Clinical and Kinematic Outcomes Based on Bone Graft Utilization for Salvage First Metatarsophalangeal Arthrodesis: A Systematic Review
Abstract
:1. Introduction
2. Methodology
2.1. Study Creation
2.2. Eligibility Criteria
2.3. Study Definitions
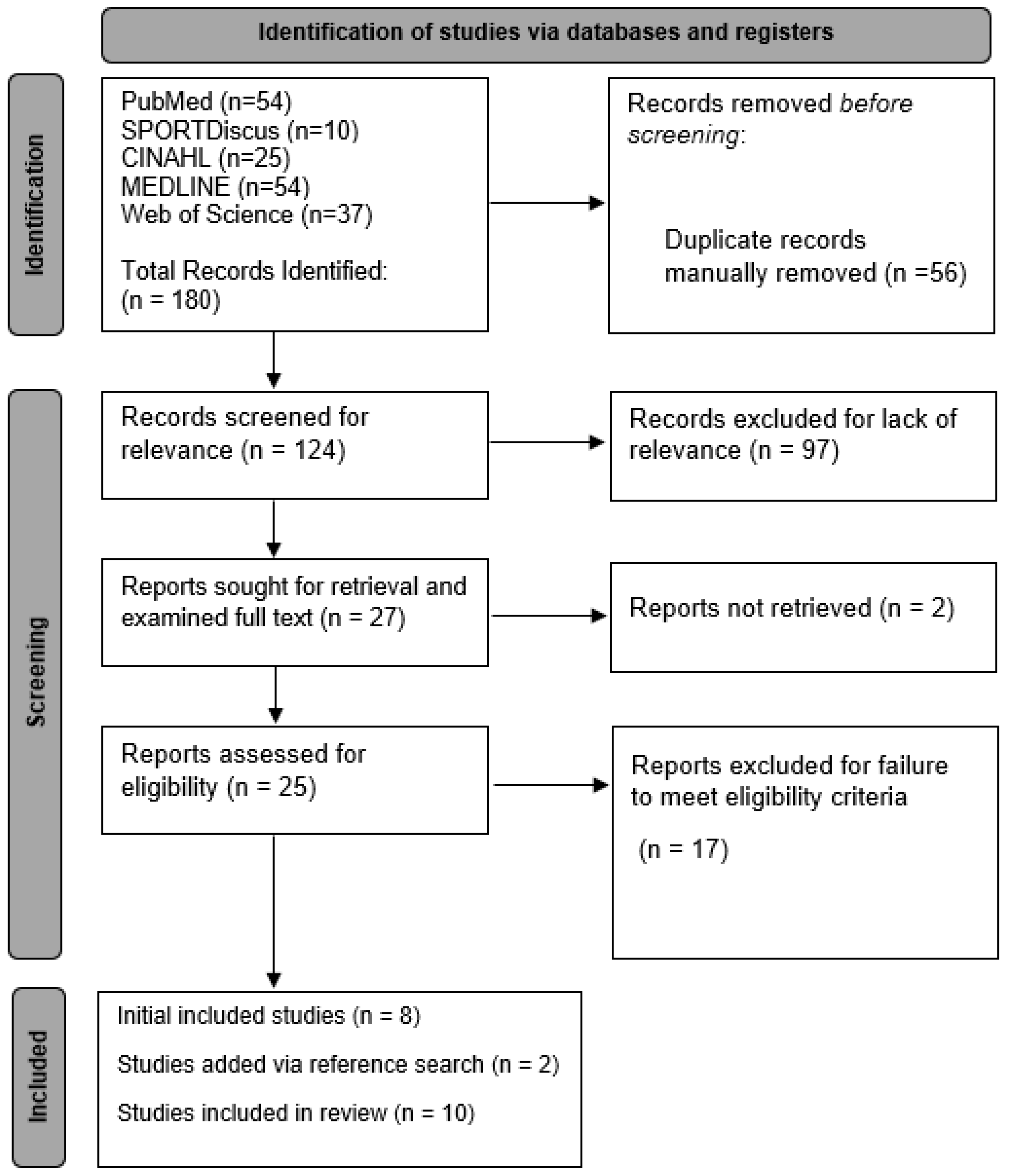
2.4. Article Selection Process
2.5. Data Extraction
2.6. Article Quality Grading
2.7. Certainty Assessment
2.8. Statistical Analysis
3. Results
3.1. Search Results
3.2. Study Quality Grading
3.3. Patient Demographics
3.4. Clinical and Radiographic Outcomes
3.5. Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Giza, E.; Sullivan, M.; Ocel, D.; Lundeen, G.; Mitchell, M.; Frizzell, L. First Metatarsophalangeal Hemiarthroplasty for Hallux Rigidus. Int. Orthop. 2010, 34, 1193. [Google Scholar] [CrossRef] [PubMed]
- Giza, E.; Sullivan, M.R. First Metatarsophalangeal Hemiarthroplasty for Grade III and IV Hallux Rigidus. Tech. Foot Ankle Surg. 2005, 4, 10–17. [Google Scholar] [CrossRef]
- Gross, C.E.; Hsu, A.R.; Lin, J.; Holmes, G.B.; Lee, S. Revision MTP Arthrodesis for Failed MTP Arthroplasty. Foot Ankle Spec. 2013, 6, 471–478. [Google Scholar] [CrossRef]
- Kumar, S.; Pradhan, R.; Rosenfeld, P.F. First Metatarsophalangeal Arthrodesis Using a Dorsal Plate and a Compression Screw. Foot Ankle Int. 2010, 31, 797–801. [Google Scholar] [CrossRef]
- Womack, J.W.; Ishikawa, S.N. First Metatarsophalangeal Arthrodesis. Foot Ankle Clin. 2009, 14, 43–50. [Google Scholar] [CrossRef]
- Singh, B.; Draeger, R.; Del Gaizo, D.J.; Parekh, S.G. Changes in Length of the First Ray with Two Different First MTP Fusion Techniques: A Cadaveric Study. Foot Ankle Int. 2008, 29, 722–725. [Google Scholar] [CrossRef]
- Schuh, R.; Trnka, H.J. First Metatarsophalangeal Arthrodesis for Severe Bone Loss. Foot Ankle Clin. 2011, 16, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Tóth, K.; Huszanyik, I.; Kellermann, P.; Boda, K.; Róde, L. The Effect of First Ray Shortening in the Development of Metatarsalgia in the Second through Fourth Rays after Metatarsal Osteotomy. Foot Ankle Int. 2007, 28, 60–63. [Google Scholar] [CrossRef]
- Lintz, F.; Welck, M.; Bernasconi, A.; Thornton, J.; Cullen, N.P.; Singh, D.; Goldberg, A. 3D Biometrics for Hindfoot Alignment Using Weightbearing CT. Foot Ankle Int. 2017, 38, 684–689. [Google Scholar] [CrossRef]
- Zhang, J.Z.; Lintz, F.; Bernasconi, A.; Zhang, S. 3D Biometrics for Hindfoot Alignment Using Weightbearing Computed Tomography. Foot Ankle Int. 2019, 40, 720–726. [Google Scholar] [CrossRef]
- Auch, E.; Barbachan Mansur, N.S.; Alexandre Alves, T.; Cychosz, C.; Lintz, F.; Godoy-Santos, A.L.; Baumfeld, D.S.; de Cesar Netto, C. Distal Tibiofibular Syndesmotic Widening in Progressive Collapsing Foot Deformity. Foot Ankle Int. 2021, 42, 768–775. [Google Scholar] [CrossRef]
