1. Introduction
Malocclusion is defined as an irregular teeth relationship compared to the accepted normal occlusion. According to the World Health Organization, it is one of the most common oral health diseases. It can affect normal individual daily functions that involve the facial area, including speaking, chewing, and swallowing, and can also have self-esteem impacts due to dentofacial appearance problems [
1,
2].
Teeth and skeletal relationships are based on Angle’s classification 3. Angle’s classification was based on the relationship of the maxillary to the mandibular teeth, with no reference to any skeletal structures [
3,
4]. Over the years, the classification has been modified, for diagnostic purposes, to facial structure classification as well [
4].
Fixation of malocclusion involves orthodontic treatment for the leveling and alignment of the teeth. However, successful treatment is based on the correct diagnosis, which leads to precise planning for necessary teeth movement. The treatment will execute the above diagnosis and planning steps [
5]. It was theorized that optimal facial esthetics is accomplished when teeth are straightened, and the occlusion is corrected to cephalometric X-ray optimal standards [
5,
6,
7].
The “envelope of discrepancy” indicates that teeth movement is limited. Using teeth movement along with growth modifications is limited to the active growth period. Sometimes, orthodontic treatment can camouflage malocclusion problems, but such treatment does not change the skeletal relationship in facial–bone discrepancies.
The camouflage treatment has been improved over time using temporary anchorage devices. However, these devices can present some adverse effects, such as of root injuries “(root injury during interradicular insertion is the most common complication associated with orthodontic miniscrews)” [
8].
Additionally, failure of miniscrews for orthodontic anchorage, analysis of risk factors correlated with the progressive susceptibility to failure or fracture, have been reported and studied [
9,
10].
Therefore, for patients with severe orthodontic problems, solely orthodontic treatment is insufficient, and these patients need combined orthodontic-surgical treatment [
11].
Class-III occlusion is a condition in which the mandibular first molar is positioned anterior to the maxillary molar. Skeletally, it can be defined as an underdeveloped maxilla relative to the mandible, overdeveloped mandible relative to the maxilla, or a combination of both [
11]. In such cases, it is essential to first diagnose the nature of the defect, whether the origin is dental-only or skeletal, and if skeletal, to decide the origin of the skeletal malocclusion.
One of the traditional ways to indicate a Class-III discrepancy is to diagnose anterior crossbite (CB) or a negative overjet (OJ). The diagnosis is based on clinical examination combined with lateral cephalometric analysis. Various indices on the cephalometric radiograph, such as Steiner’s and McNamara’s, facilitate the assessment of mandibular or maxillary deviation from the normal values relative to the base of the skull [
11,
12]. These demonstrate the severity of the malocclusion or skeletal discrepancy and help to decide the need for orthognathic surgery versus occlusion correction solely using functional devices [
13]. Orthognathic surgery is a treatment process involving orthodontics and maxillofacial surgery, and it is used to treat those dentofacial discrepancies outside the scope of conventional orthodontic treatment. Treatment may correct various underlying skeletal discrepancies, including severe Class-II or Class-III problems [
14]. When orthognathic surgery is indicated, the surgical treatment can be a mandibular setback, maxillary advancement, or a combination of both, respective to the patient’s complaint, clinical examination, study models, and facial cephalometric radiograph analysis findings [
15,
16].
The class-III facial structure usually demonstrates natural dental or dentoalveolar teeth compensation characteristics, expressed in the proclination of the maxillary incisors and the retroclination of mandibular incisors [
17]. These angles are measured by the upper teeth plane (U1) to FH and PP for the maxillary teeth (normal values are 113.6° ± 6.3° and 112° ± 6.45°, respectively, McNamara analysis) and lower teeth plane (L1) to MP for the mandibular teeth (normal values 90° ± 5°, Tweed’s analysis).
When considering orthognathic surgery for Class-III patients, the pre-surgical orthodontic treatment consists of decompensation of the teeth, which is the opposite of the compensation described, including the proclination of the lower anterior and retroclination of the upper anterior [
18,
19]. Decompensation should be planned with caution, as the pre-surgical orthodontic treatment plays a significant role in dictating the surgical movements’ magnitude.
