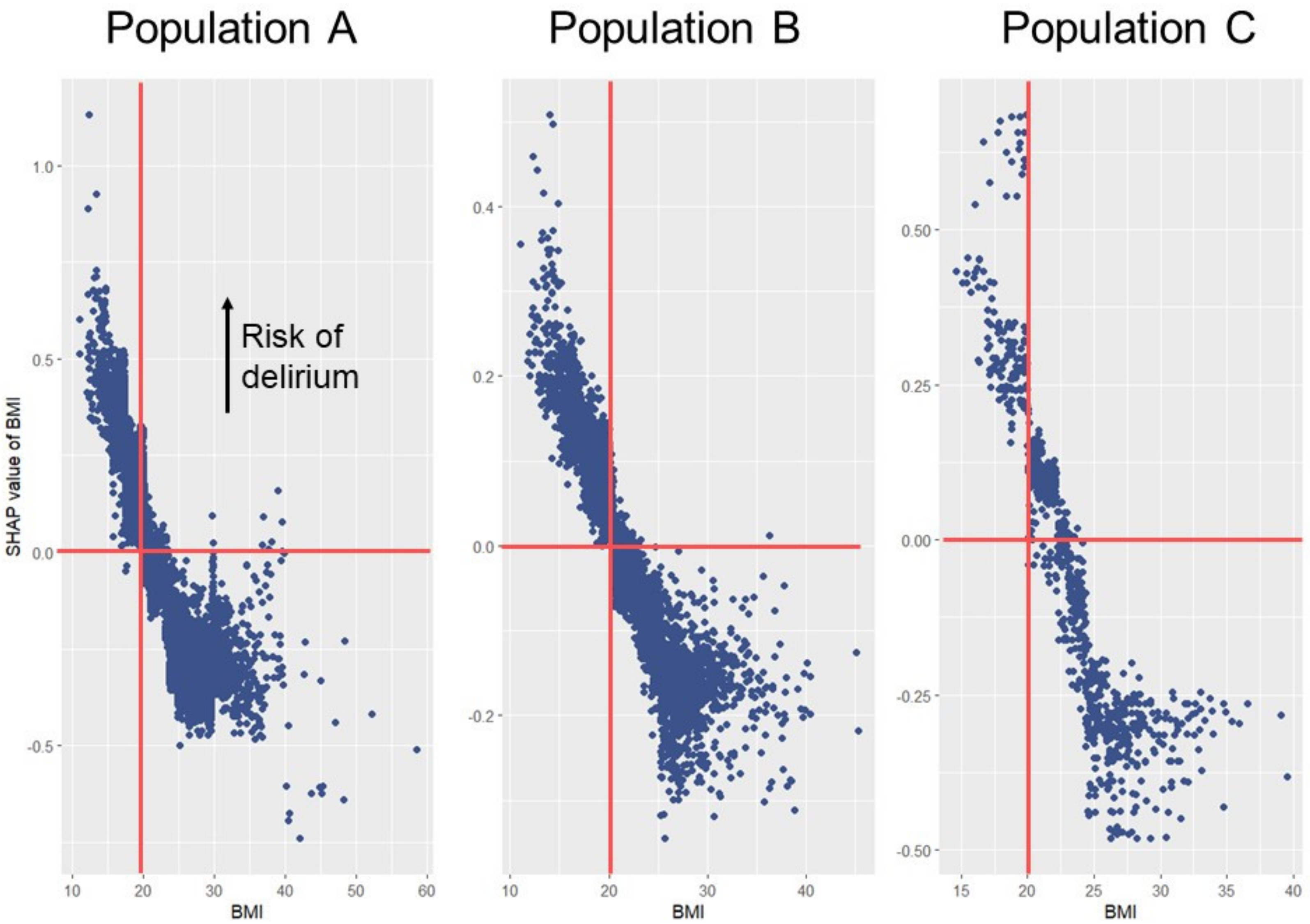
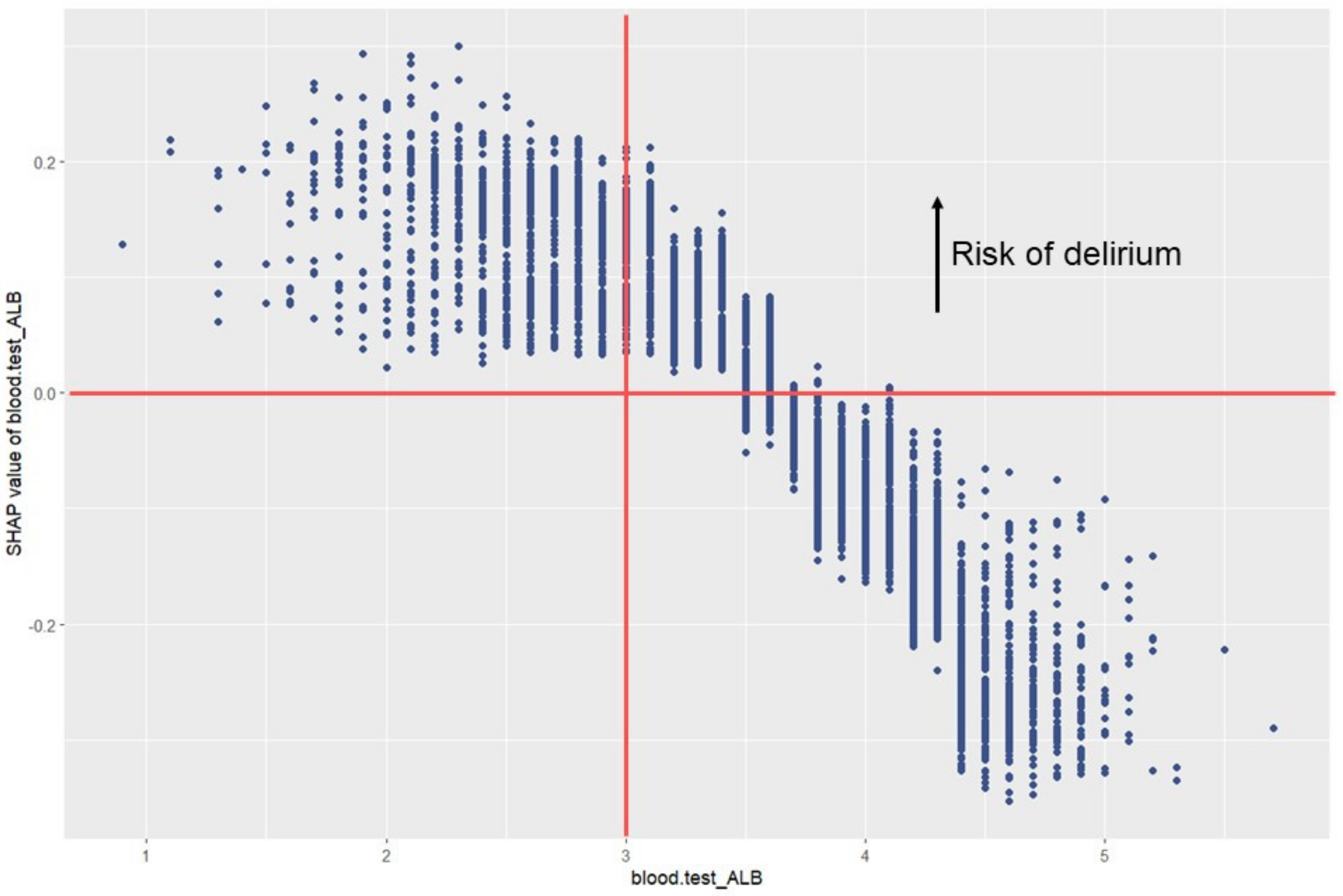
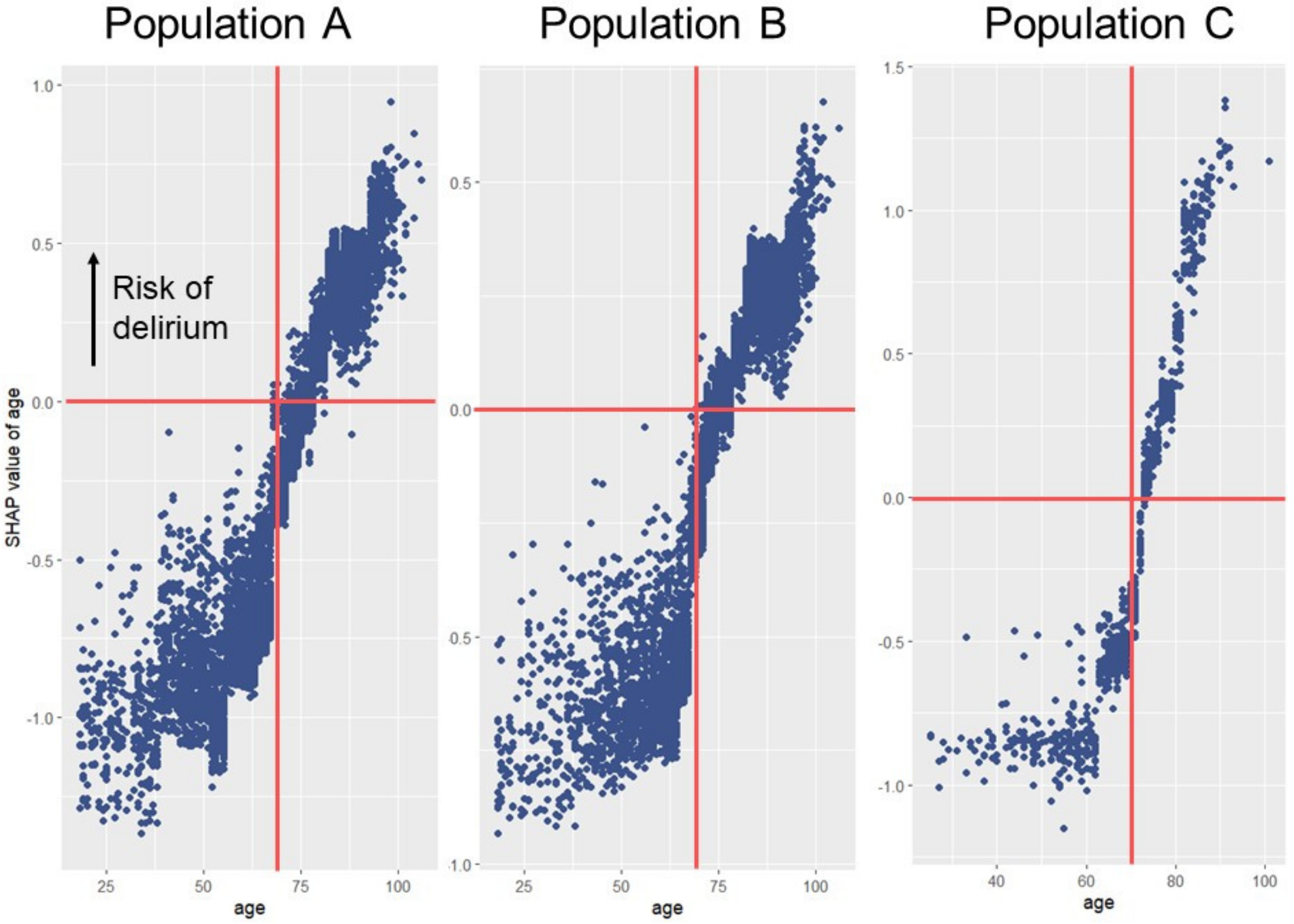
3.3. Interpretation of Predictors
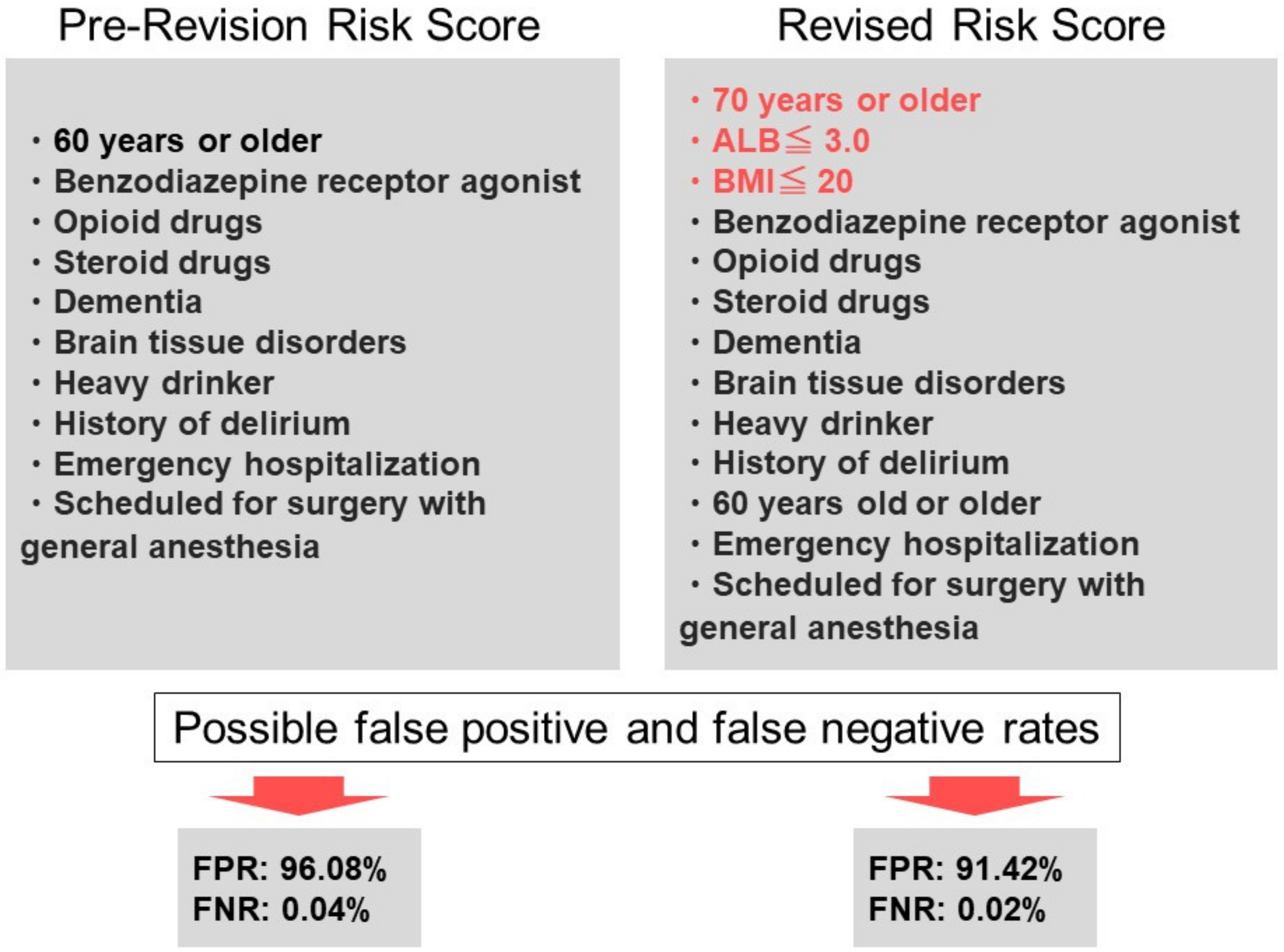
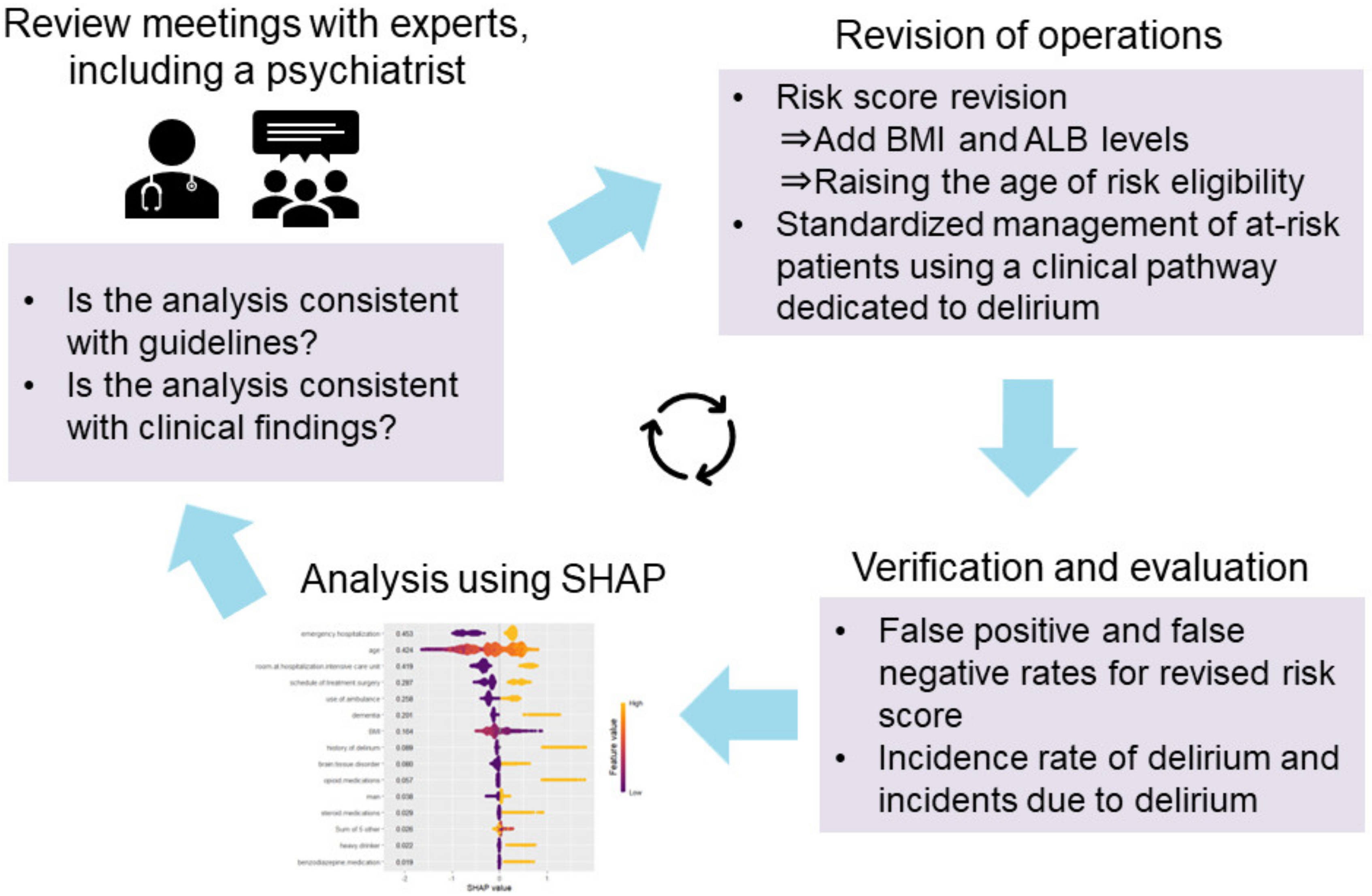
3.4. Review and Use of Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Olsen, L.A.; Aisner, D.; McGinnis, J.M. The Learning Healthcare System: Workshop Summary; National Academies Press: Washington, DC, USA, 2007. [Google Scholar]
- McGinnis, J.M.; Fineberg, H.V.; Dzau, V.J. Advancing the Learning Health System. N. Engl. J. Med. 2021, 385, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Platt, R.; Harvard Pilgrim Health Care Institute; Huang, S.S.; Perlin, J.B. A win for the learning health system. In NAM Perspect; National Academy of Medicine: Washington, DC, USA, 2013; Volume 3. [Google Scholar] [CrossRef]
- Inouye, S.K.; Westendorp, R.G.; Saczynski, J.S. Delirium in elderly people. Lancet 2014, 383, 911–922. [Google Scholar] [CrossRef] [PubMed]
- Witlox, J.; Eurelings, L.S.M.; de Jonghe, J.F.M.; Kalisvaart, K.J.; Eikelenboom, P.; van Gool, W.A. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia. JAMA 2010, 304, 443–451. [Google Scholar] [CrossRef] [PubMed]
- Inouye, S.K.; Viscoli, C.M.; Horwitz, R.I.; Hurst, L.D.; Tinetti, M.E. A predictive model for delirium in hospitalized elderly medical patients based on admission characteristics. Ann. Intern. Med. 1993, 119, 474–481. [Google Scholar] [CrossRef] [PubMed]
- Pompei, P.; Foreman, M.; Rudberg, M.A.; Inouye, S.K.; Braund, V.; Cassel, C.K. Delirium in hospitalized older persons: Outcomes and predictors. J. Am. Geriatr. Soc. 1994, 42, 809–815. [Google Scholar] [CrossRef]
- O’Keeffe, S.T.; Lavan, J.N. Predicting delirium in elderly patients: Development and validation of a risk-stratification model. Age Ageing 1996, 25, 317–321. [Google Scholar] [CrossRef]
