Abstract
Background: Neck pain (NP) is a frequent condition in women, characterized by exhibiting distinct clinical manifestations such as the presence of deep neck (DN) muscle weakness. Endurance and ultrasonography of the DN muscles, and patient-reported outcome measures, are commonly used outcomes in clinical practice. The aim of this study is to assess and correlate the endurance of the DN muscles and their morphological characteristics with pain intensity, neck disability and headache impact. Methods: An observational and correlational study was carried out. Eighty-two women were recruited, and endurance tests of neck flexor and extensor (chin tuck flexion test and neck extensor muscles endurance test), ultrasonography of the DN muscles, pain intensity, disability (neck disability index) and headache impact (HIT-6) were measured. Spearman’s rho was used to evaluate the correlation between the outcome variables, and a simple linear regression analysis was carried out to explain the model in detail. Results: Statistically significant negative correlations between the chin tuck neck flexion test and neck disability index (NDI) (r = −0.38; p < 0.001) and HIT-6 (r = −0.26; p = 0.02) were found. The neck extensor muscles endurance test showed a negative correlation with NDI (r = −0.27; p = 0.01) and HIT-6 (r = −0.26; p = 0.02). The simple linear regression analysis showed an R squared of 26.7% and was statistically significant (NDI: R squared = 0.267; F = 3.13; p = 0.004) for NDI. Conclusion: A negative correlation between deep neck muscle endurance test results and self-reported outcome measures in women with low cervical disability and neck pain were observed. This suggests that lower endurance in the deep neck muscles may be associated with poorer self-reported symptoms and functionality in these patients. The chin tuck neck flexion test and deep extensor muscles endurance test could predict self-perceived neck disability in women with low cervical disability and NP.
1. Introduction
The number of consultations in rehabilitation settings for chronic musculoskeletal disorders is rising [1]. According to the World Health Organization (WHO), the population over 60 years of age is expected to triple by 2050, from 600 million to 2 billion [2]. As a result, common chronic musculoskeletal conditions such as neck pain are likely to affect a growing number of people, causing pain, disability, and physical function limitations for longer periods of their lifetimes [2].
Neck pain is a frequent cause for seeking healthcare attention, with individuals often seeking medical help in primary care, neurology, neurosurgery and physiotherapy settings [3,4]. The global prevalence of neck pain is estimated at 2696 cases per 100,000 population, with an incidence of 579 individuals per 100,000 population. Unfortunately, neck pain frequently becomes a chronic condition, leading to prolonged disability. Approximately 267.4 individuals per 100,000 population live with neck disability, suggesting that about 50% of those experiencing neck pain are at risk of developing chronicity and disability related to this issue [5].
In Spain, the prevalence of neck pain was estimated to be 4200 and 4500 cases per 1000,000 population, with an incidence of 800–850 cases per 100,000 population [6]. The prevalence of neck pain is higher in women than in men [7]. Additionally, the occurrence of neck pain tends to increase with age, reaching a peak between the ages of 30 and 45 [8]. Moreover, women tend to experience a greater number of years lived with disability attributed to neck pain when compared to men [5].
Neck pain is clinically characterized as the sensation of discomfort or tenderness localized between the upper nuchal line and the spinous process of the first thoracic vertebra [9]. Furthermore, this discomfort may manifest as pain radiating to adjacent regions, encompassing the head, trunk, and upper extremities [9]. Many times, patients experience mild neck disability with recurrent episodes [10]. The term “low neck disability” is used to describe a condition where individuals face limitations or restrictions in their physical activities due to neck pain, but it is not severe enough to completely impede their ability to perform daily tasks [11,12]. However, despite the recurrent nature of these episodes and their tendency to persist over time, which could precede chronic pain, patients often refrain from seeking healthcare due to the perceived non-seriousness of the pain [13].
Patients with low neck disability usually have multifactorial clinical conditions. These include mild neck pain, weak neck muscles, limited neck movement, and self-reported disability, typically scoring between 5 and 14 on the Neck Disability Index (NDI) questionnaire [14,15,16,17]. The alteration of the activity of the masticatory musculature [18] and the presence of vision alterations are other common characteristics that some patients describe, as well [19]. Many neck disorders, such as chronic neck pain, cervicogenic headache, and cervicogenic dizziness, are also associated with muscle weakness [14]. Muscle weakness is considered one of the primary risk factors for neck pain and has been linked to the onset and persistence of pain [20,21,22,23].
In patients with neck pain, there is reduced endurance in the neck flexor and extensor muscles and increased tone in superficial muscles [24,25]. Prolonged reduction in neck muscle endurance may lead to a decrease in the cross-sectional area (CSA) of these muscles [26]. Several studies have found reduced CSA in muscles such as multifidus, semispinalis, and longus coli in individuals with chronic neck pain [17,27,28]. In the early stages of neck pain, patients may experience slight disruptions in their daily activities [29,30]. Zabihhosseinian et al. [31] found that individuals with low neck pain experienced challenges while raising their shoulder due to fatigue in the neck muscles compared with healthy subjects. Similarly, patients with low neck pain have been observed to show weakness in the deep neck (DN) flexor muscles. These muscles have showed myoelectric fatigue with less workload when compared to healthy subjects [32].