Pre-operational measurements include, among other things, the effective maxillary and mandibular length (Co-Gn for mandible and Co-A point for maxilla) in order to calculate the maxilla–mandibular difference (the difference between the maxillary and the mandibular length) [
19]. Patients with skeletal Class-III usually demonstrate a high maxilla–mandibular difference; the more significant the difference, the higher the severity.
Therefore, the orthodontic-surgical treatment of Class-III deformities comprises orthodontic preparation, a surgical correction of the relationship of the jaws, and final orthodontic involvement for occlusal processing subsequent to recovery from the surgery. The pre-operational orthodontic preparation should be coordinated with the surgical plan so that normal occlusion is achieved upon the completion of the surgery. Incomplete or imperfect correction of the maxillary and mandibular incisors compensation may impact both the quality of the skeletal result and the quality of the final occlusion result of the surgery [
19,
20].
The current study aimed to check if the orthodontic decompensation amount is influenced and compromised by the maxillomandibular difference.
2. Materials and Methods
The Tel-Aviv University local institutional review board (IRB) approved the research. The retrospective study analyzed 50 consecutive cephalometric radiographs from a single private surgical practice (DMA) of skeletal Class-III deformity (prognathic) patients aged 20–35. Inclusion criteria were a pre-operation cephalometric radiograph performed after completion of orthodontic preparation (de-compensation) and 1–2 weeks prior to surgery; all of the patients underwent non-extraction orthodontic treatment. Exclusion criteria were syndromic patients, including cleft lip/palate.
The cephalometric analysis serves as the gold standard in evaluating soft and hard tissue prior to orthodontic treatment, as well as for the evaluation and planning of orthognathic surgery using a list of standard-specific structures and measurements [
16,
17]. Part of the points (landmarks) on the cephalometric radiograph includes [
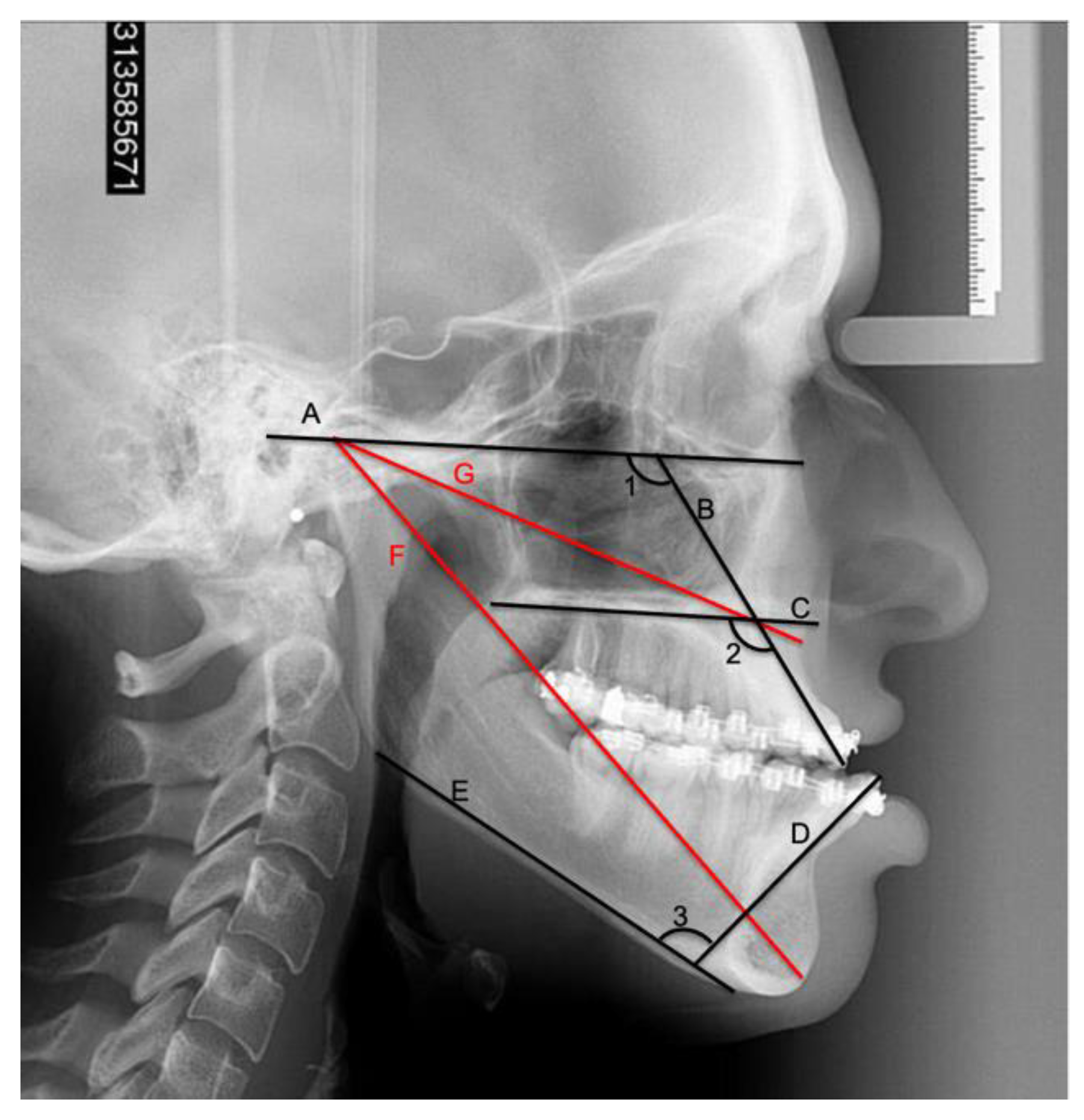