- Pendlebury, S.T.; Lovett, N.; Smith, S.C.; Cornish, E.; Mehta, Z.; Rothwell, P.M. Delirium risk stratification in consecutive unselected admissions to acute medicine: Validation of externally derived risk scores. Age Ageing 2016, 45, 60–65. [Google Scholar] [CrossRef]
- Rudolph, J.L.; Doherty, K.; Kelly, B.; Driver, J.A.; Archambault, E. Validation of a delirium risk assessment using electronic medical record information. J. Am. Med. Dir. Assoc. 2015, 17, 244–248. [Google Scholar] [CrossRef]
- de Wit, H.A.J.M.; Winkens, B.; Gonzalvo, C.M.; Hurkens, K.P.G.M.; Mulder, W.J.; Janknegt, R.; Verhey, F.R.; van der Kuy, P.-H.M.; Schols, J.M.G.A. The development of an automated ward independent delirium risk prediction model. Pharm. Weekbl. 2016, 38, 915–923. [Google Scholar] [CrossRef]
- Solà-Miravete, E.; López, C.; Martínez-Segura, E.; Adell-Lleixà, M.; Juvé-Udina, M.E.; Lleixà-Fortuño, M. Nursing assessment as an effective tool for the identification of delirium risk in older in-patients: A case-control study. J. Clin. Nurs. 2017, 27, 345–354. [Google Scholar] [CrossRef]
- Douglas, V.C.; Hessler, C.S.; Dhaliwal, G.; Betjemann, J.P.; Fukuda, K.A.; Alameddine, L.R.; Lucatorto, R.; Johnston, S.C.; Josephson, S.A. The AWOL tool: Derivation and validation of a delirium prediction rule. J. Hosp. Med. 2013, 8, 493–499. [Google Scholar] [CrossRef]
- Brown, E.G.; Josephson, S.A.; Anderson, N.; Reid, M.; Lee, M.; Douglas, V.C. Predicting inpatient delirium: The AWOL delirium risk-stratification score in clinical practice. Geriatr. Nurs. 2017, 38, 567–572. [Google Scholar] [CrossRef]
- Wong, A.; Young, A.T.; Liang, A.S.; Gonzales, R.; Douglas, V.C.; Hadley, D. Development and validation of an electronic health record-based machine learning model to estimate delirium risk in newly hospitalized patients without known cognitive impairment. JAMA Netw. Open 2018, 1, e181018. [Google Scholar] [CrossRef]
