Abstract
(1) Introduction: Deciduous traumatic dental injuries pose a serious global health concern. Root fractures show an incidence rate of approximately 2%; however, the literature is limited regarding the appropriate treatment and prognosis of affected teeth. This retrospective study aims to analyze the long-term outcomes of orthodontic splinting using brackets compared with composite resin-only splinting in two homogeneous samples affected by root fractures. The study also examines the onset and patterns of root resorption. (2) Methods: The first group included 25 patients with 27 deciduous upper incisors affected by root fracture; Group 2 consisted of 35 patients with 38 root fractures of maxillary deciduous teeth. The categorical data for both groups were analyzed using the chi-squared homogeneity test. Age groups were compared using the Mann–Whitney U test; p < 0.005 was considered statistically significant. (3) Results: In both groups, the male gender predominated similarly. In Group 1, early decidual loss occurred in 16% of cases, whereas in Group 2 it occurred in 51% of cases. Pulp canal obliteration was observed in 68% of deciduous teeth in Group 1, compared with 30% in Group 2. No complications affecting permanent teeth were noted in Group 1; in Group 2, 29% developed enamel dysplasia and 26% experienced delayed eruption, with statistically significant differences in these proportions. Apical fragment resorption was observed in 92% of cases in Group 1 and 30% in Group 2. (4) Conclusions: The treatment of deciduous tooth root fractures using orthodontic splints can yield significant benefits, such as reduction of early tooth loss. Furthermore, the study confirms that early resorption of the distal fragment of fractured roots is a common physiological phenomenon in primary teeth and typically occurs within a year following trauma.
1. Introduction
Primary dentition plays a crucial role both functionally (as it guides the eruption of permanent teeth) and aesthetically [1]. Dental emergencies and traumatic dental injuries (TDIs) are well-documented in the guidelines of the International Association of Dental Traumatology (IADT) [2,3,4]. Epidemiological studies consistently demonstrate a high incidence and prevalence of TDIs, accounting for approximately 50% of cases [2,5], as confirmed by a recent meta-analysis [5]. Consequently, TDIs pose a significant global health problem, particularly due to their potential long-term consequences on permanent teeth [6].
Furthermore, traumatic events in primary dentition, such as extrusive luxation trauma and root and alveolar fractures, can lead to occlusal interferences that require prompt treatment [3]. These traumatic events often result in tooth extraction, posing challenges for the eruption and alignment of future permanent teeth [7].
The primary maxillary central incisors are the teeth most frequently involved, with an incidence rate of up to 80% [8]. The most frequent primary TDIs are extrusion, intrusion (64%), and avulsions (92%) [9,10].
Additionally, there is a notable lack of studies on deciduous root fractures in the existing literature. Root fractures are relatively rare, with an incidence rate of approximately 2% [9]; they typically occur due to severe trauma in the crown area near the gum line or even in correspondence to the alveolar bone [10].
Intra-oral radiographic examination is crucial for accurate diagnosis, as it reveals root fractures as a line of horizontal radiolucency.
Fractures of the middle and apical third of the root are the most common.
The standard treatment involves splinting and occlusal stabilization [11,12,13,14]. According to Andreasen et al. (1998), conservative therapy has shown a good success rate, despite the challenges associated with performing splinting and limited cooperation from pediatric patients [15].
Long-term follow-up requires meticulous clinical and radiographic evaluations, particularly to monitor the onset and progression of root resorption, pulp necrosis (PN), and pulp canal obliteration (PCO). PCO is characterized by the gradual progressive obliteration of the canal walls, which is radiographically visible as a reduction of the endodontic space [16]. This retrospective study aims to analyze the outcomes of two homogeneous samples with deciduous root fractures to determine whether treatment with orthodontic splinting (utilizing orthodontic brackets and wires) compared with a control group treated only with composite fixation splinting to adjacent teeth yields a more favorable prognosis for the affected tooth and influences the onset and timing of resorption in the fractured root.
2. Materials and Methods
A retrospective observational study was conducted, analyzing the records of 60 patients with root fractures in primary dentition. The study included patients aged between 2 and 4 years of age who received treatment at the Dental Traumatology Center of the University of Cagliari (Italy) between 2012 and 2022. The treatments were performed by three equally qualified specialists (ES, NZ, and MSM), with equivalent clinical-diagnostic expertise. These specialists alternately provided acute treatment and subsequent follow-up care.
The initial basic study group (Group 1) initially included 37 patients, of whom 12 did not meet the inclusion criteria, resulting in a final sample size of 25 patients with root fractures in deciduous incisors, totaling 27 upper incisors with root fractures.
The control group (Group 2) comprised 35 patients, with a total of 38 fractures of maxillary primary teeth (Figure 1).
