Muscle Pain Sensitivity and Prevalence of Temporomandibular Disorders in Patients with Narcolepsy with Cataplexy: A Controlled Cohort Study
Abstract
1. Introduction
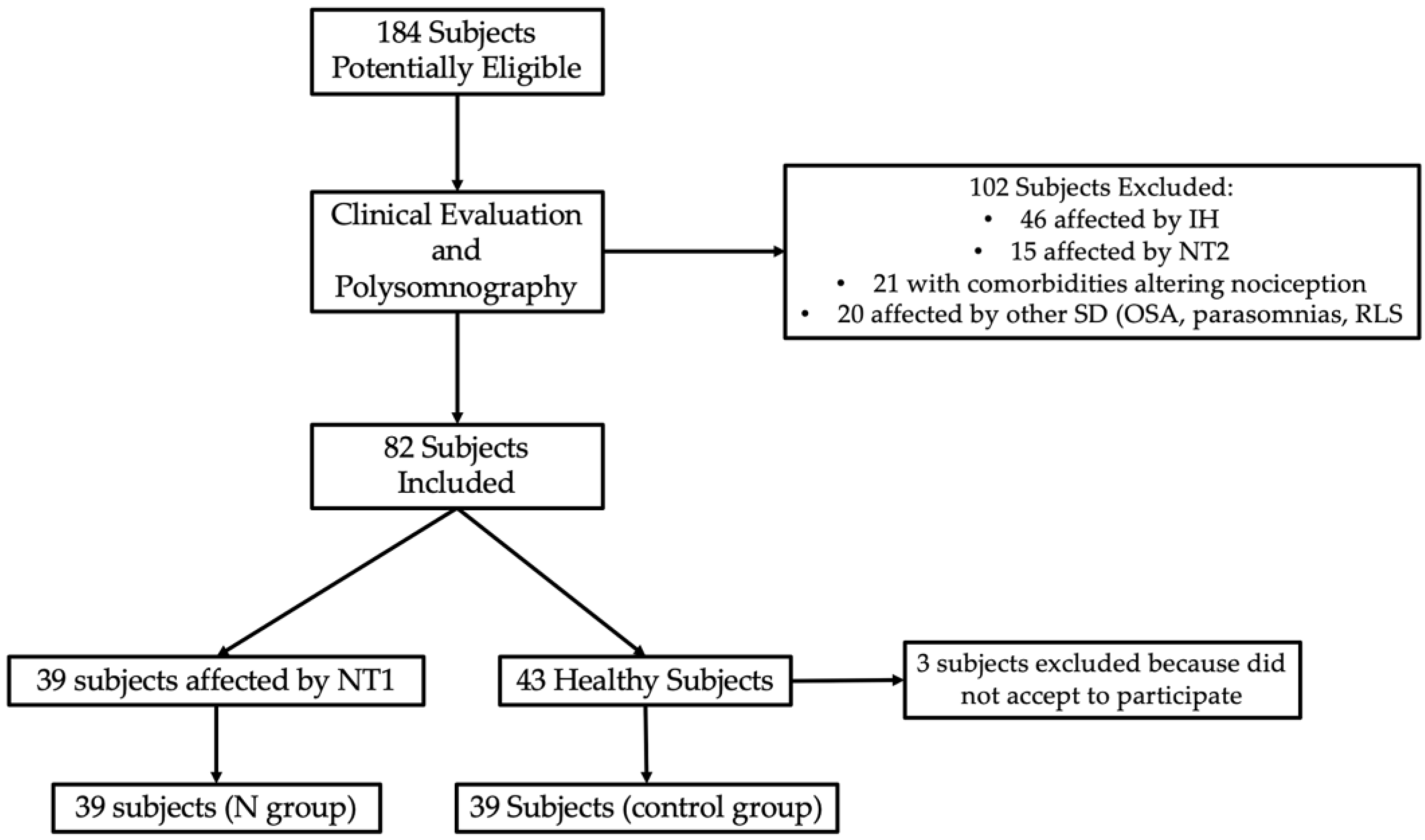
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Demarco, G.J.; Baghdoyan, H.A.; Lydic, R. Differential Cholinergic Activation of G Proteins in Rat and Mouse Brainstem: Relevance for Sleep and Nociception. J. Comp. Neurol. 2003, 457, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Burgos, I.; Richter, L.; Klein, T.; Fiebich, B.; Feige, B.; Lieb, K.; Voderholzer, U.; Riemann, D. Increased Nocturnal Interleukin-6 Excretion in Patients with Primary Insomnia: A Pilot Study. Brain Behav. Immun. 2006, 20, 246–253. [Google Scholar] [CrossRef] [PubMed]
- Vgontzas, A.N.; Papanicolaou, D.A.; Bixler, E.O.; Lotsikas, A.; Zachman, K.; Kales, A.; Prolo, P.; Wong, M.L.; Licinio, J.; Gold, P.W.; et al. Circadian Interleukin-6 Secretion and Quantity and Depth of Sleep. J. Clin. Endocrinol. Metab. 1999, 84, 2603–2607. [Google Scholar] [CrossRef] [PubMed]
- Finan, P.H.; Goodin, B.R.; Smith, M.T. The Association of Sleep and Pain: An Update and a Path Forward. J. Pain 2013, 14, 1539–1552. [Google Scholar] [CrossRef]
- Staffe, A.T.; Bech, M.W.; Clemmensen, S.L.K.; Nielsen, H.T.; Larsen, D.B.; Petersen, K.K. Total Sleep Deprivation Increases Pain Sensitivity, Impairs Conditioned Pain Modulation and Facilitates Temporal Summation of Pain in Healthy Participants. PLoS ONE 2019, 14, e0225849. [Google Scholar] [CrossRef]
- Waliszewska-Prosół, M.; Nowakowska-Kotas, M.; Chojdak-łukasiewicz, J.; Budrewicz, S. Migraine and Sleep-An Unexplained Association? Int. J. Mol. Sci. 2021, 22, 5539. [Google Scholar] [CrossRef]
- Bhaskar, S.; Hemavathy, D.; Prasad, S. Prevalence of Chronic Insomnia in Adult Patients and Its Correlation with Medical Comorbidities. J. Fam. Med. Prim. Care 2016, 5, 780. [Google Scholar] [CrossRef]
- Benoliel, R.; Sharav, Y. Chronic Orofacial Pain. Curr. Pain Headache Rep. 2010, 14, 33–40. [Google Scholar] [CrossRef]
- Lipton, J.A.; Ship, J.A.; Larach-Robinson, D. Estimated Prevalence and Distribution of Reported Orofacial Pain in the United States. J. Am. Dent. Assoc. 1993, 124, 115–121. [Google Scholar] [CrossRef]
- Sanders, A.E.; Akinkugbe, A.A.; Bair, E.; Fillingim, R.B.; Greenspan, J.D.; Ohrbach, R.; Dubner, R.; Maixner, W.; Slade, G.D. Subjective Sleep Quality Deteriorates Before Development of Painful Temporomandibular Disorder. J. Pain 2016, 17, 669–677. [Google Scholar] [CrossRef]