- Corradi, J.P.; Thompson, S.; Mather, J.F.; Waszynski, C.M.; Dicks, R.S. Prediction of Incident Delirium Using a Random Forest classifier. J. Med. Syst. 2018, 42, 261. [Google Scholar] [CrossRef]
- Davoudi, A.; Ozrazgat-Baslanti, T.; Ebadi, A.; Bursian, A.C.; Bihorac, A.; Rashidi, P. Delirium Prediction using Machine Learning Models on Predictive Electronic Health Records Data. In Proceedings of the 2017 IEEE 17th International Conference on Bioinformatics and Bioengineering (BIBE), Washington, DC, USA, 23–25 October 2017; pp. 568–573. [Google Scholar] [CrossRef]
- Kramer, D.; Veeranki, S.; Hayn, D.; Quehenberger, F.; Leodolter, W.; Jagsch, C.; Schreier, G. Development and validation of a multivariable prediction model for the occurrence of delirium in hospitalized gerontopsychiatry and internal medicine patients. Stud. Health Technol. Inform. 2017, 236, 32–39. [Google Scholar]
- Mufti, H.N.; Hirsch, G.M.; Abidi, S.R.; Abidi, S.S.R. Exploiting machine learning algorithms and methods for the prediction of agitated delirium after cardiac surgery: Models development and validation study. JMIR Public Health Surveill. 2019, 7, e14993. [Google Scholar] [CrossRef]
- Veeranki, S.P.K.; Hayn, D.; Jauk, S.; Quehenberger, F.; Kramer, D.; Leodolter, W.; Schreier, G. An improvised classification model for predicting delirium. Stud. Health Technol. Inform. 2019, 264, 1566–1567. [Google Scholar] [CrossRef]
- Chua, S.J.; Wrigley, S.; Hair, C.; Sahathevan, R. Prediction of delirium using data mining: A systematic review. J. Clin. Neurosci. 2021, 91, 288–298. [Google Scholar] [CrossRef]
- Oosterhoff, J.H.F.; Karhade, A.V.; Oberai, T.; Franco-Garcia, E.; Doornberg, J.N.; Schwab, J.H. Prediction of postoperative delirium in geriatric hip fracture patients: A clinical prediction model using machine learning algorithms. Geriatr. Orthop. Surg. Rehabil. 2021, 12, 21514593211062277. [Google Scholar] [CrossRef]