4]: A point (subnasal)—the most concave point of the maxilla; B point (supramental)—the most concave point on mandibular symphysis; N point (nasion)—the most anterior point on frontonasal suture; Or (orbitale)—the most inferior point on the margin of orbit; Po (porion)—the most superior point of outline of external auditory meatus; anterior nasal spine (ANS)—the anterior point on maxillary bone; posterior nasal spine (PNS)—posterior limit of bony palate or maxilla; condylion (Co)—the most posterior/superior point on the condyle of mandible; gnathion (Gn)—point located perpendicular on mandibular symphysis; gonion (Go)—the most posterior inferior point on the angle of the mandible.
Based on the anatomical landmarks, there are a few planes addressed on the radiograph: Frankfort horizontal plane (FH: Or–Po)—represents the habitual postural position of the head; the palatal plane (PP: ANS-PNS)—represents the plane of the maxilla; mandibular plane (MP: Go-Gn)—represents the lower border of the mandible; U1—upper incisor tooth plane, from the incisal edge to the root apex of the upper incisor tooth; L1—lower incisor tooth plane, from the incisal edge to the root apex of the lower incisor tooth.
Figure 1 shows the measurements performed on the cephalometric radiograph. The following lines were drawn and measured: Frankfort horizontal plane (FH), inferior mandibular plane (MP), palatal plane (PP), the upper incisal longitudinal axis (U1), lower incisor longitudinal axis (L1), overjet (OJ), mandibular length (CO-A), and maxillary length (CO-Gn). Measurements included the upper incisal to the Frankfort horizontal plane angle (U1 to Fh), the upper incisal to palatal plane angle (U1 to PP), the lower incisal to the mandibular plane angle (L1 to MP), the maxilla–mandibular difference (subtraction of maxillary length from the mandibular length in millimeters, Diff).
The Cephninja® Pro Version 5.02 (WA, UNITED STATES) application performed all angles and plane length measurements by calibrating the application ruler to the cephalometric radiograph and appointing the anatomical landmarks accordingly. The same examiner performed two independent measurements at two different times to check the measurements consistency.
The statistical analysis was performed using SPSS software version 25.0 (IBM, Armonk, NY, USA). Descriptive statistics were performed, followed by the Pearson correlation coefficient test in order to check for possible correlation between the maxilla–mandibular difference and the U1 to FH angle, U1 to PP angle, L1 to MP angle, and the OJ.