- Natu, V.P.; Yap, A.U.J.; Su, M.H.; Irfan Ali, N.M.; Ansari, A. Temporomandibular Disorder Symptoms and Their Association with Quality of Life, Emotional States and Sleep Quality in South-East Asian Youths. J. Oral Rehabil. 2018, 45, 756–763. [Google Scholar] [CrossRef]
- Rener-Sitar, K.; John, M.T.; Pusalavidyasagar, S.S.; Bandyopadhyay, D.; Schiffman, E.L. Sleep Quality in Temporomandibular Disorder Cases. Sleep Med. 2016, 25, 105–112. [Google Scholar] [CrossRef]
- Schmitter, M.; Kares-Vrincianu, A.; Kares, H.; Bermejo, J.L.; Schindler, H.J. Sleep-Associated Aspects of Myofascial Pain in the Orofacial Area among Temporomandibular Disorder Patients and Controls. Sleep Med. 2015, 16, 1056–1061. [Google Scholar] [CrossRef]
- Smith, M.T.; Wickwire, E.M.; Grace, E.G.; Edwards, R.R.; Buenaver, L.F.; Peterson, S.; Klick, B.; Haythornthwaite, J.A. Sleep Disorders and Their Association with Laboratory Pain Sensitivity in Temporomandibular Joint Disorder. Sleep 2009, 32, 779–790. [Google Scholar] [CrossRef]
- Terzi, R.; Yılmaz, Z. Evaluation of Pain Sensitivity by Tender Point Counts and Myalgic Score in Patients with and without Obstructive Sleep Apnea Syndrome. Int. J. Rheum. Dis. 2017, 20, 340–345. [Google Scholar] [CrossRef]
- Edwards, R.R.; Quartana, P.J.; Allen, R.P.; Greenbaum, S.; Earley, C.J.; Smith, M.T. Alterations in Pain Responses in Treated and Untreated Patients with Restless Legs Syndrome: Associations with Sleep Disruption. Sleep Med. 2011, 12, 603–609. [Google Scholar] [CrossRef] [PubMed]
- Winkelman, J.W.; Gagnon, A.; Clair, A.G. Sensory Symptoms in Restless Legs Syndrome: The Enigma of Pain. Sleep Med. 2013, 14, 934–942. [Google Scholar] [CrossRef] [PubMed]
- Topaloglu-Ak, A.; Kurtulmus, H.; Basa, S.; Sabuncuoglu, O. Can Sleeping Habits Be Associated with Sleep Bruxism, Temporomandibular Disorders and Dental Caries among Children? Dent. Med. Probl. 2022, 59, 517–522. [Google Scholar] [CrossRef] [PubMed]
- Wieczorek, T.; Wieckiewicz, M.; Smardz, J.; Wojakowska, A.; Michalek-Zrabkowska, M.; Mazur, G.; Martynowicz, H. Sleep Structure in Sleep Bruxism: A Polysomnographic Study Including Bruxism Activity Phenotypes across Sleep Stages. J. Sleep Res. 2020, 29, e13028. [Google Scholar] [CrossRef]
- Sowa, N.A. Idiopathic Hypersomnia and Hypersomnolence Disorder: A Systematic Review of the Literature. Psychosomatics 2016, 57, 152–164. [Google Scholar] [CrossRef]