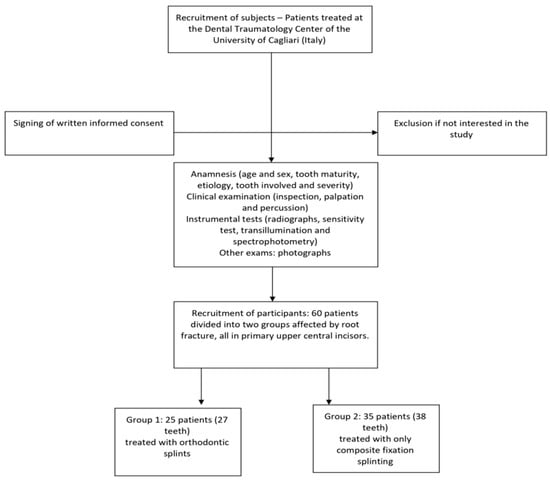
Figure 1.
The recruitment process leading to the final sample.
The most evident therapeutic difference between the two samples examined was the type of post-trauma splinting performed. In the first group, orthodontic splinting (wire and Bk) was performed, while, in the second group, the splinting was conducted solely in composite resin, allowing the evaluation of immediate complications and long-term outcomes.
The following inclusion criteria were applied:
- -
- Patients with at least one primary incisor presenting with root fracture, with or without compound vestibular cortex fracture;
- -
- Patients examined within 48 h of the dental trauma and whose data had been collected in accordance with the IADT guidelines of 2012, updated in 2020.
The exclusion criteria were as follows:
- -
- Patients with a history of previous traumatic dental injuries and/or carious lesions;
- -
- Patients who experienced additional traumatic dental injuries during the follow-up period;
- -
- Patients with ongoing interceptive and/or orthodontic therapy.
The selection process was based on clinical and radiographic findings, carried out independently by two equally qualified and experienced specialists who underwent appropriate training for approximately three months. These specialists were dentists who had graduated at least five years prior and who had been involved in pediatric dentistry and traumatology for a minimum of three years.
All selected cases were reviewed (with particular focus on radiographic data) by a third party with more experience, expertise, and decision-making authority. The level of agreement among these experts was assessed using the kappa test, which yielded a value of 0.68, indicating “moderate” agreement, according to Landis and Koch (1977) [17].
Any disagreements were resolved via discussions between all three reviewers.
2.1. Management of the Fractures
The data collection form followed a standardized protocol and included the recording of the patient’s age, sex, etiology of the trauma, the affected tooth, and the type and severity of the lesion (Table 1).

Table 1.
Evaluated parameters of the study.
Furthermore, the data collection form also included a clinical description of the lesion, information on responses to pulp sensitivity tests, radiographic and photographic investigations, details of the treatment performed, and information on long-term follow-up.
Prior to commencing treatment, written consent for clinical and therapeutic investigations was obtained from the parents or legal guardians of all patients in accordance with the protocols of the Helsinki Charter [18] and its subsequent updates.
The data were already present in the databases of the dental clinics and were anonymized with an alphanumeric code at the time of collection, as mandated by the national guidelines of the National Health and Medical Research Council (NHMRC) for retrospective clinical studies. The study complied with the “Human Experimentation Statement” and received approval from the medical direction board of the Surgical Science Department of the University of Cagliari (2020/13742).
The evaluation of each patient began with a comprehensive history taking, followed by intra- and extra-oral examination and palpation of the injured area. The clinical dental examination included tests of range of mobility, percussion sound and tenderness, response to pulp tests, and periapical or occlusal graphical X-ray examinations. During subsequent checks, the possible development of root resorption in the middle and apical third was evaluated within 6, 9, and 12 months, along with modification of the chroma of the tooth crown, onset of PCO, inflammation, and/or inflammatory complications.
Pulp sensitivity was tested using a cold spray with a maximum temperature of −26 °C. It should be noted that a negative response immediately after the trauma did not reliably indicate pulpal necrosis. In fact, additional evidence, such as radiographic and coronal dyschromic changes, were considered to determine pulpal status.
Radiographs, including periapical and standardized occlusal views, were taken using 3 × 4 mm Kodak film; changes in tooth color were also taken into account.
The classification of root fractures was based on the location of the fracture line, categorized as follows [19]: fracture of the apical third, middle third, or coronal third.
The types of splinting were classified, based on eventual physiological mobility, as:
- Rigid splinting: does not allow any physiological mobility of the tooth and may create conditions for complications of an ankylotic nature.
- Non-rigid/semi-rigid/flexible splinting: allows for physiological functional mobility of the traumatized tooth, promoting healing of the periodontal ligament with a consequent reduction of the risk of ankylosis.
In Group 1, splinting with orthodontic brackets was used, requiring the use of orthodontic brackets and wires (Figure 2a,b).