- Hur, S.; Ko, R.-E.; Yoo, J.; Ha, J.; Cha, W.C.; Chung, C.R. A machine learning-based algorithm for the prediction of intensive care unit delirium (pride): Retrospective study. JMIR Public Health Surveill. 2021, 9, e23401. [Google Scholar] [CrossRef]
- Bishara, A.; Chiu, C.; Whitlock, E.L.; Douglas, V.C.; Lee, S.; Butte, A.J.; Leung, J.M.; Donovan, A.L. Postoperative delirium prediction using machine learning models and preoperative electronic health record data. BMC Anesthesiol. 2022, 22, 8. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Wan, D.H.; Chen, M.; Li, Y.L.; Ying, H.; Yao, G.L.; Liu, Z.L.; Zhang, G.M. Automated machine learning-based model for the prediction of delirium in patients after surgery for degenerative spinal disease. CNS Neurosci. Ther. 2022, 29, 282–295. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Schlesinger, J.J.; McCoy, A.B.; Reese, T.J.; Steitz, B.; Russo, E.; Koh, B.; Wright, A. New onset delirium prediction using machine learning and long short-term memory (LSTM) in electronic health record. J. Am. Med. Inform. Assoc. 2022, 30, 120–131. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, K.; Nohara, Y.; Soejima, H.; Yonehara, T.; Nakashima, N.; Kamouchi, M. Stroke prognostic scores and data-driven prediction of clinical outcomes after acute ischemic stroke. Stroke 2020, 51, 1477–1483. [Google Scholar] [CrossRef]
- Matsumoto, K.; Nohara, Y.; Wakata, Y.; Yamashita, T.; Kozuma, Y.; Sugeta, R.; Yamakawa, M.; Yamauchi, F.; Miyashita, E.; Takezaki, T.; et al. Impact of a learning health system on acute care and medical complications after intracerebral hemorrhage. Learn. Health Syst. 2021, 5, e10223. [Google Scholar] [CrossRef]