- Khatami, R.; Luca, G.; Baumann, C.R.; Bassetti, C.L.; Bruni, O.; Canellas, F.; Dauvilliers, Y.; Del Rio-Villegas, R.; Feketeova, E.; Ferri, R.; et al. The European Narcolepsy Network (EU-NN) Database. J. Sleep Res. 2016, 25, 356–364. [Google Scholar] [CrossRef]
- American Academy of Sleep Medicine. The International Classification of Sleep Disorders, (ICSD-3): Diagnostic and Coding Manual, 3rd ed.; American Academy of Sleep Medicine: Westchester, IL, USA, 2014. [Google Scholar]
- Dauvilliers, Y.; Arnulf, I.; Mignot, E. Narcolepsy with Cataplexy. Lancet 2007, 369, 499–511. [Google Scholar] [CrossRef]
- Dauvilliers, Y.; Billiard, M.; Montplaisir, J. Clinical Aspects and Pathophysiology of Narcolepsy. Clin. Neurophysiol. 2003, 114, 2000–2017. [Google Scholar] [CrossRef]
- Barateau, L.; Pizza, F.; Plazzi, G.; Dauvilliers, Y. Narcolepsy. J. Sleep Res. 2022, 31, e13631. [Google Scholar] [CrossRef]
- Dauvilliers, Y.; Siegel, J.M.; Lopez, R.; Torontali, Z.A.; Peever, J.H. Cataplexy—Clinical Aspects, Pathophysiology and Management Strategy. Nat. Rev. Neurol. 2014, 10, 386–395. [Google Scholar] [CrossRef]
- Bassetti, C.L.A.; Adamantidis, A.; Burdakov, D.; Han, F.; Gay, S.; Kallweit, U.; Khatami, R.; Koning, F.; Kornum, B.R.; Lammers, G.J.; et al. Narcolepsy—Clinical Spectrum, Aetiopathophysiology, Diagnosis and Treatment. Nat. Rev. Neurol. 2019, 15, 519–539. [Google Scholar] [CrossRef] [PubMed]
- Dauvilliers, Y.; Paquereau, J.; Bastuji, H.; Drouot, X.; Weil, J.S.; Viot-Blanc, V. Psychological Health in Central Hypersomnias: The French Harmony Study. J. Neurol. Neurosurg. Psychiatry 2009, 80, 636–641. [Google Scholar] [CrossRef] [PubMed]
- Schuld, A.; Hebebrand, J.; Geller, F.; Pollmacher, T. Increased Body-Mass Index in Patients with Narcolepsy. Lancet 2000, 355, 1274–1275. [Google Scholar] [CrossRef] [PubMed]
- Evers, S. Migraine and Idiopathic Narcolepsy—A Case-Control Study. Cephalalgia 2003, 23, 786–789. [Google Scholar] [CrossRef]
- Dahmen, N.; Kasten, M.; Wieczorek, S.; Gencik, M.; Epplen, J.T.; Ullrich, B. Increased Frequency of Migraine in Narcoleptic Patients: A Confirmatory Study. Cephalalgia 2003, 23, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Dauvilliers, Y.; Bayard, S.; Shneerson, J.M.; Plazzi, G.; Myers, A.J.; Garcia-Borreguero, D. High Pain Frequency in Narcolepsy with Cataplexy. Sleep Med. 2011, 12, 572–577. [Google Scholar] [CrossRef] [PubMed]
- Spielberger, S.; Högl, B.; Mitterling, T.; Frauscher, B.; Löscher, W.N. Pain Perception in Narcolepsy with Cataplexy Patients. Sleep Med. 2015, 16, 310. [Google Scholar] [CrossRef] [PubMed]