Muscle properties such as the strength and CSA of the DN muscles are commonly measured in clinical practice [33]. The endurance of neck flexor and extensor muscles is assessed using clinical tests such as the chin tuck neck flexion test and neck extensor endurance test [34]. Muscle CSA is typically measured using ultrasonography. A study on chronic neck pain found a negative correlation (r = −0.39, p = 0.03) between the size of the extensor muscles and the neck disability index [17]. However, it is still unclear which muscle property presents a higher relationship with self-perceived outcomes, such as neck pain, neck disability and headache life impact, in order to prioritize it in clinical practice, particularly in patients with low cervical disability and low levels of pain, who often do not seek treatment and where we must focus on prevention so that this problem does not become chronic. Given the increasing number of patients with neck pain [2], focusing on prevention becomes increasingly important. In neck pain, the DN muscles present a reduced functional capacity, with a decrease in endurance and a decrease in CSA [17,28]. To the best of our knowledge, no study has investigated which muscle property presents the higher correlation to the main symptoms of patients with neck pain. Therefore, the aim of this study was to assess the correlation between neck muscle endurance and DN muscle CSA with pain intensity, neck disability and headache impact.
2. Materials and Methods
2.1. Design
A cross-sectional study was conducted. The patients recruited for the study were subjects with subclinical neck pain. The neck muscle strength, the CSA, the self-perceived neck disability and the headache impact were assessed to carry out the study and Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) was followed. The study has been approved by the Research Ethics Committee of the Autonomous Community of Aragon CEICA: PI21/357.
2.2. Subjects
Recruitment was carried out during September and November 2022 in Zaragoza, Spain. Finally, eighty-two women were included, with low cervical disability and neck pain. The selection criteria were:
The inclusion criteria were being over 18 years, the intensity of neck pain being <30 mm measured through the visual analogue scale (VAS), and the patient having a low cervical disability, with an NDI score between 5 and 14 points.
Subjects were excluded from the study if they had a prior history of head or neck trauma suggestive of potential red flags, including possible fractures, if they had experienced an infection in any area proximate to the face, head, or neck, if they had a known presence of tumors or were currently undergoing treatment for such conditions, if they exhibited neurological or cognitive impairments, or if they had received any form of treatment within the preceding month, be it pharmacological or physiotherapeutic [35,36].
2.3. Procedure
During the evaluation demographic data, VAS, NDI, and the headache impact test (HIT-6) were collected. The assessment of the morphological characteristics and the endurance of neck muscles were registered by two physiotherapist evaluators, both with more than ten years of experience. The assessment was carried out in a health consultation where the light was regulated, and the temperature was maintained at 20 °C. A 5 min break was allowed between the assessment of endurance and the morphological characteristics of DN flexor and extensor muscles.
2.3.1. Self-Registered Outcomes
The patients were asked about the neck pain intensity, the self-perceived neck disability and the impact of headache, and these outcomes were registered with VAS, NDI and HIT-6.
The intensity of pain was registered using a 10 cm VAS line, in which 0 was considered “no pain” and 10 was considered “worst pain imaginable”. VAS has been shown to be valid and reliable to assess pain intensity in patients with neck pain, with excellent test–retest reliability values (intraclass correlation coefficient (ICC) = 0.94 [37,38,39,40].
Neck disability was assessed with NDI. This questionnaire consists of 10 items about pain, personal care, lifting, reading, headache, concentration, work, driving, sleeping, and recreation, and the total score ranges from 0 to 50. Higher scores indicate greater disability [41,42,43]. The NDI shows psychometric properties and excellent test–retest reliability values: ICC = 0.97 [44].
The impact of the headache was assessed with the short-form HIT-6. This questionnaire consists of 6 items about pain, social participation, general activity, vitality, intellectual activity, and biological suffering, and the total score ranges from 36 to 78. Higher scores indicate greater impact [45]. The internal consistency of HIT-6 was good (Cronbach’s alpha 0.89) and the test–retest reliability was excellent: ICC = 0.78 to 0.90 [46].
2.3.2. Muscle Endurance Test
The chin tuck neck flexion test was intended to determine the endurance of the neck flexor muscles [47]. The patient rested in a supine position and was asked to tuck the chin in while slightly flexing the neck and lifting the head approximately 2.5 cm from the table. The test ended if the patient felt pain or if the patient lost flexion of the upper cervical spine. The time that the patient could maintain the correct position without experiencing any of the aforementioned issues was measured in seconds using a stopwatch [48,49,50]. This test has shown good test–retest reliability, with an ICC = 0.71–0.85 [34,47].
The extensor muscles were assessed in a prone position. The extensor muscle test was developed with the thoracic spine stabilized, fastening a belt across the T6 level, and the head protruded from the treatment table [51]. The CROM device was used to control the position of the head and an external load of 2 kg was applied to the posterior aspect of the head. The patients were instructed to maintain the chin-in position and the test was ended when the deviation of the head was higher than 5° for a minimum of 5 s. The time that the patient could maintain the correct position was measured in seconds using a stopwatch. This test had a good test–retest reliability with ICC = 0.52–0.73 [34].
2.3.3. Morphological Characteristics of Deep Neck Muscles
Ultrasound (Logic e V2 de General Electric) with 8 MHz, and a 28.7 mm linear array 3 transducer was used to measure the DN flexor and extensor muscles. The CSA was registered by tracing around the muscular border of the muscles, and the measurement unit was cm2. Ultrasonography has shown an excellent test–retest reliability with an ICC = 0.92–0.97 [52,53].