- Zhao, Q.-Y.; Wang, H.; Luo, J.-C.; Luo, M.-H.; Liu, L.-P.; Yu, S.-J.; Liu, K.; Zhang, Y.-J.; Sun, P.; Tu, G.-W.; et al. Development and validation of a machine-learning model for prediction of extubation failure in intensive care units. Front. Med. 2021, 8, 676343. [Google Scholar] [CrossRef]
- Wang, K.; Tian, J.; Zheng, C.; Yang, H.; Ren, J.; Liu, Y.; Han, Q.; Zhang, Y. Interpretable prediction of 3-year all-cause mortality in patients with heart failure caused by coronary heart disease based on machine learning and SHAP. Comput. Biol. Med. 2021, 137, 104813. [Google Scholar] [CrossRef]
- Tseng, P.-Y.; Chen, Y.-T.; Wang, C.-H.; Chiu, K.-M.; Peng, Y.-S.; Hsu, S.-P.; Chen, K.-L.; Yang, C.-Y.; Lee, O.K.-S. Prediction of the development of acute kidney injury following cardiac surgery by machine learning. Crit. Care 2020, 24, 478. [Google Scholar] [CrossRef]
- Hathaway, Q.A.; Roth, S.M.; Pinti, M.V.; Sprando, D.C.; Kunovac, A.; Durr, A.J.; Cook, C.C.; Fink, G.K.; Cheuvront, T.B.; Grossman, J.H.; et al. Machine-learning to stratify diabetic patients using novel cardiac biomarkers and integrative genomics. Cardiovasc. Diabetol. 2019, 18, 78. [Google Scholar] [CrossRef]
- Localio, A.R.; Stack, C.B. TRIPOD: A New Reporting Baseline for Developing and Interpreting Prediction Models. Ann. Intern. Med. 2015, 162, 73–74. [Google Scholar] [CrossRef]
- Inouye, S.K.; Van Dyck, C.H.; Alessi, C.A.; Balkin, S.; Siegal, A.P.; Horwitz, R.I. Clarifying confusion: The confusion assessment method. A new method for detection of delirium. Ann. Intern. Med. 1990, 113, 941–948. [Google Scholar] [CrossRef]
- Chen, T.; Guestrin, C. XGBoost: A scalable tree boosting system. In Proceedings of the KDD’16: Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–17 August 2016; pp. 785–794. [Google Scholar]