- Razavi, B.M.; Hosseinzadeh, H. A Review of the Role of Orexin System in Pain Modulation. Biomed. Pharmacother. 2017, 90, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Zhou, W.; Cheung, K.; Kyu, S.; Wang, L.; Guan, Z.; Kurien, P.A.; Bickler, P.E.; Jan, L.Y. Activation of Orexin System Facilitates Anesthesia Emergence and Pain Control. Proc. Natl. Acad. Sci. USA 2018, 115, E10740–E10747. [Google Scholar] [CrossRef]
- Kang, X.; Tang, H.; Liu, Y.; Yuan, Y.; Wang, M. Research Progress on the Mechanism of Orexin in Pain Regulation in Different Brain Regions. Open Life Sci. 2021, 16, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ren, R.; Yang, L.; Zhang, H.; Shi, Y.; Sanford, L.D.; Tang, X. Polysomnographic Nighttime Features of Narcolepsy: A Systematic Review and Meta-Analysis. Sleep Med. Rev. 2021, 58, 101488. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Vignatelli, L.; Plazzi, G.; Barbato, A.; Ferini-Strambi, L.; Manni, R.; Pompei, F.; D’Alessandro, R. Italian Version of the Epworth Sleepiness Scale: External Validity. Neurol. Sci. 2003, 23, 295–300. [Google Scholar] [CrossRef]
- Kendzerska, T.B.; Smith, P.M.; Brignardello-Petersen, R.; Leung, R.S.; Tomlinson, G.A. Evaluation of the Measurement Properties of the Epworth Sleepiness Scale: A Systematic Review. Sleep Med. Rev. 2014, 18, 321–331. [Google Scholar] [CrossRef]
- Curcio, G.; Tempesta, D.; Scarlata, S.; Marzano, C.; Moroni, F.; Rossini, P.M.; Ferrara, M.; De Gennaro, L. Validity of the Italian Version of the Pittsburgh Sleep Quality Index (PSQI). Neurol. Sci. 2013, 34, 511–519. [Google Scholar] [CrossRef]
- Mollayeva, T.; Thurairajah, P.; Burton, K.; Mollayeva, S.; Shapiro, C.M.; Colantonio, A. The Pittsburgh Sleep Quality Index as a Screening Tool for Sleep Dysfunction in Clinical and Non-Clinical Samples: A Systematic Review and Meta-Analysis. Sleep Med. Rev. 2016, 25, 52–73. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, Y.M.; Schiffman, E.; Gordon, S.M.; Seago, B.; Truelove, E.L.; Slade, G.; Ohrbach, R. Development of a Brief and Effective Temporomandibular Disorder Pain Screening Questionnaire: Reliability and Validity. J. Am. Dent. Assoc. 2011, 142, 1183–1191. [Google Scholar] [CrossRef]
- Von Korff, M.; Ormel, J.; Keefe, F.J.; Dworkin, S.F. Grading the Severity of Chronic Pain. Pain 1992, 50, 133–149. [Google Scholar] [CrossRef]