3. Results
Table 1 shows the average differences between the two separate variables’ measurements. The differences in the measurements were between 0.06 mm and 0.67 mm (jaw length, overjet, and maxilla–mandibular difference) and 0.79° to 1.02° degrees (for the angles measured). The differences were minor and clinically insignificant.
The descriptive data is shown in
Table 2. The average maxillary length was 75.24 mm and mandibular length was 108.60 mm. The maxilla–mandibular difference was 33.36 mm. The average U1 to FH angle was 122.53, U1 to PP was 119.15, L1 to MP was 90.45, and the OJ was (−3.56) mm.
Pearson correlation between maxilla–mandibular difference (diff) and measured variables (
Table 3) revealed a statistically significant correlation of maxilla–mandibular difference and U1 to FH angle (r = 0.254,
p = 0.037, sig < 0.05), U1 to PP angle (r = 0.447,
p < 0.001 sig < 0.05), and overjet (r = (−0.426),
p < 0.001 sig < 0.05). There was no statistical significance for Diff and L1 to MP angle (
p = 0.342). The associations are shown in
Table 2.
4. Discussion
Class-III dentofacial deformities are intermaxillary skeletal misalignments treated by orthognathic surgery [
11]. In 1980, Bell-Proffit-White conducted a study concerning blood supply to the down fractured maxilla and established the efficacy and safety of the surgical procedure. Other authors later defined and modified the surgical treatment in such cases. They showed how determining a surgical treatment plan (mandibular set-back, maxillary advancement, or a combination of both) is based on VTO, patient’s complaint, facial cephalometric radiographs analysis, and the model analysis [
15]. Since then, advances in surgical technics and instrumentation encouraged a global adoption of maxillary orthognathic surgery. The introduction of rigid internal fixation, oscillating and reciprocating micro-saws, piezo surgery, and distraction osteogenesis are all now an integral part of the maxillofacial armamentarium, contributing to the predictability, safety, and stability of the Le-fort osteotomy. CBCT-based computer imaging and prediction software also aids in achieving accurate treatment plans and more esthetic and accurate results. The importance of orthodontic treatment prior to the surgical procedure and the post-operative orthodontic treatment is crucial for achieving final optimal and stable occlusion [
21]. The preoperative orthodontic treatment consists of producing decompensation of the teeth for three major reasons: better position upon the alveolar bone, better periodontal condition, and sufficient negative overjet and proper inclination of the anterior teeth in order to create a mutual relationship between dentofacial occlusal and skeletal discrepancy. Proper decompensation facilitates the correction of inter-arch relationships at the time of surgery by optimizing the surgical movements. Thus, it contributes significantly to the overall aesthetic and functional outcome and long-term stability [
22,
23].
Part of the planning is performed by presurgical calculation of upper and lower incisors’ inclination relative to the facial planes according to obtained cephalometric values. Without adequate incisor decompensation surgical movement, the final skeletal position may be limited by the extent of the incisor overjet [
24].
We sought to retrospectively examine whether the preoperative inclination of upper and lower incisors in Cl-III patients just before surgery meets the requirements of proper de-compensation according to accepted cephalometric values. Furthermore, we tried to find whether achieving such an orthodontic position is affected by the severity of the deformity, as reflected by the value of maxilla–mandibular difference according to McNamara’s analysis. In our sample, we did not find a correlation between the maxilla–mandibular difference and L1 to MP. This implies that the decompensation of the lower anterior teeth is probably not (or less) influenced by the maxilla–mandibular difference. This finding is in accordance with a previous study that found decompensation to be more adequate in the mandibular arch than in the maxillary arch in Class-III surgical patients. Furthermore, the results showed better surgical correction in cases where the maxillary teeth were adequately decompensated [
25].
On the other hand, an interesting finding is that there is a significant positive correlation between maxilla–mandibular difference and immediate preoperative upper incisor proclination, i.e., U1 to FH or PP angle. This means that as the maxilla–mandibular difference increases (the higher the skeletal Class-III severity), the angle of the upper incisors is more pronounced, and the orthodontics could not achieve adequate decompensation as they should have done prior to surgery.