- De Cesar Netto, C.; Bernasconi, A.; Roberts, L.; Pontin, P.A.; Lintz, F.; Saito, G.H.; Roney, A.; Elliott, A.; O’Malley, M. Foot Alignment in Symptomatic National Basketball Association Players Using Weightbearing Cone Beam Computed Tomography. Orthop. J. Sports Med. 2019, 7, 6081. [Google Scholar] [CrossRef]
- Geng, X.; Shi, J.; Chen, W.; Ma, X.; Wang, X.; Zhang, C.; Chen, L. Impact of First Metatarsal Shortening on Forefoot Loading Pattern: A Finite Element Model Study. BMC Musculoskelet. Disord. 2019, 20, 625. [Google Scholar] [CrossRef] [PubMed]
- McAlister, J.E.; Hyer, C.F.; Black, T.E. Distraction First Metatarsophalangeal Arthrodesis with Tricortical Calcaneus Autograft. Foot Ankle Spec. 2016, 9, 522–526. [Google Scholar] [CrossRef]
- Mistry, H.; Metcalfe, A.; Colquitt, J.; Loveman, E.; Smith, N.A.; Royle, P.; Waugh, N. Autograft or Allograft for Reconstruction of Anterior Cruciate Ligament: A Health Economics Perspective. Knee Surg. Sport. Traumatol. Arthrosc. 2019, 27, 1782–1790. [Google Scholar] [CrossRef]
- Mao, D.W.; Zheng, C.; Amatullah, N.N.; Kam, C.; Kon Kam King, C. Salvage Arthrodesis for Failed First Metatarsophalangeal Joint Arthroplasty: A Network Meta-Analysis. Foot Ankle Surg. 2020, 26, 614–623. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a Web and Mobile App for Systematic Reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological Index for Non-Randomized Studies (Minors): Development and Validation of a New Instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef]
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falck-Ytter, Y.; Glasziou, P.; Debeer, H.; et al. GRADE Guidelines: 1. Introduction-GRADE Evidence Profiles and Summary of Findings Tables. J. Clin. Epidemiol. 2011, 64, 383–394. [Google Scholar] [CrossRef]
- Burke, J.; Shi, G.G.; Wilke, B.; Whalen, J.L. Allograft Interposition Bone Graft for First Metatarsal Phalangeal Arthrodesis: Salvage after Bone Loss and Shortening of the First Ray. Foot Ankle Orthop. 2021, 42, 969–975. [Google Scholar] [CrossRef] [PubMed]
- Hecht, P.J.; Gibbons, M.J.; Wapner, K.L.; Cooke, C.; Hoisington, S.A. Arthrodesis of the First Metatarsophalangeal Joint to Salvage Failed Silicone Implant Arthroplasty. Foot Ankle Int. 1997, 18, 383–390. [Google Scholar] [CrossRef] [PubMed]
- Usuelli, F.G.; Tamini, J.; Maccario, C.; Grassi, M.; Tan, E.W. Bone-Block Arthrodesis Procedure in Failures of First Metatarsophalangeal Joint Replacement. Foot Ankle Surg. 2017, 23, 163–167. [Google Scholar] [CrossRef] [PubMed]
- Bei, C.; Gross, C.E.; Adams, S.; Parekh, S.G. Dual Plating with Bone Block Arthrodesis of the First Metatarsophalangeal Joint: A Clinical Retrospective Review. Foot Ankle Surg. 2015, 21, 235–239. [Google Scholar] [CrossRef]