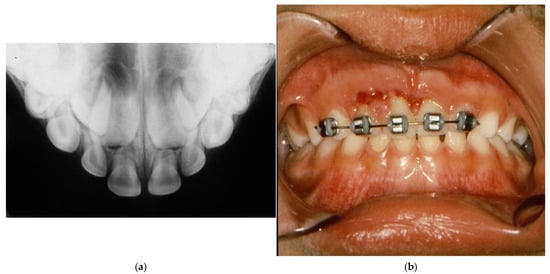
Figure 2.
(a) Intra-oral X-ray showing the root fracture of both upper maxillary incisors. (b) Treatment with orthodontic splinting (Group 1).
In Group 1, the orthodontic brackets were positioned in the middle third of the labial surface of the tooth and attachments belonging to the mini lines were preferred to avoid bulk and excessive retention of bacterial plaque and discomfort for the injured child. A 0.12–0.14 Australian round wire was typically used or, if possible, a passively matched NT 0.16 wire. The advantage of splint immobilization was the ability to synchronize tooth movement, which was especially important in cases of intrusive movement. In Group 2, a splint was performed in composite resin only (Figure 3a,b).
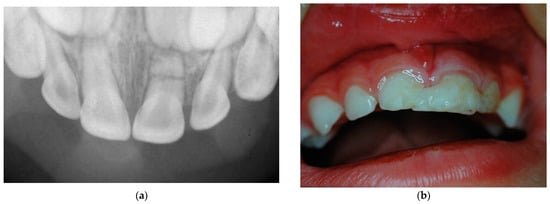
Figure 3.
(a) Intra-oral X-ray showing the root fracture of 61. (b) Splinting performed with composite resin only (Group 2).
The technique for resin splinting is simple and involves the following steps:
- Conditioning of the enamel of damaged and nearby teeth;
- Application of adhesive and composite material to the affected tooth and adjacent teeth;
- Light curing to harden the composite material.
It should be noted that a composite splint has a weak point in its increased tendency to fracture due to inter-dental occlusal forces. This treatment option was chosen in cases with unfavorable local conditions and/or uncooperative patients who would not tolerate the longer time required for bracket placement in orthodontic splinting.
2.2. Statistical Analysis
Statistical analysis was conducted by cross-tabulating the variables. Due to the limited number of observations a non-parametric test was performed using Fisher’s exact test, with a p < 0.005 that could be considered statistically significant. The statistical analysis was performed using Stata software, version 16.1 (StataCorp LLC, College Station, TX, USA).
3. Results
The results of the study are presented below, divided according to the specified search parameters.

Table 2.
Analysis of Group 1 samples. Legend: VCF—vestibular cortical fracture, OI—occlusal interference.

Table 3.
Analysis of Group 2 samples. Legend: VCF—vestibular cortical fracture, OI—occlusal interference.
3.1. General Data of the Selected Patients
Group 1 consisted of 15 males (66%) and 10 females (34%), with a mean age of 35.4 months (standard deviation: 7.09). Group 2 involved 23 males (66%) and 12 females (34%), with a mean age of 34.6 months (standard deviation: 6.8). There were no significant differences observed between the two groups in terms of age (p = 0.80) or gender (males representing the majority in both groups, 67.7% and 60.0%, respectively; p = 0.55).
3.2. Localization of the Trauma
In both Group 1 and Group 2, only maxillary central incisors were involved in the root fractures. In Group 1, the most commonly affected teeth were the left maxillary central incisors. Among the patients in Group 1, two patients had root fractures in both maxillary central incisors. In Group 2, the left maxillary central incisors were involved as frequently as the right maxillary central incisors. Among the patients in Group 2, root fracture of both maxillary central incisors occurred in three patients.
3.3. Etiology
In both Group 1 and Group 2, the most common etiological factor for root fractures was a non-specific fall accident. In Group 1, 36% of the traumas occurred at home, 36% in kindergarten, and 28% outdoors. In Group 2, 37% of the traumas occurred in the home, 26% in kindergarten, and 37% outdoors.
3.4. Location of the Root Fracture
In Group 1, the middle third of the root was involved in 68% of cases, the apical third in 24% of cases, and the cervical third in 8% of cases. In Group 2, the middle third of the root was involved in 91% of cases and the apical third in 9% of cases.
3.5. Presence of Dislocation with Extrusion
In Group 1, among the total affected teeth, extrusion occurred in 60% of cases, with 15% of cases showing palatal direction, 11% vestibular direction, and 33% without vestibular and/or palatal inclinations. In 36% of cases, there was no extrusion of the teeth affected by root fracture. In Group 2, among the total affected teeth, extrusion occurred in 53% of cases, with 18% of cases showing palatal direction, 8% vestibular direction, and 26% without vestibular and/or palatal inclinations. In 47% of cases, there was no extrusion of the teeth affected by root fracture.