The DN flexor muscles measured were the longus capitis and coli muscles. The CSA of these muscles was measured with the patient lying in a supine position and with both arms relaxed along the body [54]. The neck spine was placed in a neutral position of slight lordosis and soft support was placed underneath. To measure the size of the muscle, the thyroid cartilage was identified at the level C5–6, and the screenshot was taken 2 cm through it [55]. The linear transducer was placed horizontally on this surface and then slightly tilted up and down to visualize the DN flexor muscle. The DN flexor muscle is surrounded inferiorly and medially by the vertebral body, laterally by the carotid, and superiorly by the retropharyngeal space [53,56] (Figure 1).
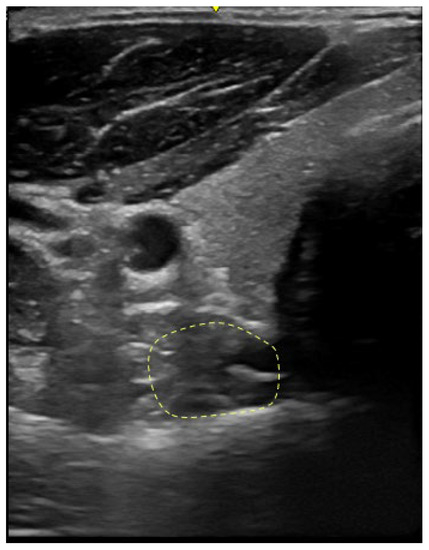
Figure 1.
Cross-sectional area of the deep neck flexor muscle marked by dotted lines.
The DN extensor muscle measured was the multifidus [28]. The CSA of the DN extensor muscle was measured with the patient in a sitting position. To measure the size of the muscle at the level of C4, the linear transducer was placed horizontally in the posterior part of the neck. The multifidus muscle was visualized lateral to the junction between the vertebral lamina and the spinous process and anterior to the semispinalis muscle of the neck [52,53,56,57,58] (Figure 2).
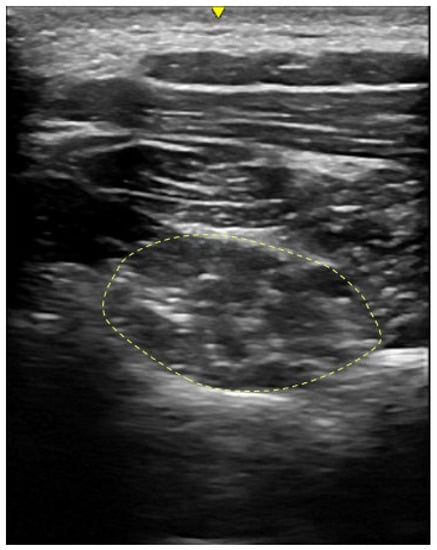
Figure 2.
Cross-sectional area of the deep neck extensor muscle marked by dotted lines.
2.4. Statistical Analysis
Statistical analysis was performed using SPSS version 20.0 for Windows. A descriptive analysis of the demographic and clinical variables of the sample was carried out. The normality of the data was evaluated using the Kolmogorov–Smirnov test and due to some of the outcome measures not being normally distributed, the Spearman’s rho was used to evaluate the correlation between pain intensity, neck disability, headache impact, muscle function tests, and muscle thickness. The association was considered weak if the r value was <0.3, moderate if the r value was between 0.3 and 0.7, and strong if the r value was >0.7 [59].
To evaluate the relationship between neck disability and headache impact with a muscle endurance test and muscle morphological characteristics in more detail, a simple linear regression analysis was carried out. Simple linear regression analysis provides the percentage of variance in the dependent variable that the independent variables explain, expressed as R squared value. NDI and HIT-6 were considered the dependent variables, and DN endurance test and flexor and extensor muscles’ CSA as independent variables.
3. Results
Eighty-two women diagnosed with neck pain with an average age of 35.56 (9.91) years were included in the study. Pain intensity measured with a VAS, neck disability measured with NDI and the impact of headache measured with HIT-6 presented low levels in most of the patients. None of the women presented co-morbidities. The mean and standard deviations of the demographic data, endurance tests and morphological characteristics of the DN flexors and extensors of all the included women are shown in Table 1.

Table 1.
Demographic and clinical characteristics of the sample.
The correlation analysis showed weak to moderate negative correlations between the endurance tests and neck disability and headache impact. The chin tuck test showed a moderate negative correlation with neck disability (r = −0.38), and a weak negative correlation with headache impact (r = −0.26). The extensor muscles test showed a weak negative correlation with neck disability (r = −0.27) and with headache impact (r = −0.26). These correlations were all statistically significant, but no significant correlation was found for any of the endurance tests and pain intensity. Concerning the CSA of the flexor and extensor muscles, only flexor muscles’ CSA showed a weak negative correlation with neck disability (r = −0.22). No associations between the flexor and extensor muscles’ CSA were found with pain intensity or headache impact. The correlation values and the significance of all the tests are shown in Table 2.

Table 2.
Correlation analysis between symptoms and muscle function and thickness.