- Luk, P.C.; Johnson, J.E.; McCormick, J.J.; Klein, S.E. First Metatarsophalangeal Joint Arthrodesis Technique With Interposition Allograft Bone Block. Foot Ankle Int. 2015, 36, 936–943. [Google Scholar] [CrossRef]
- Malhotra, K.; Nunn, T.; Qamar, F.; Rao, V.; Shanker, J. Interposition Bone Block Arthrodesis for Revision Hallux Metatarsophalangeal Joint Surgery: A Case Series. Foot Ankle Int. 2015, 36, 556–564. [Google Scholar] [CrossRef]
- Myerson, M.S.; Schon, L.C.; McGuigan, F.X.; Oznur, A. Result of Arthrodesis of the Hallux Metatarsophalangeal Joint Using Bone Graft for Restoration of Length. Foot Ankle Int. 2000, 21, 297–306. [Google Scholar] [CrossRef]
- Malagelada, F.; Welck, M.J.; Clark, C. The Dowel Technique for First Metatarso-Phalangeal Joint Arthrodesis in Revision Surgery with Bone Loss. Foot Ankle Surg. 2018, 24, 224–228. [Google Scholar] [CrossRef] [PubMed]
- Brodsky, J.W.; Ptaszek, A.J.; Morris, S.G. Salvage First MTP Arthrodesis Utilizing ICBG: Clinical Evaluation and Outcome. Foot Ankle Int. 2000, 21, 290–296. [Google Scholar] [CrossRef]
- Nix, S.; Russell, T.; Vicenzino, B.; Smith, M. Validity and Reliability of Hallux Valgus Angle Measured on Digital Photographs. J. Orthop. Sport. Phys. Ther. 2012, 42, 642–648. [Google Scholar] [CrossRef]
| Author (Year) | Study Type | Total MINORS Score | Clearly Stated Aim | Inclusion of Consecutive Patients | Prospective Collection of Data | End Points Appropriate to Study Aim | Unbiased Assessment of Study End Point | Follow-up Period Appropriate to Study Aim | Less than 5% Lost to Follow up | Prospective Calculation of the Study Size |
|---|---|---|---|---|---|---|---|---|---|---|
| Burke (2021) [21] | Non-Comparative | 12 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 |
| Hecht (1997) [22] | Non-Comparative | 11 | 2 | 2 | 0 | 2 | 2 | 2 | 1 | 0 |
| Usuelli (2017) [23] | Non-Comparative | 12 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 |
| Bei (2015) [24] | Non-Comparative | 12 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 |
| Luk (2015) [25] | Non-Comparative | 12 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 |
| Malhotra (2015) [26] | Non-Comparative | 12 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 |
| Myerson (2000) [27] | Non-Comparative | 12 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 |
| Malagelada (2018) [28] | Non-Comparative | 12 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 |
| Gross (2013) [3] | Non-Comparative | 12 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 |
| Brodsky (2000) [29] | Non-Comparative | 12 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 |