- Ohrbach, R.; Larsson, P.; List, T. The Jaw Functional Limitation Scale: Development, Reliability and Validity of 8-Item and 20-Item Versions. J. Orofac. Pain 2008, 22, 219–230. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Löwe, B.; Decker, O.; Müller, S.; Brähler, E.; Schellberg, D.; Herzog, W.; Herzberg, P.Y. Validation and Standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the General Population. Med. Care 2008, 46, 266–274. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-15: Validity of a New Measure for Evaluating the Severity of Somatic Symptoms. Psychosom. Med. 2002, 64, 258–266. [Google Scholar] [CrossRef]
- Markiewicz, M.R.; Ohrbach, R.; McCall, W.D. Oral Behaviors Checklist: Reliability of Performance in Targeted Waking-State Behaviors. J. Orofac. Pain 2006, 20, 306–316. [Google Scholar]
- Lautenbacher, S.; Rollman, G.B.; McCain, G.A. Multi-Method Assessment of Experimental and Clinical Pain in Patients with Fibromyalgia. Pain 1994, 59, 45–53. [Google Scholar] [CrossRef]
- Fischer, A.A. Pressure Algometry over Normal Muscles. Standard Values, Validity and Reproducibility of Pressure Threshold. Pain 1987, 30, 115–126. [Google Scholar] [CrossRef] [PubMed]
- Ohrbach, R.; Gale, E.N. Pressure Pain Thresholds in Normal Muscles: Reliability, Measurement Effects and Topographic Differences. Pain 1989, 37, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Jensen, K.; Andersen, H.O.; Olesen, J.; Lindblom, U. Pressure-Pain Threshold in Human Temporal Region. Evaluation of a New Pressure Algometer. Pain 1986, 25, 313–323. [Google Scholar] [CrossRef]
- Pizza, F.; Vandi, S.; Iloti, M.; Franceschini, C.; Liguori, R.; Mignot, E.; Plazzi, G. Nocturnal Sleep Dynamics Identify Narcolepsy Type 1. Sleep 2015, 38, 1277. [Google Scholar] [CrossRef]
- Cohen, A.; Mandrekar, J.; Louis, E.K.S.; Silber, M.H.; Kotagal, S. Comorbidities in a Community Sample of Narcolepsy. Sleep Med. 2018, 43, 14–18. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Liu, Z.Z.; Yang, Y.; Jia, C.X. Associations of Frequent Pain Symptoms with Excessive Daytime Sleepiness in Adolescents: A Longitudinal Study. J. Clin. Sleep Med. 2021, 17, 2415–2423. [Google Scholar] [CrossRef] [PubMed]
- Chhangani, B.S.; Roehrs, T.A.; Harris, E.J.; Hyde, M.; Drake, C.; Hudgel, D.W.; Roth, T. Pain Sensitivity in Sleepy Pain-Free Normals. Sleep 2009, 32, 1011–1017. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, K.; Miyamoto, M.; Miyamoto, T.; Inoue, Y.; Matsui, K.; Nishida, S.; Hayashida, K.; Usui, A.; Ueki, Y.; Nakamura, M.; et al. The Prevalence and Characteristics of Primary Headache and Dream-Enacting Behaviour in Japanese Patients with Narcolepsy or Idiopathic Hypersomnia: A Multi-Centre Cross-Sectional Study. PLoS ONE 2015, 10, e0139229. [Google Scholar] [CrossRef]