3.6. Other Type of Trauma
In Group 1, among the total affected teeth, occlusal interference occurred in 33%, mobility in 15%, cortical bone fracture in 29%, while no other clinical signs occurred in 52% of cases. In Group 2, among the total affected teeth, occlusal interference occurred in 45% of cases, mobility in 18%, cortical bone fracture in 10% of cases, and no other clinical signs occurred in 26%.
3.7. Treatment Time after Trauma
In Group 1, 8% of cases were treated after 24 h, while 92% were treated within 2 to 24 h. No cases were treated within 2 h of the trauma. In Group 2, 60% of cases were treated within 2 h of the injury and 40% after 24 h.
3.8. Follow-Up
In both Group 1 and 2, patients were followed up continuously for 5 years. Follow-up visits were performed at 3, 7, 14, 30, 45, 60, and 90 days and then every 3 months until the corresponding permanent incisors erupted.
3.9. Reabsorption of the Apical Root Fragment
Periodic X-ray examinations were conducted to monitor the reabsorption of the distal fracture fragment of the root. This reabsorption typically became noticeable within 6 months of the trauma and was usually complete within 12/18 months. In Group 1, reabsorption of the apical fragment was observed in all cases, while in Group 2 it occurred in 76% of cases. Among the 29 cases in Group 2, where reabsorption of the apical root fragment was found, 17 teeth suffered from early loss. However, no significant statistical relationship was found (p = 0.532; Table 4) between the groups and the reabsorption of the apical root fragment.

Table 4.
Statistical analysis of apical fragment resorption.
4. Complications
4.1. Premature Loss of Deciduous Teeth
In Group 1, a total of 4 early deciduous tooth losses were observed out of 27 teeth involved (15%). In Group 2, 18 early primary tooth losses occurred among a total of 38 teeth (47%). A statistically significant relationship was found between the two groups (p = 0.008; Table 5), indicating a higher incidence of premature deciduous tooth loss in Group 2 compared with Group 1.

Table 5.
Statistical analysis of early loss.
4.2. PCO
In Group 1, there were 17 deciduous teeth that developed PCO out of a total of 27 teeth (63%). In Group 2, 10 deciduous teeth developed PCO (26%), considering that many of these teeth were lost early. A statistically significant relationship was found (p = 0.005; Table 6), indicating a higher incidence of PCO in Group 1 compared with Group 2.

Table 6.
Statistical analysis of PCO.
4.3. Changes in Permanent Teeth
In Group 1, the permanent incisors showed no coronal outcomes, except for a minor number that suffered from delayed eruption (3 teeth of 27). In Group 2, 10 permanent incisors among a total of 38 teeth showed delayed eruption.
4.4. Splinting Time
Group 1 was splinted for a duration of 60–90 days. Group 2, on the other hand, had a mean splinting time of 48.21 days.
5. Discussion
The main goals of diagnosis and management of traumatic dental injuries (TDIs) in children with primary dentition are to relieve pain and to prevent premature loss of the affected tooth [12,19,20,21,22].
However, there is a lack of studies in the contemporary literature that investigate the long-term consequences on the permanent dentition following TDIs involving primary dentition [23,24,25]. Notably, the period between 1 and 4 years of age represents a crucial developmental phase for the occurrence of central incisor disorders.
Close attention must be given to the proximity of the deciduous tooth root apex to the permanent germ, as improper management of traumatic dental injuries (TDIs) in primary teeth could cause more damage than the initial trauma itself. Several factors should be carefully considered, including the severity of tooth displacement, the presence of tooth mobility, the degree of root maturation, and the child’s compliance [20,21]. While there is limited documentation regarding the treatment of root fractures in deciduous teeth, the existing literature predominantly focuses on cases related to the management of lateral dislocation and intrusion [20,26,27,28,29]. The present retrospective investigation of etiological data in the analyzed samples aligns with findings reported in the literature, with accidental falls at home being the most prevalent cause, followed by incidents in school environments and during outdoor games [30]. Furthermore, studies indicate that the upper central incisors are the most commonly affected teeth in TDI cases [12,31].
The sample findings reported in this study align closely with the literature results. In Group 1, the protocols outlined in the latest International Association of Dental Traumatology (IATD) guidelines were followed [3,32]. In cases of root fracture, the affected tooth was delicately repositioned and orthodontically splinted to the adjacent teeth. It is important to highlight a significant distinction, namely that orthodontic splinting, which was predominant in Group 1, resulted in fewer instances of occlusal micro-trauma due to reduced interference with opposing teeth. Consequently, there were fewer cases of early tooth loss among the traumatized teeth (only 4 out of 25). In Group 2, where orthodontic splinting was not feasible, manual repositioning of teeth was performed when immediately possible. This group exhibited more occlusal micro-interferences, resulting in a higher occurrence of premature tooth loss and subsequent ectopic and delayed eruptions of corresponding permanent teeth. These findings were consistent with a retrospective study by Cho et al., which suggested that occlusal interference contributed to a poorer prognosis for traumatized teeth [14].