| Author (Year) | Article Type | Patients (n) | Procedures (n) | Average Age | Bone Graft Information | Graft Group | Lengthening Information | Time before Salvage | Follow-Up (Months) |
|---|---|---|---|---|---|---|---|---|---|
| Burke (2021) [21] | Case Series | 36 | 38 | 59.3 (range: 33–80) | Patellar wedge bone allograft. Crushed cancellous used to fill holes as needed | Allograft | 9.5 mm (5–15). The preoperative minimum length of the proximal phalanx necessary to obtain adequate stability using 3 distal locking screws with the interposition graft was 17 mm | - | 38.4 (range: 12–120) |
| Hecht (1997) [22] | Case Series | 14 | 16 | 54 (range: 36–74) | 33% cancellous bone from metatarsal head, 67% used tricortical iliac crest autograft | Unclassified | Described a length ratio (first ray with respect to second toe) | 38 (range: 9–84) | 55 (range: 36–94) |
| Usuelli (2017) [23] | Retrospective | 12 | 12 | 58.4 (range: 25–77) | Autologous calcaneus bone graft (ipsilateral bone block fusion) | Foot and ankle autograft | Average size of block was 14.3 (range: 11–19) | 15 (range: 12–22) | 33.4 (range: 12–64) |
| Bei (2015) [24] | Retrospective | 8 | 11 | 61 ± 10.5 | Interpositional allograft | Allograft | Compared to contralateral foot. Subtracted 2 mm from MTP joint space. Mean of 1.1 mm of lengthening | - | 12.6 (range: 6–23) |
| Luk (2015) [25] | Retrospective | 15 | 15 | 57 (range: 31–68) | Interposition allograft bone block, used autograft from tibia and iliac crest to pack in the medullary cavity prior to placing the allograft bone | Unclassified | Lengthening was custom for each patient. Metatarsal head was reamed according to the degree of bone loss | - | 11.5 (range: 4.75–24.25) |
| Malhotra (2015) [26] | Case Series | 24 | 25 | 52.1 (range: 34–69) | Tricortical autograft | Non-foot and ankle autograft | Shortening of the first ray was determined via contralateral comparison. Measured the gap of the hallux during surgery by gently retracting. | - | 62 (range: 11–117) |
| Myerson (2000) [27] | Retrospective | 24 | 24 | 46.4 (range: 28–66) | Used structural autograft in 66% of patients and allograft from the tibial head was used in 33%. Used cancellous graft in cases with large holes to fill | Unclassified | Lengthening was specific to the patient. Looked for proper alignment and a graft that did not prevent wound closure. As long as the hallux was positioned at 15 degrees of dorsiflexion and 5–10 degrees of valgus with respect to the MT1, then it was considered good | 26.6 (range: 3–64) | 63 (range: 26–108) |