In a simple linear regression analysis, the statistic R squared indicates the percentage of the variance in the dependent variable that the independent variables explain collectively. NDI and HIT-6 were considered the dependent variables, and endurance test and DN muscles’ CSA as independent variables. For headache impact and pain intensity, the linear regression analysis showed an R squared below 20% and was not statistically significant (HIT-6: R squared = 0.165; F = 1.70; p = 0.113; VAS: R squared = 0.129; F = 1.27; p = 0.271). For neck disability, the simple linear regression analysis showed an R squared of 26.7% and was statistically significant (NDI: R squared = 0.267; F = 3.13; p = 0.004). The chin tuck neck flexion test, extensor muscles endurance test, and DN extensor CSA were significantly associated with the NDI score. Conversely, the DN flexor was not significantly associated with the NDI score. The full results of the linear regression analysis for NDI are shown in Table 3.

Table 3.
Summary of multivariable regression analysis for the NDI score.
4. Discussion
The aim of this study was to investigate if a neck muscle endurance test and/or morphological characteristics of DN muscles were correlated to pain intensity, neck disability and headache impact in patients with neck pain. The muscle endurance test reported a weak to moderate negative correlation to NDI and HIT-6, but not to pain intensity. No ultrasound measurements were correlated to pain intensity, NDI or HIT-6, but DN flexor muscles’ CSA showed a weak negative correlation with NDI.
In women with neck pain and low levels of disability, the endurance tests for neck flexor and extensor muscles have demonstrated a negative correlation with neck disability and the impact of headaches. This suggests that patients with mild neck disability and weakness in the neck flexor and extensor muscles experience higher levels of neck disability, and headaches have a greater impact on their daily life. Kahlaee et al. also reported similar findings, showing a negative correlation between the neck extensor endurance test and the Neck Disability Index (NDI) in patients with chronic pain [17]. Additionally, this study found that patients with chronic neck pain exhibited higher overall muscle fatigability and a smaller size of the deep neck extensor muscles. The results of this study can be added to those presented by Kahlaee et al. [17] in patients with chronic neck pain. These results could be important in the prevention of neck pain. The endurance of the neck flexor and extensor muscles is affected and correlated with the perception of neck disability and headache. In this sense, these patients rarely attend health services, given that cervical pain does not have a significant impact on quality of life [13]. However, it is crucial to consider that this pain could potentially become chronic, making it essential to train the cervical musculature to prevent self-perceived cervical disability. Further research is needed to confirm these findings and explore effective preventive measures.
The results of CSA showed a weak negative association only for DN flexor muscle and neck disability. Concerning ultrasonography measurements, only DN flexor muscles’ CSA showed a weak negative correlation with NDI [60], and therefore subjects with mild disability who have a higher CSA present a lower NDI. In this sense, patients with neck pain for less than 3 months and low levels of disability may present decreased endurance of the neck flexor and extensor muscles, but the CSA may not be affected yet. It has been described that the reduction in DN endurance may lead to a decrease in the CSA when this situation is maintained over time [26]. A clear example in the literature is patients with chronic neck pain. This type of patient presents a decreased activation of the DN flexor and extensor muscles, and a reduced CSA [17,28]. This fact is also described in women; Fernández-de-las-Peñas et al. showed a reduction in the CSA of multifidus muscles in chronic neck pain in comparation with a healthy control [28]. Therefore, compared to what happens with patients with chronic neck pain, patients with low neck disability in the acute or subacute period do not present correlations between the DN extensor muscle CSA and the self-perceived symptoms, but there is a correlation between the DN flexor CSA and NDI. Peng et al. [27] conducted a systematic review with a meta-analysis that compared the morphological characteristics of the muscles between healthy controls and patients with chronic neck pain, showing that the size of longus colli was slightly smaller in patients with chronic neck pain, but the size of the multifidus was equal between groups. Although more studies are needed in this regard, the data of the present study could suggest that the initial stages of neck pain with low self-perceived disability and pain intensity could be an ideal period to start specific neck exercises and use them for prevention. Specific neck exercise has been shown to be effective in improving the endurance of the neck musculature [60]. However, if this were the case, it would be imperative to target and raise awareness among patients exhibiting these characteristics, as well as to disseminate this knowledge within healthcare facilities. As previously mentioned, these patients typically refrain from seeking medical attention due to the mild nature of their disability and pain.
No statistically significant correlations were found between the CSA, endurance test and pain intensity in this study. The results of this study are different from those with patients with chronic neck pain, where a smaller muscle size was observed compared to healthy subjects, as well as a negative correlation between the CSA and the intensity of the neck pain [17]. In this sense, it is also suggested that the smaller the size of the muscle, the greater the pain and disability; this fact could be one of the reasons why a relationship between muscle size and pain and muscle size and neck disability was not found in the present study. The patients in this study had low neck disability, low pain intensity and were not patients with chronic neck pain.
From a clinical point of view, in patients with neck pain for less than 3 months and low levels of disability, clinical tests such as the endurance tests for the neck flexor and extensor muscles may be more useful to test and track the status of the patients in terms of disability and impact than the measurement of the CSA. However, once the situation turns chronic, the evidence showed correlations between the CSA and the main symptoms of the patients. So, future studies should consider the relationship of these outcome variables, taking into account the evolution time and the age of the patients.