Based on the achieved outcomes, the authors recommend repositioning and splinting of the coronal fragment to prevent further traumatic injuries. This is crucial, since the coronal fragment is often displaced, resulting in trauma to the periodontal ligament that leads to a dislocation injury.
However, unlike dislocation injuries in intact teeth, the root coronal fragment is shorter, so is less resistant to subsequent trauma. The severity of sequelae in the permanent tooth depends on various factors, including the type of trauma to the primary tooth, the child’s age, the treatment performed, and the direction of tooth displacement [33,34]. In Group 2, some cases of hypoplastic coronal outcomes were observed. However, these events were unlikely to be connected to root fractures since the apical root fragment remained relatively stationary and did not impact with the neighboring germ of the developing permanent tooth [33,34]. It is more plausible that these outcomes were associated with previous unrecognized traumas, direct impact on the bone cortex, or non-traumatic (dysontogenic) origins [33,34].
However, timely and appropriate treatment, as well as follow-up care, can significantly reduce complications associated with traumatic dental injuries (TDIs). The International Association of Dental Traumatology (IATD) strongly recommends splint therapy as treatment for fractures and root extrusions [3]. In Group 1, orthodontic repositioning combined with splinting proved to be effective, yielding favorable outcomes even after the trauma. Instances of early tooth loss were minimal, with no occurrences of dental necrosis. PCO was observed in 68% of cases, which often follows dental luxation injuries and may or may not be accompanied by coronal dyschromia [16,35].
A significant statistical difference was found between Group 1 and Group 2 regarding PCO. In this context, it is pertinent to mention the study by Santos et al. [16], which evaluated 112 traumatized teeth over a 9-year follow-up period, finding no association between PCO and secondary pulp necrosis. The study cited above supports the notion that root canal obliteration in deciduous teeth is a phenomenon that does not require endodontic intervention unless accompanied by suppurative manifestations, as observed in immature permanent teeth that have undergone dislocation and are evolving towards asymptomatic PCO [36,37].
In Group 2, non-orthodontic splinting immobilized the traumatized tooth, which promoted temporary healing without altering its position. As a result, the tooth often remained in interference with the opposing tooth, leading to continued periodontal micro-traumas, which resulted in early tooth loss in 18 cases and occasionally led to negative consequences, such as particularly ectopia, in the permanent dentition. Similar to previous findings, a strong statistical significance was observed between Group 1 and Group 2 in this regard. The use of space maintainers could potentially mitigate this phenomenon if the loss of deciduous teeth occurred significantly distant from the time of dental replacement. However, this specific issue is beyond the scope of the current investigation.
Regarding the duration of splint maintenance, Group 1 had longer splinting periods (ranging between 60 and 90 days) compared with Group 2, where the splint was typically removed within 60 days. Given the higher frequency of complications observed in Group 2, it may be advisable to extend the duration of splinting, particularly in the presence of occlusal interference. Spinas et al., in a previous scoping review on the treatment of deciduous root fractures, also emphasized that the recommended average duration of splinting for teeth with root fractures was between 3 weeks and 3 months, with an average of 6 weeks [12]. In addition, supporting evidence came from the study by Liu et al. [11], which confirmed that, in cases of coronal fragment dislocation, it was necessary to reposition the fragment and extend the splinting duration. In their described case, which involved root fractures in both primary incisors, the approach consisted of repositioning the displaced coronal fragment (to reduce occlusal micro-trauma) and subsequent splinting using orthodontic brackets and stainless-steel wire. In their case, the splinting was maintained for a substantial period of 3 months, resulting in excellent outcomes and no damage to the permanent central incisors [11]. Another recent study, by Santos et al. [38], discussed a root fracture in a maxillary primary incisor treated with elastic splinting (orthodontic wire and composite) for a prolonged duration of 120 days, with no complications observed in the primary tooth until the eruption of the subsequent permanent central incisor, which also exhibited favorable outcomes [38].
However, it is important to note that maintaining a composite material splint alone in this age range can be challenging due to frequent detachments. As a result, a realistic time limit for splint duration is around 60 days.
Regarding the time interval between trauma and splinting, in this study, samples exhibited considerable variation. In Group 1, the splint was consistently applied more than two hours after the trauma but before midnight. Notably, the absence of necrosis and the infrequent occurrence of local complications (early tooth loss) were observed in this group.
Conversely, in Group 2, splinting was often performed within two hours of the trauma. However, despite the prompt intervention, the present group experienced a higher number of premature losses among the traumatized elements, indicating that early intervention alone did not significantly improve the prognosis of teeth affected by root fractures.