| Malagelada (2018) [28] | Retrospective | 8 | 8 | 60.5 (range: 45–80) | Bi-cortical autograft from iliac crest | Non-foot and ankle autograft | Measured based upon size of the graft required appropriate first ray. Additional 2 cm were harvested in order to leave room for structuring | - | 37.4 (range: 12–102) |
| Gross (2013) [3] | Retrospective | 11 | 12 | 56.9 ± 10.2 | Allograft or autograft. 5/12 were iliac, 1/12 were interpositional allograft from iliac, 1/12 were bone grafting with calcaneal autograft and bone putty. 4/12 were bone grafting with morselized metatarsal heads, and 1/12 had no graft | Unclassified | Defect size dependent | 80 (range: 8–252) | 33 (range: 4–144) |
| Brodsky (2000) [29] | Retrospective | 12 | 12 | 54 (range: 35–72) | Tri-cortical iliac autograft and cancellous graft for all cases | Non-foot and ankle autograft | Defect size dependent | - | - |
| Author (Year) | Procedures (n) | AOFAS Pre | AOFAS Post (Max 95) | Success Rate |
|---|---|---|---|---|
| Burke (2021) [21] | 38 | 43.5 | 77.2 | 94.70% |
| Hecht (1997) [22] | 16 | - | - | 80% for tricortical graft |
| Usuelli (2017) [23] | 12 | 50.7 (range: 38–75) | 73.8 (range: 60–90) | 75% |
| Bei (2015) [24] | 11 | 44.50 (range: 32–60) | 87.75 (range: 76–96) | 90.90% |
| Luk (2015) [25] | 15 | - | - | 87% |
| Malhotra (2015) [26] | 25 | - | - | 88% |
| Myerson (2000) [27] | 24 | 40 (range: 22–60) | 79 (range: 66–90) | 79% |
| Malagelada (2018) [28] | 8 | - | - | 87.50% |
| Gross (2013) [3] | 12 | 51.7 ± 13.1 | 74.9 ± 8.6 | 41.70% |
| Brodsky (2000) [29] | 12 | - | 70 (range: 52–82) | 91.70% |
| Author (Year) | Procedures (n) | Length Restoration (mm) | Preoperative IMA | Postoperative IMA | Preoperative HV Angle | Postoperative HV Angle | Preoperative DFA | Postoperative DFA |
|---|---|---|---|---|---|---|---|---|
| Burke (2021) [21] | 38 | 9.5 (range: 5–15) | - | - | - | - | - | - |
| Hecht (1997) [22] | 16 | length ratio shortened from 1.17° (1.02–1.30) pre to 1.14° (1.06–1.21) | 5.5 (−2–10) | 7.3 (−1–11) | - | - | 22.1 (8.5–64) | 15.2 (5–40) |
| Usuelli (2017) [23] | 12 | length of first ray average decreased from 10.4 cm to 10.3 cm | 9.5 (6.4–14.2) | 8.4 (4.8–13.1) | 19.7 (3.6–45.8) | 14.3 (7.3–29.7) | - | - |
| Bei (2015) [24] | 11 | 1.1 ± 4.5 | - | - | - | - | - | - |
| Luk (2015) [25] | 15 | increased from mean of 10 cm to 10.6 cm | 10.5 (4–17) | 10.2 (4–15) | 12.2 (−28–30) | 12.7 (4–22) | 33.9 (15–71) | 25.6 (16–40) |
| Malhotra (2015) [26] | 25 | 4.4 (range: 0–8) | - | - | - | - | - | - |
| Myerson (2000) [27] | 24 | 13 (range: 0–29) | - | - | - | - | - | - |
| Malagelada (2018) [28] | 8 | 4.6 (range: 2.7) | - | - | 21.4 (2.6) | 11.6 (3.2) | - | - |
| Gross (2013) [3] | 12 | - | - | - | - | - | 29.1 (14.3) | - |
| Brodsky (2000) [29] | 12 | - | 9.1 (5–12) | 7.2 (5–10) | 9.5 (−8–30) | 14.1 (5–23) | 35 (20–60) | 22 (13–38) |