This study used the VAS to assess the neck pain, the NDI for the self-perceived neck disability, the HIT-6 for the impact of headache and clinical tests to measure the endurance of the neck flexor and extensor muscles and to evaluate the morphological characteristics of deep neck using ultrasonography. Several limitations were observed during the current study. Although neck pain is more prevalent among women, it is important to acknowledge that the study sample exclusively consisted of female participants. Consequently, caution must be exercised when generalizing the results to male populations. The inclusion criteria were patients with low levels of pain and disability, so the relationships may not be the same for patients with higher levels of pain and disability. Third, the linear mixed model partially explained the results, so more outcome variables should be taken into consideration. The results of this study must be taken with caution; an attempt was made to carry out a study of correlations between seven different variables, and for this purpose 12 subjects per variable were recruited, completing a sample of 82 subjects. This type of study, with such large samples, can bias the results and weaken or strengthen different correlations, so it would be important to carry out a study analyzing the variables that showed correlations in this study.
5. Conclusions
In women with low cervical disability and low neck pain, the neck muscle endurance test demonstrated a moderate correlation with self-perceived disability. This correlation suggests that individuals with lower neck muscle endurance tend to report higher NDI scores and HIT-6 scores. From a clinical point of view, it is important to evaluate the endurance of the neck muscles since this can be a predictor of the patient’s perceived disability, where subjects with lower resistance could present greater disability.
Due to the limitations inherent in this study, it is advisable to exercise caution when interpreting the data. It is not possible to extrapolate the results to men, highlighting the need for additional studies to determine whether the findings observed in this current study hold true for male participants.
Author Contributions
Conceptualization, L.C.-L., P.P.-A. and A.C.-U.; methodology, G.C., S.J.-d.-B., P.P.-A. and S.P.-G.; software, G.C. and P.P.-A.; validation, G.C., S.J.-d.-B., P.P.-A. and S.P.-G.; formal analysis, G.C. and P.P.-A.; investigation, G.C., S.J.-d.-B., P.P.-A. and S.P.-G.; resources, A.C.-U., S.C.-B., S.P.-G. and P.P.-A.; data curation, G.C. and P.P.-A.; writing—original draft preparation, S.C.-B., A.C.-U., G.C., S.J.-d.-B., P.P.-A., S.P.-G. and L.C.-L.; writing—review and editing, S.C.-B., A.C.-U., G.C., S.J.-d.-B., P.P.-A., S.P.-G. and L.C.-L.; supervision, S.C.-B., A.C.-U., G.C., S.J.-d.-B., P.P.-A., S.P.-G. and L.C.-L.; project administration, L.C.-L., S.C.-B. and A.C.-U. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The ethical approval for this study was obtained from the Research Ethics Committee of Aragón (CEICA: PI21/357, 30 August 2021).
Informed Consent Statement
All subjects participating in the study provided informed consent. Written consent has been acquired from the patient(s) for the publication of this paper.
Data Availability Statement
The data analyzed in this study are incorporated within this published article. For reasonable requests, the dataset can be obtained from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Cieza, A. Rehabilitation the Health Strategy of the 21st Century, Really? Arch. Phys. Med. Rehabil. 2019, 100, 2212–2214. [Google Scholar] [CrossRef]
- Buckinx, F.; Rolland, Y.; Reginster, J.Y.; Ricour, C.; Petermans, J.; Bruyère, O. Burden of frailty in the elderly population: Perspectives for a public health challenge. Arch. Public Health 2015, 73, 19. [Google Scholar] [CrossRef]
- Prablek, M.; Gadot, R.; Xu, D.S.; Ropper, A.E. Neck Pain. Neurol. Clin. 2023, 41, 77–85. [Google Scholar] [CrossRef]
- Verhagen, A.P. Physiotherapy management of neck pain. J. Physiother. 2021, 67, 5–11. [Google Scholar] [CrossRef]
- Shin, D.W.; Shin JIl Koyanagi, A.; Jacob, L.; Smith, L.; Lee, H.; Chang, Y.; Song, T.J. Global, regional, and national neck pain burden in the general population, 1990–2019: An analysis of the global burden of disease study 2019. Front. Neurol. 2022, 13, 955367. [Google Scholar] [CrossRef]
- Kazeminasab, S.; Nejadghaderi, S.A.; Amiri, P.; Pourfathi, H.; Araj-Khodaei, M.; Sullman, M.J.M.; Kolahi, A.-A.; Safiri, S. Neck pain: Global epidemiology, trends and risk factors. BMC Musculoskelet. Disord. 2022, 23, 26. [Google Scholar] [CrossRef]