Furthermore, in this study atypical resorption of the apical fragment was identified, which was observed radiographically shortly after the initial trauma in some patients within the samples [39]. This phenomenon has received limited discussion and investigation in the scientific literature, as it exhibits distinct characteristics common both to physiological and pathological resorption.
Atypical root resorption (ARR), also referred to as irregular, lunate, or circumferential root resorption, manifests as a radiographic finding primarily seen in maxillary central deciduous incisors. Holan et al. defined it as “superficial resorption” along the lateral or apical margins of the root (associated with previous dental traumas demonstrating a peripheral circumferential resorption pattern) and can be classified into four different patterns: types I, II, III, and IV [37,40].
In the examined sample, the occurrence of apical resorption was observed homogeneously among both orthodontically splinted teeth (Group 1) and those instead not subjected to orthodontic splinting (Group 2). Radiographically, this phenomenon could be first detected within 6 months of the injury and was typically completed within 12 to 18 months. Therefore, it could be asserted that this type of resorption is characteristic and pathognomonic of root fractures in deciduous teeth, regardless of the type of splinting employed.
These findings were in line with the retrospective study by Cho et al. [14], which emphasized that splinting cannot be considered a primary cause of root resorption in deciduous teeth with root fracture.
Supporting the suggested hypothesis of this present study, the longitudinal observational study conducted by Nam et al. could be mentioned [39], which involved six patients with root fractures of maxillary deciduous incisors. In all six cases, regardless of the treatment approach chosen, this type of root resorption occurred without any associated pulp pathology, leading the authors to confirm that ARR represented a distinct healing process in deciduous root fractures that could be observed in long-term follow-up.
Statistical analysis further reinforced that the occurrence of this resorption event did not significantly differ between the two groups, affirming the authors’ hypothesis that ARR still transpired irrespective of the type of splinting employed.
Furthermore, another notable case, reported by Di Giorgio et al. [41], highlighted the combined conservative management of extrusion and root fracture in a maxillary deciduous central incisor that exhibited root resorption in the apical fragment characteristic of ARR after 12 months.
Lastly, a recent scoping review conducted by Spinas et al. [12], analyzing eight articles involving a total of 46 patients and 62 deciduous maxillary root fractures, showed that ARR appeared to be a physiological phenomenon regardless of the treatment modality employed.
6. Conclusions
In conclusion, the authors suggest that the treatment of root fractures in deciduous teeth can be improved by utilizing orthodontic splints, which help minimize occlusal micro-traumas.
This approach also reduces the risk of premature tooth loss and has positive implications for the development of permanent dentition.
It is finally important to underline that:
- -
- Early resorption of the distal fragment of the fractured root is a common and non-pathological healing phenomenon in primary teeth, typically occurring within one year of the trauma;
- -
- PCO in primary teeth does not require endodontic treatment unless accompanied by acute symptoms as suppurative manifestations.
However, there are still unanswered questions regarding pulpal responses and other aspects of these traumatic events. Further research is necessary to enhance clinicians’ knowledge and to improve treatment outcomes, with the ultimate goal of preventing unnecessary tooth loss in young patients.
Author Contributions
Conceptualization, E.S. and M.S.M.; methodology, E.S. and M.S.M.; software, S.C.; validation, E.S., M.S.M. and N.Z.; formal analysis, L.C.; investigation, E.S.; resources, M.S.M.; data curation, E.S.; writing—original draft preparation, E.S. and M.S.M.; writing—review and editing, E.S.; visualization, N.Z.; supervision, N.Z.; project administration, S.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Approved by the Medical Direction Board of the Surgical Science Department of the University of Cagliari (2020/13742).
Informed Consent Statement
Informed and written consent to the clinical and therapeutic investigations was obtained from the parents/legal guardians of all patients involved in the study.