The patients in our study were treated by numerous orthodontists in private orthodontic practices. One might argue that treatment modalities and different levels of clinical experience have affected the outcome. However, this study design reflects the real clinical situation that the planning team of surgeons and the orthodontist have to cope with [
26]. Patients often get their orthodontics in the community from an orthodontist with limited experience in ortho-surgical preparation. Furthermore, Potts et al. reported no differences in treatment efficiency between experienced and novice clinicians [
27]. Therefore, the presented results are relevant to all practicing orthodontists.
Possible explanations for the unsatisfactory maxillary decompensation can be found in different studies. One study shows that the longitudinal axis of the root of the upper incisor is not always the same as the axis of the crown according to the cephalometric analysis, and therefore there is an angle between the crown and the root; this angle is more prominent in cases with a more lingually inclined crown. This angle between the crown root of the upper incisor is also more prominent in Class-III patients, a fact that causes great difficulty in identifying the appropriate longitudinal axis of the upper incisor [
25]. Another important argument is that decompensation (upright) of the lower incisors during pre-surgical orthodontic treatment increases the risk of periodontal defects, a fact that may be a limiting factor for the orthodontist to achieve optimal decompensation [
28]. Furthermore, we demonstrated in a previous work that cephalometric measurements may suffer from significant examiner-based bias, which is correlated to the severity of the dentofacial deformity [
29]. These findings should raise the question of whether decompensation is truly compromised as we found in the present study, at least regarding the maxillary incisors in the more severe Cl-III cases, or maybe it is merely misdiagnosed as such because of limited and biased interpretation of the cephalometric imaging.
It is very important to mention some of the limitation of our study: first, the technology we used is very dependent on the surgeon or the doctor who performs the cephalometric analysis, and secondly, the technology is very limited because of the 2D limitations.
As imaging technology improves, there is a strong tendency toward virtual surgical planning relying upon 3D cone-beam computed tomography (CBCT) with intra-oral dental scans (e.g., Dolphin 3D; Dolphin Imaging 11.9 Premium, Chatsworth, CA, USA) for generating a surgical splint, or splint fewer surgeries using commercial software for example (3D Systems Healthcare, Littleton, CO, USA) and Maxilim (Medicim, Mechelen, Belgium) that can help to facilitate the process of virtual surgical planning (VSP), rather than the conventional 2D planning using cephalometric analysis. Such preparations and planning are already frequently involved in orthodontic-surgical treatments, with promising, more accurate results [
30].
Today much more orthodontists are combining the CBCT and intraoral scanners to collect and acquire as much accurate data as possible, which will help to facilitate the planning process; for example, IPS CaseDesigner
® (KLS Martin Manufacturing, Jacksonville, FL, USA) and OrthoAnalyzer™ (3Shape, Copenhagen, Denmark), which demonstrated high accuracy when compared to the gold standard. [
31,
32].
Lastly, there has been a significant surge in the number of studies exploring the potential applications of AI and ML in orthodontics. The research has primarily focused on diagnosis and treatment planning, growth and development assessment, and automated anatomic landmark detection and analysis, with more advanced AI (artificial intelligence) and ML (machine learning) [
33].
5. Conclusions
The challenge of achieving adequate decompensation in the maxillary incisors of severe Class-III patients compared to mandibular incisors is a multifactorial issue whose precise etiology remains elusive. Factors that potentially contribute to the complexity of the process include the extent of dental compensations, skeletal discrepancies, dental or skeletal asymmetries, and the interplay between orthodontic forces and surrounding soft tissues.
The maxilla–mandibular difference should be used as a good indicator for the orthodontics to take it into account for the decompensation of the upper incisors; this should affect the treatment plan and take into consideration the extraction of premolars or any other suitable treatment.
With the advent of novel artificial intelligence (AI) and machine learning (ML) software coupled with highly accurate 3D data acquisition, there is the potential for an enhanced understanding of the limitations imposed by Class-III severity. This understanding could develop novel and innovative solutions to the challenges associated with maxillary incisor decompensation. By providing detailed information about the intricate interplay between teeth, jaws, and surrounding soft tissues, these technological advancements could support the development of individualized and precise treatment plans that optimize patient outcomes.