- Palacios-Ceña, D.; Albaladejo-Vicente, R.; Hernández-Barrera, V.; Lima-Florencio, L.; Fernández-de-las-Peñas, C.; Jimenez-Garcia, R.; López-de-Andrés, A.; de Miguel-Diez, J.; Perez-Farinos, N. Female Gender Is Associated with a Higher Prevalence of Chronic Neck Pain, Chronic Low Back Pain, and Migraine: Results of the Spanish National Health Survey, 2017. Pain Med. 2021, 22, 382–395. [Google Scholar] [CrossRef]
- Gross, A.R. Physician-Delivered Injection Therapies for Mechanical Neck Disorders: A Systematic Review Update (Non-Oral, Non-Intravenous Pharmacological Interventions for Neck Pain). Open Orthop. J. 2013, 7, 562–581. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fandim, J.V.; Nitzsche, R.; Michaleff, Z.A.; Pena Costa, L.O.; Saragiotto, B. The contemporary management of neck pain in adults. Pain Manag. 2021, 11, 75–87. [Google Scholar] [CrossRef]
- Sanmugananthan, P.; Burkitt, J.J.; Campbell, D.; Cheema, N.; Murphy, B.A.; Yielder, P. The impact of subclinical neck pain on goal-directed upper limb movement in the horizontal plane. Exp. Brain Res. 2022, 240, 1911–1919. [Google Scholar] [CrossRef]
- Vernon, H. Introduction to Cervical Outcomes Measures: State of the Art. J. Manip. Physiol. Ther. 2008, 31, 489. [Google Scholar] [CrossRef]
- Côté, P.; Wong, J.J.; Sutton, D.; Shearer, H.M.; Mior, S.; Randhawa, K.; Ameis, A.; Carroll, L.J.; Nordin, M.; Yu, H.; et al. Management of neck pain and associated disorders: A clinical practice guideline from the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Eur. Spine J. 2016, 25, 2000–2022. [Google Scholar] [CrossRef]
- Wah, S.W.; Chatchawan, U.; Chatprem, T.; Puntumetakul, R. Prevalence of Static Balance Impairment and Associated Factors of University Student Smartphone Users with Subclinical Neck Pain: Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 10723. [Google Scholar] [CrossRef] [PubMed]
- Blanpied, P.R.; Gross, A.R.; Elliott, J.M.; Devaney, L.L.; Clewley, D.; Walton, D.M.; Sparks, C.; Robertson, E.K. Clinical practice guidelines linked to the international classification of functioning, disability and health from the orthopaedic section of the American physical therapy association. J. Orthop. Sports Phys. Ther. 2017, 47, A1–A83. [Google Scholar] [CrossRef] [PubMed]
- Stenneberg, M.S.; Rood, M.; de Bie, R.; Schmitt, M.A.; Cattrysse, E.; Scholten-Peeters, G.G. To What Degree Does Active Cervical Range of Motion Differ Between Patients with Neck Pain, Patients with Whiplash, and Those Without Neck Pain? A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2017, 98, 1407–1434. [Google Scholar] [CrossRef]
- Hurwitz, E.L.; Randhawa, K.; Yu, H.; Côté, P.; Haldeman, S. The Global Spine Care Initiative: A summary of the global burden of low back and neck pain studies. Eur. Spine J. 2018, 27, 796–801. [Google Scholar] [CrossRef] [PubMed]
- Kahlaee, A.H.; Rezasoltani, A.; Ghamkhar, L. Is the clinical cervical extensor endurance test capable of differentiating the local and global muscles? Spine J. 2017, 17, 913–921. [Google Scholar] [CrossRef]
- Ginszt, M.; Szkutnik, J.; Zieliński, G.; Bakalczuk, M.; Stodółkiewicz, M.; Litko-Rola, M.; Ginszt, A.; Rahnama, M.; Majcher, P. Cervical Myofascial Pain Is Associated with an Imbalance of Masticatory Muscle Activity. Int. J. Environ. Res. Public Health 2022, 19, 1577. [Google Scholar] [CrossRef]
- Treleaven, J.; Takasaki, H. Characteristics of visual disturbances reported by subjects with neck pain. Man. Ther. 2014, 19, 203–207. [Google Scholar] [CrossRef]
- Subbarayalu, A.V.; Ameer, M.A. Relationships among head posture, pain intensity, disability and deep cervical flexor muscle performance in subjects with postural neck pain. J. Taibah Univ. Med. Sci. 2017, 12, 541–547. [Google Scholar] [CrossRef]
- Rani, B.; Paul, A.; Chauhan, A.; Pradhan, P.; Dhillon, M.S. Is Neck Pain Related to Sagittal Head and Neck Posture?: A Systematic Review and Meta-analysis. Indian J. Orthop. 2023, 57, 371–403. [Google Scholar] [CrossRef]
- Wang, D.M.; Li, C.; Hatchard, N.; Chang Chien, G.C.; Alm, J. Lower trapezius muscle function in people with and without shoulder and neck pain: A systematic review. J. Osteopath. Med. 2023, 123, 73–89. [Google Scholar] [CrossRef] [PubMed]
- Shahidi, B.; Curran-Everett, D.; Maluf, K.S. Psychosocial, Physical, and Neurophysiological Risk Factors for Chronic Neck Pain: A Prospective Inception Cohort Study. J. Pain 2015, 16, 1288–1299. [Google Scholar] [CrossRef] [PubMed]
- Kocur, P.; Wilski, M.; Lewandowski, J.; Łochyński, D. Female Office Workers with Moderate Neck Pain Have Increased Anterior Positioning of the Cervical Spine and Stiffness of Upper Trapezius Myofascial Tissue in Sitting Posture. PM&R 2019, 11, 476–482. [Google Scholar] [CrossRef]