Data Availability Statement
Data sharing not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Holan, G.; Needleman, H.L. Premature loss of primary anterior teeth due to trauma—Potential short- and long-term sequelae. Dent. Traumatol. 2013, 30, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, M.; De Carvalho Rocha, M.J. Traumatized Primary Teeth in Children Assisted at the Federal University of Santa Catarina, Brazil. Dent. Traumatol. 2002, 18, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Day, P.F.; Flores, M.T.; O’Connell, A.C.; Abbott, P.V.; Tsilingaridis, G.; Fouad, A.F.; Cohenca, N.; Lauridsen, E.; Bourguignon, C.; Hicks, L.; et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 3. Injuries in the primary dentition. Dent. Traumatol. 2020, 36, 343–359. [Google Scholar] [CrossRef] [PubMed]
- Bonanato, K.; Sardenberg, F.; Santos, E.R.; Ramos-Jorge, M.L.; Zarzar, P.M. Horizontal root fracture with displacement in the primary dentition. Gen. Dent. 2011, 57, e31-4. [Google Scholar]
- Bhayya, D.P.; Shyagali, T.R. Traumatic injuries in the primary teeth of 4- to 6-year-old school children in gulbarga city, India. A prevalence study. Oral Health Dent. Manag. 2014, 12, 17–23. [Google Scholar]
- Qassem, A.; Goettems, M.; Torriani, D.D.; Pappen, F.G. Radicular maturity level of primary teeth and its association with trauma sequelae. Dent. Traumatol. 2013, 30, 227–231. [Google Scholar] [CrossRef]
- Feldens, C.A.; Borges, T.S.; Vargas-Ferreira, F.; Kramer, P.F. Risk factors for traumatic dental injuries in the primary dentition: Concepts, interpretation, and evidence. Dent. Traumatol. 2016, 32, 429–437. [Google Scholar] [CrossRef]
- Andreasen, J.O.; Andreasen, F.M.; Andersson, L. Textbook and Color Atlas of Traumatic Injuries to the Teeth. Stomatol. EDU J. 2019, 6, 279. [Google Scholar] [CrossRef]
- Borum, M.K.; Andreasen, J.O. Therapeutic and economic implications of traumatic dental injuries in Denmark: An estimate based on 7549 patients treated at a major trauma centre. Int. J. Paediatr. Dent. 2001, 11, 249–258. [Google Scholar] [CrossRef]
- Petti, S.; Glendor, U.; Andersson, L. World traumatic dental injury prevalence and incidence, a meta-analysis-One billion living people have had traumatic dental injuries. Dent. Traumatol. 2018, 34, 71–86. [Google Scholar] [CrossRef]
- Liu, X.; Huang, J.; Bai, Y.; Wang, X.; Baker, A.; Chen, F.; Wu, L.-A. Conservation of root-fractured primary teeth-report of a case. Dent. Traumatol. 2013, 29, 498–501. [Google Scholar] [CrossRef] [PubMed]
- Spinas, E.; Di Giorgio, G.; Murgia, M.S.; Garau, V.; Pinna, M.; Zerman, N. Root Fractures in the Primary Teeth and Their Management: A Scoping Review. Dent. J. 2022, 10, 74. [Google Scholar] [CrossRef] [PubMed]
- dos Santos Fernandez, M.; Schuch, H.S.; Araújo, A.B.G.; Goettems, M.L. Splinting in the management of dental trauma in the primary dentition: A systematic review. Eur. Arch. Paediatr. Dent. 2023, 24, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Cho, W.C.; Nam, O.H.; Kim, M.S.; Lee, H.-S.; Choi, S.C. A retrospective study of traumatic dental injuries in primary dentition: Treatment outcomes of splinting. Acta Odontol. Scand. 2018, 76, 253–256. [Google Scholar] [CrossRef]
- Boorum, M.K.; Andreasen, J.O. Sequelae of trauma to primary maxillary incisors. I. Complications in the primary dentition. Dent. Traumatol. 1998, 14, 31–44. [Google Scholar] [CrossRef] [PubMed]
- dos Santos, B.Z.; Cardoso, M.; Almeida, I.C.S. Pulp canal obliteration following trauma to primary incisors: A 9-year clinical study. Pediatr. Dent. 2011, 33, 399–402. [Google Scholar]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed]
- Flores, M.T. Traumatic injuries in the primary dentition. Dent. Traumatol. 2002, 18, 287–298. [Google Scholar] [CrossRef]
- Faria, L.V.; Chaves, H.G.D.S.; Silva, E.A.B.; Antunes, L.D.S.; Antunes, L.A.A. Minimally invasive treatment of an extruded deciduous tooth—Case report. Dent. Traumatol. 2020, 36, 303–306. [Google Scholar] [CrossRef]
- Abreu, M.G.L.; Milani, A.J.; Fernandes, T.D.O.; Gomes, C.C.; Antunes, L.S.; Antunes, L.A.A. Dental trauma in primary dentition, its effect on permanent successors and on Oral Health-Related Quality of Life: A 4-year follow-up case report. Int. J. Burns Trauma 2020, 10, 201–209. [Google Scholar]