| Author (Year) | Procedures (n) | Graft Group | Nonunion Rate | Complications |
|---|---|---|---|---|
| Burke (2021) [21] | 38 | Allograft | 5% | Pain (n = 1, 2.6%), nonunion (n = 2, 5.3%), |
| Hecht (1997) [22] | 16 | Unclassified | - | Neuroma (n =1, 6.3%) |
| Usuelli (2017) [23] | 12 | Foot and ankle autograft | 25% | Nonunion (n = 3, 25%), |
| Bei (2015) [24] | 11 | Allograft | 9.09% | Superficial wound (n = 1, 9.09%), painful nonunion (n = 1, 9.09%) |
| Luk (2015) [25] | 15 | Unclassified | 6.67% | Nonunion (n = 1, 6.6%), painless arthritis, (n = 1, 6.6%), stress fracture (n = 1, 6.6%) |
| Malhotra (2015) [26] | 25 | Non-foot and ankle autograft | - | Nonunion (n = 3, 12.0%), painful neuroma (n = 2, 8%), pain at graft site (n = 1, 4%), hardware removal (n = 3, 12%), discomfort (n = 6, 33%) |
| Myerson (2000) [27] | 24 | Unclassified | 21% | Nonunion (n = 5, 21%), deep infection (n = 1, 4.2%), superficial wound infection (n = 2. 8.3%), pain syndrome (n = 1, 4.2%) |
| Malagelada (2018) [28] | 8 | Non-foot and ankle autograft | - | Removal due to discomfort (n = 1, 13%), pain (n = 1, 13%), numbness (n = 1, 13%) |
| Gross (2013) [3] | 12 | Unclassified | - | Painful nonunion (n = 2, 16.7%), prominent plate (n = 2, 16.7%), graft site irritation (n = 1, 8.35%) |
| Brodsky (2000) [29] | 12 | Non-foot and ankle autograft | 8.33% | Discomfort (n = 1, 8.25%), sesamoid discomfort (n = 4, 33%), painless nonunion (n = 1, 8.25%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Talaski, G.M.; Baumann, A.N.; Anastasio, A.T.; Walley, K.C.; de Cesar Netto, C. Clinical and Kinematic Outcomes Based on Bone Graft Utilization for Salvage First Metatarsophalangeal Arthrodesis: A Systematic Review. Appl. Sci. 2023, 13, 9436. https://doi.org/10.3390/app13169436
Talaski GM, Baumann AN, Anastasio AT, Walley KC, de Cesar Netto C. Clinical and Kinematic Outcomes Based on Bone Graft Utilization for Salvage First Metatarsophalangeal Arthrodesis: A Systematic Review. Applied Sciences. 2023; 13(16):9436. https://doi.org/10.3390/app13169436
Chicago/Turabian StyleTalaski, Grayson M., Anthony N. Baumann, Albert T. Anastasio, Kempland C. Walley, and Cesar de Cesar Netto. 2023. "Clinical and Kinematic Outcomes Based on Bone Graft Utilization for Salvage First Metatarsophalangeal Arthrodesis: A Systematic Review" Applied Sciences 13, no. 16: 9436. https://doi.org/10.3390/app13169436
APA StyleTalaski, G. M., Baumann, A. N., Anastasio, A. T., Walley, K. C., & de Cesar Netto, C. (2023). Clinical and Kinematic Outcomes Based on Bone Graft Utilization for Salvage First Metatarsophalangeal Arthrodesis: A Systematic Review. Applied Sciences, 13(16), 9436. https://doi.org/10.3390/app13169436