- Mahmoud, N.F.; Hassan, K.A.; Abdelmajeed, S.F.; Moustafa, I.M.; Silva, A.G. The Relationship Between Forward Head Posture and Neck Pain: A Systematic Review and Meta-Analysis. Curr. Rev. Musculoskelet. Med. 2019, 12, 562–577. [Google Scholar] [CrossRef]
- De Pauw, R.; Coppieters, I.; Kregel, J.; De Meulemeester, K.; Danneels, L.; Cagnie, B. Does muscle morphology change in chronic neck pain patients?—A systematic review. Man. Ther. 2016, 22, 42–49. [Google Scholar] [CrossRef]
- Peng, Q.; Zhang, Y.; Yang, S.; Meng, B.; Chen, H.; Liu, X.; Zhao, W.; Hu, M.; Zhang, L.; Tao, Y. Morphologic Changes of Cervical Musculature in Relation to Chronic Nonspecific Neck Pain: A Systematic Review and Meta-Analysis. World Neurosurg. 2022, 168, 79–88. [Google Scholar] [CrossRef]
- Fernández-De-Las-Peñas, C.; Albert-Sanchís, J.C.; Buil, M.; Benitez, J.C.; Alburquerque-Sendín, F. Cross-sectional area of cervical multifidus muscle in females with chronic bilateral neck pain compared to controls. J. Orthop. Sports Phys. Ther. 2008, 38, 175–180. [Google Scholar] [CrossRef]
- Abolfotouh, S.M.; Alnori, O.; Choma, T.; Moore, D.; Abolfotouh, M.A. Epidemiology of Work-Related Neck Pain Among Spine Surgeons. Glob. Spine J. 2022. ahead of print. [Google Scholar] [CrossRef]
- Lemeunier, N.; da Silva-Oolup, S.; Olesen, K.; Shearer, H.; Carroll, L.J.; Brady, O.; Côté, E.; Stern, P.; Tuff, T.; Suri-Chilana, M.; et al. Reliability and validity of self-reported questionnaires to measure pain and disability in adults with neck pain and its associated disorders: Part 3—A systematic review from the CADRE Collaboration. Eur. Spine J. 2019, 28, 1156–1179. [Google Scholar] [CrossRef]
- Zabihhosseinian, M.; Holmes, M.W.R.; Howarth, S.; Ferguson, B.; Murphy, B. Neck muscle fatigue differentially alters scapular and humeral kinematics during humeral elevation in subclinical neck pain participants versus healthy controls. J. Electromyogr. Kinesiol. 2017, 33, 73–82. [Google Scholar] [CrossRef]
- Zabihhosseinian, M.; Holmes, M.W.R.; Ferguson, B.; Murphy, B. Neck muscle fatigue alters the cervical flexion relaxation ratio in sub-clinical neck pain patients. Clin. Biomech. 2015, 30, 397–404. [Google Scholar] [CrossRef]
- Misailidou, V.; Malliou, P.; Beneka, A.; Karagiannidis, A.; Godolias, G. Assessment of patients with neck pain: A review of definitions, selection criteria, and measurement tools. J. Chiropr. Med. 2010, 9, 49–59. [Google Scholar] [CrossRef]
- Lourenço, A.S.; Lameiras, C.; Silva, A.G. Neck Flexor and Extensor Muscle Endurance in Subclinical Neck Pain: Intrarater Reliability, Standard Error of Measurement, Minimal Detectable Change, and Comparison with Asymptomatic Participants in a University Student Population. J. Manip. Physiol. Ther. 2016, 39, 427–433. [Google Scholar] [CrossRef]
- Buyukturan, B.; Guclu-Gunduz, A.; Buyukturan, O.; Dadali, Y.; Bilgin, S.; Kurt, E.E. Cervical stability training with and without core stability training for patients with cervical disc herniation: A randomized, single-blind study. Eur. J. Pain 2017, 21, 1678–1687. [Google Scholar] [CrossRef]
- Kang, D.Y. Deep cervical flexor training with a pressure biofeedback unit is an effective method for maintaining neck mobility and muscular endurance in college students with forward head posture. J. Phys. Ther. Sci. 2015, 27, 3207–3210. [Google Scholar] [CrossRef]
- Beinert, K.; Taube, W. The Effect of Balance Training on Cervical Sensorimotor Function and Neck Pain. J. Mot. Behav. 2013, 45, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Gupta, B.D. Effect of Deep Cervical Flexor Training vs. Conventional Isometric Training on Forward Head Posture, Pain, Neck Disability Index in Dentists Suffering from Chronic Neck Pain. J. Clin. Diagn. Res. 2013, 7, 2261. [Google Scholar] [CrossRef] [PubMed]
- Falla, D.; Lindstrøm, R.; Rechter, L.; Boudreau, S.; Petzke, F. Effectiveness of an 8-week exercise programme on pain and specificity of neck muscle activity in patients with chronic neck pain: A randomized controlled study. Eur. J. Pain. 2013, 17, 1517–1528. [Google Scholar] [CrossRef] [PubMed]
- Alpayci, M.; İlter, S. Isometric Exercise for the Cervical Extensors Can Help Restore Physiological Lordosis and Reduce Neck Pain. Am. J. Phys. Med. Rehabil. 2017, 96, 621–626. [Google Scholar] [CrossRef]
- Cleland, J.A.; Fritz, J.M.; Whitman, J.M.; Palmer, J.A. The Reliability and Construct Validity of the Neck Disability Index and Patient Specific Functional Scale in Patients with Cervical Radiculopathy. Spine 2006, 31, 598–602. [Google Scholar] [CrossRef] [PubMed]