- Ozenne, B.; Subtil, F.; Maucort-Boulch, D. The precision–recall curve overcame the optimism of the receiver operating characteristic curve in rare diseases. J. Clin. Epidemiol. 2015, 68, 855–859. [Google Scholar] [CrossRef]
- Steyerberg, E.W.; Vickers, A.J.; Cook, N.R.; Gerds, T.; Gonen, M.; Obuchowski, N.; Pencina, M.J.; Kattan, M.W. Assessing the performance of prediction models: A framework for traditional and novel measures. Epidemiology 2010, 21, 128–138. [Google Scholar] [CrossRef]
- Lundberg, S.; Lee, S.-I. A unified approach to interpreting model predictions. In Proceedings of the 31st Conference on Neural Information Processing Systems (NIPS 2017), Long Beach, CA, USA, 4–9 December 2017; pp. 4765–4774. [Google Scholar]
- Kalimisetty, S.; Askar, W.; Fay, B.; Khan, A. Models for Predicting Incident Delirium in Hospitalized Older Adults: A Systematic Review. J. Patient-Cent. Res. Rev. 2017, 4, 69–77. [Google Scholar] [CrossRef]
- Chen, X.; Lao, Y.; Zhang, Y.; Qiao, L.; Zhuang, Y. Risk predictive models for delirium in the intensive care unit: A systematic review and meta-analysis. Ann. Palliat. Med. 2021, 10, 1467. [Google Scholar] [CrossRef]
- Ruppert, M.M.B.; Lipori, J.B.; Patel, S.; Ingersent, E.; Cupka, J.B.; Ozrazgat-Baslanti, T.; Loftus, T.; Rashidi, P.; Bihorac, A.M. ICU Delirium-Prediction Models: A Systematic Review. Crit. Care Explor. 2020, 2, e0296. [Google Scholar] [CrossRef]
- Jauk, S.; Kramer, D.; Großauer, B.; Rienmüller, S.; Avian, A.; Berghold, A.; Leodolter, W.; Schulz, S. Risk prediction of delirium in hospitalized patients using machine learning: An implementation and prospective evaluation study. J. Am. Med. Inform. Assoc. 2020, 27, 1383–1392. [Google Scholar] [CrossRef]
- Sun, H.; Depraetere, K.; Meesseman, L.; Silva, P.C.; Szymanowsky, R.; Fliegenschmidt, J.; Hulde, N.; von Dossow, V.; Vanbiervliet, M.; De Baerdemaeker, J.; et al. Machine learning-based prediction models for different clinical risks in different hospitals: Evaluation of live performance. J. Med. Internet Res. 2022, 24, e34295. [Google Scholar] [CrossRef]