- Mombelli, S.; Ricordeau, F.; Gillard, L.; Lecca, R.; Vidal, T.; Pereira, B.; Beudin, P.; Vitello, N.; Bastuji, H.; Peter-Derex, L.; et al. Psychobehavioural Profile in Narcolepsy Type 1 with and without REM Sleep Behaviour Disorder. J. Sleep Res. 2023, 2023, e13925. [Google Scholar] [CrossRef]
- Pizza, F.; Magnani, M.; Indrio, C.; Plazzi, G. The Hypocretin System and Psychiatric Disorders. Curr. Psychiatry Rep. 2014, 16, 433. [Google Scholar] [CrossRef]
- Brundin, L.; Björkqvist, M.; Petersén, Å.; Träskman-Bendz, L. Reduced Orexin Levels in the Cerebrospinal Fluid of Suicidal Patients with Major Depressive Disorder. Eur. Neuropsychopharmacol. 2007, 17, 573–579. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Lobbezoo, F. Sleep Bruxism and Temporomandibular Disorders: A Scoping Review of the Literature. J. Dent. 2021, 111, 103711. [Google Scholar] [CrossRef] [PubMed]
- Bracci, A.; Lobbezoo, F.; Häggman-Henrikson, B.; Colonna, A.; Nykänen, L.; Pollis, M.; Ahlberg, J.; Manfredini, D. Current Knowledge and Future Perspectives on Awake Bruxism Assessment: Expert Consensus Recommendations. J. Clin. Med. 2022, 11, 5083. [Google Scholar] [CrossRef] [PubMed]
| Variables | Group N (n = 39) | Group C (n = 39) | p= |
|---|---|---|---|
| Age (mean ± SD) | 38.69 ± 10.89 | 43.13 ± 12.07 | 0.092 |
| Gender | 16 ♂ (41.0%) 23 ♀ (59.0%) | 22 ♂ (56.4%) 17 ♀ (43.6%) | 0.174 |
| ESS | 14.05 ± 4.80 | 8.09 ± 5.27 | 0.001 * |
| PSQI | 7.68 ± 2.57 | 6.75 ± 4.19 | 0.267 |
| TMD pain screener over cut-off | 10.2% (n = 4) | 28.2% (n = 11) | 0.021 * |
| TIB (min) | 484.99 ± 66.89 | 506.79 ± 66.47 | 0.377 |
| LS (min) | 5.15 ± 7.59 | 20.14 ± 19.27 | 0.001 * |
| LR (min) | 27.13 ± 37.88 | 81.90 ± 14.68 | 0.001 * |
| TST (min) | 413.21 ± 53.21 | 396.35 ± 63.58 | 0.406 |
| WASO (min) | 66.63 ± 47.20 | 90.30 ± 77.88 | 0.254 |
| %TST N1 | 9.91 ± 6.78 | 3.23 ± 1.57 | 0.004 * |
| %TST N2 | 39.28 ± 8.07 | 42.56 ± 9.70 | 0.297 |
| %TST N3 | 29.46 ± 12.54 | 29.88 ± 10.51 | 0.926 |
| %TST REM | 21.35 ± 5.62 | 24.33 ± 3.05 | 0.120 |
| AHI | 2.21 ± 3.22 | 0.96 ± 1.76 | 0.256 |
| Muscles | Group N (n = 39) | Group C (n = 39) | t= | p= |
|---|---|---|---|---|
| Anterior Temporal | 2.53 ± 0.80 | 2.43 ± 0.76 | −0.753 | 0.442 |
| Middle Temporal | 2.97 ± 1.04 | 2.89 ± 1.00 | −0.437 | 0.634 |
| Posterior Temporal | 3.35 ± 1.07 | 3.24 ± 0.99 | −0.360 | 0.500 |
| Masseter | 2.07 ± 0.71 | 1.98 ± 0.63 | 0.571 | 0.392 |
| Sternocleidomastoid | 1.60 ± 0.59 | 1.58 ± 0.51 | −1.150 | 0.788 |