- Alfonso Andrade Ortega, J.; Damián Delgado Martínez, A.; Almécija Ruiz, R. Validación de una versión española del Índice de Discapacidad Cervical. Med. Clin. 2008, 130, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, G.F.; Chaves, T.C.; Gonçalves, M.C.; Florencio, L.L.; Braz, C.A.; Dach, F.; de Las Peñas, C.F.; Bevilaqua-Grossi, D. Comparison between Neck Pain Disability and Cervical Range of Motion in Patients with Episodic and Chronic Migraine: A Cross-Sectional Study. J. Manip. Physiol. Ther. 2014, 37, 641–646. [Google Scholar] [CrossRef]
- Escalona-Marfil, C.; Coda, A.; Ruiz-Moreno, J.; Riu-Gispert, L.M.; Gironès, X. Validation of an Electronic Visual Analog Scale mHealth Tool for Acute Pain Assessment: Prospective Cross-Sectional Study. J. Med. Internet Res. 2020, 22, e13468. [Google Scholar] [CrossRef]
- Castien, R.F.; Blankenstein, A.H.; Windt DA van der Dekker, J. Minimal clinically important change on the Headache Impact Test-6 questionnaire in patients with chronic tension-type headache. Cephalalgia 2012, 32, 710–714. [Google Scholar] [CrossRef]
- Martin, M.; Blaisdell, B.; Kwong, J.W.; Bjorner, J.B. The Short-Form Headache Impact Test (HIT-6) was psychometrically equivalent in nine languages. J. Clin. Epidemiol. 2004, 57, 1271–1278. [Google Scholar] [CrossRef] [PubMed]
- Cleland, J.A.; Childs, J.D.; Fritz, J.M.; Whitman, J.M. Interrater Reliability of the History and Physical Examination in Patients with Mechanical Neck Pain. Arch. Phys. Med. Rehabil. 2006, 87, 1388–1395. [Google Scholar] [CrossRef]
- Domenech, M.A.; Sizer, P.S.; Dedrick, G.S.; McGalliard, M.K.; Brismee, J.-M. The Deep Neck Flexor Endurance Test: Normative Data Scores in Healthy Adults. PM&R 2011, 3, 105–110. [Google Scholar] [CrossRef]
- Jarman, N.F.; Brooks, T.; James, C.R.; Hooper, T.; Wilhelm, M.; Brismée, J.M.; Domenech, M.A.; Kotara, S.J.; Sizer, P.S. Deep Neck Flexor Endurance in the Adolescent and Young Adult: Normative Data and Associated Attributes. PM&R 2017, 9, 969–975. [Google Scholar] [CrossRef]
- Dimitriadis, Z.; Kapreli, E.; Strimpakos, N.; Oldham, J. Reliability of the chin tuck neck flexion test for assessing endurance of short neck flexors in healthy individuals. Physiother. Theory Pract. 2015, 31, 299–302. [Google Scholar] [CrossRef]
- Lee, H.; Nicholson, L.L.; Adams, R.D. Neck Muscle Endurance, Self-Report, and Range of Motion Data from Subjects with Treated and Untreated Neck Pain. J. Manip. Physiol. Ther. 2005, 28, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Amiri-Arimi, S.; Bandpei, M.; Rezasoltani, A.; Javanshir, K.; Biglarian, A. Measurement of cervical multifidus and longus colli muscle dimensions in patients with cervical radiculopathy and healthy controls using ultrasonography: A reliability study. PM&R 2019, 11, 236–242. [Google Scholar] [CrossRef]
- Ghamkhar, L.; Kahlaee, A.H. Are Ultrasonographic Measures of Cervical Flexor Muscles Correlated with Flexion Endurance in Chronic Neck Pain and Asymptomatic Participants? Am. J. Phys. Med. Rehabil. 2017, 96, 874–880. [Google Scholar] [CrossRef]
- Cagnie, B.; Derese, E.; Vandamme, L.; Verstraete, K.; Cambier, D.; Danneels, L. Validity and reliability of ultrasonography for the longus colli in asymptomatic subjects. Man. Ther. 2009, 14, 421–426. [Google Scholar] [CrossRef]
- Javanshir, K.; Mohseni-Bandpei, M.A.; Rezasoltani, A.; Amiri, M.; Rahgozar, M. Ultrasonography of longus colli muscle: A reliability study on healthy subjects and patients with chronic neck pain. J. Bodyw. Mov. Ther. 2011, 15, 50–56. [Google Scholar] [CrossRef]
- Moghadam, R.E.; Rahnama, L.; Karimi, N.; Amiri, M.; Rahnama, M. An ultrasonographic investigation of deep neck flexor muscles cross-sectional area in forward and normal head posture. J. Bodyw. Mov. Ther. 2018, 22, 643–647. [Google Scholar] [CrossRef]
- Kristjansson, E. Reliability of ultrasonography for the cervical multifidus muscle in asymptomatic and symptomatic subjects. Man. Ther. 2004, 9, 83–88. [Google Scholar] [CrossRef]
- Lee, J.-P.; Tseng, W.-Y.I.; Shau, Y.-W.; Wang, C.-L.; Wang, H.-K.; Wang, S.-F. Measurement of segmental cervical multifidus contraction by ultrasonography in asymptomatic adults. Man. Ther. 2007, 12, 286–294. [Google Scholar] [CrossRef]
- Hopkins, W.G.; Marshall, S.W.; Batterham, A.M.; Hanin, J. Progressive statistics for studies in sports medicine and exercise science. Med. Sci. Sports Exerc. 2009, 41, 3–12. [Google Scholar] [CrossRef]
- Villanueva-Ruiz, I.; Falla, D.; Lascurain-Aguirrebeña, I. Effectiveness of Specific Neck Exercise for Nonspecific Neck Pain; Usefulness of Strategies for Patient Selection and Tailored Exercise-A Systematic Review with Meta-Analysis. Phys. Ther. 2022, 102, pzab259. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).