- Berger, T.D.; Kenny, D.J.; Casas, M.J.; Barrett, E.J.; Lawrence, H.P. Effects of severe dentoalveolar trauma on the quality-of-life of children and parents. Dent. Traumatol. 2009, 25, 462–469. [Google Scholar] [CrossRef] [PubMed]
- Karataş, M.S.; Sönmez, I. Developmental Disturbances of a Maxillary Central Incisor due to Trauma to Its Predecessor: A Case Report. Med. Princ. Pr. 2013, 22, 590–592. [Google Scholar] [CrossRef] [PubMed]
- Mello-Moura, A.C.; Bonini, G.A.; Suga, S.S.; Navarro, R.S.; Wanderley, M.T. Multidisciplinary approach on rehabilitation of primary teeth traumatism repercussion on the permanent successor: 6-year follow-up case report. J. Indian Soc. Pedod. Prev. Dent. 2009, 27, 125–130. [Google Scholar] [CrossRef] [PubMed]
- Arenas, M.; Barberia, E.; Lucavechi, T.; Maroto, M. Severe trauma in the primary dentition—Diagnosis and treatment of sequelae in permanent dentition. Dent. Traumatol. 2006, 22, 226–230. [Google Scholar] [CrossRef]
- Huang, B.; Marcenes, W.; Croucher, R.; Hector, M. Activities related to the occurrence of traumatic dental injuries in 15- to 18-year-olds. Dent. Traumatol. 2009, 25, 64–68. [Google Scholar] [CrossRef]
- Fidalgo, T.K.; Maia, L.C. Minimally invasive intervention of acute trauma in the primary dentition: Successful five-year follow-up. Gen. Dent. 2012, 60, e158-61. [Google Scholar]
- Ruviére, D.B.; Costa, M.M.; Cunha, R.F. Conservative management of severe intru-sion in a primary tooth: A 4-year follow-up. J. Dent. Child. 2009, 76, 87–91. [Google Scholar]
- Charone, S.; Kuchler, E.; Costa, M.D.C.; Maia, L. A successful outcome using a minimal invasive approach to manage a severe trauma to the primary maxillary incisor in a toddler. Dent. Traumatol. 2010, 26, 294–297. [Google Scholar] [CrossRef]
- de Amorim, L.F.G.; da Costa, L.R.R.S.; Estrela, C. Retrospective study of traumatic dental injuries in primary teeth in a Brazilian specialized pediatric practice. Dent. Traumatol. 2011, 27, 368–373. [Google Scholar] [CrossRef]
- Lin, S.; Pilosof, N.; Karawani, M.; Wigler, R.; Kaufman, A.Y.; Teich, S.T. Occurrence and timing of complications following traumatic dental injuries: A retrospective study in a dental trauma department. J. Clin. Exp. Dent. 2016, 8, e429–e436. [Google Scholar] [CrossRef]
- Levin, L.; Day, P.F.; Hicks, L.; O’Connell, A.; Fouad, A.F.; Bourguignon, C.; Abbott, P.V. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: General introduction. Dent. Traumatol. 2020, 36, 309–313. [Google Scholar] [CrossRef]
- Spinas, E.; Melis, A.; Savasta, A. Therapeutic approach to intrusive luxation inju-ries in primary dentition. A clinical follow-up study. Eur. J. Paediatr. Dent. 2006, 7, 179–186. [Google Scholar] [PubMed]
- La Monaca, G.; Pranno, N.; Vozza, I.; Annibali, S.; Polimeni, A.; Bossù, M.; Cristalli, M.P. Sequelae in permanent teeth after traumatic injuries to primary dentition. Minerva Dent. Oral Sci. 2019, 68, 332–340. [Google Scholar] [CrossRef] [PubMed]
- Lopes, T.D.S.; Santin, G.C.; Marengoni, L.A.; Crispim, J.B.; Ceron, L.C.; Fracasso, M.D.L.C. Clinical and Radiographic Sequelae in Primary Teeth due to Dental Trauma. Pesqui. Bras. Odontopediatria Clin. Integr. 2019, 19, e4526. [Google Scholar] [CrossRef]
- Spinas, E.; Deias, M.; Mameli, A.; Giannetti, L. Pulp canal obliteration after extrusive and lateral luxation in young permanent teeth: A scoping review. Eur. J. Paediatr. Dent. 2021, 22, 55–60. [Google Scholar] [CrossRef]
- Spinas, E.; Giannetti, L.; Mameli, A.; Re, D. Dental injuries in young athletes, a five-year follow-up study. Eur. J. Paediatr. Dent. 2018, 19, 187–193. [Google Scholar] [CrossRef]
- Santos, L.V.; da Hora, K.C.; Alves, A.C. Successful minimally invasive intervention in a primary central incisor after root fracture: A case report. Dent. Traumatol. 2021, 37, 807–812. [Google Scholar] [CrossRef]
- Nam, O.H.; Kim, M.S.; Kim, G.T.; Choi, S.C. Atypical root resorption following root fractures in primary teeth. Quintessence Int. 2017, 48, 793–797. [Google Scholar] [CrossRef]
- Holan, G.; Yodko, E.; Sheinvald-Shusterman, K. The association between traumatic dental injuries and atypical external root resorption in maxillary primary incisors. Dent. Traumatol. 2015, 31, 35–41. [Google Scholar] [CrossRef]
- Di Giorgio, G.; Zumbo, G.; Saccucci, M.; Luzzi, V.; Ierardo, G.; Biagi, R.; Bossù, M. Root Fracture and Extrusive Luxation in Primary Teeth and Their Management: A Case Report. Dent. J. 2021, 9, 107. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).