| Predictors | Overall n = 55,389 | No Delirium n = 50,928 | Delirium n = 4461 | p Value | % Missing |
|---|---|---|---|---|---|
| Predisposing risk factors | |||||
| Age, year | 73.0 (64.0–82.0) | 72.0 (64.0–81.0) | 83.0 (74.0–89.0) | <0.001 | 0.0 |
| Body mass index, kg/m² | 22.5 (20.0–25.1) | 22.7 (20.2–25.3) | 20.6 (18.2–23.2) | <0.001 | 1.1 |
| Men | 33,829 (61.1) | 31,474 (61.8) | 2355 (52.8) | <0.001 | 0.0 |
| Intake of benzodiazepine medications | 977 (1.8) | 812 (1.7) | 165 (3.8) | <0.001 | 4.4 |
| Intake of opioid medications | 896 (1.7) | 690 (1.4) | 206 (4.7) | <0.001 | 4.4 |
| Intake of steroid medications | 1829 (3.5) | 1573 (3.2) | 256 (5.9) | <0.001 | 4.4 |
| Dementia | 4907 (9.3) | 3450 (7.1) | 1457 (33.3) | <0.001 | 4.4 |
| Brain tissue disorder | 7028 (13.3) | 5950 (12.3) | 1078 (24.7) | <0.001 | 4.4 |
| Heavy drinker | 878 (1.7) | 701 (1.4) | 177 (4.0) | <0.001 | 4.4 |
| History of delirium | 1307 (2.5) | 802 (1.7) | 505 (11.5) | <0.001 | 4.4 |
| Emergency hospitalization | 30,043 (54.2) | 26,075 (51.2) | 3968 (88.9) | <0.001 | 0.0 |
| Use of ambulance | 19,189 (34.6) | 15,948 (31.3) | 3241 (72.7) | <0.001 | 0.0 |
| Room at hospitalization | <0.001 | 0.0 | |||
| Bay of general ward | 16,139 (29.1) | 15,570 (30.6) | 569 (12.8) | ||
| Intensive care unit | 12,216 (22.1) | 9661 (19.0) | 2555 (57.3) | ||
| Private room of general ward | 27,034 (48.8) | 25,697 (50.5) | 1337 (30.0) | ||
| Schedule of treatment | <0.001 | 0.0 | |||
| Catheterization | 7249 (13.1) | 6950 (13.6) | 299 (6.7) | ||
| Endoscopic treatment | 5032 (9.1) | 4792 (9.4) | 240 (5.4) | ||
| Preserved treatment | 23,554 (42.5) | 21,421 (42.1) | 2133 (47.8) | ||
| Surgery | 19,554 (35.3) | 17,765 (34.9) | 1789 (40.1) |