| Occipital | 2.95 ± 1.23 | 2.96 ± 1.22 | 0.364 | 0.948 |
| Splenius capitis | 2.73 ± 1.02 | 2.18 ± 0.75 | −1.831 | 0.238 |
| Thenar | 4.65 ± 1.73 | 4.51 ± 1.67 | 0.403 | 0.606 |
| Group N (n = 39) | Group C (n = 39) | Χ2= | p= | |
|---|---|---|---|---|
| TMD | 28.2% (n = 11) | 38.5% (n = 15) | 0.923 | 0.337 |
| Muscle TMD | 20.5% (n = 8) | 23.1% (n = 9) | 0.075 | 0.784 |
| Articular TMD | 23.1% (n = 9) | 28.2% (n = 11) | 0.269 | 0.604 |
| Reported Headache | 38.5% (n = 15) | 30.8% (n = 12) | 0.510 | 0.475 |
| Pain on muscle palpation | 33.3% (n = 13) | 33.3% (n = 13) | 0.000 | 1.000 |
| Questionnaires | Group N (n = 39) | Group C (n = 39) | Χ2= | p= |
|---|---|---|---|---|
| GCPS 2.0 Chronic Orofacial Pain | 23.1% (n = 9) | 28.2% (n = 11) | 0.269 | 0.604 |
| JFLS-20 | 23.1% (n = 9) | 7.7% (n = 3) | 4.754 | 0.093 |
| PHQ-9 | 74.4% (n = 33) | 56.4% (n = 22) | 20.844 | 0.006 * |
| PHQ-15 | 69.2% (n = 27) | 66.7% (n = 26) | 0.059 | 0.808 |
| GAD-7 | 56.4% (n = 22) | 43.6% (n = 17) | 1.282 | 0.258 |
| OBC | 56.4% (n = 22) | 52.6% (n = 20) | 1.040 | 0.594 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bartolucci, M.L.; Incerti Parenti, S.; Pizza, F.; Maglioni, A.; Vandi, S.; Bortolotti, F.; Plazzi, G.; Alessandri-Bonetti, G. Muscle Pain Sensitivity and Prevalence of Temporomandibular Disorders in Patients with Narcolepsy with Cataplexy: A Controlled Cohort Study. Appl. Sci. 2023, 13, 6917. https://doi.org/10.3390/app13126917
Bartolucci ML, Incerti Parenti S, Pizza F, Maglioni A, Vandi S, Bortolotti F, Plazzi G, Alessandri-Bonetti G. Muscle Pain Sensitivity and Prevalence of Temporomandibular Disorders in Patients with Narcolepsy with Cataplexy: A Controlled Cohort Study. Applied Sciences. 2023; 13(12):6917. https://doi.org/10.3390/app13126917
Chicago/Turabian StyleBartolucci, Maria Lavinia, Serena Incerti Parenti, Fabio Pizza, Alessandro Maglioni, Stefano Vandi, Francesco Bortolotti, Giuseppe Plazzi, and Giulio Alessandri-Bonetti. 2023. "Muscle Pain Sensitivity and Prevalence of Temporomandibular Disorders in Patients with Narcolepsy with Cataplexy: A Controlled Cohort Study" Applied Sciences 13, no. 12: 6917. https://doi.org/10.3390/app13126917
APA StyleBartolucci, M. L., Incerti Parenti, S., Pizza, F., Maglioni, A., Vandi, S., Bortolotti, F., Plazzi, G., & Alessandri-Bonetti, G. (2023). Muscle Pain Sensitivity and Prevalence of Temporomandibular Disorders in Patients with Narcolepsy with Cataplexy: A Controlled Cohort Study. Applied Sciences, 13(12), 6917. https://doi.org/10.3390/app13126917