| Analysis Population | Algorithm | Discrimination | Calibration | Overall | ||||
|---|---|---|---|---|---|---|---|---|
| Sensitivity | Specificity | AUROC | AUPRC | Slope | Intercept | Brier Score | ||
| A, n = 55,389 | XGBoost | 0.838 (0.015) | 0.721 (0.022) | 0.852 (0.005) | 0.329 (0.015) | 1.013 (0.038) | 0.001 (0.049) | 0.062 (0.002) |
| B, n = 30,043 | 0.783 (0.027) | 0.690 (0.015) | 0.806 (0.006) | 0.365 (0.014) | 1.102 (0.017) | 0.002 (0.017) | 0.098 (0.001) | |
| C, n = 4293 | 0.767 (0.084) | 0.709 (0.040) | 0.794 (0.033) | 0.177 (0.052) | 1.032 (0.347) | −0.047 (0.306) | 0.044 (0.004) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matsumoto, K.; Nohara, Y.; Sakaguchi, M.; Takayama, Y.; Fukushige, S.; Soejima, H.; Nakashima, N. Delirium Prediction Using Machine Learning Interpretation Method and Its Incorporation into a Clinical Workflow. Appl. Sci. 2023, 13, 1564. https://doi.org/10.3390/app13031564
Matsumoto K, Nohara Y, Sakaguchi M, Takayama Y, Fukushige S, Soejima H, Nakashima N. Delirium Prediction Using Machine Learning Interpretation Method and Its Incorporation into a Clinical Workflow. Applied Sciences. 2023; 13(3):1564. https://doi.org/10.3390/app13031564
Chicago/Turabian StyleMatsumoto, Koutarou, Yasunobu Nohara, Mikako Sakaguchi, Yohei Takayama, Shota Fukushige, Hidehisa Soejima, and Naoki Nakashima. 2023. "Delirium Prediction Using Machine Learning Interpretation Method and Its Incorporation into a Clinical Workflow" Applied Sciences 13, no. 3: 1564. https://doi.org/10.3390/app13031564
APA StyleMatsumoto, K., Nohara, Y., Sakaguchi, M., Takayama, Y., Fukushige, S., Soejima, H., & Nakashima, N. (2023). Delirium Prediction Using Machine Learning Interpretation Method and Its Incorporation into a Clinical Workflow. Applied Sciences, 13(3), 1564. https://doi.org/10.3390/app13031564









